Abstract
The emergence of drug-resistant Mycobacterium tuberculosis strains is a threat to global health necessitating the discovery of novel chemotherapeutic agents. Natural products drug discovery, which previously led to the discovery of rifamycins, is a valuable approach in this endeavor. Against this backdrop, we set out to investigate the in vitro antimycobacterial properties of medicinal plants from Ghana and South Africa, evaluating 36 extracts and their 252 corresponding solid phase extraction (SPE) generated fractions primarily against the non-pathogenic Mycobacterium smegmatis and Mycobacterium aurum species. The most potent fraction was further evaluated in vitro against infectious M. tuberculosis strain. Crinum asiaticum (bulb) (Amaryllidaceae) emerged as the most potent plant species with specific fractions showing exceptional, near equipotent activity against the non-pathogenic Mycobacterium species (0.39 µg/ml ≤ MIC ≤ 25 µg/ml) with one fraction being moderately active (MIC = 32.6 µg/ml) against M. tuberculosis. Metabolomic analysis led to the identification of eight compounds predicted to be active against M. smegmatis and M. aurum. In conclusion, from our comprehensive study, we generated data which provided an insight into the antimycobacterial properties of Ghanaian and South African plants. Future work will be focused on the isolation and evaluation of the compounds predicted to be active.
Similar content being viewed by others
Introduction
Tuberculosis, an ancient infectious bacterial disease mainly caused by Mycobacterium tuberculosis, remains a major global health conundrum with one third of the world latently infected1. Globally, according to the World Health Organisation (WHO), 10.6 million new cases of tuberculosis were reported in 20222. Unfortunately, 1.3 million fatalities caused by this respiratory infectious disease were recorded in this period, making tuberculosis one of the leading causes of mortality in the world2. The WHO regions with the highest burden of this disease in 2022 were South-East Asia (46%), Africa (23%) and the Western Pacific (18%)2. The WHO African region was particularly affected by tuberculosis with the greatest number of representatives, ca. 47%, amongst the 30 high-burden tuberculosis countries in 2022. Moreover, three African countries, including South Africa, were amongst the top eight countries with the highest incidence rates of tuberculosis in the world2.
The fight against tuberculosis is currently being incapacitated by the emergence and spread of drug-resistant M. tuberculosis strains. In 2022 there were 410 000 incident cases of multidrug-resistant (MDR) and rifampicin-resistant tuberculosis2. Drug-resistant tuberculosis is often immensely challenging to cure, requiring an extended period and yet having low treatment success rates3. Furthermore, compared to drug-susceptible tuberculosis, MDR and extremely drug-resistant tuberculosis (XDR) are more expensive to treat. For example, in the United States of America it costs, per patient, US$ 17,000 to treat the conventional drug-susceptible tuberculosis while MDR and XDR cost US$ 134 000 and US$ 430 000, respectively4. An additional challenge with drug-resistant tuberculosis is that the second-line treatment regimen used for its treatment has severe adverse effects to patients including permanent hearing loss4. South Africa is one of the most burdened by this drug-resistant tuberculosis phenomenon. The prevalence of MDR tuberculosis in South Africa has previously been found to be 3.4% and 7% amongst new and retreatment cases of tuberculosis, respectively5. The WHO recommended a first-line treatment regimen for tuberculosis consisting of a rifamycin, isoniazid, pyrazinamide, and ethambutol. In their comprehensive study carried out between 2012 and 2014, Ismail et al.6 found prevalence of resistance to rifampicin, isoniazid, pyrazinamide and ethambutol to be 4.6%, > 5%, 44.7% and 59.1% amongst MDR tuberculosis cases, respectively6. This is a precarious challenge posing a significant threat to global health which demands urgent attention. One way of addressing this is by the expeditious discovery and development of effective, affordable, and safe novel antimycobacterial chemotypes.
Natural products have previously served as an indispensable source of effective novel pharmaceutical agents including those used for the treatment of tuberculosis7. Microbial derived natural products have been the most crucial in this regard8. The most prolific class of microbial derived antibiotics in the battle against tuberculosis have been rifamycins, including rifampicin and rifapentine8. Rifamycins were originally isolated from the bacterium Amycolatopsis rifamycinica9. The rifamycins are an integral component of the first-line treatment regimen for tuberculosis10. Other noteworthy microbial derived tuberculosis antibiotics include the aminoglycoside kanamycin, originally isolated from Streptomyces kanamyceticus, and its derivative amikacin8. Both kanamycin and amikacin are, unfortunately, ototoxic11. Streptomycin, first isolated from Streptomyces griseus, was the first ever aminoglycoside to have been discovered. It was also the first ever antibiotic that was used for the treatment of tuberculosis, and currently constitutes the second-line regimen artillery used for treatment of MDR tuberculosis10,12. While spectinomycin, originally isolated from S. spectabilis, has marginal activity against M. tuberculosis, its semisynthetic derivatives, the spectinamides, have shown remarkable potency against both the drug-susceptible and MDR tuberculosis in vitro and in vivo13,14.
Plants have played a low-key role in Western medicine for the treatment of tuberculosis. However, it’s worth noting that pyrazinamide is an analogue of nicotinamide, a vitamin which occurs across different natural sources including vegetables15. Plants have been used in Eastern medicine for the treatment of tuberculosis, particularly in China, for thousands of years16. Different compounds including baicalin, and tuberostemonine, have been identified as active ingredients in plants16,17. Currently, some Traditional Chinese Medicinal (TCM) herbal remedies serve as complementary medicines co-administered with conventional treatment regimens for tuberculosis. Some of these TCM decoctions have been clinically proven to be efficacious in treating tuberculosis (Reported in Zhang et al.16). The African populace has likewise for decades been using traditional medicines for the treatment of tuberculosis18,19, including communities in Ghana and South Africa20,21,22. However, challenges associated with handling of the highly infectious M. tuberculosis have limited the antimycobacterial activity evaluation of most traditional medicinal plants. Airborne infectious agents such as M. tuberculosis can only be handled safely in Biosafety Level III facilities, which very few institutions have23. This challenge in handling the bacterium has also made it difficult to isolate the active compounds using the commonly adopted classical bioassay-guided fractionation process. Bioassay-guided fractionation demands several steps, during which fractions and sub-fractions need to be screened against M. tuberculosis. Nonetheless, attempts to investigate several plants have provided interesting leads, including Crinum asiaticum and Artemisia afra24,25. However, active ingredients against Mycobacterium in both plants have not been identified.
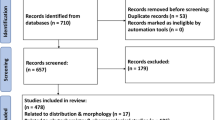
To accelerate the discovery of new antimycobacterial leads from African plant species, in the current extensive collaborative investigation, we screened ca. 290 extracts and fractions for activity against two non-pathogenic M. tuberculosis surrogate strains, Mycobacterium smegmatis and Mycobacterium aurum. Using metabolomics techniques, we tentatively identified the bioactive natural compounds. We further assessed the activity of these putative compounds using a classification machine learning model.
