Abstract
Hydrogels are extensively explored as biomaterials for tissue scaffolds, and their controlled fabrication has been the subject of wide investigation. However, the tedious mechanical property adjusting process through formula control hindered their application for diverse tissue scaffolds. To overcome this limitation, we proposed a two-step process to realize simple adjustment of mechanical modulus over a broad range, by combining digital light processing (DLP) and post-processing steps. UV-curable hydrogels (polyacrylamide-alginate) are 3D printed via DLP, with the ability to create complex 3D patterns. Subsequent post-processing with Fe3+ ions bath induces secondary crosslinking of hydrogel scaffolds, tuning the modulus as required through soaking in solutions with different Fe3+ concentrations. This innovative two-step process offers high-precision (10 μm) and broad modulus adjusting capability (15.8–345 kPa), covering a broad range of tissues in the human body. As a practical demonstration, hydrogel scaffolds with tissue-mimicking patterns were printed for cultivating cardiac tissue and vascular scaffolds, which can effectively support tissue growth and induce tissue morphologies.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Tissue scaffold plays an important role in tissue engineering, providing structural support for the biomimetic characteristics of tissues1. The main motivation is to replicate the specific structures and mechanical environments of human tissues, thereby promoting effective tissue remodeling2. However, the morphology and modulus of soft tissues vary widely within the human body, e.g. liver (modulus < 10 kPa3,4) possesses functional hepatic lobules arranged in a radial distribution, cardiac tissue (modulus ~ 10 kPa5,6,7,8,9,10) exhibits an organized orientation, blood vessels (modulus ~ 103 kPa11) feature network-like structures. Moreover, the modulus of cardiac tissue increases with development, starting at approximately 12 kPa in the embryonic stage and reaching around 30 kPa in adulthood12. This makes the manufacturing of diverse tissue scaffolds challenging while aiming to match the complexed structural and mechanical properties.
Hydrogels find extensive applications in tissue engineering, due to their excellent properties including flexibility, stretchability, and biocompatibility13,14,15,16. UV-curable hydrogels, in particular, offer a versatile solution for creating high-resolution 3D structures through techniques like Stereolithography or Digital Light Processing (DLP)17,18,19,20,21. It is feasible to efficiently and rapidly manufacture bionic tissue scaffolds with macro-microscopic structures. For example, tissue scaffolds with structures like networked blood vessel scaffolds22,23, tendon-like scaffolds24, and irregular-shaped bone and cartilage engineering scaffolds25,26 can be manufactured using UV-curable hydrogel in DLP fabrication27. And DLP-printed hydrogel scaffolds can easily replicate the specific structures of diverse tissue.
Currently, the mechanical properties of hydrogel scaffolds can be generally modulated through UV exposure control28,29, structural design30, and formula adjustment23,31. UV energy intensity and exposure time have a pronounced effect on the mechanical behavior of hydrogels28,29. However, unavoidable scattering, transmission, and refraction of light occur during printing, resulting in varying crosslinking densities across different parts of the scaffold (where monomers are not fully crosslinked). This becomes more pronounced in scaffolds with complex structures27,29. Structural design is another important way to modify the modulus of a scaffold. Incorporating hollow structures into the scaffold reduces the overall stiffness of a sample28,30. The cells sense the local modulus of scaffolds, which indicates a structural resolution of micrometer scale is required. Such methods would greatly reduce the efficiency and raise the cost of printing32,33.
By adjusting the components or ratios in the formula, the polymer network and the modulus of the DLP-printed sample can be regulated remarkably23,31. An increase in the monomer content or the number of unsaturated bonds in the formula can raise the crosslinking density of the polymer network rapidly29,34. On the contrary, if components prone to hydrolysis are added to the polymer network, the crosslinking density of the polymer network decrease, which results in a reduction of the modulus35. The presence of additives in solid form into the polymer network will also enhance the sample modulus. The addictive and hydrogels form composite materials, and the cured sample exhibited higher modulus with increasing the additive contents36. However, scaffolds produced with the same formula have a limited modulus adjusting range, making it challenging to match the mechanical environment required by a variety of tissues. On the other hand, altering the formula reduces versability, raises printing costs, and lowers its maneuverability.
Herein, we report a two-step process to realize simple adjustment of mechanical modulus over a broad range, by combining DLP and post-processing steps. In contrast to methods that require adjustment of formulas or processes, this two-step process allows broad modulation of modulus using a single UV-curable hydrogel formula and DLP process parameters. Through this two-step process, hydrogel scaffolds with exceptional resolution, biomimetic microstructural, and adjustable modulus were fabricated. These attributes represent a distinctive advantage not attainable through other bioprinting processes. The fabricated scaffold, mirroring the morphology and modulus of native tissue, effectively induced the cultivation of well-organized, synchronized beating cardiac tissue or branching coronary artery. Importantly, this manufacturing process is user-friendly and broadly applicable to ion-crosslinked double network hydrogel systems, and is expected to provide an important method for biomimetic tissue engineering.
