Abstract
Cardiometabolic risk factors increase the chance of developing cardiovascular disease (CVD) and type 2 diabetes. Most CVD risk factors are influenced by total and regional obesity. A higher risk of developing CVD may be linked to vitamin D deficiency, which is more prevalent in the older population. With the goal of evaluating the association between vitamin D and cardiometabolic risk factors and total and regional obesity in older adults, this research included 25 (OH) vitamin D3 concentrations and biochemical markers associated with cardiometabolic diseases, as well as total and regional adiposity, which was measured by DXA. A total of 1991 older participants in the PoCOsteo study were included. Overall, 38.5% of participants had vitamin D deficiency. After adjusting for confounders, the results of multiple linear and logistic regression suggested an inverse association between vitamin D and body mass index (P = 0.04), waist circumference (P = 0.001), total fat (P = 0.02), android fat (P = 0.001), visceral fat (P < 0.001), subcutaneous fat (P = 0.01), trunk fat (P = 0.006), arm fat (P = 0.03), high systolic blood pressure (P = 0.004), high total cholesterol (P < 0.001), high LDL-cholesterol (P < 0.001), high serum triglycerides (P = 0.001), and high fasting glucose (P < 0.001). Additionally, higher vitamin D concentrations decreased the risk of dyslipidemia by 2%. Our results showed a significant association between serum vitamin D and a number of cardiometabolic risk factors, including total and regional obesity.
Similar content being viewed by others
Introduction
Based on the American Heart Association definition, risk factors for developing cardiovascular disease (CVD) and type 2 diabetes are termed cardiometabolic risk factors1. Among the wide range of these factors, age, gender, smoking, hyperglycemia, high blood pressure, dyslipidemia, inflammation, insulin resistance, psychosocial stress, insufficient vegetable consumption, inactivity, and obesity can be mentioned2,3,4. Therefore, the fact that obesity independently raises the risk for almost all CVD risk factors, including dyslipidemia, hypertension, metabolic syndrome, abnormal glucose concentrations, inflammation, and type 2 diabetes mellitus, is evident5,6. CVD continues to be a key reason for early deaths and disabilities, which increases the cost of healthcare. The number of those who experienced CVD almost doubled from 1990 to 20197.
Vitamin D, produced in the skin when exposed to sunlight or consumed through diet, is necessary to keep the serum concentration of calcium in the normal physiological range for the health of muscles and bones8. In addition to osteoporosis prevention, vitamin D may help prevent cardiometabolic risk factors such as obesity and type 2 diabetes9,10,11,12,13,14. This positive metabolic effect of vitamin D has been detected in almost all noncommunicable diseases (NCDs), which are responsible for more than 70% of mortality worldwide and 90% in industrialized countries such as the USA or Germany. A large number of scientific papers in the last 20 years have shown this extraordinary positive feature of vitamin D. This is due to the fact that vitamin D, although it is found in small amounts in food, is also a hormone whose precursor is produced abundantly by our skin when it is properly exposed to the sun. The receptors for vitamin D are detected in the cells of almost all tissues of the body15. Up to 1 billion people worldwide are estimated to have subclinical deficiency of vitamin D. Obese patients and older adults have a higher incidence of vitamin D deficiency16. In Iran, 67% of the older population has vitamin D deficiency, compared to 61% of older Americans17. In the older population, some research also indicates that low serum vitamin D concentrations are an independent risk factor for developing cardiometabolic diseases18,19,20,21. However, the cardiometabolic effect of vitamin D is inconsistent. Several recent studies have shown that vitamin D supplementation did not reduce the prevalence of cardiometabolic diseases22,23,24. Furthermore, some studies revealed that high serum concentrations of vitamin D only had an inverse association with fasting glucose or regional adiposity but were not related to other cardiometabolic risk factors25,26.
Additionally, obesity is often measured using body mass index (BMI), but BMI has poor predictive ability for determining the exact body fat distribution and content27. Those with high body fat percentages, even those with normal BMIs, have an elevated chance of developing cardiometabolic diseases28. Moreover, individuals with excess visceral adipose tissue are more likely to have insulin resistance and metabolic diseases than those with extra subcutaneous adipose tissue29. However, dual-energy X-ray absorptiometry (DXA) can easily detect total and regional adiposity30.
Furthermore, previous research indicates that the population of Bushehr has a high prevalence of vitamin D deficiency and chronic diseases, including cardiovascular diseases31,32. Therefore, the present study was conducted in the older population of southern Iran with the aim of investigating the relationship between the 25 hydroxyvitamin D serum concentration and cardiometabolic risk factors and total and regional adiposity, assessed by DXA, based on the PoCOsteo study.
Method
Study population
This cross-sectional research was conducted using the findings of the PoCOsteo study. The PoCOsteo study was a prospective cohort investigation performed in Iran and Austria with the major goal of creating a multimodal model for assessing the risk of fracture. Two separate study centers, the Medical University of Graz and the Endocrinology and Metabolism Research Institute (EMRI) at Tehran University of Medical Sciences (TUMS), were independently recruited to gather data from derivation cohorts. These cohorts were established to identify potential differences specific to certain populations. From the start of spring 2018, data were collected for each center using a cohort approach. The subjects were followed up for at least three years or until the end of the project in autumn 2021. The PoCOsteo study serves as an extension to the second stage of BEH, and its primary focus was on musculoskeletal diseases. BEH was a prospective cohort study conducted by the EMRI of TUMS and the Persian Gulf Marine Biotechnology Research Centre (PGTMRC). The study aimed to investigate the prevalence of noncommunicable diseases (NCDs) among the elderly population33. In the Iranian part of the study, the older population who had lived in Bushehr for at least a year prior to being recruited, had no intention of leaving the city for the ensuing 5 years, and had adequate mental and physical health for participating in the research were enrolled as the study sample. By using random cluster sampling, a total of 1991 people aged 48 and over were selected from 75 Bushehr neighborhoods. The detailed protocol and methodology of the PoCOsteo study are described elsewhere34.
