Abstract
Computational drug repurposing methods adapt Artificial intelligence (AI) algorithms for the discovery of new applications of approved or investigational drugs. Among the heterogeneous datasets, electronic health records (EHRs) datasets provide rich longitudinal and pathophysiological data that facilitate the generation and validation of drug repurposing. Here, we present an appraisal of recently published research on computational drug repurposing utilizing the EHR. Thirty-three research articles, retrieved from Embase, Medline, Scopus, and Web of Science between January 2000 and January 2022, were included in the final review. Four themes, (1) publication venue, (2) data types and sources, (3) method for data processing and prediction, and (4) targeted disease, validation, and released tools were presented. The review summarized the contribution of EHR used in drug repurposing as well as revealed that the utilization is hindered by the validation, accessibility, and understanding of EHRs. These findings can support researchers in the utilization of medical data resources and the development of computational methods for drug repurposing.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
It takes an average of 13 years and 2–3 billion dollars to bring a new drug from bench to bedside, with the process comprising examination of its efficacy, toxicity, and pharmacokinetic and pharmacodynamic profiles in cell- and animal-based studies to safety and efficacy in human subjects in clinical trials1. The escalating cost and length of time make drug development a less desirable business for investment2. Drug repurposing, on the other hand, aims to discover new medical indications for an approved or investigational drug. As the dosing and safety of the drug are well studied, clinical trials can be accelerated, significantly reducing the development time and cost. There are some successful examples of drug repurposing, such as the usage of metformin for various cancers3, sildenafil citrate for erectile dysfunction, and thalidomide for erythema nodosum leprosum (ENL) and multiple myeloma.2
The most critical task of drug repurposing is to identify new associations between drugs and diseases. Traditional biomedical experiments are based on binding assays and phenotypic screening, which are expensive and time-consuming. Conversely, in-silico methods gain their popularity through the analysis of heterogeneous data based on Artificial intelligence (AI) methods4, such as genetic association analysis, pathway mapping, molecular docking, and signature profile matching5, as such methods allow for all analysis to be done computationally in a time and cost-efficient manner. Computational drug repurposing can utilize a diverse set of data resources, including omics data (e.g., gene and protein expression)6, biomedical association/relation knowledgebase7, biomedical literature8, and the electronic health record (EHRs)6. Big EHR datasets offer a real-world perspective rooted in clinical care that provides rich longitudinal diagnostic and pathophysiological patient data, which can facilitate the generation and validation of drug repurposing hypotheses (e.g., statistical significance)3. The unique capability of incorporating EHR-based data into repurposing methods is the ability to test a large number of drug repurposing hypotheses in parallel by identifying the cohorts that either have or have not been prescribed a particular medication using large patient populations followed for several years9. For this reason, EHR-based drug repurposing has been identified as a unique, cost-effective opportunity by the drug development field, and a diverse set of applications have been proposed, including phenome-wide association studies (PheWAS) based on statistic tests10,11,12, similarities based on disease network6,13, and association rule-based interaction mining14.
In this survey, we reviewed current computational drug repurposing approaches utilizing EHR-based data. We retrieved 1145 combined results containing 1370 publications from four databases (i.e., Embase, Medline, Scopus, and Web of Science) between January 2000 and January 2022, in which 33 articles were included in the final review. Compared to the existing surveys5,13,15,16, we systematically investigated the relevant studies from four perspectives, (1) publication venue, (2) data types and sources, (3) method used for data processing and drug repurposing prediction, and (4) disease targeted, the validation for the experiment, and tools released. We learned that, compared to validation, EHR is mainly used for building the predictive models, where drug effects on laboratory tests, drugs used for diseases, genetic mutations related to diseases, and disease-laboratory tests associations were the most popular data used among all the studies. While EHR datasets have gained popularity in drug repurposing, the utilization is hindered by the validation (e.g., discoveries are unverifiable using other available knowledge derived from published literature and clinical trial and application), the accessibility (e.g., the release and sharing of datasets and tools due to patients’ privacy), and understanding (e.g., adaptations of NLP tools and standardization). This study enabled us to gain a more concrete understanding of how the EHR is utilized in a drug repurposing context and to provide potential guidelines for designing the EHR-based drug repurposing methods.
Results
We abstracted 33 articles based on four themes with the following flow, (1) journal and articles, (2) data used, (3) methods, and (4) results of repurposing. During the process for each theme, important data elements were identified by the first author and validated by all seven reviewers. The synthesis of the articles for each data element was conducted by each reviewer. The results were finally validated and organized by the first author. The disagreements in synthesis were resolved among all the reviewers in the consensus meeting. The general summarization of the articles is shown in Supplementary Table 1. The flow details for each article can be found in Supplementary Method 1.