Experimental
Materials
Acrylamide (AAm) (Macklin, Shanghai, China) as the monomer; poly(ethylene glycol) diacrylate (PEGDA, Mw = 1000) (Macklin, Shanghai, China) as crosslinker. Sodium alginate (Alg) (Rhawn, Shanghai, China) was introduced as a second crosslinking network, Lithiumpheny-2,4,6-trimethyl-benzoylphosphinate (LAP) (Energy Chemical, Shanghai, China) photoinitiator, Tartrazine (Aladdin, Shanghai, China) as a UV absorber. FeCl3·6H2O (Acmec, Shanghai, China) was used as ionic crosslinks to adjust the modulus of the sample. Deionized water (DI water) was produced for laboratory pure water systems (Master-Q30UT, HHitech, Shanghai, China).
Preparation of UV-curable hydrogel solutions
The proposed UV-curable hydrogel formula was a mixture of AAm, PEGDA, and Alg precursors. The basic printing solution was developed with a composition of AAm: PEGDA: LAP: Tartrazine: DI water = 1: 0.03: 0.03: 0.015: 4. The hydrogel solution was prepared at five concentrations of Alg (0, 1, 2, 4, and 6% Alg/AAm ratios). Alg solution was prepared by dissolving quantitative powder in 100 g of DI water under magnetic stirring for 12 h at 35 °C. 0.75 g of LAP and 0.375 g of Tartrazine were dissolved in the Alg solution by stirring for 2 h at 25 °C. 25 g AAm and 0.75 g PEGDA were added to the above mixture solution and stirred for 5 h to obtain the desired UV-curable hydrogel solution. It is worth noting that stirring should be conducted in the dark, and the resulting hydrogel solution should be stored in a refrigerator.
Hydrogel samples manufacturing
The samples were fabricated using a 3D printer (S240, BMF Precision Tech Inc., Chong Qin, China) based on digital light processing technology, which provides a resolution of 10 μm (Fig. 1a). A 405 nm light source was used, and the light energy density was adjusted to 43.1 mW/cm2 for our experiments. The 3D digital model was sliced using CHITUBOX V1.9.4, with 10–40 μm for each layer, corresponding to an exposure time of 4–6 s.
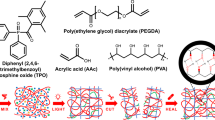
Two-step process: DLP printing and modulus adjustment. (a) Schematic diagram of top-down DLP printing. (b) Treatment of the sample in an ion bath. (c) Crosslinking process of the hydrogel solution: First step, the solution was cured under 405 nm light to form a long-chain polymer network during the DLP process, and the sample was 3D molded at this stage. Second step, the secondary crosslinking of alginate in the samples was performed using Fe3+ ion bath treatment. The sample modulus can be regulated by controlling the Fe3+ concentration.
The printed samples were immersed in a 40 wt% ethanol solution for 15 min to dissolve any hydrogel solution on the surface. All sample surface was dried using a high-pressure air gun. Then the samples were post-cured under UV light (1000 mW, 15 min). Subsequently, the samples were soaked in a corresponding concentration of Fe3+ solution for 24 h to guarantee a complete ion exchange and crosslinking with alginate in the ion bath (Fig. 1b)37. To ensure uniform crosslinking, a sufficient amount of Fe3+ ion bath solution is provided so as to maintain the stability of the ion concentration during the soaking (Fig. 1c).
Characterization of hydrogels
The rheological properties of hydrogel solutions were measured using a rotational viscometer (MCR302, Anton Paar, Graz, Austria). All measurements were performed at 25°C (except for temperature scans) and low viscosity solutions were tested using a cone-and-plate geometry of CP50-1 (cone angle: 1°, diameter: 50 mm).
The swelling behavior of hydrogel samples was evaluated using rectangular specimens measuring 16 mm × 10 mm × 2 mm. The lengthwise deformation of the samples was recorded for 7 days after crosslinking with Fe3+ at concentrations of 0, 0.005 M, 0.01 M, 0.02 M, and 1 M, for alginate content of 0 wt%, 1 wt%, 2 wt%, 4 wt%, and 6 wt% (Alg/AAm).
At room temperature, the mechanical properties of hydrogel samples were measured using an electromechanical universal testing machine (E43, Meters Industrial Systems, USA) @2 mm/min with a 50 N load cell. Each sample was tested and recorded with a dial caliper with a precision of 0.01 mm. Unless otherwise specified, the hydrogel samples were subjected to ion bath treatment for 1 day and soaked in DI water for 7 days. According to the diffusion formula of ions in an aqueous solution, prolonged soaking allows for the uniform diffusion of Fe3+ into the hydrogel samples37. The structures of testing models and hydrogel scaffolds were characterized and measured using a digital microscope (DSX1000, Olympus Corporation, Japan).
After ion bath treatment, PAAm-Alg hydrogels were cut into equal-sized pieces (~ 6 mm × 6 mm × 3 mm) for biocompatibility testing. After rinsing thoroughly with phosphate-buffered saline (PBS), the hydrogel samples were incubated in quantitative DMEM medium (the ratio of surface area to medium volume is 3 cm2/mL) for 72 h @37 °C. The biocompatibility was tested on fibroblast cells cultured in the extract of hydrogels using Enzyme Markers (K3 Touch, Thermo Fisher, USA), and a CCK-8 kit (Shanghai Beyoncé Bio, C0043) after 72 h.
