Abstract
The serum uric acid to serum creatinine ratio (SUA/sCr) is a standardized index of renal function. More importance was attached to the significance of this ratio in the progression of hypertension. While the association between the prognosis of hypertension and SUA/sCr is unknown. Therefore, we aimed to prospectively examine the associations of serum uric acid to serum creatinine ratio and all-cause and CVD mortality in adults with hypertension. Participants with hypertension from NHANES 1999–2018 (n = 15,269) were included. They were stratified by 1 increment of SUA/sCr ratio and categorized into 6 groups as ≤ 4, > 4 to 5, > 5 to 6, > 6 to 7, > 7 to 8, and > 8. The reason for categorization in 6 groups was to analyze the influence of different ratios on outcomes accurately and provide more precise guidance. The sample size is large enough that even if divided into 6 groups, it does not affect the statistical power. The primary outcomes were all-cause and CVD mortality. Weighted multivariable Cox proportional hazards regression models were used to estimate hazard ratio (HRs) of mortality. Restricted cubic spline regression models were utilized to examine dose–response associations between the serum uric acid to serum creatinine ratio and all-cause and CVD mortality. Relatively comprehensive stratified analyses were conducted to confirm the accuracy and stability of the results. There were 15,269 total participants, 49.4% of whom were men, with an average age of 56.6 years. Weighted multivariable Cox proportional hazards regression models demonstrated participants in the lowest group (≤ 4) had the HRs (95% CIs) of 1.43 (1.18, 1.73) for all-cause mortality and 2.8 (1.92, 4.10) for CVD mortality when compared to the reference group. Participants in the highest group (> 8) had the HRs (95% CIs) of 0.47 (0.25, 0.89) for CVD mortality when compared to the reference group. There were progressively lower risks for all-cause and CVD mortality with the SUA/sCr ratio increased (both P trend < 0.01). The SUA/sCr ratio was (P for nonlinearity < 0.01) nonlinearly correlated with all-cause mortality, with inflection points of 6.25. In addition, the restricted cubic splines results indicated that the SUA/sCr ratio (P for nonlinearity = 0.32) showed linear and negative associations with cardiovascular mortality with inflection points of 6.54. The inverse associations between SUA/sCr ratio and all-cause mortality were consistent across all subgroups except for the subgroup of eGFR < 45 ml/min/1.73 m2 and never smokers (P trend = 0.20 and 0.13, respectively), and the inverse associations between low SUA/sCr ratio and CVD mortality were consistent across all subgroups (P trend < 0.01). Contrary to previous studies, outcomes suggest that lower SUA/sCr ratio was associated with higher risks of all-cause and CVD mortality in adults with hypertension.
Similar content being viewed by others
Introduction
Hypertension is one of the majorities of public health challenges around the world1. Over time, the incidence of hypertension has risen steadily. By 2025, the number of individuals with hypertension is expected to rise to 1.56 billion2. Hypertension is more likely to arise from several nutritional disorders, one of which is the excretion and metabolism of abnormal uric acid. 20% to 40% of individuals with hypertension have hyperuricemia3, whereas 25% to 50% of gout patients have a comparable incidence of hypertension4. Moreover, serum creatinine was associated with cardiovascular risk factors in adults with hypertension, and kidney-sparing therapy is essential for patients with hypertension to slow down the deterioration of kidney function and optimize control of cardiovascular risk5.
The serum uric acid to serum creatinine ratio (SUA/sCr) is a standardized index of renal function. Because the kidney is where the uric acid is mainly excreted, any abnormality in the renal function can cause a significant decrease in urate excretion with consequently increasing in serum urate levels. Hence, the plasma levels of uric acid are directly associated with serum creatinine and the negative prognostic effect described for hyperuricemia is actually an indirect effect of renal dysfunction which is a noted risk factor for cardiovascular diseases. The application of the SUA/sCr ratio to patients with hypertension as well as other categories (patients with coronary artery disease, diabetes, etc.) could significantly increase the discriminatory possibility of abnormal serum uric acid and understand a “functional biomarker” whose role cannot be correctly interpreted only by looking at his “biochemical” expression more thoroughly6. Emerging data suggest that a higher SUA to SCr ratio (SUA/sCr) is linked to a higher risk of hypertension and cardiovascular mortality7,8. More importance was attached to the significance of SUA/sCr ratio in the progression of hypertension. While the association between the prognosis of hypertension and SUA/sCr ratio is unknown. Additionally, the SUA/sCr ratio used in prior studies vary, and most of them classify individuals according to quantiles, which hamper the clinical applicability. Hence, the present research aimed to analyze the association between the SUA/sCr ratio and all-cause and CVD mortality in people with hypertension and to obtain understanding of the function of the SUA/sCr ratio in prognosis of hypertension using data from the US National Health and Nutrition Examination Survey (NHANES).