Publication venue
The 33 papers reviewed consisted of 29 journals and four conference articles (see Fig. 1). We manually categorized those articles into three types: (1) Computer Science, (2) Informatics/Biomedical Informatics, and (3) Medicine/Biology/Pharmacology. The majority of the articles were Informatics/Biomedical (n = 22) and Medicine/Biology/Pharmacology (n = 10). We also noticed that the conference articles were Informatics/Biomedical, suggesting this topic or methodology is more popular among the Biomedical Informatics community. Most studies were conducted in the United States (n = 22), with the remainder being scattered amongst Asian and European countries. In addition, the topic of EHR-based drug repurposing gains popularity from the year 2012 (n = 1) to 2021 (n = 10).
Data
The majority of studies relied on the EHR from an institution affiliated with either the authors themselves (e.g., Vanderbilt University Medical Center17,18,19) or one of their collaborators (e.g., Mayo Clinic18,19). Only three studies utilized publicly available datasets, including IBM Watson Health Explorys database20, MIMIC-II21, and adverse event reporting systems (AERSs)22. Most of the studies used only EHR, while others utilized multiple kinds of sources to facilitate the drug repurposing, such as knowledge bases (N = 11), Omics databases (N = 7) (Please note, we distinguished Omics data from EHR data) (see Supplementary Fig. 2a). Among all the association knowledge bases, drug-gene information was the most popular (see Supplementary Fig. 2b). Drugbank23 was the main source of drug-gene (protein) information in the studies (N = 11). We noticed widespread usage of biomedical repositories, such as Sider24 for side effect information (N = 3) and OMIM25 for gene-disease relations (N = 2).
Amongst all the 22 EHR data types covered in our survey, medication (N = 22), diagnosis (N = 19), lab test (N = 17), and demographic (N = 16) were the most frequently used (see Fig. 2a). Most studies were conducted based on patient cohort sizes of less than 10,000 (N = 8), 10,000 to 100,000 (N = 6), and 100,000 to 1,000,000 (N = 6) (see Fig. 2b). We note that a few studies did not specify the size of the patient cohort used (N = 3). Supplementary Table 2 shows the detailed information of the data in the reviewed studies.
Drug repurposing methods
Figure 3 shows the number of papers with different data processing methods for EHR data regarding natural language processing (NLP), standardization, or temporal data processing. Of the surveyed studies, five studies utilized NLP to process their data, seven used standardization, and four dealt with temporal data. We note that three studies implemented more than one data processing method (e.g., MedEx and RxNorm CUI were used to extract and standardize medication information19, and the Observational Medical Outcomes Partnership Common Data Model (OMOP CDM) was used for both drug prescription and laboratory tests26).
NLP pipelines were used to extract a diverse set of information that differed depending on individual study needs. For example, drugs and diseases were extracted from triads of sentences by using MetaMap21. Regarding the adoption of standardization methods, standardization efforts are mainly focused on using standard terminologies for medical concepts. For example, Proteomics Standard Initiative—Molecular Interactions (PSI-MI) codes were used for proteomics, Gene Ontology (GO) for genomics, Anatomical Therapeutic Chemical (ATC) codes for drugs, and ICD-10 and Online Mendelian Inheritance in Man (OMIM) for disease data27. Similarly, Systematized Nomenclature of Medicine-Clinical Terms (SNOMED CT) was also used for diseases, RxNorm for drugs, logical observation identifier names and codes (LOINC) for Laboratory tests20, standard billing codes for clinical phenotypes28, and Unified Medical Language System (UMLS) for multiple kinds of biomedical related concepts29. Temporal information was primarily used to track disease progression. For example, temporal data was used in one study to analyze the association between the virological status of patients and all-cause mortality as well as other individual-level factors30. Supplementary Table 3 shows the summary information of data processing in the studies.
As shown in Fig. 3, statistical analysis and machine learning are two predominant computational approaches used for drug repurposing through mining a large set of health data. In statistical analysis methods, statistical models and tests are used to determine the effect of drugs on disease targets or other related clinical variables such as genes and laboratory tests. For example, Wang et al.31 searched drug and gene information from public pharmacological and genomic databases as well as private EHRs for glaucoma diseases. It used p values based on the chi-square tests and false discovery rates (FDR) of drugs targeted to glaucoma genes/diseases to detect potential treatment candidates. For example, the prevalence of glaucoma was 0.11% in theophylline-treated patients, and 0.058% in celecoxib-treated patients, suggesting these drugs may have antiglaucoma effects as the incidence of glaucoma was significantly lower in these drug-use cohorts than in healthy individuals. Wu et al.19 classified a patient cohort into two comparison groups—an exposure group with drug prescription and a non-exposure group without drug prescription and applied cox regression to measure the association of drugs with cancer survival for suggesting repurposing candidates. Goldstein et al.17 used logistic regression (or multivariate regression) and derived p values to examine the association between drug candidates and genetic mutation (or glucose tolerance test) data for identifying drug repurposing candidates for gestational diabetes.