Results and discussion
Plant material collection, extraction, and solid phase extraction (SPE) fractionation
A total of 31 different medicinal plant species were evaluated in the study (Table 1 and Supplementary File Table S1). These plant species were selected for evaluation based on either their traditional medicinal use, or that of related species, for the treatment of tuberculosis20 and other bacterial diseases. The Asteraceae plant family was the most represented with seven species (Table 1). It was closely followed by the Amaryllidaceae which had five different species with most of them assigned to the genus Crinum. The Lamiaceae plant family had three representatives closely followed by Meliaceae, Zingiberaceae, and Hypericaceae which each had two representative species. The most investigated plant parts were the leaves. Bulbs were used in the case of Crinum spp. while whole plants, flowers and stems were utilised for some plant species. Each plant species provided one extract and seven fractions. Exceptions were Hedychium flavescens, Cyrtanthus mackenii, Tulbaghia simmleri, Crinum jagus and Crinum asiaticum which each provided two different extracts (of different parts of the plant) and their 14 respective fractions (Table 1). From the plant extraction and high-throughput pre-fractionation process, a total of 36 crude extracts and their corresponding 252 solid phase extraction (SPE) generated fractions (7 fractions per extract) were attained. All extracts and fractions were completely dissolved in 100% dimethyl sulphoxide (DMSO) at a stock concentration of 20 mg/mL. These stock solutions were stored in 96 deep-well plates covered with aluminum plates at 4 °C in a fridge prior to being subjected to in vitro biological evaluation.
Antimycobacterial properties of extracts and their fractions
Having acquired the crude extracts of plants and their SPE fractions, the next step was to assess their in vitro antimycobacterial activity. This assessment was carried out using the high-throughput spot culture growth inhibition assay (HT-SPOTi) method26. The Middlebrook 7H10 agar culture medium supplemented with 0.5% glycerol and 10% (v/v) oleic albumin dextrose and catalase (OADC) was used for the assay. The activity of the extracts and fractions was evaluated against M. smegmatis and M. aurum. Both strains, M. smegmatis and M. aurum, have the advantage of being non-pathogenic and hence can be handled regularly with relative ease in a BSL-2 biosafety cabinet. Furthermore, they are fast growing and most importantly have a drug susceptibility profile which closely resembles that of the infectious M. tuberculosis strain8. Rifamycin served as a positive control drug for the inhibition of proliferation of M. smegmatis and M. aurum with MIC values of 7.813 and 3.907 µg/mL, respectively, consistent with that reported in other studies.
The results showed that most species demonstrated some level of potency against either one of the two Mycobacterium strains or both (Table 1). Mycobacterium smegmatis was the most susceptible Mycobacterium species with 79 fractions being active (MIC ≤ 200 µg/mL), representing a 31% hit rate (calculated by dividing the total number of active fractions by the total number of fractions screened against the bacterial species, i.e., 252). Sixty-seven fractions were active against M. aurum with a calculated hit rate of 27%. The SPE generated fractions F4 and F5 had the greatest number of actives totaling 32 and 31, respectively, against both M. smegmatis and M. aurum while F1 and F2 had the least number of actives totaling 10 and 11, respectively. The plant species which had the greatest number of active fractions against both M. smegmatis and M. aurum, were Terminalia phanerophlebia and Ekebergia capensis, each with a total of 10 and 9 active fractions, respectively, against both strains. They were closely followed by Geranium robustum, Senegalia burkei, Hypericum roeperianum, and Artemsia annua each with eight active fractions. H. flavescens (flowers), Siphonochilus aethiopicus, C. mackenii (leaves and roots), and Gymnanthemum corymbosum did not have any active fractions against either of the two Mycobacterium strains (Table 1). There was no plant family which distinctly emerged as the most promising in having the highest proportion of active fractions. However, the Lamiaceae emerged as the least attractive, having the fewest number of active fractions per plant species part evaluated, i.e., an average of 2.3 active fractions (calculated by dividing the total number of active fractions in the family with the total number of extracts evaluated in the family).
Further examination of the potency of the plant species highlighted C. asiaticum (bulbs) to be the most active as six of its fractions were highly active (MIC values ≤ 30 µg/mL) against both M. smegmatis and M. aurum (Table 2). Fraction 5 of C. asiaticum emerged as the most active, being equipotent against both Mycobacterium strains with a remarkable MIC of 0.39 µg/mL. Other notable highly active SPE fractions against M. aurum were those of G. robustum (Fractions 1, 2 and 3), H. flavescens (stems) (Fraction 6), Helichrysum odoratissimum (Fractions 5 and 6), and Gymnanthemum myrianthum (Fractions 4 and 5) (Table 2). It was interesting to note that despite having highly active extracts against M. aurum (MIC = 12.5 µg/mL), SPE-fractions of H. flavescens were all inactive. In contrast to this, SPE-fractions of G. robustum, G. myrianthum and C. asiaticum showed marked activity despite the extract being inactive (MIC > 200 µg/mL) (Table 2). Having emerged as the most active sample, Fraction 5 of C. asiaticum and its parent extract were prioritised for further evaluation against the infectious M. tuberculosis H37RvMA strain.
The in vitro activity of the crude extract of C. asiaticum and its SPE-fraction 5 (F5) were phenotypically assessed against the infectious M. tuberculosis H37RvMA strain at the Holistic Drug Discovery and Development Centre (H3D), University of Cape Town, South Africa27. The microplate Alamar blue assay was used to determine the MIC of the extract and its fraction28. Cognisant of the influence of different media supplements on the activity of compounds in the test samples, the assay was carried out in three different culture mediums (Table 3)29. Moxifloxacin and isoniazid served as positive controls with both standard drugs showing expected MIC values (Table 3) consistent with previous studies30.
Encouragingly, fraction F5 demonstrated moderate activity against M. tuberculosis with an average MIC of 32.6 µg/mL (Table 3). This activity was only observed in the serum free medium 7H9_CAS_GLU_TX (Table 3). However, this level of activity for fraction F5 was observed to be ca. 100-fold less than that measured against M. smegmatis and M. aurum. Nevertheless, this activity was regarded as promising, warranting further continued investigation of C. asiaticum to identify the active ingredients.
Metabolomic analysis to predict active compounds in C. asiaticum
Having shown its potency against the three different Mycobacterium strains, we sought to obtain insight as to which compounds of C. asiaticum (bulb) could be active antimycobacterial constituents. Towards this goal, we first classified fractions F4 to F6 as active and the rest as inactive based on their MIC values (≤ 30 µg/mL) against M. smegmatis and M. aurum. We employed a more robust procedure, namely chemometrics analysis of active and inactive fractions of C. asiaticum31,32. In this component of the study, for each fraction we acquired their UPLC-HRMS (ESI+) data in triplicate. The acquired mass spectrometry data was first pre-processed using Waters MakerLynx XS® resulting in a data matrix file. This file was imported as a Microsoft Excel sheet which was used as an input for multivariate analysis on SIMCA®-P.