Methods
On the NHANES website, all data are accessible to the general public. (https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx). Relevant R code is accessible from the corresponding author. Details of study implementation are available for online access: https://wwwn.cdc.gov/nchs/nhanes/tutorials/module2.aspx.
Participants
The National Health and Nutritional Examination Survey (NHANES), which is conducted by the National Center for Health Statistics, collected information regarding the health and nutritional status of the US citizens every 2 years. Informed consent was provided by all participants9. A multistage, cluster‐sampling strategy is used to make sure that samples are representative, which are obtained from the nationwide United States. The primary outcomes were all-cause and CVD mortality. Eligible hypertensive participants aged > 20 years were enrolled. Participants with hypertension from NHANES 1999–2018 (n = 21,198) were included. We excluded individuals: (1) who were pregnant at baseline (n = 89), (2) who had cancer at baseline (n = 3102), (3) whose values of serum uric acid or eGFR were missing (n = 1847), (4) whose values of blood pressure were missing (n = 644), (5) who aged less than 20 or had sampling weight of zero (n = 227) and whose data on follow-up were missing (n = 20). In the end, this study contained a sizable national representative sample (n = 15,269) of general adults in the US with hypertension. Figure 1 depicts the screening procedure's flowchart.
Definition of hypertension
Per the standardized protocol, each blood pressure was calculated at 30-s intervals 3 or 4 times after resting for 5 min. Hypertension was determined by 1 or more of the following requirements: (1) self-reported physician diagnosis of hypertension; (2) ongoing antihypertensive treatment; (3) mean diastolic BP ≥ 90 mmHg, and (4) mean systolic BP ≥ 140 mmHg1.
Covariate information
Covariates that may influence the associations between SUA/sCr and all-cause and CVD mortality were included in the present study, including age, sex, race, body mass index, family income, education, smoking, drinking, physical activity, cardiovascular diseases, total cholesterol, high-density lipoprotein cholesterol, estimated glomerular filtration rate (eGFR), glycated hemoglobin (HbA1c), meat intake, fiber intake, energy intake, prescription of allopurinol, and urinary albumin to creatinine ratio (ACR). Metabolic equivalent of task (MET) was used to express the intensity level of physical activity and to indicate the rate of energy consumption for a specific activity. Physical activity was categorized as inactive group (no leisure-time physical activity), insufficiently active group (leisure-time moderate activity 1–5 times per week with MET ranging from 3 to 6 or leisure-time vigorous activity 1–3 times per week with MET > 6), or active group (those who had more leisure-time moderate-or-vigorous activity than above)10. We estimated GFR using the 4-variable Modification of Diet in Renal Disease study equation11:
Serum uric acid and serum creatinine measurement
Serum uric acid and serum creatinine were analyzed on a Beckman UniCel DxC800 Synchron by Collaborative Laboratory Services, LLC. Serum creatinine was analyzed using the Jaffe rate method. SUA was assessed using a timed endpoint method. The details of the serum creatinine measurement process and serum uric acid acquisition process are available at http://cdc.gov/nchs/nhanes.
Mortality
Using the NHANES allocated sequence number, the anonymized 1999 longitudinal Medicare and mortality data. Up until December 31, 2019, mortality follow-up statistics were accessible from the date of survey participation (http://www.cdc.gov/nchs/data-linkage/mortality-public.htm). Using the International Classification of Diseases, Tenth Revision (ICD-10) as a basis, the National Center for Health Statistics identified the underlying causes of death for participants. Mortality from all causes and cardiovascular diseases (ICD codes I00–I99) were the study's main outcomes.
