Abstract
Although the efficacy of mechanical thrombectomy (MT) for acute basilar artery occlusion (ABAO) has been established in two randomized controlled studies, many patients have miserable clinical outcomes after MT for ABAO. Predicting severe disability prior to the procedure might be useful in determining the appropriateness of treatment interventions. Among the ABAO cases treated at 10 hospitals between July 2014 and December 2021, 144 were included in the study, all of whom underwent MRI before treatment. A miserable outcome was defined as a modified Rankin Scale (mRS) of 5–6 at 3 months. The associations between clinical, imaging, and procedural factors and miserable outcomes were evaluated. A miserable outcome was observed in 54 cases (37.5%). Multivariate analysis identified the National Institutes of Health Stroke Scale (NIHSS), transverse diameter of brainstem infarction, and symptomatic intracerebral hemorrhage as independent factors associated with miserable outcomes, with cutoff values of NIHSS 22 and transverse diameter of brainstem infarction 15 mm. Cases with a higher preoperative severity may result in miserable postoperative outcomes. Particularly, the transverse diameter of a brainstem infarction can be easily measured and serves as a useful criterion for determining treatment indications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Acute basilar artery occlusion (ABAO) represents the most devastating type of ischemic stroke, which is associated with a > 90% mortality rate and high level of dependency among survivors if mechanical thrombectomy (MT) is not performed1. Recently, the efficacy of MT for ABAO has been established in two randomized controlled studies, compared with receiving standard medical therapy only2,3. However, in clinical settings, many patients have miserable clinical outcomes after MT for ABAO. One of the reasons for this miserable outcome is pretreatment brainstem infarction. The brainstem is an important pathway of the brain, cerebellum, and spinal cord; therefore, even small infarctions can lead to very serious clinical consequences4. Given that those pathways pass longitudinally the transverse, rather than the anteroposterior, diameter of the brainstem infarction should contribute to the clinical outcome. However, no reports have investigated the importance of the transverse diameter of brainstem infarction for miserable outcomes after MT for ABAO. Therefore, we conducted a multicenter hospital-based surveillance at 10 hospitals in Chiba Prefecture, Japan, to validate the prognostic value of the transverse diameter of brainstem infarction in patients with ABAO treated with MT.
Results
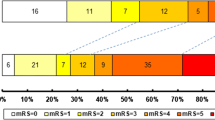
During the study period, MT was performed in 188 patients who presented with ABAO in the 10 participating hospitals. Of these, 34, 5, and 5 patients were excluded because no MR imaging was available, their mRS before MT was ≥ 4, and their mRS was unknown at 3 months, respectively. Thus, the final total was 144 patients (108 men, 36 women; mean age 73.0 ± 12.5 years) with 3 months of available functional outcomes were enrolled. Twenty-three patients (16.0%) were in a vegetative state and 31 (21.5%) were deceased. Based on these results, 54 (37.5%) patients were assigned to the miserable outcome group (Fig. 1). The detailed baseline and clinical characteristics and MR imaging characteristics according to clinical outcome are shown in Table 1.
Clinical outcomes
Detailed procedural results are shown in Table 2. RtPA was injected intravenously in 34 patients (23.6%). The mean time from symptom onset to MT was 358 min, the mean procedure time was 61 min, and the mean time to recanalization was 420 min. Fifty (34.7%) patients were treated with a combination of the aspiration device and stent retriever techniques. Successful recanalization was achieved in 134 (93.1%) patients. Eight (5.6%) patients had symptomatic ICH.