First, we performed an unsupervised statistical analysis using principal component analysis (PCA) on SIMCA® (Fig. 1a). The PCA showed good separation of the seven different fractions F1 to F7 (Fig. 1a). The two PCA components, 1 and 2, accounted for a combined 45% of the total variation. The highly polar fractions F1 (CAf1) to F3 (CAf3) were grouped to the right while the moderately polar fractions F4 (CAf4) to F7 (CAf7) were organised to the left of the PCA scores plot (Fig. 1a). For better resolution, supervised multivariate analysis was performed using orthogonal projections to latent structures Discriminant Analysis (OPLS-DA). The OPLS-DA scores plot was created, and it distinctly showed separation of active and inactive fractions (Fig. 1b). The quality of the OPLS-DA model was assessed by evaluation of the goodness of fit and predictive ability. The following parameters, R2X = 0.529, R2Y = 1, and Q2 = 0.991 were observed indicative of the OPLS-DA model to be a good fit with acceptable predictive capacity.
Multivariate analysis of UPLC-MS/MS data of C. asiaticum fractions using PCA and OPLS-DA models to identify the potentially active compounds. Unsupervised (a) PCA scores plots, (b) OPLS-DA scores plots, (c) OPLS-DA loadings S-plot and (d) contribution plot. Compounds projecting above 0 on the contribution plot are positively associated with activity while those below 0 are negatively correlated to activity. VIP is the variable importance in projection score which is computed for the OPLS-DA model. It provides an estimate on the importance of the respective variable. For each fraction UPLC-MS/MS data was acquired in triplicate, i.e., fraction F1.1 to F1.3 (CAf1.1 to CAf1.3) up to F7.1 to F7.3 (CAf7.1 to CAf7.3). The bottom left quadrant has discriminating features positively associated with activity against M. smegmatis and M. aurum. (1) dihydronarcissidine, (2) 3,4-dimethoxyhydrocinnamic acid, (3) ambellin, (4) acetylcaranine, (5) 6-(2-(5-Hydroxy-1,4-dioxo-1,4-dihydronaphthalen-2-yloxy)acetamido)hexanoic acid, (6) 3,4-dihydroxyphenylglycol, (7) 3',4'-dimethoxy-2-hydroxyacetophenone, and (8) (E)-8,11,12-trihydroxyoctadec-9-enoic acid.
Having confidently shown that the OPLS-DA scores plot was able to satisfactorily separate the active and inactive fractions, we then generated its loadings S-plot (Fig. 1c). This loadings plot showed discriminating variables, each dot representing a feature (compound), unique between the two groups of fractions. Of most interest were the extreme discriminate features in the bottom left quadrant which are positively associated with antimycobacterial potency of the active fractions. This positive contribution to activity is further noted on the contributions plot and the respective VIP values for these variables (Fig. 1d). These discriminating features were then manually annotated based on analysis carried out on MarkerLynx (v 4.1) and published literature sources (Table 4 and Supplementary File F1 to F8)33,34,35,36,37,38,39,40. This process led to the tentative identification of eight annotated compounds, namely (1) dihydronarcissidine, (2) 3,4-dimethoxyhydrocinnamic acid, (3) ambellin, (4) acetylcaranine, (5) 6-(2-(5-Hydroxy-1,4-dioxo-1,4-dihydronaphthalen-2-yloxy)acetamido)hexanoic acid, (6) 3,4-dihydroxyphenylglycol, (7) 3',4'-dimethoxy-2-hydroxyacetophenone, and (8) (E)-8,11,12-trihydroxyoctadec-9-enoic acid (Table 4, Fig. 2). These eight compounds are potentially responsible for the potency against M. smegmatis and M. aurum. Using NPClassifier41, many of the compounds, namely 1, 3, and 4, were assigned into the Pathway, Super Class and Class of Alkaloids, Tyrosine alkaloids and Amaryllidaceae alkaloids, respectively. Exceptions were compounds 5 (Polyketides, Naphthalenes and Naphthoquinones), 6 (Alkaloids, Tyrosine alkaloids and Phenylethylamines), 7 (Shikimates and Phenylpropanoids) and 8 (Fatty acids, Octadecanoids and Other Octadecanoids). Compound 2 was classified into Shikimates and Phenylpropanoids, Phenylpropanoids (C6-C3) and Cinnamic acids and derivatives based on structural similarity to cinnamic acid.
2D chemical representations of tentative compounds from C. asiaticum predicted to be active against M. smegmatis and M. aurum. (1) dihydronarcissidine, (2) 3,4-dimethoxyhydrocinnamic acid, (3) ambellin, (4) acetylcaranine, (5) 6-(2-(5-hydroxy-1,4-dioxo-1,4-dihydronaphthalen-2-yloxy)acetamido)hexanoic acid, (6) 3,4-dihydroxyphenylglycol, (7) 3',4'-dimethoxy-2-hydroxyacetophenone, and (8) (E)-8,11,12-trihydroxyoctadec-9-enoic acid. Mr molecular mass, cLogP consensus LogP, TPSA total polar surface area and #RB number of rotatable bonds. TPSA, cLogP and #RB were computed using the online SwissADME application44.
Discussion
As the antimicrobial resistance phenomenon continues to render tuberculosis treatment regimens less effective, there is a need to discover and develop new therapeutics to turn the tide against this scourge. The aim of this study was to find new chemical scaffolds from which antimycobacterial drugs could be developed. To facilitate the process to identify potential antimycobacterial compounds from the potent plant species we employed UPLC-HRMS metabolomics integrated with multivariate analysis. This is a proven robust tool in the natural products drug discovery field for the identification of active compounds from different natural product sources including plants31,32,45,46,47,48,49,50,51. Apart from its reliability in predicting potent compounds, it also has the advantage of being less time consuming compared to the classical bioassay-guided approach. This metabolomics approach allowed us to identify nine potential antimycobacterial compounds from C. asiaticum.