Machine learning is another type of common computational approach for predicting new disease targets of existing drugs. Three popular machine learning methods are based on similarity/interaction network, the least-square optimization method, and deep learning. For instance, Zhou et al.20 developed a network-based prediction system of disease-target interactions by modeling phenotypic and genetic relationships among drugs, side effects, diseases, and genes for identifying repositioned drug candidates. Ghalwash et al.32 formulated the problem of finding drugs that have an effect on the levels of laboratory test results as a regularized least-square unconstrained convex optimization problem. Liu et al.33 created a high-throughput screening framework with existing large-scale real-world data. The framework extracted potential repurposing drug ingredients, identifies the corresponding user and non-user sub-cohorts, computes features and disease progression outcomes for all patients in both sub-cohorts, and estimates the treatment effects using deep learning methods. Supplementary Table 4 summarizes the computational methods in detail.
Evaluation of EHR-based computational drug repositioning research is critical to ensure valid and reliable computation methods and new signals. Unlike predictive modeling or adverse drug reaction detection, where the gold standard outcomes can be well defined, there may be a lack of well-established evidence or ground truth to validate the newly discovered target signals in drug repositioning research. Therefore, the evaluation may rely on multiple internal and external sources of evidence. Figure 4 summarizes the sources for training and validation. Of the 33 papers reviewed, six did not present any methods for assessing drug performance. Of the 27 that did, the most common performance metrics used were machine learning related (e.g., precision-recall, AUC-ROC). Risk ratios (e.g., hazard, odds, and relative risk) were commonly reported to evaluate the effectiveness of candidate drugs. With respect to validation, 12 papers performed validation of any hypothesis candidate drugs against other data sources based on EHR data, ten based on biomedical literature, and nine based on public knowledge bases.
The EHR is the most frequently reported source for training and validation since it contains rich, dense, and longitudinal information. The drug effects on laboratory tests were mainly used in building predictive models (N = 12). For validation, Drug-Disease information (N = 6) observed in the EHR is mainly used. Please note, that a dataset can be both used for training and validation. The validation can be conducted by retrospectively analyzing EHR data to estimate the usage and effects of the candidate drug. For example, Wang et al. searched EHR data to obtain information on the usage of the candidate drugs and glaucoma31. Due to potential issues of data quality or information representation (e.g., unstructured text), manual chart reviews are often required when leveraging EHR for evaluation. Cai et al. conducted a chart review of EHRs based on randomly selected 20 participants to determine the accuracy of newly identified phenotypes34. In addition to EHRs, external databases such as Drugbank and clinical trials databases can be great resources for evaluation purposes. One common way of leveraging these databases is through study replication, a method by which target associations are reproduced using the same computational methods on a different dataset, and the difference in the study outcomes is statistically compared. Cai et al.34 used two additional external data sources BioVU and UK Biobank to cross-examine the association between a genetic variant and coronary heart disease phenotypes. Xu et al.35 performed a comprehensive performance comparison to the existing state-of-the-art drug repositioning methods to reveal the advantages of the proposed methods. Out of 33 articles, two studies27,35 conducted an additional laboratory study to validate the potential therapeutic effect on animal models and demonstrated additional validity to the proposed methods.
Due to the lack of ground truth and potential EHR-related data quality issues, we recommend having multiple evaluations on different data sources. We found that 13 out of 33 studies reported more than one evaluation method. For example, Wu et al.19 incorporated two different validation methods: (1) supporting evidence from biomedical literature, and (2) supporting evidence from human interventional cancer trials. Paik et al. 27 used computational evaluation (tenfold cross-validation) on known associations in a vivo zebrafish model of ALS. Hsieh et al. 36 validated the candidate drugs through both in vitro drug screening and real-world population-based studies leveraging EHRs. Supplementary Table 5 summarizes the validation methods in detail.
Drug repurposing results
Figure 5 shows the disease targeted. The most common repurposing target was diabetes-related, consisting of 10 out of the 33 publications17,26,29,32,37,38,39,40,41,42, including type 2 diabetes37,41,42, gestational diabetes17, diabetes (unspecified)26,29, diabetes-related tests including glycated hemoglobin32 and Fasting Blood Glucose38,39,40. Six publications did not focus on any specific diseases21,22,27,28,43,44. For example, Dang et al.21 aimed to establish a generic process and method to integrate phenomic data in EHR with omic and drug data.
Cardiovascular-related diseases are also focused on in seven publications. Specifically, Jang et al.41 targeted congestive heart failure, myocardial ischemia, and stroke, Ghalwash et al.32 targeted low-density lipoprotein, which is a risk factor for cardiovascular and vascular diseases, Kim et al.26 targeted dyslipidemia, Cai et al.34 targeted cardiovascular disease, Liu et al.33 targeted coronary artery disease, Nordon et al.29 targeted hypertension, and 366 targeted coronary heart disease, congestive heart failure, heart attack, and stroke. In addition, there are four publications targeting at cancer18,19,35,45, three targeting at COVID36,46,47, two targeting at asthma41,42.