Data collection
Dual X-ray absorptiometry (DXA Discovery WI, Hologic, Bedford, Virginia, USA) was applied to measure body fat composition, including total fat, android fat, visceral adipose tissue (VAT), subcutaneous adipose tissue (SAT), gynoid fat, trunk fat, leg fat, and arm fat.
Information on age, gender, medical history, education level, occupation, income, marital status, tobacco smoking (cigarettes or water pipes), medication use, and vitamin D supplementation was gathered through a comprehensive, valid questionnaire that was privately administered by a qualified interviewer. In addition, the level of physical activity was evaluated by a standardized questionnaire using metabolic equivalent (MET) levels35,36. To gather data on blood pressure and anthropometric measures, the subjects underwent a physical examination. After 15 min of rest, the systolic and diastolic blood pressure of the participants was obtained by calculating the average of two measurements on the right arm in a sitting position with a 10-min interval. BMI was calculated by dividing weight in kilograms by squared height in meters squared. The height and weight of individuals were measured via a fixed stadiometer and a digital scale after wearing light clothes and taking the shoes off. To determine the waist and hip circumferences, a flexible and fixed elastic band was used, respectively, at the midpoint between the last rib and the iliac crest and the widest part of the hip in the standing position.
Laboratory tests were performed using the Pars Azmun kit (Pars Azmun, Karaj, Iran). For measuring fasting blood glucose, hemoglobin A1C, total cholesterol, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglycerides, and serum 25-hydroxy vitamin D3 concentration (the most useful form in assessing vitamin D status), 20 ml of venous blood was drawn after overnight fasting for 8–12 h. 25(OH) vitamin D3 was measured using the ECLIA (Roche) method. Lipid measurements were performed using the following methods: enzymatic (CHOD-PAP) colorimetric method for total cholesterol, enzymatic (CHE&CHO) colorimetric method for LDL-C and HDL-C, and enzymatic (GPO-PAP) colorimetric method for triglyceride. Fasting blood glucose was measured by the enzymatic (glucose oxidase) colorimetric method, and hemoglobin A1C was assessed by CERAGEM MEDISYS, chungcheongnam-do, Korea. All processes were carried out by professional personnel.
Definition of terms
Sufficient vitamin D is defined when the serum 25-hydroxyvitamin D [25(OH)D] concentration is at least 30 ng/ml, while 25(OH)D concentrations between 20 and 29 ng/ml are thought to be insufficient, and a serum concentration below 20 ng/ml indicates vitamin D deficiency37,38. Diabetes was diagnosed as taking any antidiabetic drugs, fasting blood glucose ≥ 126 mg/dl, and hemoglobin A1C (HbA1C) ≥ 6.5%39. Hypertension was defined as systolic blood pressure of 140 mmHg or more, diastolic blood pressure of at least 90 mmHg, or the use of medications for high blood pressure control40. Triglyceride concentrations greater than 149 mg/dl were considered hypertriglyceridemia41. Lipid disorders, including total cholesterol ≥ 200 mg/dl, LDL-C ≥ 130 mg/dl, HDL-C ≤ 40 mg/dl for men or ≤ 50 mg/dl for women, or hypertriglyceridemia, are defined as dyslipidemia42,43.
Statistical analysis
In this study, categorical variables have been reported using frequency and percentage, while continuous variables were described with mean and standard deviation values. The normality of the data was analyzed through the Kolmogorov‒Smirnov test. The male and female groups have been compared in demographic and clinical features, body composition, cardiovascular risk factors, and vitamin D consumption with the chi-square test for categorical variables and the T test for continuous variables, whereas for evaluating them based on the status of vitamin D serum concentrations, the one-way ANOVA test for continuous variables and the chi-square test for categorical variables has been used. The association between vitamin D status and obesity markers was investigated using logistic and linear regression analysis after adjusting for confounding variables, including age, gender, marital status, physical activity, smoking, income, occupation, education, and use of vitamin D supplements. Additionally, to indicate the relationship between vitamin D concentration and cardiometabolic risk factors, logistic and linear regression analyses have been performed after adjustment in two models: first for age, gender, marital status, physical activity, smoking, income, occupation, education, and use of vitamin D supplements as confounding factors, and second for all mentioned factors and total fat mass. STATA statistical software (14 version) and SPSS 20 were used for all analyses, and a significance threshold was defined as a p value of 0.05 or lower.
Ethics approval and consent to participate
The Ethics Committee of Bushehr University of Medical Sciences granted ethical permission for this study (Ethical Code: IR.BPUMS.REC.1402.063) in compliance with the Helsinki Declaration and national guidelines for research ethics. Before research enrollment, all participants gave their informed consent after being informed about the procedures involved in the study. Participation was entirely optional, and any participant could withdraw consent at any moment with no repercussions.
Consent for publication
The authors confirm that human research participants provided informed consent for publication of their data.