A preeminent indicator as to what kind of compound in C. asiaticum could be potent against M. tuberculosis emerged from the in vitro assays against this bacterium. The hint was the fact that activity against M. tuberculosis was only observed in serum free medium. The influence of culture medium supplements, particularly serum and albumin, is well documented within the tuberculosis drug discovery field29. The influence is by way of extensively binding to some molecules, especially those that are lipophilic. When serum binds tightly to lipophilic compounds it reduces their concentration in medium to levels unable to exert any effect on the target organism52. This hypothesis could hold true for compound 8 which had a noticeable high cLogP making it lipophilic. It is logical to assume this could have happened in serum supplemented media leading to loss of activity which was regained in serum free medium. In fact, a thorough literature search revealed that structurally similar compounds, namely fatty acids, have been demonstrated to have activity against M. tuberculosis in vitro53. Choi53 showed moderate activity of different isomers of linoleic acid and their conjugated forms against M. tuberculosis grown in Middlebrook 7H9 broth supplemented with 10% (v/v) oleic acid/albumin/dextrose/catalase enrichment and 0.05% (v/v) Tween 80. This included compound 9, structurally closely related to 8, with an MIC value of 75 µg/mL (Fig. 3)53. The mechanism of action of fatty acids has been postulated to be possible through causing membrane leakage by disrupting its integrity54. From a medicinal chemistry perspective, this compound has limitations such as the high number of rotatable bonds. This could make it highly flexible, allowing it to fit into many different active sites hence becoming toxic.
Cinnamic acids have received marked interest in the antimycobacterial drug discovery field55,56,57. Most notable is the study by Andrade-Ochoa et al.58 in which cinnamic acid (10, Fig. 3) was evaluated and shown to be potent against M. tuberculosis H37Rv (MIC = 8.16 µg/mL) and M. bovis AN5 (MIC = 7.29 µg/mL) strains cultured in Middlebrook 7H9 liquid media supplemented with 10% Middlebrook OADC enrichment, 0.05% Tween, and 0.2% Glycerol. Equally impressively potent was cinnamaldehyde (11, Fig. 3) with MIC values of 3.12 µg/mL and 12.5 µg/mL against M. tuberculosis H37Rv and M. bovis AN5, respectively58. Compound 2 is structurally unique in that it has two ether groups. This novelty in its structural architecture could endow it with improved physicochemical properties. This has been observed in the conversion of the alcohol functional moiety in dihydroartemisinin to a methyl ether functional group in artemether. The structural transformation resulted in a more potent and biological stable drug, i.e., artemether59. This makes it a worthwhile undertaking to isolate and investigate compound 2. Moreover, beyond potency against M. tuberculosis, cinnamic acids have also been shown to enhance the activity of tuberculosis drugs56,57. Interestingly, the different geometric isomers show marked differences in potency against M. tuberculosis. The cis-cinnamic is more potent than the trans-cinnamic form with minimum bactericidal concentrations of 2.5 µg/mL and 300 µg/mL, respectively, against M. tuberculosis56. The cis-cinnamic also had more pronounced synergistic activity in enhancing potency of standard tuberculosis drugs against MDR M. tuberculosis56. This could be an interesting avenue to explore for compound 2 as well. The predicted ADME properties of compound 2 do make it an interesting prospect for medicinal chemistry development.
The Amaryllidaceae alkaloids have received minimal interest for their antimycobacterial activity. Maafi et al.60 previously screened a series of 9 Amaryllidaceae alkaloids against a non-pathogenic M. tuberculosis H37Ra ITM-M006710 (ATCC 9431) strain. The culture medium used for the assay was Middlebrook 7H9 broth enriched with 0.4% glycerol and 10% Middlebrook OADC growth supplement. All nine compounds, including the highly toxic lycorine, were inactive in vitro against M. tuberculosis. In the same study, the authors developed derivatives of the Amaryllidaceae alkaloids. Interestingly, only the derivatives with high lipophilicity (cLogP ranging from 4.2 to 5.99) were observed to be active against M. tuberculosis, including one which had an MIC value of 1.25 µg/mL. However, the selectivity index of these derivatives was low, something which future studies will need to improve on60.
An interesting candidate to have emerged from our study is compound 5, a naphthoquinone. Despite the limited evaluation of this class of natural products, a study by van der Kooy et al.61 examined the activity of six naphthoquinones, isolated from a South African plant species Euclea natalensis (Ebenaceae), against M. tuberculosis. They used “enriched Middlebrook 7H9 broth base supplemented with bovine serum albumin, catalase, casein hydrolysate and 14C labelled substrate (palmitic acid) as a source of carbon.”61. Most of the compounds showed good activity with 7-methyljuglone (12) emerging as the most potent with an MIC of 0.5 µg/mL against M. tuberculosis (Fig. 3). Because of the structural similarity between 12 and menaquinone, a substrate of enzymes involved in the Mycobacterial electron transport chain, the authors suggested that the mechanism of action of this compound could be by negatively affecting this essential biological process in M. tuberculosis. This presumably could be by way of competitive inhibition. Given the structural resemblance of compound 5 to menaquinone, it is logical to hypothesise that this compound might possibly demonstrate this mechanism of action. This will be a subject of future research.
The distribution of plant families evaluated in the study was largely consistent with that reported by Sharma et al.62 who showed the Asteraceae to be the most represented family for antimycobacterial studies in their comprehensive systematic study. The reported activity of C. asiaticum reported here is the most prolific thus far compared to previous studies25. This clearly demonstrated the advantage of fractionation in improving activity. It was surprising to note the less pronounced activity of A. afra fractions. From a prior study, A. afra DCM extract was active against M. aurum (IC50 = 270 µg/mL) while, interestingly, its water and methanol extracts were inactive24. This suggested that compounds of medium polarity were most likely responsible for activity, given the fact that polar compounds in the highly polar solvents were inactive. The extract used in the current study was a DCM : MeOH extract while fractionation was largely carried out using a combined mixture of water and methanol with CAN : MeOH (50:50), a medium polar solvent, only used in the last fractionation step. This could explain the lack of activity as most likely the fractionation process failed to extract the medium polar compounds in the crude extract. Only fraction F7 was active with an MIC = 200 µg/mL against M. aurum.
Conclusion
To advance antimycobacterial drug discovery from plant derived natural products, our collaborative study investigated African medicinal plants leading to the identification of a fraction of C. asiaticum which showed pronounced activity against M. smegmatis and M. aurum. This fraction was additionally moderately active against M. tuberculosis. UPLC-HRMS combined with multivariate analysis led to the prediction of 3 Amaryllidaceae alkaloids, a cinnamic acid derivative, a naphthoquinone and fatty acid as active constituents. To the best of our knowledge, none of these eight compounds have been experimentally evaluated for their activity against M. tuberculosis, making them promising prospects for continued studies. These natural compounds will be isolated and screened for their antimycobacterial activity in future studies.