It is worthwhile to note that some of the reviewed articles did not report on specific drugs, but rather presented a selection of top n repurposed drug candidates as determined by their respective methodologies. Of those that did subset reported drugs, they were typically sub-selected by certain drug types, such as statins, triptans, PPIs, and nasal steroids in one study, α1‐adrenoceptor antagonists in another, and antihypertensive calcium channel blockers in a third. Of the 33 studies reviewed, only five reported results focused on a single drug, metformin in the case of Xu et al.18, febuxostat in the case of Muraki et al.48, terbutaline sulfate in the case of Paik et al.27, Fluoxetine in the case of Bi et al.45, and Dextromethorphan in the case of Cummings et al.49. Intuitively, this finding makes sense as most methods are focused on presenting candidates for further screening rather than having a pre-existing drug that should be further studied, and as such methods would result in a selection of candidates that should then be cross-validated against known clinical indications for method validity, rather than a clinical validation of an individual drug itself selected from said list of candidates. Supplementary Tables 1, 6 show the drugs explored and the corresponding diseases targeted in detail.
Data and tools published
Despite the widespread and vital use of EHR data for drug repurposing research, datasets and tools were not readily electronically available to the public in many of the surveyed studies. Table 1 shows the publically shared data and tools among the reviewed studies. Only 1 study33 of the 33 reviewed studies can be fully reproducible with publically available EHR and the tool so as to verify the original studies to follow-up studies. In terms of the dataset, seven of these studies used publicly open EHR datasets: IBM Watson Health Explorys database20,50,51, IBM Health MarketScan database33,45,51, and MIMIC-II21, which are the only research that shared their original dataset, Vanderbilt Synthetic Derivatives database17, through data use agreement. From the perspective of sharing developed tools, five studies shared their own tools28,29,33,36,42. In contrast, others indicated open software, which they used, without their practical implementations20,27,45. Lastly, some of the studies shared the analysis and results in the form of supplements or separated links19,26,27,31,33,35,36,41,42,44,45,46,47,49,50,51,52.
Discussion
EHRs are an invaluable source of large-scale clinical data capable of simulating drug repurposing strategies in an uncontrolled, real-world environment as opposed to the controlled environment of clinical trials, which is one of the biggest benefits of drug repurposing. EHRs were gaining popularity in diverse applications for drug repurposing, such as COVID 1953, or the upstream applications (e.g., providing a support/input resource for other applications, medical cost reduction43) and downstream applications (e.g., utilizing the results from other applications as an input). In this paper, we systematically reviewed the literature published between 2000 and 2022 to better understand how EHR datasets are directly utilized to facilitate drug repurposing. In the course of our review, we noted the following considerations when applying EHR data to drug repurposing tasks:
Firstly, as the real-world evidence (RWE), EHRs provide clinical evidence with a heterogeneous set of healthcare data captured outside the existing paradigms and standards of the drug development process, which has tremendous value by improving the applicability of the results to a real-world environment54. As such, more than 90% of pharmaceutical companies make RWE investments across the entire life cycle in drug development55. Compared to pharmaceutical companies, research organizations have limited resources to leverage heterogeneous healthcare datasets from multiple sources. The risk of biased results caused by the limited EHR drives the academic organizations to focus more on the studies in a controlled environment (e.g., clinical trials), which is the main reason that we have only 33 articles fitting the inclusion criteria.
Secondly, a substantial (50%) proportion of reviewed papers performed their validation tasks via cross-referencing data, either against the EHR itself when the hypothesis generation methodology did not incorporate that data, or other data sources such as biomedical literature, clinical trials, public knowledge bases, and drug information datasets when it did. Fundamentally, this suggests that the knowledge contained in any one of these data sources is likely to be present within some amalgamation of the others. This observation reflects the reality of the EHR itself—the EHR contains a record of clinical decision making, which, with some rare aberrations, is typically reflective of contemporaneous best practices which are themselves reflections of known medical knowledge derived from published literature and empirical observations and evaluated through clinical trial and application. It is therefore rare that a hypothesis generated by some in-silico EHR-based framework will be unverifiable using other available knowledge—instead, we postulate that the value in bringing in EHR data for drug repurposing tasks lies in its reflection of real-world considerations such as evaluating and alleviating the impact of socioeconomic determinants of health on drug choices and identifying alternative therapies, as opposed to other knowledge sources which are typically conducted in more controlled environments (particularly those studies involving pure physical/chemical simulation).