Results
Sociodemographic and clinical characteristics of the subjects
A total of 1991 older adults aged 48–95 years were included in this study. Overall, the mean (SD) age of the participants in the study was 62.1 (± 8.06) years; 57.1% (n = 1137) were women, and 86.4% (n = 1721) were married. Table 1 presents demographic and clinical factors stratified by sex. Men had significantly lower total cholesterol, LDL-cholesterol, abdominal obesity, BMI, total fat, and subcutaneous and visceral fat than women (P < 0.001). In contrast, women showed higher concentrations of HDL cholesterol and vitamin D than men (P < 0.001). Typically, the proportion of women with supplementation was much higher than that of men (54.4% vs. 34.9%) and, in consequence, showed a much higher mean vitamin D blood concentration: 28.6 ng/ml vs. 24.3 ng/ml (Table 1).
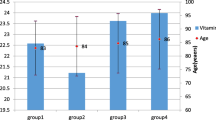
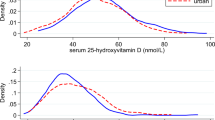
Sociodemographic and clinical characteristics according to vitamin D status
The prevalence of vitamin D deficiency, insufficiency, and sufficiency of participants in the study was 38.5% (95% CI 36.4–40.7), 26.8% (95% CI 24.8–28.7), and 34.7% (95% CI 32.5–36.7), respectively. Based on the results of Table 2, in men and women with sufficient serum 25(OH)D concentrations, the mean waist circumference, total cholesterol, LDL-cholesterol, and triglyceride were lower, and the HDL-cholesterol concentration was higher.
Serum vitamin D and total and regional obesity
The associations between serum 25(OH)D and obesity markers are shown in Table 3. After adjusting for age, gender, marital status, physical activity, tobacco, income status, education, job, and vitamin D supplementation, there was an inverse association between serum 25(OH) D and BMI (β = − 0.015, 95% CI − 0.0297 to − 0.0007, P = 0.04) and waist circumference (β = − 0.060, 95% CI − 0.0951 to − 0.0252, P = 0.001). The results of multiple linear regression suggested that an increase in plasma 25(OH) D concentration was inversely associated with total fat (β = − 0.023, 95% CI − 0.0428 to − 0.0036, P = 0.02), android fat (β = − 0.003, 95% CI − 0.0059 to − 0.0014, P = 0.001), visceral fat (β = − 0.001, 95% CI − 0.0023 to − 0.0007, P < 0.001), SAT fat (β = − 0.001, 95% CI − 0.0027 to − 0.0003, P = 0.01), trunk fat (β = − 0.016, 95% CI − 0.0279 to − 0.0046, P = 0.006), and arm fat (β = − 0.001, 95% CI − 0.0028 to − 0.0008, P = 0.03).
Serum vitamin D and cardiometabolic risk factors
For the cardiometabolic markers, an inverse association between 25(OH)D and high systolic blood pressure was observed, which was significant after adjusting for age, gender, marital status, physical activity, tobacco, income status, education, job, BMI, vitamin D supplementation, and total fat mass (OR 0.98, 95% CI 0.98–0.99, P = 0.004). In addition, serum 25(OH) D was inversely associated with the lipid profile in individuals, including high LDL-cholesterol (OR 0.98, 95% CI 0.98–0.99, P < 0.001), high total cholesterol (OR 0.98, 95% CI 0.98–0.99, P < 0.001) and high serum triglycerides (OR 0.98, 95% CI 0.98–0.99, P = 0.001), after adjusting for potential confounders. Furthermore, in the multiple logistic regression model, the association of serum 25(OH)D and high fasting blood glucose was statistically significant (OR 0.98, 95% CI 0.98–0.99, P < 0.001). Finally, in the multiple-adjusted logistic regression analysis, an increase in serum 25(OH)D reduced the odds of dyslipidemia by 2% (Table 4).
Discussion
The results of this study demonstrated an inverse relationship between low serum concentrations of vitamin D and multiple cardiometabolic risk variables, including lipid profile, fasting blood sugar, and systolic blood pressure. Furthermore, it was shown that there is an inverse association between vitamin D concentrations and several markers of total and local obesity, such as BMI, waist circumference, total fat mass, android fat, visceral adipose tissue, subcutaneous fat, trunk fat, and arm fat mass.
By considering the higher prevalence of vitamin D deficiency, CVD, and obesity in the older population, we designed this research to determine whether there is any association between low vitamin D serum concentrations and cardiometabolic risk factors and obesity. Lower vitamin D concentrations are more common in the older population44. This age-related deficiency is a result of reduced vitamin D synthesis in the skin due to a reduction in dermis and epidermis thickness and a decreased concentration of epidermal 7-dehydrocholesterol, which is the basic substance for vitamin D synthesis. Moreover, the production of renal 1,25-dihydroxyvitamin D, a biologically active form of vitamin D, is also reduced by aging. In addition, the lifestyle of older adults, such as low vitamin D consumption following poor appetite or limited exposure to sunlight due to a lower ability for outside activities, can also decrease vitamin D concentrations45.
The results of this investigation revealed that almost 65% of the study population did not have the optimal concentration of vitamin D. Although this rate of vitamin D deficiency is almost double that of the United States, in comparison to a study that showed the vitamin D status of older adults in Iran in 2013, the prevalence of vitamin D deficiency is 15–20 percent lower17. This discrepancy might be caused by Bushehr having more sunny days in Iran. On the other hand, different cutoff values for vitamin D deficiency in different published studies and the high rate of vitamin D supplementation in our female population must be considered.