Materials and methods
Plant collection
Twenty-nine of the plants used in the study were collected from the Biodiscovery Center, Department of Chemistry, University of Pretoria. This batch of plants consists of those previously collected and prepared by Clarkson et al.63, Fouche et al.64, Fouche et al.65, Moyo et al.66 and Mianda et al.67. C. asiaticum and C. jagus were collected in Ghana as per previous reports25,68 (Supplementary File Table S1 and voucher specimen numbers included). Permission to collect plant material was provided by relevant authorities in Ghana and South Africa. Collected plants were identified by botanists with respective voucher specimens deposited either at the South African National Biodiversity Institute (SANBI), H.G.W.J. Schweickerdt Herbarium of the University of Pretoria, and the herbarium of the Faculty of Pharmacy and Pharmaceutical Sciences, KNUST, Kumasi, Ghana (Supplementary File Table S1). Collected plants were identified by the following, Mr. J. Simpson, University of Pretoria66, Dr. Henry Sam69 and Mr. Clifford Asare25,68, Department of Herbal Medicine, Faculty of Pharmacy and Pharmaceutical Sciences, Kwame Nkrumah University of Science and Technology, Ghana, and Mr D Schuhardt, Mr E Nienaber, Mr Hans Vahrmeijer, Mr J Male, Mr FJ Potgieter, DJE Venter, Mr E Nienaber and JD Spies (all employed by Council for Scientific and Industrial Research at the time of collections and identifications done at South African Biodiversity Institute) and Mr JJ Meyer of the South African Biodiversity Institute. All experiments were carried out in accordance with relevant guidelines and regulations.
Extraction and fractionation
A modified version by Invernizzi et al.70 of the National Cancer Institute (NCI) protocol by Thornburg et al.71 was used for the microextraction and fractionation of the plant samples. Dry plant material (7.2 g) was loaded into an extraction glass vessel70. A 50 mL 1:1 mixture of dichloromethane (DCM) : methanol (MeOH) was added to the vessel containing the plant material and sonicated in an ultrasonic bath for 1 h at a temperature of ca. 38ºC70. Following the extraction, the DCM : MeOH solution was subsequently drained, and collected into round bottom flasks, before carrying out a second extraction cycle with 50 mL MeOH. The extracts were combined and dried using an SP Genevac HT6 (Genevac Ltd., Ipswich, UK). A HypeSep C8 SPE cartridge (2 g/6 ml) was used to fractionate each extract into 7 fractions using a Gilson GX-241 ASPEC® liquid handler70. The DCM : MeOH extract (600 mg) was dissolved in 6 ml of a DCM : MeOH solution (liquid handling done manually) and adsorbed onto a cottonwool roll. The cottonwool roll with the crude extract was dried before being transferred to an empty prewashed 10 mL SPE cartridge70. Fractionation commenced as previously described Invernizzi et al.70: 19:1 (H2O : MeOH); 4:1 (H2O : MeOH); 3:2 (H2O : MeOH); 1:1 (H2O : MeOH); 2:3 (H2O : MeOH); 1:4 (H2O : MeOH) and 1:1 (ACN : MeOH) resulting in 7 fractions (F1 to F7) collected per each extract. The collected fractions were dried using an SP Genevac HT6. The resulting dried fractions and extracts were dissolved in 100% dimethyl sulphoxide (DMSO) to a stock solution of 20 mg/mL and stored in a freezer at 4ºC prior to screening.
Antimycobacterial screening
In vitro M. smegmatis and M. aurum screening
The MIC of fractions and the reference antibiotic was measured using the previously established high-throughput spot culture growth inhibition assay (HT-SPOTi) approach26. In summary, autoclaved Middlebrook 7H10 agar with 0.5% glycerol was used. Agar was treated with 10% (v/v) oleic albumin dextrose and catalase (OADC). To achieve a larger range of concentration, the extracts and fractions were serially diluted with 0.3% DMSO in a PCR half-skirted 96-well plate.
Mycobacterial strains (M. smegmatis (NCTC 8159, ATCC 19420) and M. aurum (NCTC 10437, ATCC 23366) were inoculated in Falcon tubes with 10 mL MB7H10 and incubated at 37ºC for 18–24 h. As previously reported by Danquah et al.26 and Ofori et al.25, 2 µL of extracts, fractions and positive control drug, rifamycin, were transferred from a PCR half-skirted plate into a 96-well plate. Prepared agar (200 µL) was added to each well of the plate containing the already dispensed fractions. Each well of the 96-well plate received 2 µL of the bacterial suspension containing ca. 1 × 106 cfu/mL. The bacterial spot suspension was absorbed into the agar over a 5-min period. The plates were sealed with parafilm, wrapped with aluminum foil, and incubated at 37 °C for 18–24 h. Wells with no drug served as growth control. After incubation, plate was observed, and the minimum inhibitory (MIC) concentration determined. Assays were carried out in technical duplicates.
In vitro M. tuberculosis assay
Antimycobacterial assays were outsourced to the H3D Center, University of Cape Town, South Africa27. The MIC, i.e., concentration required to inhibit 90% of the culture of M. tuberculosis H37RvMA ATCC 27294, was determined using the slightly microplate Alamar blue assay previously described by Franzblau et al.28. The crude extract and fraction F5 were evaluated in three media compositions as follows: (1) 7H9_ADC_GLU_TW: Middlebrook 7H9 media (Difco) supplemented with 0.2% Glucose, Middlebrook albumin-dextrose- catalase (ADC) enrichment (Difco) and 0.05% Tween 80, (2) 7H9_ADC_GLU_TX: Middlebrook 7H9 media (Difco) supplemented with 0.2% Glucose, Middlebrook albumin-dextrose- catalase (ADC) enrichment (Difco) and 0.05% Tyloxapol and (3) 7H9_CAS_GLU_TX: Middlebrook 7H9 media (Difco) supplemented with 0.4% Glucose, 0.03% Casitone (Gibco Bacto) and 0.05% Tyloxapol.
The test samples were received as liquid stocks at concentrations of 20 mg/mL and 16.7 mg/mL for the crude extract of C. asiaticum and its fraction F5, respectively. Two-fold serial dilutions were prepared in growth medium in 96-well round bottom plates. A concentration range of 125–0.244 µg/mL and 104.37–0.203 µg/mL was investigated for each sample respectively. Isoniazid and moxifloxacin were included as the positive control drugs in all experiments. A maximum inhibition control (rifamycin at 0.15 µM) and a minimum inhibition control (0.625% DMSO) were included on each test plate.
The culture of M. tuberculosis H37RvMA72, in 7H9_ADC_GLU_TW, was grown to an optical density (OD600) of 0.5–0.7 and diluted down to OD600 of 0.001 in each medium. 50 µL of the diluted culture (ca. 1 × 104 bacilli) was added to each well of each test plate, for a final volume of 100 µL per well. Each plant sample was tested in technical duplicate. The assay plates were incubated at 37 °C with 5% CO2 and humidification for 7 days. One tenth of the assay volume of resazurin (0.2 mg/mL prepared in phosphate buffered saline) was then added to each well of the assay plate and re-incubated for 24 h. The relative fluorescence units (RFU) (excitation 540 nm; emission 590 nm) of each well was measured using a SpectraMax iD3-3130 plate reader at day 8 (Molecular Devices Corporation, CA, USA).