Generation of HiPSC derived cardiomyocytes and endothelial cells
HiPSC (Beijing Cel-lapy Biological Technology Co. Ltd., Beijing, China) were cultured on matrigel-coated (0.15%, Corning, 356234) six-well plates in StemFlexTM medium (Gibco, A3349401) at 37 °C in 5% CO2. The hiPSCs were labeled with green fluorescent by introducing an EGFP expressional element in an AAVS1 locus. HiPSC-CMs were cultured according to previous publications38,39.
Human Coronary Artery Endothelial Cells (HCAEC) (FengHuiShengWu, CL0117) were cultivated as adherent cells in Endothelial Cell Medium (ECM, Sciencell, 1001). When the cell confluence reached 80%, a 0.05% trypsin solution was employed for a digestion period of 8–10 min. To halt the enzymatic digestion, a serum-containing culture medium was used. Subsequently, the cells were gently detached using a pipette, transferred to a centrifuge tube, and subjected to centrifugation at 200g for 5 min. After discarding the supernatant, the cell pellet was resuspended in ECM to achieve a concentration of 5 × 106/mL and then seeded onto the hydrogel substrates.
Seeding and culture of the cardiomyocytes and endothelial cells
All samples underwent sterilization through γ-ray irradiation. The hydrogel scaffolds were immersed in the culture medium three consecutive times, with each immersion lasting no less than 3 h. Subsequently, the samples were immersed in the culture medium for more than 72 h and stored in a refrigerator. Before cell seeding, all hydrogel scaffolds were coated with porcine gelatin (Sigma, V900863) at 2% w/v in phosphate-buffered saline (PBS) for 2 days @37 °C.
Cardiac tissue scaffolds: a cell suspension was prepared by mixing cardiomyocytes and fibroblasts with a ratio of 2:1. 500 μL cell suspension (3 × 105/well) was seeded on a hydrogel scaffold, and all samples were incubated for 12 h @37 °C to allow cell attachment. Subsequently, the devices were cultured in the RPMI 1640 Medium with 3% KnockOut Serum Replacement @37 °C, and 5% CO2 every 2–3 days changes of media for the duration of the experiment.
Vasculature-like hydrogel scaffolds: 15 μL of endothelial cell suspension (7.5 × 104/well) were pipetted onto the central groove of the samples. Culture medium was added 4 h later. For immunofluorescence staining, cells were fixed with 4% paraformaldehyde for 20 min, followed by permeabilization with 0.25% Triton-X 100 (Sigma-Aldrich) in PBS for 20 min at room temperature.
The morphology of tissues cultured on the scaffold was recorded using a fluorescence microscope (MF52-N, Mshot, China). Furthermore, rhythmic contractions of tissue were induced using a custom-made electrical stimulation device, employing a pair of electrodes to generate a uniform electric field. Unless otherwise specified, the electrical field strength applied to the cardiac tissue by the stimulation device was set at 8 V/cm. The cardiac tissue contractions were recorded through video documentation.
Statistical analysis
The data were indicated by the mean ± standard deviation (SD). We conducted swelling, surface morphology, and mechanical testing calculations for each experimental group at least three times. We used OriginPro2017 software for statistical analysis was applied to compare the mean values within each group. The data of Stress–strain curves in the paper has undergone smoothing processing.
Ethical approval
The cardiomyocytes and endothelial cells used in the study were commercially cells. All cells experiment in the manuscript were approved by the Declaration of Helsinki guidelines.
Results and discussions
Printability and swelling behaviors of the hydrogel formula
To meet the desired printability and swelling behaviors, the AAm-Alg hydrogel formula was carefully designed, as shown in Fig. 1. AAm has been extensively studied as a UV-curable hydrogel solution. To minimize the toxicity of printed samples, the hydrogel formula was improved by using LAP and Tartrazine, which have superior biocompatibility. And PEGDA (Mw = 1000) was added as a crosslinker to form rigid chains connecting the flexible chains of polyacrylamide (PAAm), enhancing the mechanical properties of the polymer network40,41. Among the variety of choices, a formable formula (AAm: PEGDA: LAP: Tartrazine: DI water = 1: 0.03: 0.03: 0.015: 4) was selected.
A sufficient fluidity of the UV-curable formula is crucial to reduce the difficulty of the recoating process in DLP printing, thereby improving both the printing efficiency and quality. A hydrogel solution with low viscosity enhances printability, including continuity and thickness control42,43. Samples printed with high viscosity hydrogel solution are prone to defects in structures44,45. However, to create a dual-network hydrogel with an adjustable modulus, Alg was added into the formula. The addition of alginate increased the viscosity and brought distinct non-Newtonian fluid behavior to the hydrogel solution, as shown in Fig. 2a. At a low shear rate of 10 s−1, the viscosity of the hydrogel solution (0–6 wt% Alg/AAm) increased from 3.58 mPa s to 168 mPa s (Fig. 2a). Besides, the rheological properties of this formula are temperature-sensitive. In a temperature scan ranging from 25 to 60 °C, the 4 wt% solution viscosity decreased from 61.4 mPa s to 26.4 mPa s @50 s−1 (Supplementary Fig. S1).
Viscosity and swelling properties of hydrogel. (a) Viscosity curves of hydrogel solutions with Alg/AAm ratios of 0–6%. (b) Swelling properties of cured hydrogel samples with different Alg/AAm ratios subjected to 1 M Fe3+ crosslinking (dashed) or without crosslinking (solid), compared by the lengthwise deformation of the testing samples. (c) The swelling of a 4% Alg/AAm ‘Hydrogel Ruler’ in different conditions.
