Abstract
Telemedicine has gained popularity due to the increasing use of technology in our lives. However, no studies have explored the demographic factors affecting acceptability, desirability and adherence (ADA) to telemedicine in Singapore. Our study aims to evaluate the level of ADA of telemedicine services within demographic factors and to explore the association of potential demographic factors with the degree of acceptability, desirability and adherence of telemedicine among older adults in Singapore. A cross-sectional study was conducted with Singapore citizens or permanent residents aged 40–99 years, who were able to provide informed consent. Interviewers conducted door-to-door surveys in 67 Blocks of Housing & Development Board flats in Singapore, offering a self-administered electronic questionnaire available in four languages. Random sampling without replacement determined the order of blocks, floors and units visited. The questionnaire utilised Qtelemediab scoring and covered sociodemographic data, usage of telemedicine, as well as ADA towards telemedicine. A total of 324 valid responses were analysed. Increased age was associated with a significant decrease across all three domains of ADA namely acceptability (β = − 0.02, 95%CI − 0.03; − 0.02, p-value = 0.002), desirability (β = − 0.02, 95%CI − 0.02; − 0.02, p-value < 0.001) and adherence (β = − 0.02, 95%CI − 0.03; − 0.0.02, p-value < 0.001). Additionally, lower education was associated with a decrease in all domains of ADA. Conversely, employment and increased household income were associated with higher ADA scores across all three domains. These associations were independent of gender, chronic health conditions and smoking history. Older participants with lower income and lesser education demonstrated lower levels of acceptability, desirability and adherence towards telemedicine. Our study highlights the importance of considering these factors in the implementation and promotion of telemedicine solutions.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Technological advances have given way to a new form of patient care–telemedicine.
According to the World Health Organization (WHO), telemedicine is “the provision of healthcare services at a distance with communication conducted between healthcare providers seeking clinical guidance and support from other healthcare providers; or conducted between remote healthcare users seeking health services and healthcare providers”1.
The COVID-19 pandemic accelerated the adoption of telemedicine2. With social distancing measures and stretched healthcare system capacities3, telemedicine became a convenient way to access various outpatient services remotely4. COVID-19 forced patients to adopt telemedicine, and became permanent in healthcare5.
Telemedicine offers many benefits, including increased accessibility, (especially for busy, geographically remote and non-ambulating patients)6, time efficiency (by reducing travel and wait times)7, continuous patient monitoring (especially for chronic conditions)8 and reduced costs9. This increases the quality of healthcare and health outcomes through early detection, intervention and consistent follow up10.
However, many older adults are overlooked due to technological challenges and acceptance towards telemedicine services. This digital divide between young and elderly users is exacerbated in Singapore, as it evolves into a Smart Nation.
Additionally, there are barriers to implementing telemedicine. One study suggests reduced perceived effectiveness from a patient’s perspective11. From a practical standpoint, technical issues, personal data breaches, an inability to conduct physical examinations12, cost13, poor technological infrastructure within a community and staff resistance to change has hindered telemedicine’s expansion14.
In this context, acceptability is a subjective measure of whether telemedicine is considered suitable, appropriate, or satisfactory by patients or providers15. Desirability refers to the quality of being valued16. Adherence17 refers to behaviour that consistently conforms to prescribed guidelines, often in pursuit of a favourable outcome17. Acceptability, desirability and adherence (ADA) to telemedicine are influenced by multiple factors such as age, gender, education level, geographical location, income and social influences18.
While previous studies have investigated the ADA of telemedicine during COVID-1919, research during non-emergencies is vital to comprehend telemedicine's lasting use beyond crises. This can provide insights into the attitudes towards telemedicine, allowing for the development of targeted interventions in routine healthcare. Notably, there is a gap in literature regarding the impact of patients' demographic factors on the ADA towards telemedicine, with only one study targeting patients with diabetes18.
This knowledge gap highlights the necessity for further investigation into how sociodemographic factors like age, income, education, and chronic conditions impact patient views and use of telemedicine. This understanding is crucial to customise initiatives and ensure equitable access to telemedicine. Hence, our study aims to explore the association of potential demographic factors with the degree of acceptability, desirability and adherence of telemedicine among older adults in Singapore.
We hypothesise that demographic factors such as younger age, higher education level and higher socioeconomic status have greater acceptance towards the use of telemedicine.