We found an inverse association between vitamin D concentrations and only systolic blood pressure before and after adjusting for confounding factors. This finding was consistent with the results of the previous meta-analysis46. However, this study demonstrated no considerable association between serum 25(OH)D concentrations and hypertension. Similarly, a large study that included 2456 men and women reported no evidence of an association between vitamin D serum concentrations and hypertension47. Likewise, previous recent studies have revealed that vitamin D supplementation does not reduce blood pressure48,49,50. Nevertheless, serum vitamin D status has been shown to be inversely correlated with the risk of adult hypertension in a meta-analysis of 283,537 participants51. Possible effects of vitamin D on the renin-angiotensin system and vascular tone regulation may contribute to the decrease in blood pressure49,52,53. In addition, UVA and UVB radiation themselves may have a seasonal influence on systolic and diastolic blood pressure54,55. However, our results showed that sufficient serum concentrations of vitamin D have a small, statistically significant impact on reducing blood pressure, especially systolic blood pressure. A recent review revealed that while it is still difficult to prove that vitamin D has a direct antihypertensive impact on its own, adding vitamin D with another typical antihypertensive medication to decrease the BP showed favorable outcomes48. Consequently, more studies are needed to investigate the direct effects of vitamin D on blood pressure.
Vitamin D has been shown to affect factors that lead to the onset of type 2 diabetes, including chronic inflammation, insulin sensitivity, and insulin production56,57. The existence of vitamin D receptors in muscle, adipocytes, and hepatocytes, as well as the improvement of insulin receptor expression and sensitivity to insulin for glucose transport, are some of the ways that vitamin D might decrease insulin resistance. In another way, vitamin D may also do this by regulating calcium metabolism, which is crucial for intracellular activities mediated by insulin58. Although in this study, the relationship between vitamin D and type 2 diabetes mellitus was not statistically significant, we observed an independent inverse association between fasting blood glucose and vitamin D status. Likewise, a meta-analysis in 2018 including 44,161 individuals found that vitamin D supplementation may enhance the metabolism of glucose and insulin without influencing the risk of type 2 diabetes in adults without diabetes59. Additionally, there was no significant relationship reported in our research between hemoglobin A1C and vitamin D concentrations. Similarly, a recent meta-analysis revealed that eating foods higher in vitamin D was linked to a lower HbA1c; however, the difference was not statistically significant60. Nonetheless, some research findings indicate that vitamin D significantly lowers HbA1c in those with prediabetes or diabetes 61,62,63. Additionally, a number of earlier studies have demonstrated that vitamin D supplementation can lower the risk of developing diabetes in prediabetic persons58,62,64,65,66. As a result, it appears that sufficient vitamin D concentrations have a positive impact on lowering blood sugar concentrations, especially in the prediabetic population. However, the intensity of this impact is dependent on the initial vitamin D concentration and the risk of developing type 2 diabetes. Moreover, this effect is inadequate to prevent or cure diabetes independently over the nondiabetic population. This conclusion is supported by some recent investigations26,56,67,68. However, further research is still needed to fully understand the relationship between vitamin D and diabetes.
It has been shown that there is likely a significant association between the lipid profile and vitamin D concentration69. However, a recent review reported that while many observational studies indicate a potential link between vitamin D and lipid concentration in the blood, the results of interventional studies don't seem to entirely support the findings70. Although the exact mechanism underlying this possible relationship is still unclear, studies have shown that vitamin D has beneficial impacts on reducing lipogenesis by raising calcium concentrations and lowering the prevalence of hyperparathyroidism, increasing lipolysis by promoting leptin concentrations, and having a role in lipoprotein lipase regulation71. In the same way, our findings show a considerable inverse association between plasma 25(OH)D and total cholesterol, LDL cholesterol, and triglycerides. However, the association with HDL cholesterol was not statistically significant. Additionally, previous results regarding the relationship between HDL cholesterol and vitamin D were controversial72,73. As a result, this study found a substantial association between vitamin D and dyslipidemia, which is compatible with how vitamin D affects the majority of lipid profile markers.
There is a well-established association between decreased vitamin D concentrations and some body adiposity indicators74. This inverse association can be attributed to a reduced bioavailability of circulating vitamin D as a result of increased vitamin D deposition in adipose tissue or a reduction in sunshine exposure in obese people75. Moreover, the catabolism rate of vitamin D is higher in adipose tissue, and vitamin D may have anti-inflammatory effects and be connected to visceral obesity, which is linked to inflammation76. However, a recent article states that the association between vitamin D and obesity is still debatable because of significant confounding factors in studies77. Conversely, after adjusting for confounding variables, we discovered a significant inverse association between serum vitamin D concentrations and indices of total and regional obesity, including BMI, waist circumference, total fat mass, visceral fat mass, subcutaneous fat mass, android fat mass, trunk fat mass, and arm fat. In contrast to arm fat, our study's findings regarding the association between vitamin D and leg fat were not statistically significant. Furthermore, prior research indicated that although leg fat is associated with a more favorable blood lipid profile, arm fat appears to have no effect. This could be because femoral adipose tissue secretes fewer proinflammatory molecules and more beneficial adipokines, which could help maintain a healthier adipokine profile78. To our knowledge, the mechanism underlying this variation in how vitamin D affects them is still unclear. Similar to several previous studies, our findings showed that lower serum concentrations of vitamin D were not associated with hip circumference or gynoid fat76,79,80. It has been claimed that the risk of CVD is inversely associated with increased gynoid fat, despite android fat mass81,82. This finding has been linked to gynoid adipocyte-enhanced lipoprotein lipase activity and more efficient free fatty acid accumulation compared to visceral adipocytes83. As mentioned before, vitamin D may regulate lipoprotein lipase function and affect the lipid profile through several hypothetical mechanisms. Thus, it would be interesting to conduct research into the process that results in the various effects of vitamin D on different areas of fat.