In addition, the swelling behaviors of hydrogels are closely related to Alg. Cured PAAm-Alg hydrogels exhibit hydrophilicity due to the abundant hydrophilic functional groups in the polymer chains. Therefore, those cured samples swelled at immersion in solutions, resulting in undesirable shape changes46. Excessive deformation is not conducive to printing scaffolds with high resolution. Advanced dual-network hydrogel formula design helps the swelling control. The deformation extent of 0–6 wt% (Alg/AAm) UV-curable hydrogel samples in DI water, 0.005 M, 0.01 M, 0.02 M, and 1 M Fe3+ environments was recorded for 7 days. At the same Alg content, the samples treated in different ion baths exhibit similar deformations (Supplementary Fig. S2). However, the swelling deformations ratio of the samples decreased with a higher content of alginate in the same ion bath (Fig. 2b). Notably, the addition of alginate created a double network hydrogel that limited swelling even in DI water without ionic crosslinking. After 1 M Fe3+ bath treatment, the swelling deformation of 4 wt% and 6 wt% samples (~ 130%, and ~ 120%, respectively) were comparable and acceptable. Ultimately, balancing the viscosity and swelling requirements of the formula, a UV-curable hydrogel solution containing 4 wt% alginate was selected in this study. To visualize the swelling deformation of hydrogel samples, a 10 mm hydrogel ruler (4 wt% Alg/AAm) was printed. In Fig. 2c, the state of the hydrogel ruler was shown directly after printing, either with 1 M Fe3+ bath treatment, or after immersion in DI water. The ratio of their length to width was nearly equal (2.67, 2.53, 2.67 respectively). It could be confirmed that, after swelling, the manufactured hydrogel samples undergo consistent deformation on a macroscopic scale.
It is worth mentioning that the cost-effective UV-curable hydrogel (priced at approximately $10 for 100 g solution) exclusively incorporates readily accessible commercial-grade raw materials, thereby diminishing the entry threshold for 3D bioprinting.
Optimization of DLP parameters
To achieve high-resolution printing, the optimal printing parameters for the UV-curable hydrogel solution were investigated. Based on the Beer-Lambert law, the curing behavior of photocurable inks can be described by Jacobs equation43,47:
where Cd is the depth of cure at a given exposure E, Dp is the transmission depth of UV-curable solutions, and Ec is the critical exposure intensity. Printing hollow structures with a transverse channel using different energy densities inputted on the top layer was performed (Supplementary Fig. S3). The thickness of the top layer film of the channel was measured to characterize the cured depth of the hydrogel solution, and the relationship between the cured depth and the energy density was fitted (Fig. 3a, Dp = 44.4 μm, ln(Ec) = 4.97 mJ/cm2). According to this model, the ideal exposure time for 10–40 μm thick film is 4–6 s.
Utilizing these optimized process parameters, micro lines with a width ranging from 10–50 μm (Fig. 3b) were printed, achieving the upper limit resolution of the DLP printer. The application of a higher precision UV source could further improve the resolution. Furthermore, hydrogel samples with complex 2D/3D patterns were printed, including the Xiamen University emblem (Fig. 3c) and a 3D octopus (Fig. 3d), which reproduced the details of the circular design and characters with fidelity.
To further validate the printability of the material, a flexible sample containing double-helix internal channels was printed with a diameter of 1 mm (Fig. 3e). The two channels were infused with different liquids, which demonstrated smooth flow without any obstruction (Supplementary Video S1). These features endow this hydrogel formula with the capability to manufacture integrated flexible and complex 3D microfluidic chips.
Mechanical properties of the hydrogels with adjustable modulus
Alginate in the hydrogel formula formed an adjustable ion crosslinking network in the environment of multivalent cations. Different multivalent ions exhibited varying effects on crosslinking alginate, such as Na+, Ca2+, Sr2+, Ba2+, Al3+, or Fe3+37,48. Besides, the concentration of the cations was also related to the crosslinking density of the polymer chains49. By controlling the Fe3+ concentration in the ion bath, the crosslinking density of the PAAm-Alg double network hydrogel was manipulated, which allowed Young's modulus adjustment to hydrogel samples. After Fe3+ ion bath treatment, the color of the samples intensifies with the rising Fe3+ concentrations.
The introduction of Alg into the hydrogel formula led to a subtle increase of modulus in untreated samples pre- and post-swelling (Fig. 4b), due to the physical double network hydrogels of PAAm-Alg50. Following the Fe3+ ion bath treatment, the hydrogel modulus exhibited a proportional increase with the ascending ion concentration, ranging from 15.8 to 345 kPa (Fig. 4a). Such a large modulus adjustable range allows the printed hydrogel scaffold to simulate the modulus of almost all human soft tissues. As shown in Fig. 4c and Supplementary Fig. S4, the elastic deformation portion of the stress–strain curves in Fig. 4a was used to calculate Young’s modulus of hydrogel samples, revealing its relationship with the Fe3+ concentration in the ion bath. The modulus increased rapidly and proportionally with the ion concentration, which indicated a rise in crosslinking density. However, with further increasing the Fe3+ ion concentration (> 0.1 M), the modulus value gradually flatten. This deceleration was attributed to a reduction in ion crosslinking sites within the alginate segments. Cyclic stretching tests on hydrogel samples (0.1 M Fe3+) showed that the stress–strain curves of the samples had good repeatability under 15–30% strain (Fig. 4d). However, when producing higher modulus hydrogel samples, the enhancement becomes significantly limited after exposure to higher concentration Fe3+ ion baths using the current hydrogel formula.