Methods
Study design and setting
A population-based cross-sectional study was conducted in Tampines district, Street 21 (Blocks 245–251, 253, 267–271), 22 (Blocks 272–282), 11 (Blocks 102–114, 117, 124–127, 138, 139), 12 (Blocks 140–145, 149–151, 156–166) and Avenue 5 (Blocks 146–148). Given that Singapore’s population demographics are relatively homogenous across Singapore, we concluded that focusing on this district is representative of the wider population demographics across Singapore and will have little influence on the analysis20. This study was designed and implemented in July 2023 and August 2023 by medical students from Yong Loo Lin School of Medicine, National University of Singapore, under faculty supervision. Ethics approval was sought from the Departmental Ethics Review Committee (DERC), NUS (Reference Number: SSHSPH-205). Informed consent was obtained from all subjects. All procedures were performed in accordance with relevant guidelines and regulations.
Sources and methods of selection
A multistage random sampling process was used to select participants (Supplementary Fig. 1). Random sampling without replacement was employed to generate the order of blocks, floors and units visited. Firstly, public housing apartments were enumerated, of which 50% were randomly selected. Secondly, 50% of floors in each selected block were randomly chosen, and every unit on those floors was included in the sampling frame. Within each selected unit, all individuals who fulfilled the inclusion criteria were enumerated. One eligible resident available at the time of the survey was selected to participate. If > 1 resident per household was eligible, a random sampling method (e.g. Kish grid) was employed.
We started off with a total of 67 blocks (7236 units) and narrowed down to 3618 units after random sampling. 373 participants attempted the questionnaire and 324 valid responses were collected.
Participants
Inclusion criteria
Our inclusion criteria were: (1) Singapore citizens or Permanent Residents aged 40–99 years residing in Singapore, (2) Individuals able to read and understand English, Chinese, Malay or Tamil, (3) Able to provide informed consent to participate in the study.
Exclusion criteria
Our exclusion criteria was; individuals unable to provide informed consent due to cognitive impairment (score < 4 in Abbreviated Mental Test (AMT-4)). For participants aged > 65, before administering the questionnaire, AMT-4 was used to screen for cognitive impairment. If scores were deemed abnormal, participants were ineligible for the survey.
Recruitment
A notification letter was distributed a week before door-to-door visits allowing residents to opt-out of the research. This cross-sectional study was carried out via door-to-door self-administered electronic questionnaires with interviewer assistance, if required, at residents' homes. Research team members followed standardised scripts delineating the objectives, procedure, benefits and risks of enrolling into the study. The questionnaire was made available in four languages: English, Chinese, Malay and Tamil. Participants were given privacy to complete the questionnaire with clarification provided if needed. Both original and translated questionnaires underwent testing among the interviewers to assess its validity and were rated easily understandable and comprehensive, before administering it to study participants.
Questionnaire design and scoring
The survey consisting of multiple-choice, closed-ended questions can be completed < 30 min. The questionnaire collected participants’ responses on: Social demographics, Acceptability (17 items), Desirability (24 items), Adherence (7 items).
The questionnaire tool, QTelemeDiab was adopted to measure ADA. QTelemeDiab consists of three sections. In section one, Q6-9 (which assesses questions on telemedicine consultations, its usage in management of acute and chronic conditions, preference of online medical consultation) were organised into Likert-scale questions, utilising a 5-point scale (1 = Not at All, 3 = Neutral, 5 = Very much). Dichotomous responses for Q1 (Have you ever used telemedicine?), Q3 (would you use telemedicine in the future?) and Q4 (would you accept to use telemedicine when your doctor would recommend it to you?) were scored 1 for ‘No’ and 5 for ‘Yes’. For unfilled responses to Q3-4, 0 points were allocated, according to their response for Q1. Q2 (which technical category of telemedicine have you used?) and Q5 (Which of the following are the instances whereby you would be comfortable using telemedicine?) were scored with 1 point for each item and accumulated points for each domain were combined to produce an aggregate domain score, which was used in our analysis. No points were deducted for participants who expressed disinterest towards telemedicine in each domain.
For section two, we included variables according to the selected social demographics. Section three was replaced by a question to account for presence of chronic conditions.
The sum of Q1-2 and Q4-5 was calculated to give the acceptability score (Minimum: 2; Maximum: 25). The sum of Q6-8 was calculated to give the desirability score (Minimum: 24; Maximum: 120). The sum of Q3 and 9 was calculated to give the adherence score (Minimum: 8; Maximum: 40).