While studies have supported the idea that vitamin D's anti-inflammatory effects modify a number of factors that contribute to autoimmune and cardiovascular diseases, the findings of some interventional studies still did not approve a decrease in inflammatory markers following vitamin D supplementation84,85,86,87. For instance, following vitamin D supplementation, several randomized controlled trials showed no decrease in interleukin (IL)-6 or high-sensitivity C-reactive protein (hs-CRP)88,89. Moreover, findings of the VITAL randomized trial showed that after two years, vitamin D3 supplementation reduced hs-CRP without effect on any other inflammatory markers like interleukin-6 or tumor necrosis factor-α90. Consequently, the findings of research regarding vitamin D's impact on inflammation remain debatable and require further investigation in the future.
In addition to the mechanisms mentioned about the effect of vitamin D on each of the cardiometabolic risk factors, recent studies have shown that vitamin D changes the composition of the gut microbiota and increases the number of beneficial bacteria, processes resulting from the gut microbiota that are strongly correlated with several cardiometabolic risk factors, including glucose homeostasis, lipid metabolism, blood pressure, adiposity, vascular inflammation, and atherosclerosis91,92,93.
The main strengths of the present study are that it was conducted in a considerable population and that it was the first study to evaluate a wide range of cardiometabolic risk factors in relation to vitamin D concentrations while also comprehensively investigating fat mass and distribution in the older population of Iran. The availability of important confounding factors is another advantage. However, there are also limitations to take into account. Since our study was cross-sectional, no causal relationships can be deduced from the findings. Another limitation of our research is that the analysis of the study wasn't adjusted for the use of anti-lipid or antidiabetic medications. Furthermore, it may not be possible to generalize the results to all Iranian older adults because the study was conducted in a population of a specific geographic region. This study's inability to account for the older subjects' eating habits was another flaw.
In conclusion, the study results revealed that serum concentrations of vitamin D are inversely associated with several cardiometabolic risk factors, including total cholesterol, LDL-cholesterol, triglycerides, fasting blood glucose, and systolic blood pressure. Moreover, it was observed that total and regional obesity, such as android, visceral, subcutaneous, trunk, and arm fat, are also inversely related to vitamin D status. Although further investigations are needed to determine the causative relationship, maintaining optimal vitamin D concentrations is essential for lowering the consequences of cardiometabolic disorders.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Després, J. P. & Lemieux, I. Abdominal obesity and metabolic syndrome. Nature. 444(7121), 881–887 (2006).
Leiter, L. A. et al. Cardiometabolic risk in Canada: A detailed analysis and position paper by the cardiometabolic risk working group. Can. J. Cardiol. 27(2), e1–e33 (2011).
Mezhal, F. et al. High prevalence of cardiometabolic risk factors amongst young adults in the United Arab Emirates: The UAE Healthy Future Study. BMC Cardiovasc. Disord. 23(1), 137 (2023).
Nichols, G. A. et al. Cardiometabolic risk factors among 1.3 million adults with overweight or obesity, but not diabetes, in 10 geographically diverse regions of the United States, 2012–2013. Prev. Chronic Dis. 14, 22 (2017).
Brown, J. C., Gerhardt, T. E., Kwon, E. Risk Factors for Coronary Artery Disease (StatPearls Publishing LLC., 2023).
Lavie, C. J. et al. Healthy weight and obesity prevention: JACC health promotion series. J. Am. Coll. Cardiol. 72(13), 1506–1531 (2018).
Roth, G. A. et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 76(25), 2982–3021 (2020).
Chauhan, K., Shahrokhi, M. & Huecker, M. R. Vitamin D (StatPearls Publishing LLC, 2023).
Amirkhizi, F., Khademi, Z., Hamedi Shahraki, S. & Rahimlou, M. Vitamin D insufficiency and its association with adipokines and atherogenic indices in patients with metabolic syndrome: A case-control study. Front. Endocrinol. (Lausanne). 14, 1080138 (2023).
Ganji, V., Tangpricha, V. & Zhang, X. Serum vitamin D concentration ≥75 nmol/L is related to decreased cardiometabolic and inflammatory biomarkers, metabolic syndrome, and diabetes; and increased cardiorespiratory fitness in US adults. Nutrients. 12(3), 730 (2020).
Hajhashemy, Z., Shahdadian, F., Ziaei, R. & Saneei, P. Serum vitamin D levels in relation to abdominal obesity: A systematic review and dose-response meta-analysis of epidemiologic studies. Obes. Rev. 22(2), e13134 (2021).
Pham, T. M., Ekwaru, J. P., Setayeshgar, S. & Veugelers, P. J. The effect of changing serum 25-hydroxyvitamin D concentrations on metabolic syndrome: A longitudinal analysis of participants of a preventive health program. Nutrients. 7(9), 7271–7284 (2015).
Szymczak-Pajor, I., Miazek, K., Selmi, A., Balcerczyk, A. & Śliwińska, A. The action of vitamin D in adipose tissue: Is there the link between vitamin D deficiency and adipose tissue-related metabolic disorders?. Int. J. Mol. Sci. 23(2), 956 (2022).
Wolters, M. et al. Longitudinal associations between vitamin D status and cardiometabolic risk markers among children and adolescents. J. Clin. Endocrinol. Metab. 108, e1731–e1742 (2023).
Nemeth, Z., Patonai, A., Simon-Szabó, L. & Takács, I. Interplay of vitamin D and SIRT1 in tissue-specific metabolism—Potential roles in prevention and treatment of non-communicable diseases including cancer. Int. J. Mol. Sci. 24(7), 6154 (2023).