Prognostic factors
As shown in Tables 1 and 2, the univariate analyses revealed significant differences in the preoperative NIHSS score (30.9 ± 9.1 vs. 19.2 ± 10.0, p < 0.001), pc-ASPECTS (5.8 ± 2.3 vs. 7.3 ± 1.9, p < 0.001), BSS (3.0 ± 2.3 vs. 1.5 ± 1.6, p < 0.001), PMT score (4.6 ± 3.4 vs. 2.2 ± 2.2, p < 0.001), transverse diameter of brainstem infarction (14.5 ± 9.8 mm vs. 6.3 ± 6.2 mm, p < 0.001), successful recanalization (88.9% vs. 95.6%, p = 0.024), and symptomatic ICH (11.1% vs. 2.2%, p = 0.026) between the miserable outcome and control groups. In multivariate analysis, preoperative NIHSS score (odds ratio [OR] 1.08; 95% confidence interval [CI] 1.03–1.14; p = 0.001), transverse diameter of brainstem infarction (OR 1.11; 95% CI 1.00–1.23; p = 0.041), and symptomatic ICH (OR 19.0; 95% CI 2.6–139.8; p = 0.020) were independent predictors of poor outcome at 3 months. The threshold determined by the ROC curve for predicting miserable outcomes using preoperative NIHSS and transverse diameter of brainstem infarction were 24 or higher (with an AUC of 0.818), and 15 mm or higher (with an AUC of 0.789), respectively (Table 3).
Discussion
The results of this study revealed that despite thrombectomy for ABAO, 37.5% of cases experienced a miserable outcome. Predictive factors for miserable outcomes included the transverse diameter of brainstem infarction in addition to pre-treatment NIHSS and symptomatic ICH. This finding is considered novel.
Several studies have reported a significant correlation between MRI and DWI sequences and clinical outcomes in patients with posterior-circulation stroke5,6,7. Most popular score is pc-ASPECTS on DWI, which was established by Puetz et al.5 Pc-ASPECTS is a 10-point scoring system, 1 point was subtracted in each side cerebellum, posterior cerebral artery territory, or thalamus, and 2 points were subtracted in each midbrain and pons. Although this score had been used for predicting clinical outcome after MT to ABAO, that usefulness is controversial8. Yang et al. reported that a pc-ASPECTS score ≥ 6 did not predict favorable outcome9. In contrast, Yoon et al. reported that pc-ASPECTS was an independent predictor of clinical outcome of ABAO10. Mourand et al. reported that the BSS was an independent predictor of clinical outcome after mechanical thrombectomy for BAO, which is a semiquantitative DWI score (12-point system) of the brain stem, whereas pc-ASPECTS score≧7 was not statistically relevant for predicting good outcome6. Furthermore, the Liu et al. proposed the PMT score for predicting clinical outcome after MT to ABAO7. They emphasized the pretreatment DWI based PMT score showed better prognostic value for clinical outcome than pc-ASPECTS and BSS. It is understandable that the PMT score can be a valuable predictor of miserable outcomes compared to the pc-ASPECTS and BSS, owing to meticulous evaluation of high signal areas and scoring them in great detail. However, due to its detailed assessment, it poses challenges such as complexity and susceptibility to inter-rater differences. In this study, multivariate analysis revealed that the PMT score was not an independent predictor for miserable outcomes. This could be attributed to the difficulty in measurements affecting the results. Considering the necessity for swift determination of treatment indications in clinical settings, it is imperative to develop more simplified measurement techniques.
Measuring the transverse diameter of brainstem infarction may help identify patients who could benefit from recanalization therapy. As the measurement method is remarkably simple, it is possible to measure the transverse diameter of brainstem infarction in an emergency.
The reason that the transverse diameter of brainstem infarction is an independent predictor of a miserable outcome might be considered as follows. Numerous neural tracts ascend or descend through the brainstem, such as the pyramidal tract and ascending pathway11. Therefore, if ischemic stroke occurs with a long axis in the anteroposterior direction, it affects a limited number of tracts. However, when a stroke extends along the left–right axis, it can impact various tracts, suggesting that the transverse diameter of infarction in the brainstem becomes a determinant factor in clinical outcome. Given the results of the present study, the treatment indication of MT for ABAO should be considered carefully for patients whose transverse diameter of brainstem infarction is 15 mm or longer.