Demographics
Selected demographics were grouped into categories to ensure that each demographic had a sizable number of participants to be analysed. Marital status was grouped into married and unmarried (Widowed/Divorced/Single). Ethnicity was split into Chinese and non-Chinese (Malay/Indian/Others). Highest educational qualification was divided into none/primary education, secondary education, tertiary education (Junior College/Nitec/Diploma equivalent) and degree holders (Bachelor’s/Master’s/Doctorate). Employment status was split into employed (Full/Part-time) and unemployed (Student/Unemployed, not seeking active employment/Unemployed, seeking active employment). Monthly household income was grouped into Low (< $3000), Middle ($3000–7000) and High (> $7000). Type of housing was categorised by type of flats (1–2 room/3-room/4–5 room or executive flats). Smoking history was divided into smokers and non-smokers (Non/Ex-smoker).
Statistical analysis
The mean and standard deviation for continuous variables were calculated, whereas the numbers and percentages were presented for categorical variables. As ADA scores are not normally distributed, we log-transformed these variables for normal distribution. We used descriptive statistics to show the distribution of demographics factors across ADA scores. We constructed linear regression models with the respective beta coefficient value, 95% CI and p-values to determine the association between sociodemographic factors and ADA scores. In the univariate analysis, we examined the association of each demographic factor with ADA scores. Multivariate regression models in a forward stepwise method were also constructed. The Akaike Information Criterion (AIC) of each regression model was used to select the best fit model for each of our 3 dependent variables. The statistical significance was set at p < 0.05. All data analysis was conducted using R (Version, 4.3.1).
Results
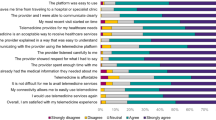
Table 1 shows the characteristics of the study participants. The mean age is 59.7 (SD = 12). A total of 52.8% participants were females and majority were Chinese (65.4%) and married (75%). The data was largely concentrated amongst participants who completed at least primary education (85.0%). Approx. 52.8% were employed and 54.6% earned < $3000/month. Over half of the participants (55.8%) resided in 4–5 room/executive HDB flats, followed by those residing in 3-room HDB flats (38.0%) and 1–2 room flats (6.2%). Lastly, over half of the participants did not have any chronic conditions (55.2%). Of the remaining participants, high blood pressure was the most prevalent (31.5%), followed by high cholesterol (20.1%) and diabetes (18.8%). Most participants were non-smokers (87%). The responses across all three categories of ADA is provided in Supplementary Fig. 2 to 10.
In Table 2, lower ADA scores were found in participants from older age groups, who are ethnic Chinese and unemployed. Those with lower educational qualifications, lower average household incomes and chronic conditions such as high blood pressure and cholesterol have lower ADA scores. Females, non-smokers and patients with diabetes displayed lower desirability and adherence scores. Participants living in smaller housing types have lower adherence and acceptability scores. Non-married participants have lower adherence scores.
Tables 3, 4 and 5 summarise the univariate associations between participants’ ADA scores and each of the sociodemographic factors respectively. Across all three outcomes, older participants generally had lower ADA scores. Degree holders had the highest ADA scores, followed by tertiary then secondary school graduates. Employed participants displayed higher ADA scores. Higher average monthly household incomes saw higher ADA scores. Participants earning > $7000 had highest ADA scores, followed by those earning $3000–7000, and finally those < $3000. Participants with high cholesterol also demonstrated lower ADA scores.
Men had higher desirability and adherence scores than women, also seen in non-Chinese participants compared to the Chinese participants. In terms of housing, participants residing in 4–5 room/executive HDB flats had higher desirability and adherence scores, followed by those residing in 3-room flats and lastly those in 1–2 room flats. Participants with high blood pressure reflected lower desirability and adherence scores, while participants with diabetes had lower acceptability and desirability scores.
Participants living in 4–5 room/executive HDB flats had significantly higher acceptability scores than those in 1–2 room flats. Participants who smoked showed higher adherence scores.
Tables 6, 7 and 8 summarise the multivariate associations between participants’ ADA scores and each of the sociodemographic factors that were chosen in our linear models. An increase in age was significantly associated with lower scores across all domains of ADA, while participants with higher educational qualifications generally had higher scores across all domains. Better housing types were generally associated with greater desirability and adherence scores. Those unemployed had lower acceptability scores. Participants with higher average monthly household income were observed to have higher desirability scores. Non-Chinese participants had higher adherence scores than their Chinese counterparts.