Thirdly, the biggest issue of EHR-based methods is the inaccessibility of any data involved56. Thus only primary academic medical centers can fully leverage any advantages of utilizing EHR-based methods. While sharing data and tools across collaborating healthcare providers or institutions as a small group may be feasible while the study is ongoing, there is a rare movement to deposit the data and tools for public usage. The main barrier is rooted in protecting the privacy of patient health data. Therefore, significant burdens and efforts are additionally required for researchers to provide freely available resources. For example, additional funds and efforts are required to perform the de-identification process of the given EHR (e.g., MIMIC-II21) or further ongoing management to process restricted data use agreement (e.g., Vanderbilt Synthetic Derivatives database17) is essential. Furthermore, advanced data processing methods (e.g., NLP) are needed for handling unstructured data, different data formats, bias (e.g., more expensive drugs are more likely to be prescribed like lenalidomide for multiple myeloma)3, and missing data5. Standardization of EHR (e.g., Fast Healthcare Interoperability Resources and OMOP Common Data Model) to represent data elements in a standardized format (e.g., terminologies or coding systems) may be a good investment to support computational pipelines.
Lastly, EHR provides large longitudinal medical records in clinical settings, which improves the applicability/reliability of the predictive models. However, temporal information is seldom incorporated into the experiment. The data model that incorporates temporal information will reduce the bias in the validation. Another issue of EHR-based methods is that they cannot reveal causality56. More mechanisms (e.g., biological pathways related to drug targets) need to be studied to better understand the toxicity and tolerability of drugs in humans. The leverage of genetic information provides another potential to improve the performance and interpretability of drug repurposing. For example, both the eMERGE network and the All of US Initiative link EHR to genetic information for multisite studies11. The integration of EHR and patients’ genetic information will increase the number of features (e.g., phenotypes and genotypes) to further promote the development of drug repurposing.
There are a few limitations in this review that must be mentioned. Firstly, while the authors tried their best to conduct a comprehensive review, the authors acknowledge that some bias may still exist in the selection, filtering and review of the papers due to the perspectives and backgrounds of the authors. Additionally, some related articles published may not be included due to the selection of search strings, databases, and language. For instance, in some studies57,58,59, where usage of EHR is not explicitly mentioned in the text and inferred by a human reader, thus causing them to not be retrieved by our search query. Secondly, this review only focused on the studies that directly used EHR for drug repurposing, and studies that used EHR (e.g., a follow-up study based on a study utilizing EHR to explore epilepsy and twelve autoimmune diseases60) indirectly to facilitate drug repurposing are excluded. We acknowledged that some studies excluded may be potentially important and provide new methods of leveraging EHR. It is worth noting that the scope of our review is limited only to the methodologies involved in drug repurposing utilizing EHR data. There are, however, other factors that can affect the viability and efficiency of such methods, including questions surrounding the source EHR data itself, such as how patients relevant to the studies in question are identified, computational representation of EHR data, and varying methods to render EHR data more computationally accessible, such as natural language processing. While studies on these topics have been excluded from our review due to being out of scope, their importance to the overall topic cannot be understated, and we would encourage readers to further review existing works on the different applications of EHR (e.g., refs. 61,62,63,64) as such topics will have a profound impact on the feasibility and performance of many of the methodologies discussed in this review. In addition, while there are sub-topics in EHR-related studies (e.g., EHR data harmonization, high dimensionality, confounding adjustment, patient matching) critical to our survey, we are unable to discuss them in our manuscript as those topics are not sufficiently presented in the reviewed papers. We further suggest the readers refer to the surveys on those topics (refs. 65,66,67,68) for a more comprehensive discussion.
Methods
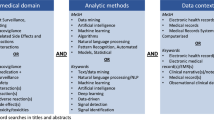
We followed Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) guidelines69 to perform our review. We conducted a thorough search which was restricted to the full-length research articles published in journals and conference proceedings from four databases (Embase, Medline, Scopus, and Web of Science) published within 22 years (i.e., January 1, 2000, to Jan 10, 2022). We only included the original research articles written in English and excluded those in the forms of review, abstract, poster, podium, commentary, perspective, note, and editorial. The detailed keywords used as tailored for each database are provided in Supplementary Note 1.
Our literature search obtained 1145 combined results that consisted of 1370 distinct articles (one result may contain multiple articles in one conference proceeding). Seven reviewers (Y.Z., S.M., S.F., L.W., M.H., Y.Y., and A.W.) independently reviewed the titles and abstracts of these articles and filtered out those studies which are (1) not computational drug repurposing, (2) did not utilize EHR data in the modeling or experimenting, (3) are not full research article (e.g., conference and journal) with two round reviews. The excluded articles were double-checked by the first author, NZ. Any disputation of the exclusion is discussed and resolved among the reviewers. This survey focuses on the remaining 33 research articles. A flow chart of how the articles were filtered and reviewed is shown in Fig. 6.
Data availability
Any data generated or analyzed are included in this article and the Supplementary Information files. Aggregate data analyzed in this study are available from the corresponding author on reasonable request.