Sizar, O., Khare, S., Goyal, A. & Givler, A. Vitamin D deficiency (StatPearls Publishing LLC, 2023).
Palacios, C. & Gonzalez, L. Is vitamin D deficiency a major global public health problem?. J. Steroid Biochem. Mol. Biol. 144(Pt A), 138–145 (2014).
Lee, S. J. et al. Associations of serum 25-hydroxyvitamin D with metabolic syndrome and its components in elderly men and women: The Korean Urban Rural Elderly cohort study. BMC Geriatr. 19(1), 102 (2019).
Liu, L. et al. Vitamin D deficiency and metabolic syndrome in elderly Chinese individuals: Evidence from CLHLS. Nutr. Metab. 17(1), 58 (2020).
Mutt, S. J. et al. Vitamin D status and components of metabolic syndrome in older subjects from Northern Finland (Latitude 65°North). Nutrients. 11(6), 1229 (2019).
Wang, C. M. et al. Inverse relationship between metabolic syndrome and 25-hydroxyvitamin D concentration in elderly people without vitamin D deficiency. Sci. Rep. 8(1), 17052 (2018).
Joseph, P. et al. Vitamin D supplementation and adverse skeletal and non-skeletal outcomes in individuals at increased cardiovascular risk: Results from the International Polycap Study (TIPS)-3 randomized controlled trial. Nutr. Metab. Cardiovasc. Dis. 33(2), 434–440 (2023).
Manson, J. E. et al. Vitamin D supplements and prevention of cancer and cardiovascular disease. N. Engl. J. Med. 380(1), 33–44 (2019).
Pittas, A. G. et al. Vitamin D supplementation and prevention of type 2 diabetes. N. Engl. J. Med. 381(6), 520–530 (2019).
Karuppusami, R. et al. Association of serum 25-hydroxy vitamin D with total and regional adiposity and cardiometabolic traits. PLoS One. 15(12), e0243850 (2020).
Mba, C. M. et al. Association between circulating 25-hydroxyvitamin D and cardiometabolic risk factors in adults in rural and urban settings. Nutr. Diabetes. 12(1), 34 (2022).
Romero-Corral, A. et al. Accuracy of body mass index in diagnosing obesity in the adult general population. Int. J. Obes. (Lond). 32(6), 959–966 (2008).
Kim, J. Y., Han, S. H. & Yang, B. M. Implication of high-body-fat percentage on cardiometabolic risk in middle-aged, healthy, normal-weight adults. Obesity (Silver Spring). 21(8), 1571–1577 (2013).
Lu, Y. C., Lin, Y. C., Yen, A. M. & Chan, W. P. Dual-energy X-ray absorptiometry-assessed adipose tissues in metabolically unhealthy normal weight Asians. Sci. Rep. 9(1), 17698 (2019).
Shepherd, J. A., Ng, B. K., Sommer, M. J. & Heymsfield, S. B. Body composition by DXA. Bone. 104, 101–105 (2017).
Khosravi Shadmani, F., Farzadfar, F., Larijani, B., Mirzaei, M. & Haghdoost, A. A. Trend and projection of mortality rate due to non-communicable diseases in Iran: A modeling study. PLoS One. 14(2), e0211622 (2019).
Marzban, M. et al. Prevalence of vitamin D deficiency and its associated risk factors among rural population of the northern part of the Persian Gulf. BMC Endocr. Disord. 21(1), 219 (2021).
Shafiee, G. et al. Bushehr Elderly Health (BEH) programme: Study protocol and design of musculoskeletal system and cognitive function (stage II). BMJ Open. 7(8), e013606 (2017).
Khashayar, P. et al. Protocol for a multicentre, prospective cohort study of clinical, proteomic and genomic patterns associated with osteoporosis to develop a multidimensional fracture assessment tool: The PoCOsteo Study. BMJ Open. 10(9), e035363 (2020).
Aadahl, M. et al. Recent temporal trends in sleep duration, domain-specific sedentary behaviour and physical activity. A survey among 25–79-year-old Danish adults. Scand. J. Public Health. 41(7), 706–711 (2013).
Aadahl, M. & Jørgensen, T. Validation of a new self-report instrument for measuring physical activity. Med. Sci. Sports Exerc. 35(7), 1196–1202 (2003).
Płudowski, P. et al. Guidelines for preventing and treating vitamin D deficiency: A 2023 update in Poland. Nutrients. 15(3), 695 (2023).
Rosen, C. J. Clinical practice. Vitamin D insufficiency. N. Engl. J. Med. 364(3), 248–254 (2011).
ElSayed, N. A. et al. 2. Classification and diagnosis of diabetes: Standards of care in diabetes-2023. Diabetes Care. 46(Suppl 1), S19–S40 (2023).
Unger, T. et al. 2020 international society of hypertension global hypertension practice guidelines. Hypertension. 75(6), 1334–1357 (2020).
Miller, M. et al. Triglycerides and cardiovascular disease: A scientific statement from the American Heart Association. Circulation. 123(20), 2292–2333 (2011).
Third Report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 106(25), 3143–3421 (2002).
Rader, D. J., Hoeg, J. M. & Brewer, H. B. Jr. Quantitation of plasma apolipoproteins in the primary and secondary prevention of coronary artery disease. Ann. Intern. Med. 120(12), 1012–1025 (1994).
Boettger, S. F. et al. Prevalence and predictors of vitamin D-deficiency in frail older hospitalized patients. BMC Geriatr. 18(1), 219 (2018).