This study has some limitations. First, as the study was multicentric, patient selection and treatment procedures were not standardized. Second, the study design was retrospective and observational, and no control group received the best medical treatment. Third, the imaging scoring and evaluation of the mRS at 3 months were performed in each hospital. Fourth, we measured the transverse diameter of the brainstem regardless of the region affected. Naturally, this presented a problem since the affected areas differ regionally. Specifically, there was an issue in that the symptoms varied between cases where the sensory fibers were predominantly affected and those where the corticospinal tract was predominantly affected. Lastly, the sample size was small, and a larger cohort might provide better statistical power for accurate analysis.
Conclusions
In this multicenter retrospective study, 37.5% of patients with ABAO experienced miserable outcomes after MT, whereas successful recanalization was achieved in 93.1% of patients. Our findings show that the transverse diameter of brainstem infarction is useful in predicting miserable outcomes for ABAO treated with mechanical thrombectomy and may simplify the decision-making algorithm. Further studies with a larger number of cases are required.
Methods
Patients
This was a retrospective multicenter study of patients with ABAO who underwent magnetic resonance imaging (MRI) before MT in multiple hospitals in Chiba Prefecture. All study protocols were approved by the Institutional Review Board (IRB) of the Chiba University Graduate School of Medicine (approval no. M10386). A total of 10 neurosurgical centers participated in this retrospective study, and the IRBs of all 10 participating centers approved the study protocol. Given that the design of this study was noninvasive and retrospective, the requirement for informed written consent from included patients was waived.
We evaluated the data from patients who presented with ABAO and were treated with mechanical thrombectomy at all 10 hospitals between July 2014 and June 2022. The indications for mechanical thrombectomy for acute basilar artery occlusion were: (1) acute occlusion of the basilar artery confirmed by magnetic resonance (MR) angiography and (2) a National Institute of Health Stroke Scale (NIHSS) score of ≥ 6. Other indications were dependent on each hospital. The exclusion criteria were as follows: (1) MR imaging was not performed before MT (2) modified Rankin Scale (mRS) before MT was ≥ 4; (3) loss to follow-up.
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki. Our study was approved with a waiver of the requirement for informed consent by Research ethics committee of the graduate school of medicine, Chiba university.
Mechanical thrombectomy
Each center could decide on the strategy for revascularization and select the devices deemed most appropriate for treatment. During the study period, the usable stent retrievers were second-generation stents, such as Solitaire (Covidien, Irvine, CA) or Trevo (Stryker, Fremont, CA). The usable aspiration devices were the Penumbra System (Penumbra, Oakland, CA), Sofia System (Microvention, Aliso Viejo, CA), React System (Covidien), and Catalyst System (Stryker).
Endpoint
The primary outcome of the present study was a miserable outcome at 3 months. The functional outcome was evaluated using the modified Rankin Scale (mRS) 3 months after treatment. A miserable outcome was defined as an mRS score of 5 or 6. Furthermore, factors associated with miserable outcomes were analyzed for background characteristics, MR imaging characteristics, and treatments. Univariate analyses were performed using a control group of patients with an mRS score of ≤ 4. Background characteristics were patient age, sex, past history, NIHSS score on admission, and stroke type. MR imaging characteristics were posterior circulation Acute Stroke Prognosis Early CT score (pc-ASPECTS 5, brain stem score (BSS) 6, Pons-Midbrain and Thalamus (PMT) score 7, and transverse diameter of brainstem infarction. The transverse diameter of the brainstem infarction was measured using Synapse version 3.2.0 (FUJIFILM Medical System USA's Synapse PACS System, USA). The infarct area was defined as the high-intensity area on diffusion-weighted imaging (DWI). Representative cases for measuring the transverse diameter of brainstem infarctions are shown in Fig. 2. Treatments were the use of recombinant tissue plasminogen activator (rtPA), types of revascularization devices used, number of passes required, modified Thrombolysis In Cerebral Infarction (mTICI) grade time from onset to recanalization (OTR), and a symptomatic intracerebral hemorrhage (ICH), which was defined as any ICH that caused neurological deterioration with an increase of ≥ 4 on the NIHSS12. Successful revascularization was defined as a mTICI grade of 2b or 313.