References
Yella, J. K., Yaddanapudi, S., Wang, Y. & Jegga, A. G. Changing trends in computational drug repositioning. Pharmaceuticals 11, 57 (2018).
Pushpakom, S. et al. Drug repurposing: progress, challenges and recommendations. Nat. Rev. Drug Discov. 18, 41–58 (2019).
Zhang, Z. et al. Overcoming cancer therapeutic bottleneck by drug repurposing. Signal Transduct. Target. Ther. 5, 1–25 (2020).
Jang, I.-J. Artificial intelligence in drug development: clinical pharmacologist perspective. Transl. Clin. Pharmacol. 27, 87 (2019).
Xu, H., Li, J., Jiang, X. & Chen, Q. Electronic health records for drug repurposing: Current status, challenges, and future directions. Clin. Pharmacol. Ther. 107, 712–714 (2020).
Chen, B. & Butte, A. Leveraging big data to transform target selection and drug discovery. Clin. Pharmacol. Ther. 99, 285–297 (2016).
Zong, N. et al. Drug–target prediction utilizing heterogeneous bio-linked network embeddings. Brief. Bioinforma. https://doi.org/10.1093/bib/bbz147 (2019).
Zheng, S., Dharssi, S., Wu, M., Li, J. & Lu, Z. Text mining for drug discovery. Methods Mol. Biol. 1939 231–252 (2019).
Hodos, R. A., Kidd, B. A., Shameer, K., Readhead, B. P. & Dudley, J. T. In silico methods for drug repurposing and pharmacology. Wiley Interdiscip. Rev. Syst. Biol. Med. 8, 186–210 (2016).
Banerjee, A. G., Khan, M., Higgins, J. & Das, A. K. In 2015 International Conference on Healthcare Informatics. 390–397 (IEEE, 2015).
Denny, J. C., Van Driest, S. L., Wei, W. Q. & Roden, D. M. The influence of big (clinical) data and genomics on precision medicine and drug development. Clin. Pharmacol. Ther. 103, 409–418 (2018).
Kingsmore, K. M., Grammer, A. C. & Lipsky, P. E. Drug repurposing to improve treatment of rheumatic autoimmune inflammatory diseases. Nat. Rev. Rheumatol. 16, 32–52 (2020).
Yao, L., Zhang, Y., Li, Y., Sanseau, P. & Agarwal, P. Electronic health records: Implications for drug discovery. Drug Discov. Today 16, 594–599 (2011).
Davazdahemami, B. & Delen, D. The confounding role of common diabetes medications in developing acute renal failure: a data mining approach with emphasis on drug-drug interactions. Expert Syst. Appl. 123, 168–177 (2019).
Roden, D., Xu, H., Denny, J. & Wilke, R. Electronic medical records as a tool in clinical pharmacology: opportunities and challenges. Clin. Pharmacol. Ther. 91, 1083–1086 (2012).
Singh, G., Schulthess, D., Hughes, N., Vannieuwenhuyse, B. & Kalra, D. Real world big data for clinical research and drug development. Drug Discov. Today 23, 652–660 (2018).
Goldstein, J. A. et al. Calcium channel blockers as drug repurposing candidates for gestational diabetes: Mining large scale genomic and electronic health records data to repurpose medications. Pharmacol. Res. 130, 44–51 (2018).
Xu, H. et al. Validating drug repurposing signals using electronic health records: a case study of metformin associated with reduced cancer mortality. J. Am. Med. Inform. Assoc. 22, 179–191 (2014).
Wu, Y. et al. Discovery of noncancer drug effects on survival in electronic health records of patients with cancer: a new paradigm for drug repurposing. JCO Clin. Cancer Inform. 3, 1–9 (2019).
Zhou, M., Zheng, C. & Xu, R. Combining phenome-driven drug-target interaction prediction with patients’ electronic health records-based clinical corroboration toward drug discovery. Bioinformatics 36, i436–i444 (2020).
Dang, T.-T., Ouankhamchan, P. & Ho, T.-B. In 2016 IEEE RIVF International Conference on Computing & Communication Technologies, Research, Innovation, and Vision for the Future (RIVF) 223–228 (IEEE, 2016).
Tatonetti, N. P., Patrick, P. Y., Daneshjou, R. & Altman, R. B. Data-driven prediction of drug effects and interactions. Sci. Transl. Med. 4, 125ra131–125ra131 (2012).
Wishart, D. S. et al. DrugBank: a comprehensive resource for in silico drug discovery and exploration. Nucleic Acids Res. 34, D668–D672 (2006).
Kuhn, M., Letunic, I., Jensen, L. J. & Bork, P. The SIDER database of drugs and side effects. Nucleic Acids Res. 44, D1075–D1079 (2015).