Discussion
Our study has shown that ADA scores were lower among older and less educated participants. Acceptability scores were lower in unemployed individuals. Desirability scores were lower among individuals of Chinese background with lower monthly household income, smoking history, diabetes mellitus and poorer housing types. Lastly, adherence scores were lower among individuals of Chinese background and poorer housing types.
In particular, the association with age and educational qualification aligns with previous studies. One showed that younger participants and those with access to digital services were more receptive to telemedical interventions21, likely due to their familiarity with technology. Conversely, less tech-savvy older adults might struggle adapting to virtual consultations, lowering acceptability and adherence. Furthermore, our findings revealed an association between lower desirability scores and participants with Chinese background, lower monthly household income, smoking history, diabetes mellitus, and poorer housing types. This concurs with a cross-sectional study conducted in a diverse urban setting, where individuals from lower socioeconomic backgrounds faced challenges in telemedicine access and use due to limited technological access, unreliable internet connectivity, and lower health literacy22.
Within a Singaporean context, a lower educational background is associated with decreased technological literacy and access to technology among the elderly23. As a result, the barrier to adopting technology and using it for their healthcare is far greater than for someone with higher educational attainment. Technology may appear a foreign medium to them, leading to lower acceptance and use of it (ADA).
Additionally, elders in Singapore might have a decreased ADA towards telemedicine due to a lack of awareness of the various available resources24,25. While many elders feel that using technology for healthcare will keep them independent for longer, financial factors might contribute to their apprehension about adopting telemedicine26.
Singapore launched the Seniors Go Digital initiative in May 2020, making phone plans and equipment more affordable for older adults to help bridge the digital divide27. However, more government initiatives are needed to promote digital literacy. For example, frequent lessons should be provided where elders can learn in a conducive environment, and their progress in digital literacy should be monitored to ensure they become more confident in using technology.
Similarly, we observed a lower adherence score among individuals of Chinese background, highlighting the need to consider cultural and linguistic factors when promoting telemedicine to the Chinese community.
We postulate that cultural factors such as the use of Complementary and Alternative Medicines (CAMs), may play a significant role in decreasing the usage of telemedicine. In Singapore, 84% of the Chinese community uses CAMs compared to 69% in both the Malay and Indian communities. Specifically, Traditional Chinese Medicine (TCM) is the most widely used form of CAM (88%), followed by traditional Malay medicine (Jamu) (8%) and traditional Indian (Ayuverdic) Medicine (3%)28. This preference for CAMs, particularly TCM, which emphasizes in-person consultations and treatments, such as acupuncture, herbal medicine, and other physical therapies, might influence the adoption and acceptance of telemedicine in the Chinese community. This cultural preference can reduce the reliance on telemedicine, which may not offer the same personalized, hands-on approach29.
Moreover, there is often a deep-rooted trust in traditional medicine practices within the Chinese community. Studies have shown that individuals who use CAMs tend to have a holistic view of health, which includes physical, emotional, and spiritual aspects. This holistic approach may not align well with the perceived impersonal nature of telemedicine consultations30.
While Singapore is a multilingual country, language proficiency and comfort with technology can vary. Older generations in the Chinese community, who may be less fluent in English and less tech-savvy, might find it challenging to use telemedicine platforms that are predominantly in English or require navigating complex technology31. Future research should delve into the diverse perspectives on telemedicine among various racial groups in Singapore to fully understand and identify any relationships that may exist between specific ethnic groups and their adherence to telemedicine. This will enhance our understanding and foster more inclusive healthcare solutions. Tailoring initiatives to address cultural perceptions of healthcare and providing information in dialects may improve adherence rates.
Notably, while a previous study demonstrated high ADA for telemedicine among patients with diabetes18, our findings indicated lower desirability scores for this group. This contrast may stem from the timing of the studies. The previous study was conducted during the peak of the COVID-19 pandemic, when telemedicine was embraced as a safer alternative, skewing the results towards higher desirability. In contrast, our study was conducted in a daily epidemiological context, providing a more realistic assessment of desirability scores. This highlights the importance of considering the broader healthcare landscape and external factors when interpreting study results and formulating telemedicine policies.
Nevertheless, our study has several limitations. Notably, the use of a non-probability, voluntary sampling method may introduce selection bias: participants who self-selected to participate may not represent the broader population accurately, limiting our findings’ generalisability. Additionally, using self-reported data introduces social desirability bias. Participants might have provided responses perceived as more socially acceptable or desirable, leading to inflated or inaccurate ADA scores. Moreover, the small sample size of 324 participants further limits our findings’ generalisability. Our study's scope is restricted to the Singaporean population, thus caution is required when applying the results to other populations. Cultural factors in a Singaporean context must be considered when interpreting the data.