Statistical analysis
The NHANES dataset was analyzed in accordance with the standards established by the Centers for Disease Control and Prevention, taking into account masked variance and employing their recommended weighting methods. To enable more excellent statistical reliability, the MEC sample weights (WTMEC2YR/7) were used for weighted analyses (https://wwwn.cdc.gov/nchs/nhanes/tutorials/default.aspx). Analysis of variance (ANOVA) and Chi-square tests, respectively, were used to compare demographic characteristics that were either continuous or categorical among SUA/sCr groups.
Firstly, to detect nonlinear associations and better delineate the effects of low SUA/sCr ratio on mortality, the study participants were stratified by 1 increment of SUA/sCr ratio and categorized into 6 groups as ≤ 4, > 4 to 5, > 5 to 6, > 6 to 7, > 7 to 8, and > 8. Participants with SUA/sCr ratio of > 6 to 7 were set as the reference group. Secondly, a weighted multivariable Cox proportional hazards regression model which was completely modified was created. The model was adjusted for age, sex, race, education, poverty to income ratio, total energy intake, BMI, physical activity, smoking, alcohol, cardiovascular diseases, fiber and meat consumption, HDL-C, TC, systolic blood pressure, diastolic blood pressure, allopurinol, ACR, eGFR, antihypertensives that may alter serum uric acid levels and serum albumin. We subsequently utilized a restricted cubic spline regression model with three knots at the 5th, 50th, and 95th percentiles of the SUA/sCr ratio, excluding the most extremely 5% amounts to decrease the possible impact of anomalies, to examine dose–response associations between the SUA/sCr ratio and all-cause and CVD mortality. Nonlinearity was tested by utilizing the probability proportion examination. Additionally, subgroup analyses based on the fully adjusted model were carried out to determine the stratified relationships between SUA/sCr and all-cause and CVD mortality. For most of the covariates, < 5.0% of the data were missing. While there was a lack of data in 20.6% of the study participants for drinking status, and 9.6% for poverty income ratio. Multiple imputation was performed to minimize sample size reduction due to missing covariates. Furthermore, we excluded participants who died within the first 2 years during follow-up to minimize the reverse-causality bias.
Ethical approval
This research was conducted in accordance with the guidelines outlined in the Declaration of Helsinki. Approval for the study was obtained from the Ethics Committee at the National Center for Health Statistics. Written informed consent was provided by all patients/participants prior to their involvement in this study.
Results
There were 15,269 total participants, 49.4% of whom were men, with an average age of 56.6 years. The median (interquartile range) of SUA/sCr was 6.28 (5.22, 7.56). The maximum was 38.5 and the minimum was 0.34. For the female, the median (interquartile range) of SUA/sCr was 6.50 (5.33, 7.83). The maximum was 20.0 and the minimum was 0.43. For the male, the median (interquartile range) of SUA/sCr was 6.09 (5.09, 7.29). The maximum was 38.5 and the minimum was 0.34. For the elderly (age > 60), the median (interquartile range) of SUA/sCr was 6.00 (5.00, 7.24). The maximum was 20.6 and the minimum was 0.40. For the others (age ≤ 60), the median (interquartile range) of SUA/sCr was 6.60 (5.44, 7.88). The maximum was 38.5 and the minimum was 0.34. Table 1 displays the participant's demographic information stratified by the SUA/sCr ratio. Compared with the reference group (SUA/sCr: > 6 to 7), participants with lower SUA/sCr were older, had lower percentage of college education, higher blood pressure, and higher baseline eGFR. Furthermore, the low SUA/sCr ratio (≤ 4) group had more risks for all-cause and CVD mortality. Per the census date (December 31, 2019), 3664 (22.1%) adults with hypertension died of all‐cause mortality and 1084 (6.5%) of cardiovascular mortality at a median follow-up duration of 95 months.
Associations between the SUA/sCr ratio and all-cause and cardiovascular mortality
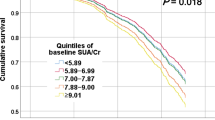
Table 2 displays the outcomes from the multivariable Cox regression model for risk of all-cause and CVD mortality across stratified SUA/sCr ratio. Participants in the lowest group (≤ 4) had the HRs (95% CIs) of 1.43 (1.18, 1.73) for all-cause mortality and 2.8 (1.92, 4.10) for CVD mortality when compared to the reference group. Participants in the highest group (> 8) had the HRs (95% CIs) of 0.47 (0.25, 0.89) for CVD mortality when compared to the reference group. There were progressively lower risks for CVD mortality with the SUA/sCr ratio increased (P trend < 0.01). Analyses showed that the SUA/sCr ratio was (P for nonlinearity < 0.01) nonlinearly correlated with all-cause mortality, with inflection points of 6.25 (Fig. 2).