Data analysis was performed using the built-in Spectramax protocol. Briefly, raw RFU data was normalised to the minimum and maximum inhibition controls to generate a dose response curve (% inhibition), using the Levenberg–Marquardt damped least-squares method, from which the MIC is calculated using the 4-parameter curve fit protocol. The lowest concentration of drug that inhibits 90% of growth of the bacterial population was interpreted to be the MIC.
UPLC-HRMS instrumentation chromatographic and MS conditions
Chromatographic analysis was performed on a Waters Aquity UPLC and system (Waters Inc., MA, USA). The SPE-fractions were dissolved in MeOH to a concentration of 1500 ppm (1.5 mg/mL) following which they were centrifuged for 30 s using a Mini Centrifuge (BOECO, Germany) to completely dissolve the fractions. The dissolved fractions (5 µL per injection) were run using a Waters ACQUITY UPLC® BEH C18 (2.1 mm × 100 mm, 1.7 µm) column (Waters Inc., MA, USA). The mobile gradient phase consisted of two solvents, namely A = H2O + 0.1% formic acid and B = MeOH + 0.1% formic acid, applied in gradient mode as follows, 0 min 3% B, 1 min 3% B, 14 min 100% B, 17 min 100% B, 17.5 min 3% B, 20 min 3% B. the flow rate and column temperature were held constant throughout the runs at 0.3 mL/min and 50 °C. The separated compounds were tentatively identified using a Xevo® G2 QTof mass spectrometer, run in electrospray ionization positive (ESI+) mode, coupled to an ACQUITY QDa mass detector (Waters Inc., MA, USA). The system was operated with MassLynx™ (v 4.1) software (Waters Inc., MA, USA) for data independent acquisition. The source conditions were as follows: the capillary voltage for ESI was 2.8 kV ESI+. The source temperature was set at 120 °C, the sampling cone voltage at 30 V, extraction cone voltage at 4.0 V and cone gas (nitrogen) flow at 20 L/h. The desolvation temperature was set at 350 °C with a desolvation gas (nitrogen) flow rate of 600.0 L/h. Fragmentation was performed using high energy collision induced dissociation (CID). The fragmentation energy was set at 2 V and 3 V for the trap and collision energy, respectively. The ramping was set from 3 to 4 V and 20 to 40 V for the trap and transfer collision energy, respectively. Mass spectral scans were collected every 0.3 s. Leucine enkephalin (m/z 555.2693, 2 ng/µL) was used as an internal lockmass standard with direct infusion at a flow rate of 3 µL/min. The raw data was collected in the form of a continuous profile. Mass to charge ratios (m/z) between 50 and 1 200 Da were recorded. Compound annotation was carried out by generating the respective molecular formula, Fit Confidence %, accurate mass and fragmentation pattern on MassLynx (v 4.1) and comparing them with published data. Discovery setting tolerance was set to 5 ppm for m/z, 10% for i-Fit confidence and MassFragment software was used for fragment matching. Annotation of compounds was carried out to Confidence Level 343. The physicochemical properties of the compounds were computed online using SwissADME application44.
Data processing and chemometrics analysis
Raw mass spectral data was processed using MarkerLynx XS Method Editor (v 4.1) (Waters Inc., MA, USA) and carried using the parameters indicated on Table 5. Features were generated using a marker tolerance of 0.05 Da for m/z and ± 0.2 min for RT. The resulting Data matrix sheet, which included peak intensities, retention time, m/z values was exported as a Microsoft Excel CSV sheet. The Excel sheet was used an input file on SIMCA®-P (v 17) (Sartorius Stedim Data Analytics AB, Umeå, Sweden) for principal component analysis (PCA) and orthogonal projections to latent structures Discriminant Analysis (OPLS-DA) multivariate analysis. The PCA and OPLS-DA models were constructed of Pareto Scale transformed data. For this analysis, active SPE-fractions were classified as those with an MIC ≤ 30 µg/mL. Results generated by the PCA and OPLS-DA models were visualised as scores and loadings plots. Discriminate variables of significance were noted from the S-plot, their corresponding variable importance in the projection (VIP) values (> 1) and contribution plot generated from the OPLS-DA model.
Data availability
The datasets generated in this study are available from the corresponding author on reasonable request.
References
Houben, R. M. & Dodd, P. J. The global burden of latent tuberculosis infection: A re-estimation using mathematical modelling. PLoS Med. 13, e1002152 (2016).
World Health Organization. Global Tuberculosis Report 2023. (World Health Organization, 2023).
Seung, K. J., Keshavjee, S. & Rich, M. L. Multidrug-resistant tuberculosis and extensively drug-resistant tuberculosis. Cold Spring Harbor Perspect. Med. 5, 12 (2015).
Marks, S. M. et al. Treatment practices, outcomes, and costs of multidrug-resistant and extensively drug-resistant tuberculosis, United States, 2005–2007. Emerg. Infect. Dis. 20, 812 (2014).
Monedero-Recuero, I., Gegia, M., Wares, D. F., Chadha, S. S. & Mirzayev, F. Situational analysis of 10 countries with a high burden of drug-resistant tuberculosis 2 years post-UNHLM declaration: Progress and setbacks in a changing landscape. Int. J. Infect. Dis. 108, 557–567 (2021).
Ismail, N. A. et al. Prevalence of drug-resistant tuberculosis and imputed burden in South Africa: A national and sub-national cross-sectional survey. Lancet. Infect. Dis 18, 779–787 (2018).
Newman, D. J. & Cragg, G. M. Natural products as sources of new drugs over the nearly four decades from 01/1981 to 09/2019. J. Nat. Prod. 83, 770–803 (2020).
Nguta, J. M., Appiah-Opong, R., Nyarko, A. K., Yeboah-Manu, D. & Addo, P. G. Current perspectives in drug discovery against tuberculosis from natural products. Int. J. Mycobacteriol. 4, 165–183 (2015).
Floss, H. G. & Yu, T.-W. Rifamycin mode of action, resistance, and biosynthesis. Chem. Rev. 105, 621–632 (2005).
World Health Organization. WHO Consolidated Guidelines on Tuberculosis. Module 4: Treatment-Drug-Resistant Tuberculosis Treatment. (World Health Organization, 2020).
Sataloff, J., Wagner, S. & Menduke, H. Kanamycin ototoxicity in healthy men. Arch. Otolaryngol. 80, 413–417 (1964).
Hinshaw, H. C., Feldman, W. H. & Pfuetze, K. H. Streptomycin in treatment of clinical tuberculosis. Am. Rev. Tuberculosis 54, 191–203 (1946).