Mechanical properties of Fe3+-treated PAAm-Alg hydrogel samples. (a) Stress-strain curves of hydrogel samples treated with 0-1 M Fe3+ ion bath treatment. (b) Stress-strain curves of untreated (0, 4 wt% Alg) hydrogel samples, where the solid line represents the sample without swelling and exhibits significantly higher fracture strain than the swollen samples. (c) Relationship between Fe3+ concentration in the ion bath and the Young's modulus of the treated samples. (d) Cyclic tensile testing (with 15%, 20%, 25%, and 30% strain) of hydrogel samples treated with 0.1 M ion bath, with the top left inset showing the sample after 100 cycles of 30% strain.
Patterned tissue induced by hydrogel scaffolds
Various soft tissues within the human body exhibit inherent orientations, such as the organization of cardiac tissue and the intricate patterns in vascular networks. Utilizing patterned hydrogel scaffolds offers a promising method for inducing well-organized or patterned tissue growth. The cell viabilities of hydrogels crosslinked with 0 M and 1 M Fe3+ were 1.01 and 0.98, as shown in Supplementary Fig. S6, compared to the control group, indicating no obvious toxicity. However, the surface of PAAm-Alg hydrogel samples lacks protein segments that facilitate cell adhesion. To improve cell adhesion to the hydrogel scaffolds, it is necessary to immerse the printed scaffolds in a porcine gelatin solution.
Cardiac tissue scaffolds with periodic H-shaped grooves (width of 100 μm, depth of 200 μm, gap of 110 μm) were manufactured. Upon immersion in DI water, the printed H-shaped grooves experienced controlled expansion. To facilitate communication between induced cardiac tissues within each groove, additional vertical grooves were incorporated into the H-shaped grooves (Fig. 5a,c). This design allowed the seeding of cells onto the hydrogel scaffold, inducing the formation of a cohesive and organized tissue. Cardiac tissue is characterized by its softness, with a modulus of ~ 10 kPa5,6,7,8,9,10. Therefore, the cardiac tissue scaffold was prepared without Fe3+ bath treatment to maintain a minimum modulus of ~ 16 kPa. A mixed suspension of self-fluorescent cardiomyocyte and fibroblast cell (2:1) was seeded onto the flexible scaffolds. Due to the gravity, a considerable number of cells were settled down and distributed within the grooves. Cardiomyocytes gradually migrated and aggregated, forming organized and continuous tissue (Fig. 5a). As shown in Fig. 5d, cardiomyocytes transitioned from an initial spherical shape to an organized tissue structure induced by H-shaped grooves. The tissue in different lines was connected through the horizontal connections. Therefore, an organized mesh-like tissue was formed through topographical constraint. The analysis of tissue orientation from 0 to 72 h (Supplementary Fig. S7a) reveals that, during the 0–48 h culture period, cardiomyocytes gradually aligned under the induction of H-shaped grooves. Cells grew across the grooves in 72 h, forming a continuous cardiac tissue.
Fluorescent cardiomyocytes were cultured on cardiac tissue scaffolds. (a) Schematic illustration of the cultivation process on the scaffold with H-shaped grooves: (i) Cell seeding in H-shaped grooves, (ii) Induction of cardiac tissue by grooves. (b) Schematic illustration of cultivation process on the flat substrate: (i) Cell seeding on a flat substrate, (ii) Formation of cardiac tissue clusters. (c) Cardiac tissue hydrogel scaffold with H-shaped grooves, images of the printed sample and the swollen scaffold. and (e) flat substrates. Observing cardiac tissue cultivates on (d) scaffolds with H-shaped grooves and (f) flat substrates at 0, 4, 8, 24, 48, and 72 h reveals distinct patterns. In the H-shaped grooves, tissues were induced to form an organized sheet. On the flat substrate, cardiomyocytes gradually aggregate, forming noticeable boundaries between clusters.
Comparatively, cardiac tissue cultured on a flat substrate (Fig. 5e) failed to form an organized structure and tended to grow in clusters (Fig. 5b,f). As shown in Supplementary Fig. S7b, the cardiac tissue exhibits an overall disordered state, with no distinct peaks indicating a predominant orientation. Those cells underwent arbitrary clustering, displaying uncontrollable boundaries between tissue clusters, which is more apparent in the stained images (Supplementary Fig. S8). The organized cardiac tissue could be driven to contract under an electric field generated by the electrical stimulation device. Under a pulse field with frequencies ranging from 0.5 to 1.5 Hz, the cardiac tissue exhibited synchronous contractions that followed the applied frequency (Supplementary Video S2). However, at 2 Hz, although the tissue demonstrated contractions, it failed to keep pace with the frequency of the electric field.