Lastly, the cross-sectional study design captures data at a single point in time, making it challenging to establish causal relationships between telemedicine exposure and ADA scores. Longitudinal studies with repeated measures over time would provide more robust evidence of any temporal relationships between telemedicine adoption and the study outcomes.
Future studies could explore the role of health or digital literacy in improving participants' ability to understand telemedicine instructions, navigate virtual platforms, and engage in telemedicine consultations. A retrospective cohort study could be carried out to confirm the inverse relationship between age, lower educational levels and ADA of telemedicine.
Research could be expanded to assess the impact of telemedicine uptake on health outcomes such as blood glucose levels and quality of life. This will enable researchers to link telemedicine utilisation with specific health outcomes and identify disparities amongst sociodemographic groups. Such insights can be instrumental in designing targeted telemedicine interventions to address specific health needs.
Conclusion
Participants who are older, with lower income and education qualification demonstrated lower ADA scores. Evidently, sociodemographic factors significantly impact ADA scores. To ensure equitable access and utilisation of telemedicine, policymakers and healthcare providers should consider these factors when designing initiatives. Tailored outreach programs, digital literacy training, and culturally sensitive communication strategies can bridge the gap and make telemedicine more accessible for all.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request at saimahilal@nus.edu.sg.
References
Organization WH. Implementing telemedicine services during COVID: Guiding principles and considerations for a stepwise approach [cited 2020]. https://apps.who.int/iris/handle/10665/336862. Accessed 7 Aug 2023.
Hincapié, M. A. G. J., Gempeler, A., Piñeros, J. A., Nasner, D. & Escobar, M. F. Implementation and usefulness of telemedicine during the COVID-19 pandemic: A scoping review. J. Prim. Care Community Health 11, 2150132720980612 (2020).
Kok, T. W. K. C. S., Yau, W. K. J., Raj Kumar, P. & Chua, S. B. R. Nationwide implementation of a centralised telemedicine platform in Singapore to fight the COVID-19 pandemic. J. Telemed. Telecare https://doi.org/10.1177/1357633X221122890 (2022).
Lai, S. H. S. T. C. Telemedicine and COVID-19: Beyond just virtual consultations - the Singapore experience. Bone Jt. Open 1(6), 203–204 (2020).
Mann, D. M. C. J., Chunara, R., Testa, P. A. & Nov, O. COVID-19 transforms health care through telemedicine: Evidence from the field. J. Am. Med. Inform. Assoc. 27(7), 1132–1135 (2020).
Xu, T. P. S., Sutton, S. & Rhee, M. Telemedicine in the management of type 1 diabetes. Prev. Chronic Dis. 15, E13 (2018).
Nm, H. Benefits and drawbacks of telemedicine. J. Telemed. Telecare 11(2), 60–70 (2005).
Bhaskar, S. B. S. et al. Telemedicine as the new outpatient clinic gone digital: Position paper from the pandemic health system REsilience PROGRAM (REPROGRAM) international consortium (Part 2). Front. Public Health 8, 410 (2020).
Sayani, S. M. M., Saleh, K., Muqeet, A., Zaidi, F. & Shaikh, T. Addressing cost and time barriers in chronic disease management through telemedicine: An exploratory research in select low- and middle-income countries. Ther. Adv. Chronic Dis. 10, 2040622319891587 (2019).
Haleem, A. J. M., Singh, R. P. & Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens. Int. 2, 100117 (2021).
Nguyen, M. T. G. F. et al. Satisfaction can co-exist with hesitation: Qualitative analysis of acceptability of telemedicine among multi-lingual patients in a safety-net healthcare system during the COVID-19 pandemic. BMC Health Serv. Res. 22(1), 195 (2022).
Balestra, M. Telehealth and legal implications for nurse practitioners. J. Nurse Pract. 14(1), 33–39 (2018).
Zachrison, K. S. B. K., Hayden, E. M., Espinola, J. A. & Camargo, C. A. Jr. Understanding barriers to telemedicine implementation in rural emergency departments. Ann. Emerg. Med. 75(3), 392–399 (2020).
Sagaro, G. G. B. G. & Amenta, F. Barriers to sustainable telemedicine implementation in Ethiopia: A systematic review. Telemed. Rep. 1(1), 8–15 (2020).