Chalcraft, J. R. et al. Vitamin D synthesis following a single bout of sun exposure in older and younger men and women. Nutrients. 12(8), 2237 (2020).
Vimaleswaran, K. S. et al. Association of vitamin D status with arterial blood pressure and hypertension risk: A mendelian randomisation study. Lancet Diabetes Endocrinol. 2(9), 719–729 (2014).
Qi, D., Nie, X. L., Wu, S. & Cai, J. Vitamin D and hypertension: Prospective study and meta-analysis. PLoS One. 12(3), e0174298 (2017).
Jensen, N. S., Wehland, M., Wise, P. M. & Grimm, D. Latest knowledge on the role of vitamin D in hypertension. Int. J. Mol. Sci. 24(5), 4679 (2023).
Vaidya, A. & Forman, J. P. Vitamin D and hypertension: Current evidence and future directions. Hypertension. 56(5), 774–779 (2010).
Zhang, D. Effect of vitamin D on blood pressure and hypertension in the general population: An update meta-analysis of cohort studies and randomized controlled trials. Prev. Chronic Dis. 17 (2020).
Kunutsor, S. K., Apekey, T. A. & Steur, M. Vitamin D and risk of future hypertension: Meta-analysis of 283,537 participants. Eur. J. Epidemiol. 28, 205–221 (2013).
Cianciolo, G. et al. Vitamin D effects on bone homeostasis and cardiovascular system in patients with chronic kidney disease and renal transplant recipients. Nutrients. 13(5), 1453 (2021).
Latic, N. & Erben, R. G. Vitamin D and cardiovascular disease, with emphasis on hypertension, atherosclerosis, and heart failure. Int. J. Mol. Sci. 21(18), 6483 (2020).
Kapil, V. & Gupta, A. K. Solar UV radiation: A potential modifiable risk factor for hypertension. J. Am. Heart Assoc. 9(5), e015627 (2020).
Weller, R. B. et al. Does incident solar ultraviolet radiation lower blood pressure?. J. Am. Heart Assoc. 9(5), e013837 (2020).
Grammatiki, M., Rapti, E., Karras, S., Ajjan, R. A. & Kotsa, K. Vitamin D and diabetes mellitus: Causal or casual association?. Rev. Endocr. Metab. Disord. 18(2), 227–241 (2017).
Mitri, J. & Pittas, A. G. Vitamin D and diabetes. Endocrinol. Metab. Clin. N. Am. 43(1), 205–232 (2014).
Zhang, Y. et al. Effects of vitamin D supplementation on prevention of type 2 diabetes in patients with prediabetes: A systematic review and meta-analysis. Diabetes Care. 43(7), 1650–1658 (2020).
Tang, H. et al. Effects of vitamin D supplementation on glucose and insulin homeostasis and incident diabetes among nondiabetic adults: A meta-analysis of randomized controlled trials. Int. J. Endocrinol. 2018, 7908764 (2018).
Emadzadeh, M. et al. A systematic review and meta-analysis of the effect of Vitamin D-fortified food on glycemic indices. Biofactors. 46(4), 502–513 (2020).
Pannu, P. K., Piers, L. S., Soares, M. J., Zhao, Y. & Ansari, Z. Vitamin D status is inversely associated with markers of risk for type 2 diabetes: A population based study in Victoria, Australia. PLoS One. 12(6), e0178825 (2017).
Zhang, Y. et al. Effect of vitamin D supplementation on glycemic control in prediabetes: A meta-analysis. Nutrients. 13(12), 4464 (2021).
Zoppini, G. et al. Glycated haemoglobin is inversely related to serum vitamin D levels in type 2 diabetic patients. PLoS One. 8(12), e82733 (2013).
Mirhosseini, N., Vatanparast, H., Mazidi, M. & Kimball, S. M. Vitamin D supplementation, glycemic control, and insulin resistance in prediabetics: A meta-analysis. J. Endocr. Soc. 2(7), 687–709 (2018).
Pittas, A. G. et al. Vitamin D and risk for type 2 diabetes in people with prediabetes: A systematic review and meta-analysis of individual participant data from 3 randomized clinical trials. Ann. Intern. Med. 176(3), 355–363 (2023).
Sacerdote, A., Dave, P., Lokshin, V. & Bahtiyar, G. Type 2 diabetes mellitus, insulin resistance, and vitamin D. Curr. Diabetes Rep. 19(10), 101 (2019).
Kawahara, T. et al. Effect of active vitamin D treatment on development of type 2 diabetes: DPVD randomised controlled trial in Japanese population. BMJ. 377, e066222 (2022).
Md Isa, Z., Amsah, N. & Ahmad, N. The impact of vitamin D deficiency and insufficiency on the outcome of type 2 diabetes mellitus patients: A systematic review. Nutrients. 15(10), 2310 (2023).
Surdu, A. M. et al. Vitamin D and its role in the lipid metabolism and the development of atherosclerosis. Biomedicines. 9(2), 172 (2021).
Al Refaie, A. et al. Vitamin D and dyslipidemia: Is there really a link? A narrative review. Nutrients. 16(8), 1144 (2024).
Huang, X., Yang, Y., Jiang, Y., Zhou, Z. & Zhang, J. Association between vitamin D deficiency and lipid profiles in overweight and obese adults: A systematic review and meta-analysis. BMC Public Health. 23(1), 1653 (2023).
Dibaba, D. T. Effect of vitamin D supplementation on serum lipid profiles: A systematic review and meta-analysis. Nutr. Rev. 77(12), 890–902 (2019).