Association between SUA/sCr ratio and all-cause mortality among patients with hypertension in NHANES 1999–2018. HRs were adjusted for age, sex, race, education, poverty to income ratio, total energy intake, BMI, physical activity, smoking, alcohol, cardiovascular diseases, fiber and meat consumption, HDL-C, TC, systolic blood pressure, diastolic blood pressure, allopurinol, ACR, eGFR, antihypertensives that may alter serum uric acid levels and serum albumin.
In addition, the restricted cubic splines results indicated that the SUA/sCr ratio (P for nonlinearity = 0.32) showed linear and negative associations with cardiovascular mortality with inflection points of 6.54 (Fig. 3).
Association between SUA/sCr ratio and cardiovascular mortality among patients with hypertension in NHANES 1999–2018. HRs were adjusted for age, sex, race, education, poverty to income ratio, total energy intake, BMI, physical activity, smoking, alcohol, cardiovascular diseases, fiber and meat consumption, HDL-C, TC, systolic blood pressure, diastolic blood pressure, allopurinol, ACR, eGFR, antihypertensives that may alter serum uric acid levels and serum albumin.
Stratified associations between SUA/sCr ratio with all-cause and CVD mortality
Based on the fully adjusted model, as shown in Tables 3 and 4, we further examined the relationships between SUA/sCr and all-cause and CVD mortality in a particular subgroup by age, sex, smoking, eGFR, BMI and serum uric acid. The inverse associations between low SUA/sCr ratio and all-cause mortality were consistent across all subgroups except for the subgroup of eGFR < 45 ml/min/1.73 m2 and never smokers, and the inverse associations between low SUA/sCr ratio and CVD mortality were consistent across all subgroups (P trend < 0.01).
Sensitivity analyses
In sensitivity analyses, the negative association of SUA/sCr ratio with the risk of all‐cause and cardiovascular mortality in the adjusted full model was unchanged if participants with hypertension who died during the first 2 years of follow‐up were excluded (Table S1). Participants in the lowest group (≤ 4) had the HRs (95% CIs) of 1.43 (1.18, 1.74) for all-cause mortality and 2.68 (1.77, 4.07) for CVD mortality when compared to the reference group. Participants in the highest group (> 8) had the HRs (95% CIs) of 0.50 (0.17, 0.87) for CVD mortality when compared to the reference group.
Discussion
According to our knowledge, this is the first research that used the NHANES 1999–2018 data to analyze associations between SUA/sCr and all-cause and CVD mortality in a significant, national representative population of US individuals affected by hypertension. The current investigation discovered that higher SUA/sCr ratio was associated with lower risks of all-cause and CVD mortality in adults with hypertension.
Uric acid, which is abundantly present in the epithelium liquid of the human respiratory tract, serves as a crucial primary protection versus reactive oxygen species12,13. According to some evidence, the rise in SUA levels brought on by the decline in urate oxidase function may serve as a barrier to prevent damage from oxidation14. The latest study has found exposure to Arsenic (only in men) and cadmium may increase the level of UA, which indicates that increased SUA is thought to be a biomarker of oxidative stress and the activation of inflammatory cytokines15. In multivariate analysis, they also found urinary Pb was inversely associated with SUA/sCr ratio. This may partly explain the results of this study. A longitudinal investigation involving 375,163 South Korean men and women who underwent medical exams from 2002 to 2012 found a association between low SUA concentrations and increased risks of all-cause, CVD, and cancer death16. Additionally, an extensive Taiwanese population study revealed that SUA levels below 4 mg/dL were associated with increased mortality in elderly people17. Furthermore, the study also found malnourishment participated in low SUA-associated higher mortality.