Pang, N. Q. L. J., Fong, S. Y., Wong, C. Y. & Tan, K. K. Telemedicine acceptance among older adult patients with cancer: Scoping review. J. Med. Internet. Res. 24(3), e28724 (2022).
Lehoux, P. Why examining the desirability of health technology matters. Healthc. Policy 3(3), 29 (2008).
Vrijens, B. D. G. S. et al. A new taxonomy for describing and defining adherence to medications. Br. J. Clin. Pharmacol. 73(5), 691–705 (2012).
Patrascu, R. A. A. et al. Factors influencing the desirability, acceptability, and adherence of patients with diabetes to telemedicine. Medicina (Kaunas) 58(8), 997 (2022).
Batsis, J. A. M. A. et al. Feasibility and acceptability of a rural, pragmatic, telemedicine-delivered healthy lifestyle programme. Obes. Sci. Pract. 5(6), 521–530 (2019).
Department of Statistics Singapore. (2020). Census of Population 2020 Statistical Release 1: Demographic Characteristics, Education, Language and Religion.
Nadarzynski, T. B. J., Llewellyn, C., Kidsley, S. & Graham, C. A. Acceptability of artificial intelligence (AI)-enabled chatbots, video consultations and live webchats as online platforms for sexual health advice. BMJ Sex Reprod. Health 46(3), 210–217 (2020).
Harris, A. J. A. et al. Disparities in telemedicine literacy and access in the United States. Plast. Reconstr. Surg. 151(3), 677–685 (2023).
Soundararajan, A. et al. smartphone ownership, digital literacy, and the mediating role of connectedness and loneliness in improving the wellbeing among community-dwelling Singaporean older adults of low socio-economic status. PLoS ONE 18(8), e0290557 (2022).
Man, R. E. K. et al. Awareness and attitudes of elderly Southeast Asian adults towards telehealth during the COVID-19 pandemic: A qualitative study. Singap. Med. J. https://doi.org/10.4103/singaporemedj.SMJ-2022-117 (2023).
Man, R. et al. Awareness and attitudes of elderly Southeast Asian adults towards telehealth during the COVID-19 pandemic: A qualitative study. Singap. Med. J. https://doi.org/10.4103/singaporemedj.SMJ-2022-117 (2023).
Ho, V. & Merchant, R. A. The acceptability of digital technology and tele-exercise in the age of COVID-19: Cross-sectional study. JMIR Aging. 5(2), e33165. https://doi.org/10.2196/33165 (2022).
Infocomm Media Development Authority. Seniors Go Digital [Internet]. Available from: https://www.imda.gov.sg/how-we-can-help/seniors-go-digital
Lim, M. K., Sadarangani, P., Chan, H. L. & Heng, J. Y. Complementary and alternative medicine use in multiracial Singapore. Complement. Ther. Med. 13, 16–24 (2005).
Lim, J., Wong, C., Teo, T. & Ang, J. Understanding the prevalence and factors associated with the use of complementary and alternative medicine in Singapore. J. Ethnopharmacol. 182, 19–25 (2016).
Lee, G. B., Charn, T. C., Chew, Z. H. & Ng, T. P. Complementary and alternative medicine use in patients with chronic diseases in primary care is associated with perceived quality of care and cultural beliefs. Family Pract. 21(6), 654–660 (2004).
Chia, P. H., Lian, W. K. & Seow, J. E. The impact of language proficiency and technological literacy on telemedicine usage among the elderly in Singapore. J. Telemed. Telecare 26(5), 298–306 (2020).
Funding
S. Hilal was supported by National Medical Research Council Singapore, Transition Award [A-0006310-00-00], Ministry of Education, Academic Research Fund Tier 1 [A-0006106-00-00] and Absence Leave Grant [A-8000336-00-00].
Author information
Authors and Affiliations
Contributions
Jia Yang Tan, Jeremie Shun Hong Choo, Shruthi C Iyer, Beth Shi Yu Lim, Jarell Jie-Rae Tan, Joanna Min Yu Ng, and Terence Teng Yang Lian wrote the main manuscript. Saima Hilal supervised the study. The authors would like to thank the members of the Yong Loo Lin School of Medicine Community Health Project Group 2 2023/24 for their contribution to the early design of data collection for this study.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tan, J.Y., Choo, J.S.H., Iyer, S.C. et al. A cross sectional study of role of technology in health for middle-aged and older adults in Singapore. Sci Rep 14, 18645 (2024). https://doi.org/10.1038/s41598-024-68410-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-68410-x
- Springer Nature Limited