Lupton, J. R. et al. Deficient serum 25-hydroxyvitamin D is associated with an atherogenic lipid profile: The Very Large Database of Lipids (VLDL-3) study. J. Clin. Lipidol. 10(1), 72-81.e1 (2016).
Ganji, V. et al. Serum 25-hydroxyvitamin D concentrations are inversely associated with body adiposity measurements but the association with bone mass is non-linear in postmenopausal women. J. Steroid Biochem. Mol. Biol. 212, 105923 (2021).
Vanlint, S. Vitamin D and obesity. Nutrients. 5(3), 949–956 (2013).
Vitezova, A. et al. Vitamin D and body composition in the elderly. Clin. Nutr. 36(2), 585–592 (2017).
Karampela, I. et al. Vitamin D and obesity: Current evidence and controversies. Curr. Obes. Rep. 10(2), 162–180 (2021).
Sánchez-López, M. et al. Leg fat might be more protective than arm fat in relation to lipid profile. Eur. J. Nutr. 52(2), 489–495 (2013).
Andreozzi, P. et al. Relationship between vitamin D and body fat distribution evaluated by DXA in postmenopausal women. Nutrition. 32(6), 687–692 (2016).
Li, H. et al. Central body fat deposits are associated with poor vitamin D status in Chinese children and adolescents. Nutrition. 99–100, 111651 (2022).
Liu, C. A. et al. The relationship between fat distribution in central region and comorbidities in obese people: Based on NHANES 2011–2018. Front. Endocrinol. (Lausanne). 14, 1114963 (2023).
Yang, Y. et al. Sex differences in the associations between adiposity distribution and cardiometabolic risk factors in overweight or obese individuals: A cross-sectional study. BMC Public Health. 21(1), 1232 (2021).
Wiklund, P. et al. Abdominal and gynoid fat mass are associated with cardiovascular risk factors in men and women. J. Clin. Endocrinol. Metab. 93(11), 4360–4366 (2008).
Ao, T., Kikuta, J. & Ishii, M. The effects of vitamin D on immune system and inflammatory diseases. Biomolecules. 11(11), 1624 (2021).
Hahn, J. et al. Vitamin D and marine omega 3 fatty acid supplementation and incident autoimmune disease: VITAL randomized controlled trial. BMJ. 376, e066452 (2022).
Mousa, H., Islam, N., Ganji, V. & Zughaier, S. M. Serum 25-hydroxyvitamin D is inversely associated with monocyte percentage to HDL cholesterol ratio among young healthy adults in Qatar. Nutrients. 13(1), 127 (2020).
Yin, K. & Agrawal, D. K. Vitamin D and inflammatory diseases. J. Inflamm. Res. 7, 69–87 (2014).
Costenbader, K. H. et al. Effects of one year of vitamin D and marine omega-3 fatty acid supplementation on biomarkers of systemic inflammation in older US adults. Clin. Chem. 65(12), 1508–1521 (2019).
Limonte, C. P. et al. Effects of long-term vitamin D and n-3 fatty acid supplementation on inflammatory and cardiac biomarkers in patients with type 2 diabetes: Secondary analyses from a randomised controlled trial. Diabetologia. 64(2), 437–447 (2021).
Dong, Y. et al. Effects of vitamin D(3) and marine omega-3 fatty acids supplementation on biomarkers of systemic inflammation: 4-Year findings from the VITAL randomized trial. Nutrients. 14(24), 5307 (2022).
Tangestani, H., Boroujeni, H. K., Djafarian, K., Emamat, H. & Shab-Bidar, S. Vitamin D and the gut microbiota: A narrative literature review. Clin. Nutr. Res. 10(3), 181–191 (2021).
Warmbrunn, M. V. et al. Gut microbiota: A promising target against cardiometabolic diseases. Expert Rev. Endocrinol. Metab. 15(1), 13–27 (2020).
Witkowski, M., Weeks, T. L. & Hazen, S. L. Gut microbiota and cardiovascular disease. Circ. Res. 127(4), 553–570 (2020).
Acknowledgements
The authors would like to express their appreciation to all medical research center employees at Bushehr University of Medical Sciences (BPUMS) and Tehran University of Medical Sciences (TUMS) for their dedication and collaboration. The authors would also like to convey their heartfelt appreciation to the Persian Gulf Martyrs Hospital’s Clinical Research Development Center, the “Student Research Committee” and the Persian Gulf Tropical Medicine Research Center in Bushehr University of Medical Sciences. We would like to thank all participants for their participation in the study.
Funding
The Persian Gulf Biomedical Sciences Research Institute, affiliated with Bushehr (Port) University of Medical Sciences (BPUMS), and the Endocrinology and Metabolism Research Institute, affiliated with Tehran University of Medical Sciences, both contributed to funding for the BEH Program. This study project was designed and carried out with the help of researchers from both research institutions. Availability of data and materials of the datasets used during the current study are available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Contributions
A.N., H.E., A.F. designed and conceptualized the study. S.A., A.J. conducted the main statistical analysis. A.N., Z.J., Z.T. wrote the original manuscript. A.J., A.F., H.E., J.S. reviewed, edited and finalized the manuscript. A.J., I.N., B.L., J.S. provided critical comments on the results and discussion. I.N., B.L. funding acquisition and data curation. All authors reviewed and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Nejabat, A., Emamat, H., Afrashteh, S. et al. Association of serum 25-hydroxy vitamin D status with cardiometabolic risk factors and total and regional obesity in southern Iran: evidence from the PoCOsteo study. Sci Rep 14, 17983 (2024). https://doi.org/10.1038/s41598-024-68773-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-68773-1
- Springer Nature Limited