Compared with cardiac tissue, blood vessels possess a higher modulus and exhibit a more intricate macroscopic structure. Vasculature-like hydrogel scaffolds were printed and treated with 1 M Fe3+ to obtain Young's modulus of ~ 345 MPa, mimicking that of native blood vessels as shown in Fig. 6a. The vascular tissue scaffold was designed with semi-open channels of varying diameters. After swelling, the diameter raised from the designed 1.2, 0.3, and 0.1 mm to 1.52, 0.47, and 0.16 mm, respectively. HCAECs were seeded onto the scaffold, forming a semi-open vascular network. Tissues grown on scaffolds exhibited apparent vascular morphological features. Upon staining HCAECs across the entire scaffold, it was evident that HCAECs could be well-distributed on the scaffold and microchannels (Fig. 6b–d). Within those 0.16 mm grooves (Fig. 6e), HCAECs exhibited distinctive vascular pattern. Conversely, endothelial cells cultured on a substrate devoid of grooves did not exhibit any noticeable pattern (Fig. 6f).
HCAECs on the vasculature-like hydrogel scaffold were stained. (a) The Vasculature-like hydrogel scaffold, the crosslinked sample (above) and the printed sample (below). (b–e) HCAECs seeded onto the scaffold, growing along the grooves to form vasculature-like structures. (b) grooves with width of 1.52 mm, (c) grooves with width of 0.47 mm, (d) grooves with width of 0.16 mm. (e) HCAECs were seeded at the bottom of the grooves, inducing tissue formation. (f) HCAECs cultured on a flat substrate exhibited disorganized distribution.
Conclusions
In conclusion, a simple and versatile two-step process, combining DLP and post-treatment. Ion bath treatment is performed after the DLP printing. Using a single AAm-Alg hydrogel formula, hydrogel structures with biocompatible, high-resolution, and adjustable modulus can be fabricated. This two-step process makes bioprinting more cost-effective and straightforward. The UV-curable hydrogel solution exhibited excellent printability, achieving a printing feature of 10 μm (limited by the resolution of the light source) that resembles the characteristic morphology of biological tissues. The ion bath treatment enables a wide range of modulus adjustments (15.83–344.67 kPa) in a simple way, with the ability to customize the modulus of hydrogel samples. Patterned hydrogel scaffolds with low or high moduli were respectively designed and manufactured for cultivating cardiac and vascular tissue. The cultivated tissues were induced by the scaffold morphology, even resembling a biomimetic multilevel vascular network. The cultured organized cardiac tissue exhibits synchronous beating under electrical stimulation. We believe that this two-step process provides an easily feasible method for manufacturing tailored scaffolds for a broad range of tissues in the human body.
Data availability
All data analyzed during this study are included in this published article.
References
Zhang, F. & King, M. W. Biodegradable polymers as the pivotal player in the design of tissue engineering scaffolds. Adv. Healthc. Mater. https://doi.org/10.1002/adhm.201901358 (2020).
Calo, E. & Khutoryanskiy, V. V. Biomedical applications of hydrogels: A review of patents and commercial products. Eur. Polym. J. 65, 252–267. https://doi.org/10.1016/j.eurpolymj.2014.11.024 (2015).
Guimaraes, C. F., Gasperini, L., Marques, A. P. & Reis, R. L. The stiffness of living tissues and its implications for tissue engineering. Nat. Rev. Mater. 5, 351–370. https://doi.org/10.1038/s41578-019-0169-1 (2020).
Jiang, X., Li, L. & Xue, H.-Y. The impact of body position and exercise on the measurement of liver Young’s modulus by real-time shear wave elastography. Technol. Health Care 30, 445–454. https://doi.org/10.3233/thc-213218 (2022).
Singh, G. & Chanda, A. Mechanical properties of whole-body soft human tissues: A review. Biomed. Mater. https://doi.org/10.1088/1748-605X/ac2b7a (2021).
Bhana, B. et al. Influence of substrate stiffness on the phenotype of heart cells. Biotechnol. Bioeng. 105, 1148–1160. https://doi.org/10.1002/bit.22647 (2010).
Bajaj, P., Tang, X., Saif, T. A. & Bashir, R. Stiffness of the substrate influences the phenotype of embryonic chicken cardiac myocytes. J. Biomed. Mater. Res. Part A 95A, 1261–1269. https://doi.org/10.1002/jbm.a.32951 (2010).
Shi, X. et al. Elasticity of cardiac cells on the polymer substrates with different stiffness: An atomic force microscopy study. PCCP 13, 7540–7545. https://doi.org/10.1039/c1cp20154a (2011).
Forte, G. et al. Substrate stiffness modulates gene expression and phenotype in neonatal cardiomyocytes in vitro. Tissue Eng. Part A 18, 1837–1848. https://doi.org/10.1089/ten.tea.2011.0707 (2012).
Tallawi, M., Rai, R., Boccaccini, A. R. & Aifantis, K. E. Effect of substrate mechanics on cardiomyocyte maturation and growth. Tissue Eng. Part B Rev. 21, 157–165. https://doi.org/10.1089/ten.teb.2014.0383 (2015).
Camasao, D. B. & Mantovani, D. The mechanical characterization of blood vessels and their substitutes in the continuous quest for physiological-relevant performances. A critical review. Mater. Today Bio. https://doi.org/10.1016/j.mtbio.2021.100106 (2021).