External and internal purines are metabolically converted to SUA, which is the ultimate result18. Alcohol consumption, tobacco use, elevated BMI, lipid disorders, and HTN have all been linked to hyperuricemia19,20,21,22. So, when evaluating the relationship between SUA/sCr and all-cause and CVD mortality, we should carefully evaluate these parameters. Greater systolic and diastolic blood pressure values were associated with higher SUA/sCr ratio in the Chinese population8. While inconsistent with that, individuals in the present study with low SUA/sCr ratio had higher systolic and diastolic blood pressure values than other groups in the US population. The difference may be explained as follows: in that study, Chinese subjects with metabolic healthy phenotype were included. While in the present study, individuals with hypertension were included. In the Chinese study, subjects were assigned based on the quartile of SUA/sCr ratio. While in the present study, a more even stratified strategy of SUA/sCr ratio was employed.
Our outcomes conflict with those from two Chinese studies and one Us study. The large cross-sectional US research found that a higher blood uric acid to serum creatinine ratio might foresee the risk of overall and cause-specific mortality. The study also used NHANES data from 1999 to 201022. Although elevated blood pressure was a variable in the study, accuracy and stability of this association in hypertension subgroup analysis were not taken into consideration. Additionally, two other Chinese investigations revealed that increased SUA/sCr was linked to unfavorable outcomes in both pregnant women and elderly hemodialysis patients23,24. A study with 332 adult Saudi with T2DM found that a higher SUA/sCr correlated strongly with an increased risk in the prevalence of Mets and its components. They also reported that OR for central obesity, hypertriglyceridemia, low HDL-C and HTN was 2.61, 1.42, 1.45 and 1.16, respectively for those in the highest compared with the lowest SUA/Cr tertile25. While these studies had important limitations worth mentioning, including the retrospective study design and limited sample sizes. In the present study, we conducted relatively comprehensive stratified analysis to confirm the accuracy and stability of the results. Correspondingly, the results of the present study were accurate and stable.
Limitations
However, there are some limitations that must be considered when comprehending our outcomes. Firstly, because our study uses the NHANES database, we are unable to determine causation. In order to confirm the causality, larger-scale cohort studies remain required. Secondly, even though we have made numerous confounding factors adjustments, there are still additional potentially confounding factors that are not taken into account. Last but not least, because our research is based on the NHANES database, its generalizability is limited to the American population. The connection between SUA/sCr and all-cause and CVD mortality will need to be studied in greater detail in the future.
Conclusion
In this nation-based adults with hypertension, the present study showed that the low SUA/sCr ratio (≤ 4) was significantly associated with higher all-cause and CVD mortality in participants with hypertension. Contrary to previous studies, the high SUA/sCr ratio (> 8) was associated with the lowest all-cause and CVD mortality in such people. Further studies are required to investigate the mechanism involved.
Data availability
The data that support the outcomes of this study are openly available in https://www.cdc.gov/nchs/nhanes/.
References
Unger, T. et al. 2020 International Society of Hypertension global hypertension practice guidelines. J. Hypertens. 38(6), 982–1004 (2020).
Kearney, P. M. et al. Global burden of hypertension: Analysis of worldwide data. Lancet. 365(9455), 217–223 (2005).
Lin, C. S. et al. Prevalence of hyperuricemia and its association with antihypertensive treatment in hypertensive patients in Taiwan. Int. J. Cardiol. 156(1), 41–46 (2012).
Zhu, Y., Pandya, B. J. & Choi, H. K. Comorbidities of gout and hyperuricemia in the US general population: NHANES 2007–2008. Am. J. Med. 125(7), 679-687.e1 (2012).
Chen, X. et al. Serum creatinine levels, traditional cardiovascular risk factors and 10-year cardiovascular risk in Chinese patients with hypertension. Front. Endocrinol. 16(14), 1140093 (2023).
Borghi, C. & Piani, F. Uric acid and estimate of renal function. Let’s stick together. Int. J. Cardiol. 1(310), 157–158 (2020).
Casiglia, E. et al. Serum uric acid/serum creatinine ratio as a predictor of cardiovascular events. Detection of prognostic cardiovascular cut-off values. J. Hypertens. 41(1), 180–186 (2023).
Zhao, L. & Qiu, X. Higher ratio of serum uric acid to serum creatinine (SUA/sCr) increases the risk of metabolic unhealthy phenotype. Nutr. Metab. Cardiovasc. Dis. 33(10), 1981–1988 (2023).
World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA. 310(20), 2191–2194 (2013).