Lee, R. E. et al. Spectinamides: A new class of semisynthetic antituberculosis agents that overcome native drug efflux. Nat Med. 20, 152–158 (2014).
Gonzalez-Juarrero, M. et al. Preclinical evaluation of inhalational spectinamide-1599 therapy against tuberculosis. ACS Infect. Dis. 7, 2850–2863 (2021).
Singh, P. et al. The paradox of pyrazinamide: An update on the molecular mechanisms of pyrazinamide resistance in Mycobacteria. J. Commun. Dis. 38, 288 (2006).
Zhang, S.-Y. et al. Improvement cues of lesion absorption using the adjuvant therapy of traditional Chinese medicine Qinbudan tablet for retreatment pulmonary tuberculosis with standard anti-tuberculosis regimen. Infect. Dis. Poverty 9, 1–11 (2020).
Zheng, Y. et al. Identification of plant-derived natural products as potential inhibitors of the Mycobacterium tuberculosis proteasome. BMC Complement. Altern. Med. 14, 1–7 (2014).
Getachew, S., Medhin, G., Asres, A., Abebe, G. & Ameni, G. Traditional medicinal plants used in the treatment of tuberculosis in Ethiopia: A systematic review. Heliyon 8, e09478 (2022).
Oryema, C., Rutaro, K., Oyet, S. W. & Malinga, G. M. Ethnobotanical plants used in the management of symptoms of tuberculosis in rural Uganda. Trop. Med. Health 49, 92 (2021).
Semenya, S. S. & Maroyi, A. Medicinal plants used for the treatment of tuberculosis by Bapedi traditional healers in three districts of the Limpopo Province, South Africa. Afr. J. Tradit. Complement. Altern. Med. 10, 316–323 (2013).
Nguta, J. M., Appiah-Opong, R., Nyarko, A. K., Yeboah-Manu, D. & Addo, P. G. A. Medicinal plants used to treat TB in Ghana. Int. J. Mycobacteriol. 4, 116–123 (2015).
Lawal, I. O., Grierson, D. S. & Afolayan, A. J. Phytotherapeutic information on plants used for the treatment of tuberculosis in Eastern Cape Province, South Africa. Evid.-Based Complem. Altern. Med. 2014, 735423 (2014).
Pauli, G. F. et al. New perspectives on natural products in TB drug research. Life Sci. 78, 485–494 (2005).
Ntutela, S. et al. Efficacy of Artemisia afra phytotherapy in experimental tuberculosis. Tuberculosis 89, S33–S40 (2009).
Ofori, M., Danquah, C. A., Ativui, S., Doe, P. & Asamoah, W. A. In-vitro anti-tuberculosis, anti-efflux pumps and anti-biofilm effects of Crinum asiaticum bulbs. Biomed. Pharmacol. J. 14, 1905–1915 (2021).
Danquah, C. A., Maitra, A., Gibbons, S., Faull, J. & Bhakta, S. HT-SPOTi: A rapid drug susceptibility test (DST) to evaluate antibiotic resistance profiles and novel chemicals for anti-infective drug discovery. Curr. Protoc. Microbiol. 40, 171811–171812 (2016).
Singh, V., Mambwe, D., Korkor, C. M. & Chibale, K. Innovation Experiences from Africa-led drug discovery at the holistic drug discovery and development (H3D) centre. ACS Med. Chem. Lett. 13, 1221–1230 (2022).
Franzblau, S. G. et al. Rapid, low-technology MIC determination with clinical Mycobacterium tuberculosis isolates by using the microplate Alamar Blue assay. J. Clin. Microbiol. 36, 362–366 (1998).
Franzblau, S. G. et al. Comprehensive analysis of methods used for the evaluation of compounds against Mycobacterium tuberculosis. Tuberculosis 92, 453–488 (2012).
Basarab, G. S. et al. Spiropyrimidinetriones: A class of DNA gyrase inhibitors with activity against mycobacterium tuberculosis and without cross-resistance to fluoroquinolones. Antimicrob. Agents Chemother. 66, e02192-e12121 (2022).
Yuliana, N. D., Khatib, A., Choi, Y. H. & Verpoorte, R. Metabolomics for bioactivity assessment of natural products. Phytother. Res. 25, 157–169 (2011).
Okada, T. et al. Metabolomics of medicinal plants: The importance of multivariate analysis of analytical chemistry data. Curr. Comput.-Aided Drug Des. 6, 179–196 (2010).
Refaat, J., Kamel, M. S., Ramadan, M. A. & Ali, A. A. Crinum; an endless source of bioactive principles: A review: Part III; crinum alkaloids: Belladine-, galanthamine-, lycorenine-, tazettine-type alkaloids and other minor types. Int. J. Pharmaceut. Sci. Res. 3, 3630 (2012).
Boit, H. G. & Ehmke, H. Alkaloide von Nerine Bowdenii, Crinum Powellii, Amaryllis Belladonna und Pancratium maritimum (XII. Mitteil. Über Amaryllidaceen-Alkaloide). Chem. Berichte 89, 2093–2097 (1956).
Nair, J. J. & van Staden, J. Antiplasmodial lycorane alkaloid principles of the plant family Amaryllidaceae. Planta Med. 85, 637–647 (2019).
Manickam, M. et al. Design, synthesis and anticancer activity of 2-amidomethoxy-1, 4-naphthoquinones and its conjugates with Biotin/polyamine. Bioorgan. Med. Chem. Lett. 31, 127685 (2021).
Sang, S. et al. Antifungal constituents from the seeds of Allium fistulosum L.. J. Agric. Food Chem. 50, 6318–6321 (2002).
de Moreira, L. D., Guimarães, E. F. & Kaplan, M. A. C. A C-glucosylflavone from leaves of Piper lhotzkyanum. Phytochemistry 55, 783–786 (2000).
Khalifa, A. Non alkaloidal constituents from Crinum bulbispermum bulbs. Bull. Pharmaceut. Sci. Assiut 24, 41–45 (2001).
Ahmed, S. A., Taha, E., Koriem, I. & Kamel, E. M. Butanolide, tyrosol ester and acetophenone derivatives from terrestrial Streptomyces spp. World J. Pharm. Res. 4, 300–310 (2015).
Kim, H. W. et al. NPClassifier: A deep neural network-based structural classification tool for natural products. J. Nat. Prod. 84, 2795–2807 (2021).
Ghosal, S., Rao, P. H., Jaiswal, D. K., Kumar, Y. & Frahm, A. W. Alkaloids of Crinum pratense. Phytochemistry 20, 2003–2007 (1981).
Blaženović, I., Kind, T., Ji, J. & Fiehn, O. Software tools and approaches for compound identification of LC-MS/MS data in metabolomics. Metabolites 8, 31 (2018).