Heras-Bautista, C. O. et al. Cardiomyocytes facing fibrotic conditions re-express extracellular matrix transcripts. Acta Biomater. 89, 180–192. https://doi.org/10.1016/j.actbio.2019.03.017 (2019).
Yar, M. et al. Triethyl orthoformate mediated a novel crosslinking method for the preparation of hydrogels for tissue engineering applications: Characterization and in vitro cytocompatibility analysis. Mater. Sci. Eng. C-Mater. Biol. Appl. 56, 154–164. https://doi.org/10.1016/j.msec.2015.06.021 (2015).
Rizwan, M. et al. pH sensitive hydrogels in drug delivery: Brief history, properties, swelling, and release mechanism, material selection and applications. Polymers. https://doi.org/10.3390/polym9040137 (2017).
Hu, M. et al. Low chemically cross-linked PAM/C-dot hydrogel with robustness and superstretchability in both as-prepared and swelling equilibrium states. Macromolecules 49, 3174–3183. https://doi.org/10.1021/acs.macromol.5b02352 (2016).
Hu, L. et al. Hydrogel-based flexible electronics. Adv. Mater. https://doi.org/10.1002/adma.202205326 (2023).
Li, J., Wu, C., Chu, P. K. & Gelinsky, M. 3D printing of hydrogels: Rational design strategies and emerging biomedical applications. Mater. Sci. Eng. R Rep. https://doi.org/10.1016/j.mser.2020.100543 (2020).
Gao, Q. et al. 3D printing of complex GelMA-based scaffolds with nanoclay. Biofabrication https://doi.org/10.1088/1758-5090/ab0cf6 (2019).
Gao, Q., He, Y., Fu, J.-Z., Liu, A. & Ma, L. Coaxial nozzle-assisted 3D bioprinting with built-in microchannels for nutrients delivery. Biomaterials 61, 203–215. https://doi.org/10.1016/j.biomaterials.2015.05.031 (2015).
Zhao, H. et al. Airflow-assisted 3D bioprinting of human heterogeneous microspheroidal organoids with microfluidic nozzle. Small https://doi.org/10.1002/smll.201802630 (2018).
Sun, Y. et al. Modeling the printability of photocuring and strength adjustable hydrogel bioink during projection-based 3D bioprinting. Biofabrication https://doi.org/10.1088/1758-5090/aba413 (2021).
Kim, S. H. et al. Precisely printable and biocompatible silk fibroin bioink for digital light processing 3D printing. Nat. Commun. https://doi.org/10.1038/s41467-018-03759-y (2018).
He, Y. et al. A photocurable hybrid chitosan/acrylamide bioink for DLP based 3D bioprinting. Mater. Des. https://doi.org/10.1016/j.matdes.2021.109588 (2021).
He, Y. et al. A universal and simple method to obtain hydrogels with combined extreme mechanical properties and their application as tendon substitutes. ACS Appl. Mater. Interfaces 14, 54215–54224. https://doi.org/10.1021/acsami.2c16198 (2022).
Lim, K. S. et al. Bio-resin for high resolution lithography-based biofabrication of complex cell-laden constructs. Biofabrication. https://doi.org/10.1088/1758-5090/aac00c (2018).
Tao, J. et al. DLP-based bioprinting of void-forming hydrogels for enhanced stem-cell-mediated bone regeneration. Mater. Today Bio https://doi.org/10.1016/j.mtbio.2022.100487 (2022).
Li, Y. et al. High-fidelity and high-efficiency additive manufacturing using tunable pre-curing digital light processing. Addit. Manuf. https://doi.org/10.1016/j.addma.2019.100889 (2019).
Xue, D., Zhang, J., Wang, Y. & Mei, D. Digital light processing-based 3D printing of cell-seeding hydrogel scaffolds with regionally varied stiffness. ACS Biomater. Sci. Eng. 5, 4825–4833. https://doi.org/10.1021/acsbiomaterials.9b00696 (2019).
Bhusal, A. et al. Multi-material digital light processing bioprinting of hydrogel-based microfluidic chips. Biofabrication https://doi.org/10.1088/1758-5090/ac2d78 (2022).
Zhang, Y. S. et al. Bioprinting 3D microfibrous scaffolds for engineering endothelialized myocardium and heart-on-a-chip. Biomaterials 110, 45–59. https://doi.org/10.1016/j.biomaterials.2016.09.003 (2016).
Luo, F. et al. Tough polyion-complex hydrogels from soft to stiff controlled by monomer structure. Polymer 116, 487–497. https://doi.org/10.1016/j.polymer.2017.02.042 (2017).
Yamada, S., Pokutta, S., Drees, F., Weis, W. I. & Nelson, W. J. Deconstructing the cadherin-catenin-actin complex. Cell 123, 889–901. https://doi.org/10.1016/j.cell.2005.09.020 (2005).
Elsdale, T. & Bard, J. Collagen substrata for studies on cell behavior. J. Cell Biol. 54, 626–637 (1972).
Shen, Y. et al. DLP printing photocurable chitosan to build bio-constructs for tissue engineering. Carbohydr. Polym. https://doi.org/10.1016/j.carbpol.2020.115970 (2020).