Hamosh, A., Scott, A. F., Amberger, J. S., Bocchini, C. A. & McKusick, V. A. Online Mendelian inheritance in man (OMIM), a knowledgebase of human genes and genetic disorders. Nucleic Acids Res. 33, D514–D517 (2005).
Kim, D. H. et al. High‐throughput algorithm for discovering new drug indications by utilizing large‐scale electronic medical record data. Clin. Pharmacol. Ther. 108, 1299–1307 (2020).
Paik, H. et al. Repurpose terbutaline sulfate for amyotrophic lateral sclerosis using electronic medical records. Sci. Rep. 5, 1–8 (2015).
Challa, A. P. et al. Systematically prioritizing candidates in genome-based drug repurposing. Assay. Drug Dev. Technol. 17, 352–363 (2019).
Nordon, G., Koren, G., Shalev, V., Horvitz, E. & Radinsky, K. In Proc. AAAI Conference on Artificial Intelligence (ed. Myers, k.) 9565–9572 (AAAI Press, Palo Alto, California USA, 2019).
Pinoges, L. et al. Risk factors and mortality associated with resistance to first-line antiretroviral therapy: multicentric cross-sectional and longitudinal analyses. J. Acquir. Immune Defic. Syndr. 68, 527–535 (2015).
Wang, H., Deng, Y., Wan, L. & Huang, L. A comprehensive map of disease networks and molecular drug discoveries for glaucoma. Sci. Rep. 10, 1–13 (2020).
Ghalwash, M., Li, Y., Zhang, P. & Hu, J. In Proc. 2017 ACM on Conference on Information and Knowledge Management (eds Lim, E.-P. & Winslett, M.) 1837–1846 (Association for Computing Machinery, New York, NY, United States, 2017).
Liu, R., Wei, L. & Zhang, P. A deep learning framework for drug repurposing via emulating clinical trials on real-world patient data. Nat. Mach. Intell. 3, 68–75 (2021).
Cai, T. et al. Association of interleukin 6 receptor variant with cardiovascular disease effects of interleukin 6 receptor blocking therapy: a phenome-wide association study. JAMA Cardiol. 3, 849–857 (2018).
Xu, C. et al. Accurate drug repositioning through non-tissue-specific core signatures from cancer transcriptomes. Cell Rep. 25, 523–535. e525 (2018).
Hsieh, K. et al. Drug repurposing for COVID-19 using graph neural network and harmonizing multiple evidence. Sci. Rep. 11, 1–13 (2021).
Koren, G., Nordon, G., Radinsky, K. & Shalev, V. Identification of repurposable drugs with beneficial effects on glucose control in type 2 diabetes using machine learning. Pharmacol. Res. Perspect. 7, e00529 (2019).
Kuang, Z. et al. In Computational Methods for Drug Repurposing (ed. Vanhaelen, Q.) Ch. 15 (Springer, 2019).
Kuang, Z. et al. In IJCAI: Proceedings of the Conference. 2521 (NIH Public Access).
Kuang, Z. et al. In Proc. 22nd ACM SIGKDD International Conference on Knowledge Discovery and Data Mining (eds Krishnapuram, B. & Shah, M.) 491–500 (Association for Computing Machinery, New York, NY, United States, 2016).
Jang, D., Lee, S., Lee, J., Kim, K. & Lee, D. Inferring new drug indications using the complementarity between clinical disease signatures and drug effects. J. Biomed. Inform. 59, 248–257 (2016).
Wen, Q., Liu, R. & Zhang, P. Clinical connectivity map for drug repurposing: using laboratory results to bridge drugs and diseases. BMC Med. Inform. Decis. Mak. 21, 1–11 (2021).
Stenner, S. P. et al. ePrescribing: reducing costs through in-class therapeutic interchange. Appl. Clin. Inform. 7, 1168 (2016).
Malki, M. A., Dawed, A. Y., Hayward, C., Doney, A. & Pearson, E. R. Utilizing large electronic medical record data sets to identify novel drug–gene interactions for commonly used drugs. Clin. Pharmacol. Ther. 110, 816–825 (2021).
Bi, J. et al. Targeting glioblastoma signaling and metabolism with a re-purposed brain-penetrant drug. Cell Rep. 37, 109957 (2021).
Reznikov, L. R. et al. Identification of antiviral antihistamines for COVID-19 repurposing. Biochem. Biophys. Res. Commun. 538, 173–179 (2021).
Bejan, C. A. et al. DrugWAS: drug‐wide association studies for COVID‐19 drug repurposing. Clin. Pharmacol. Ther. 110, 1537–1546 (2021).
Muraki, S. et al. Population pharmacodynamic analysis of uric acid–lowering effects of febuxostat based on electronic medical records in two hospitals. J. Clin. Pharmacol. 58, 304–313 (2018).
Cummings, T. H., Magagnoli, J., Hardin, J. W. & Sutton, S. S. Drug repurposing of dextromethorphan as a cellular target for the management of influenza. Pharmacotherapy 41, 796–803 (2021).