Daina, A., Michielin, O. & Zoete, V. SwissADME: A free web tool to evaluate pharmacokinetics, drug-likeness and medicinal chemistry friendliness of small molecules. Sci. Rep. 7, 42717 (2017).
Aminov, R. Metabolomics in antimicrobial drug discovery. Exp. Opin. Drug Discov. 17, 1047–1059 (2022).
Wishart, D. S. Applications of metabolomics in drug discovery and development. Drugs R & D 9, 307–322 (2008).
Pandohee, J., Kyereh, E., Kulshrestha, S., Xu, B. & Mahomoodally, M. F. Review of the recent developments in metabolomics-based phytochemical research. Crit. Rev. Food Sci. Nutr. 5, 1–16 (2021).
Li, P. et al. Identification of xanthones from the mangosteen pericarp that inhibit the growth of Ralstonia solanacearum. ACS Omega 5, 334–343 (2019).
More, G. K., Vervoort, J., Steenkamp, P. A. & Prinsloo, G. Metabolomic profile of medicinal plants with anti-RVFV activity. Heliyon 8, 8936 (2022).
Khin, M. et al. Capturing the antimicrobial profile of Rosmarinus officinalis against methicillin-resistant Staphylococcus aureus (MRSA) with bioassay-guided fractionation and bioinformatics. J. Pharmaceut. Biomed. Anal. 197, 113965 (2021).
Kamal, N., Viegelmann, C. V., Clements, C. J. & Edrada-Ebel, R. Metabolomics-guided isolation of anti-trypanosomal metabolites from the endophytic fungus Lasiodiplodia theobromae. Planta Med. 234, 565–573 (2017).
Smit, F. J. et al. Synthesis and antimycobacterial activity of disubstituted benzyltriazoles. Med. Chem. Res. 28, 2279–2293 (2019).
Choi, W. H. Evaluation of anti-tubercular activity of linolenic acid and conjugated-linoleic acid as effective inhibitors against Mycobacterium tuberculosis. Asian Pac. J. Trop. Med. 9, 125–129 (2016).
Tanvir, R., Javeed, A. & Rehman, Y. Fatty acids and their amide derivatives from endophytes: New therapeutic possibilities from a hidden source. FEMS Microbiol. Lett. 365, 114 (2018).
Bairwa, R. et al. Novel molecular hybrids of cinnamic acids and guanylhydrazones as potential antitubercular agents. Bioorgan. Med. Chem. Lett. 20, 1623–1625 (2010).
Chen, Y.-L. et al. Transformation of cinnamic acid from trans-to cis-form raises a notable bactericidal and synergistic activity against multiple-drug resistant Mycobacterium tuberculosis. Eur. J. Pharmaceut. Sci. 43, 188–194 (2011).
Rastogi, N., Goh, K. S., Horgen, L. & Barrow, W. W. Synergistic activities of antituberculous drugs with cerulenin and trans-cinnamic acid against Mycobacterium tuberculosis. FEMS Immunol. Med. Microbiol. 21, 149–157 (1998).
Andrade-Ochoa, S. et al. Quantitative structure-activity relationship of molecules constituent of different essential oils with antimycobacterial activity against Mycobacterium tuberculosis and Mycobacterium bovis. BMC Complem. Altern. Med. 15, 1–11 (2015).
Guo, Z. The modification of natural products for medical use. Acta Pharm. Sin. B 7, 119–136 (2017).
Maafi, N. et al. Semisynthetic derivatives of selected Amaryllidaceae alkaloids as a new class of antimycobacterial agents. Molecules 26, 6023 (2021).
Van der Kooy, F., Meyer, J. & Lall, N. Antimycobacterial activity and possible mode of action of newly isolated neodiospyrin and other naphthoquinones from Euclea natalensis. S. Afr. J. Bot. 72, 349–352 (2006).
Sharma, A. et al. BioPhytMol: A drug discovery community resource on anti-mycobacterial phytomolecules and plant extracts. J. Cheminform. 6, 46 (2014).
Clarkson, C. et al. In vitro antiplasmodial activity of medicinal plants native to or naturalised in South Africa. J. Ethnopharmacol. 92, 177–191 (2004).
Fouché, G. et al. In vitro anticancer screening of South African plants. J. Ethnopharmacol. 119, 455–461 (2008).
Fouche, G. et al. Investigation of in vitro and in vivo anti-asthmatic properties of Siphonochilus aethiopicus. J. Ethnopharmacol. 133, 843–849 (2011).
Moyo, P. et al. In vitro inhibition of Plasmodium falciparum early and late stage gametocyte viability by extracts from eight traditionally used South African plant species. J. Ethnopharmacol. 185, 235–242 (2016).
Mianda, S. M. et al. In vitro dual activity of Aloe marlothii roots and its chemical constituents against Plasmodium falciparum asexual and sexual stage parasites. J. Ethnopharmacol. 297, 115551 (2022).
Minkah, P.A.B. & Danquah, C.A. Anti-infective, anti-inflammatory and antipyretic activities of the bulb extracts of Crinum jagus (J. Thomps.) Dandy (Amaryllidaceae). Sci. Afr. 12, e00723 (2021).
Ofori, M. et al. Betulin and Crinum asiaticum L. bulbs extract attenuate pulmonary fibrosis by down regulating pro-fibrotic and pro-inflammatory cytokines in bleomycin-induced fibrosis mice model. Heliyon 9, e16914 (2023).
Invernizzi, L. et al. Use of hyphenated analytical techniques to identify the bioactive constituents of Gunnera perpensa L., a South African medicinal plant, which potently inhibit SARS-CoV-2 spike glycoprotein–host ACE2 binding. Anal. Bioanal. Chem. 414, 3971–3985 (2022).
Thornburg, C. C. et al. NCI program for natural product discovery: A publicly-accessible library of natural product fractions for high-throughput screening. ACS Chem. Biol. 13, 2484–2497 (2018).
Ioerger, T. R. et al. Variation among genome sequences of H37Rv strains of Mycobacterium tuberculosis from multiple laboratories. J. Bacteriol. 192, 3645–3653 (2010).
Acknowledgements
The H3D is acknowledged for M. tuberculosis in vitro screening service of two samples reported in this study.
Author information
Authors and Affiliations
Contributions
VJM, CAD, LM and PM conceptualized the work. VJM and CAD supervised the data acquisition. PM, MO, OB, KK, and MW performed experiments and data analysis. PM, MO, MW and VJM wrote the first original draft article. LM, CAD, KK, and OB reviewed and edited the draft manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Moyo, P., Ofori, M., Bodede, O.S. et al. Investigation of the antimycobacterial activity of African medicinal plants combined with chemometric analysis to identify potential leads. Sci Rep 14, 14660 (2024). https://doi.org/10.1038/s41598-024-65369-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-65369-7
- Springer Nature Limited