Galarraga, J. H., Dhand, A. P., Enzmann, B. P. & Burdick, J. A. Synthesis, characterization, and digital light processing of a hydrolytically degradable hyaluronic acid hydrogel. Biomacromolecules 24, 413–425. https://doi.org/10.1021/acs.biomac.2c01218 (2023).
Xie, X. et al. Microtissue-based bioink as a chondrocyte microshelter for DLP bioprinting. Adv. Healthc. Mater. https://doi.org/10.1002/adhm.202201877 (2022).
Yang, C. H. et al. Strengthening alginate/polyacrylamide hydrogels using various multivalent cations. ACS Appl. Mater. Interfaces 5, 10418–10422. https://doi.org/10.1021/am403966x (2013).
Lin, B. et al. Culture in glucose-depleted medium supplemented with fatty acid and 3,3 ’, 5-triiodo-L-thyronine facilitates purification and maturation of human pluripotent stem cell-derived cardiomyocytes. Front. Endocrinol. (Lausanne). https://doi.org/10.3389/fendo.2017.00253 (2017).
Liu, L. et al. Integrated manufacturing of suspended and aligned nanofibrous scaffold for structural maturation and synchronous contraction of HiPSC-derived cardiomyocytes. Bioengineering-Basel. https://doi.org/10.3390/bioengineering10060702 (2023).
Elbarbary, A. M., Abd El-Rehim, H. A., El-Sawy, N. M., Hegazy, E. S. A. & Soliman, E. S. A. Radiation induced crosslinking of polyacrylamide incorporated low molecular weights natural polymers for possible use in the agricultural applications. Carbohydr. Polym. 176, 19–28. https://doi.org/10.1016/j.carbpol.2017.08.050 (2017).
Cakmak, B., Saglam-Metiner, P., Beceren, G., Zhang, Y. S. & Yesil-Celiktas, O. A 3D in vitro co-culture model for evaluating biomaterial-mediated modulation of foreign-body responses. Bio-Des. Manuf. 5, 465–480. https://doi.org/10.1007/s42242-022-00198-z (2022).
Luo, Y., Le Fer, G., Dean, D. & Becker, M. L. 3D printing of poly(propylene fumarate) oligomers: Evaluation of resin viscosity, printing characteristics and mechanical properties. Biomacromolecules 20, 1699–1708. https://doi.org/10.1021/acs.biomac.9b00076 (2019).
Vazquez-Martel, C., Becker, L., Liebig, W. V., Elsner, P. & Blasco, E. Vegetable oils as sustainable inks for additive manufacturing: A comparative study. ACS Sustain. Chem. Eng. 9, 16840–16848. https://doi.org/10.1021/acssuschemeng.1c06784 (2021).
Choi, J.-W. et al. Fabrication of 3D biocompatible/biodegradable micro-scaffolds using dynamic mask projection microstereolithography. J. Mater. Process. Technol. 209, 5494–5503. https://doi.org/10.1016/j.jmatprotec.2009.05.004 (2009).
Lee, K.-W., Wang, S., Yaszemski, M. J. & Lu, L. Physical properties and cellular responses to crosslinkable poly(propylene fumarate)/hydroxyapatite nanocomposites. Biomaterials 29, 2839–2848. https://doi.org/10.1016/j.biomaterials.2008.03.030 (2008).
Li, X. et al. 3D printing of flexible liquid sensor based on swelling behavior of hydrogel with carbon nanotubes. Adv. Mater. Technol. https://doi.org/10.1002/admt.201800476 (2019).
Li, Z. et al. Additive manufacturing of lightweight and high-strength polymer-derived SiOC ceramics. Virtual Phys. Prototyp. 15, 163–177. https://doi.org/10.1080/17452759.2019.1710919 (2020).
Yang, C. et al. Strengthening alginate/polyacrylamide hydrogels using various multivalent cations. ACS Appl. Mater. Interfaces 5, 13484–13484. https://doi.org/10.1021/am4052443 (2013).
Giron-Hernandez, J., Gentile, P. & Benlloch-Tinoco, M. Impact of heterogeneously crosslinked calcium alginate networks on the encapsulation of beta-carotene-loaded beads. Carbohydr. Polym. https://doi.org/10.1016/j.carbpol.2021.118429 (2021).
Xu, X., Jerca, V. V. & Hoogenboom, R. Bioinspired double network hydrogels: From covalent double network hydrogels via hybrid double network hydrogels to physical double network hydrogels. Mater. Horizons 8, 1173–1188. https://doi.org/10.1039/d0mh01514h (2021).
Acknowledgements
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publicaiton of this article: This work was supported by the National Natural Science Foundation of China (No. U2005214) and the National Key Research and Development Program of China (2022YFB4600600).
Author information
Authors and Affiliations
Contributions
F.X.: conceptualization, methodology, data analysis and writing (original draft). H.J., H.W. and A.J.: investigation, validation and data analysis. B.Q., L.L. and Q.G.: validation and data analysis. B.L., W.K.: investigation and data analysis. S.C., and D.S.: conceptualization, writing (review and editing) and funding acquisition.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xu, F., Jin, H., Wu, H. et al. Digital light processing printed hydrogel scaffolds with adjustable modulus. Sci Rep 14, 15695 (2024). https://doi.org/10.1038/s41598-024-66507-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-66507-x
- Springer Nature Limited