Zhou, M. et al. Drug repurposing for opioid use disorders: integration of computational prediction, clinical corroboration, and mechanism of action analyses. Mol. Psychiatry 26, 5286–5296 (2021).
Ozery-Flato, M., Goldschmidt, Y., Shaham, O., Ravid, S. & Yanover, C. Framework for identifying drug repurposing candidates from observational healthcare data. JAMIA Open 3, 536–544 (2020).
Bai, L. et al. Computational drug repositioning of atorvastatin for ulcerative colitis. J. Am. Med. Inform. Assoc. 28, 2325–2335 (2021).
Gurwitz, D. Repurposing current therapeutics for treating COVID‐19: a vital role of prescription records data mining. Drug Dev. Res. 81, 777–781 (2020).
Varnai, P., Davé, A., Farla, K., Nooijen, A. & Petrosova, L. The Evidence REVEAL study: exploring the use of real‐world evidence and complex clinical trial design by the European pharmaceutical industry. Clin. Pharmacol. Ther. 110, 1180–1189 (2020).
Olson, M. Can real-world evidence save pharma US $1 billion per year? A framework for an integrated evidence generation strategy. J. Comp. Eff. Res. 9, 79–82 (2019).
Paranjpe, M. D., Taubes, A. & Sirota, M. Insights into computational drug repurposing for neurodegenerative disease. Trends Pharmacol. Sci. 40, 565–576 (2019).
Xu, J. et al. Multimodal single-cell/nucleus RNA sequencing data analysis uncovers molecular networks between disease-associated microglia and astrocytes with implications for drug repurposing in Alzheimer’s disease. Genome Res. 31, 1900–1912 (2021).
Zhou, Y. et al. A network medicine approach to investigation and population-based validation of disease manifestations and drug repurposing for COVID-19. PLoS Biol. 18, e3000970 (2020).
Fang, J. et al. Endophenotype-based in silico network medicine discovery combined with insurance record data mining identifies sildenafil as a candidate drug for Alzheimer’s disease. Nat. Aging 1, 1175–1188 (2021).
Rindflesch, T. C. et al. Investigating the role of interleukin-1 beta and glutamate in inflammatory bowel disease and epilepsy using discovery browsing. J. Biomed. Semant. 9, 1–14 (2018).
Si, Y. et al. Deep representation learning of patient data from Electronic Health Records (EHR): a systematic review. J. Biomed. Inform. 115, 103671 (2021).
Xiao, C., Choi, E. & Sun, J. Opportunities and challenges in developing deep learning models using electronic health records data: a systematic review. J. Am. Med. Inform. Assoc. 25, 1419–1428 (2018).
Xie, F. et al. Deep learning for temporal data representation in electronic health records: a systematic review of challenges and methodologies. J. Biomed. Inform. 126, 103980 (2021).
Wang, Y. et al. Clinical information extraction applications: a literature review. J. Biomed. Inform. 77, 34–49 (2018).
Kruse, C. S., Goswamy, R., Raval, Y. J. & Marawi, S. Challenges and opportunities of big data in health care: a systematic review. JMIR Med. Inform. 4, e5359 (2016).
Tiase, V. L. et al. Patient-generated health data and electronic health record integration: a scoping review. JAMIA Open 3, 619–627 (2020).
Shivade, C. et al. A review of approaches to identifying patient phenotype cohorts using electronic health records. J. Am. Med. Inform. Assoc. 21, 221–230 (2014).
Williams, R., Kontopantelis, E., Buchan, I. & Peek, N. Clinical code set engineering for reusing EHR data for research: a review. J. Biomed. Inform. 70, 1–13 (2017).
Tricco, A. C. et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann. Intern. Med. 169, 467–473 (2018).
Acknowledgements
This work was supported by grants from the National Institute of Health (NIH) NIGMS (K99GM135488). We thank Gerberi, Danielle J. from Mayo Clinic Library to provide a literature search.
Author information
Authors and Affiliations
Contributions
N.Z. conceived and designed the study. N.Z., Y.Z., S.M., S.F., L.W., M.H., Y.Y, and A.W developed the search strategy and made the inclusion decisions and the quality assessment. N.Z., Y.Z., S.M., S.F., L.W., M.H., Y.Y., A.W., and Y.W., provided methodological expertize. N.Z., Y.Z., S.M., S.F., L.W., M.H., Y.Y., and A.W. wrote the draft of the manuscript; Y.W., G.Z., M.M., J.R.C., and H.L. revised the work. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zong, N., Wen, A., Moon, S. et al. Computational drug repurposing based on electronic health records: a scoping review. npj Digit. Med. 5, 77 (2022). https://doi.org/10.1038/s41746-022-00617-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41746-022-00617-6
- Springer Nature Limited