Beddhu, S., Baird, B. C., Zitterkoph, J., Neilson, J. & Greene, T. Physical activity and mortality in chronic kidney disease (NHANES III). Clin. J. Am. Soc. Nephrol. 4(12), 1901–1906 (2009).
Manjunath, G., Sarnak, M. J. & Levey, A. S. Prediction equations to estimate glomerular filtration rate: An update. Curr. Opin. Nephrol. Hypertens. 10(6), 785–792 (2001).
van der Vliet, A. et al. Determination of low-molecular-mass antioxidant concentrations in human respiratory tract lining fluids. Am. J. Physiol. 276(2), L289–L296 (1999).
Housley, D. G., Mudway, I., Kelly, F. J., Eccles, R. & Richards, R. J. Depletion of urate in human nasal lavage following in vitro ozone exposure. Int. J. Biochem. Cell Biol. 27(11), 1153–1159 (1995).
Guo, M. et al. The protective role of serum uric acid against premature membrane rupture in gestational diabetes: A cross-sectional study. BMC Endocr. Disord. 21(1), 95 (2021).
Gao, W. et al. Exposure to cadmium, lead, mercury, and arsenic and uric acid levels: Results from NHANES 2007–2016. Biol. Trace Elem. Res. 201(4), 1659–1669 (2023).
Cho, S. K., Chang, Y., Kim, I. & Ryu, S. U-shaped association between serum uric acid level and risk of mortality: A cohort study. Arthritis Rheumatol. 70(7), 1122–1132 (2018).
Tseng, W. C., Chen, Y. T., Ou, S. M., Shih, C. J. & Tarng, D. C. U-shaped association between serum uric acid levels with cardiovascular and all-cause mortality in the elderly: The role of malnourishment. J. Am. Heart Assoc. 7(4), e007523 (2018).
Kang, D. H. & Ha, S. K. Uric acid puzzle: Dual role as anti-oxidantand pro-oxidant. Electrolyte Blood Press. 12(1), 1–6. https://doi.org/10.5049/EBP.2014.12.1.1 (2014) (Epub 2014 Jun 30).
Rathmann, W., Haastert, B., Icks, A., Giani, G. & Roseman, J. M. Ten-year change in serum uric acid and its relation to changes in other metabolic risk factors in young black and white adults: The CARDIA study. Eur. J. Epidemiol. 22(7), 439–445 (2007).
Kutzing, M. K. & Firestein, B. L. Altered uric acid levels and disease states. J. Pharmacol. Exp. Ther. 324(1), 1–7 (2008).
Conen, D. et al. Prevalence of hyperuricemia and relation of serum uric acid with cardiovascular risk factors in a developing country. BMC Public Health. 25(4), 9 (2004).
Mazidi, M., Katsiki, N. & Banach, M. Α higher ratio of serum uric acid to serum creatinine could predict the risk of total and cause specific mortality—insight from a US national survey. Int. J. Cardiol. 1(326), 189–193 (2021).
Piani, F. et al. Serum uric acid to creatinine ratio and risk of preeclampsia and adverse pregnancy outcomes. J. Hypertens. 41(8), 1333–1338 (2023).
Ding, Z., Fan, Y., Yao, C. & Gu, L. The association between the serum uric acid to creatinine ratio and all-cause mortality in elderly hemodialysis patients. BMC Nephrol. 23(1), 177 (2022).
Al-Daghri, N. M., Al-Attas, O. S., Wani, K., Sabico, S. & Alokail, M. S. Serum uric acid to creatinine ratio and risk of metabolic syndrome in saudi type 2 diabetic patients. Sci. Rep. 7(1), 12104 (2017).
Funding
This work was supported by the National Natural Science Foundation of China (82000305, 82070483), and Jiangsu Province Capability Improvement Project through Science, Technology and Education (ZDXK202230).
Author information
Authors and Affiliations
Contributions
Zhiwei Tang developed the essence of the text, and participated in all phases of the manuscript creation. Hong Liu, Yi Ding and Chunze Yuan performed additional literature searches. Yongfeng Shao guided the dissection procedure, discussed the results, and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tang, Z., Liu, H., Ding, Y. et al. Association between serum uric acid to serum creatinine ratio with cardiovascular and all-cause mortality in adults with hypertension. Sci Rep 14, 18008 (2024). https://doi.org/10.1038/s41598-024-69057-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-69057-4
- Springer Nature Limited