(A) Prethrombectomy diffusion weighted imaging (DWI) of a 72-year-old man with tetraplegia in a coma. Dashed line showed transverse diameter of brainstem infarction. That length was 25 mm. The modified Rankin Scale was 5 at 3 months after mechanical thrombectomy. (B) Prethrombectomy DWI of an 81-year-old woman with right hemiplegia. Dashed line showed transverse diameter of brainstem infarction. That length was 7 mm. The modified Rankin Scale was 2 at 3 months after mechanical thrombectomy.
Statistical analysis
Statistical evaluations were performed using JMP 16.1.0 (SAS Institute Inc., NC, USA). For univariate analyses, data were compared using the Student’s t-test for continuous variables or chi-squared tests for categorical variables. To determine the predictors of a miserable clinical outcome, a forward, stepwise logistic regression analysis that included all variables with a p value of < 0.2 in the univariate analyses was performed. Statistical significance was set at p < 0.05. Receiver Operating Characteristic (ROC) curves were used to determine the threshold for predicting miserable outcomes.
Data availability
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
References
Brandt, T., von Kummer, R., Müller-Küppers, M. & Hacke, W. Thrombolytic therapy of acute basilar artery occlusion. Variables affecting recanalization and outcome. Stroke 27, 875–881 (1996).
Tao, C. et al. Trial of endovascular treatment of acute basilar-artery occlusion. N. Engl. J. Med. 387, 1361–1372 (2022).
Jovin, T. G. et al. N. Engl. J. Med. 387, 1373–1384 (2022).
Tajima, Y., Hayasaka, M., Ebihara, K., Yokoyama, D. & Suda, I. Predictors of very poor outcome after mechanical thrombectomy for acute basilar artery occlusion. Neurol. Med. Chir. (Tokyo) 60, 507–513 (2020).
Puetz, V. et al. Extent of hypoattenuation on CT angiography source images predicts functional outcome in patients with basilar artery occlusion. Stroke. 39, 2485–2490 (2008).
Mourand, I. et al. A predictor of outcome in acute basilar artery occlusion treated with the solitaire FR device. AJNR Am. J. Neuroradiol. 35, 1117–1123 (2014).
Liu, L. et al. Novel diffusion-weighted imaging score showed good prognostic value for acute basilar artery occlusion following endovascular treatment. The pons-midbrain and thalamus score. Stroke. 52, 3989–3997 (2021).
Tei, H., Uchiyama, S., Usui, T. & Ohara, K. Posterior circulation ASPECTS on diffusion-weighted MRI can be a powerful marker for predicting functional outcome. J. Neurol. 257, 767–773 (2010).
Yang, H. et al. Early diffusion-weighted imaging brain stem score for acute basilar artery occlusion treated with mechanical thrombectomy. J. Stroke Cerebrovasc. Dis. 27, 2822–2828 (2018).
Yoon, W. et al. Predictors of good outcome after stent-retriever thrombectomy in acute basilar artery occlusion. Stroke. 46, 2972–2975 (2015).
Shah, A., Jhawar, S. S., Nunez, M., Goel, A. & Goel, A. Brainstem anatomy: A study on the basis of the pattern of fiber organization. World Neurosurg. 134, e826–e846 (2020).
Trouillas, P. & von Kummer, R. Classification and pathogenesis of cerebral hemorrhages after thrombolysis in ischemic stroke. Stroke. 37, 556–561 (2016).
Kass-Hout, T. et al. Clinical, angiographic and radiographic outcome differences among mechanical thrombectomy devices: Initial experience of a large-volume center. J. Neurointerv. Surg. 7, 176–181 (2015).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conceptualization of this study. Data curation and formal analysis were performed by all authors. Y.T. wrote the original draft of the manuscript. All authors reviewed and edited the earlier versions of the manuscript. All the authors have read and approved the final version of the manuscript submitted for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tajima, Y., Yoshida, Y., Kubota, M. et al. Transverse diameter of brainstem infarction is a strong predictor of miserable outcome after mechanical thrombectomy for acute basilar artery occlusion. Sci Rep 14, 18201 (2024). https://doi.org/10.1038/s41598-024-68865-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-68865-y
- Springer Nature Limited