Abstract
Prolonged ventricular repolarization has been associated with cardiovascular disease. We sought to investigate the association of prolonged ventricular repolarization with mild cognitive impairment (MCI) and the potential underlying neuropathological mechanisms in older adults. This cross-sectional study included 4328 dementia-free participants (age ≥ 65 years; 56.8% female) in the baseline examination of the Multidomain INterventions to delay dementia and Disability in rural China; of these, 989 undertook structural brain magnetic resonance imaging (MRI) scans. QT, QTc, JT, JTc, and QRS intervals were derived from 12-lead electrocardiograph. MCI, amnestic MCI (aMCI), and non-amnestic MCI (naMCI) were defined following the Petersen’s criteria. Volumes of gray matter (GM), white matter, cerebrospinal fluid, total white matter hyperintensities (WMH), periventricular WMH (PWMH), and deep WMH (DWMH) were automatically estimated. Data were analyzed using logistic and general linear regression models. Prolonged QT, QTc, JT, and JTc intervals were significantly associated with an increased likelihood of MCI and aMCI, but not naMCI (p < 0.05). In the MRI subsample, QT, QTc, JT, and JTc intervals were significantly associated with larger total WMH and PWMH volumes (p < 0.05), but not with DWMH volume. Statistical interactions were detected, such that prolonged QT and JT intervals were significantly associated with reduced GM volume only among participants with coronary heart disease or without APOE ε4 allele (p < 0.05). Prolonged ventricular repolarization is associated with MCI and cerebral microvascular lesions in a general population of older adults. This underlies the importance of cognitive assessments and brain MRI examination among older adults with prolonged QT interval.
Similar content being viewed by others
Introduction
Mild cognitive impairment (MCI) is considered a transitional stage between normal cognitive aging and dementia, and people with MCI show an increased risk of progression to dementia1. MCI can be subdivided into amnestic MCI (aMCI) and non-amnestic MCI (naMCI), based on the presence of memory impairment, where aMCI is more commonly associated with progression to Alzheimer's dementia (AD)2. Accumulated evidence has shown that cardiometabolic risk factors and related cardiovascular disease (CVD) are tightly associated with cognitive impairment3,4,5, partially due to common pathophysiological mechanisms (e.g., arterial stiffness, thrombo-embolism, and cerebral hypoperfusion)6. The ventricular electrocardiogram (ECG) profiles are the early markers of cardiovascular disorders. For example, QT interval and JT interval (QT-QRS) reflect ventricular repolarization, while QRS interval indicates ventricular depolarization. Besides, a prolonged QT interval was associated with coronary heart disease (CHD), impaired right ventricular function, and clinical stroke7,8,9, suggesting that altered ventricular repolarization may have an impact on the brain, and thus, cognitive function. Previous studies have linked prolonged QT interval with poor cognitive function10,11, but the community-based studies that explore the relationships of prolonged ventricular repolarization with MCI and its subtypes in older adults are currently lacking.
The underlying neuropathological pathways linking ECG markers to cognitive phenotype are poorly characterized. Data from the Prospective Study of Pravastatin in the Elderly at Risk (PROSPER) showed no associations of prolonged ventricular repolarization with any of the examined brain MRI metrics (e.g., grey matter volume, number of microbleeds, and white matter hyperintensities [WMH]) in older individuals with high cardiovascular risk12. However, whether prolonged QT and JT intervals are associated with structural brain lesions in a general population of older adults is unknown.
In this cross-sectional study, we sought to examine the association of QT, QTc, JT, JTc, and QRS intervals with MCI, subtypes of MCI, and brain MRI metrics in rural older adults in China. Our hypothesis was that prolonged ventricular repolarization was associated with structural brain lesions, and thus, with MCI, in old age (Fig. 1).
Results
Characteristics of study participants (n = 4328)
The mean age of the 4,328 participants was 71.02 years (age range, 65–91 years; standard deviation [SD], 4.7 years), 56.8% were female, and 37.4% had no formal education. Out of these, 1172 (27.1%) were diagnosed with MCI, including 991 with aMCI and 181 with naMCI. Compared to cognitively normal participants (n = 3156), those with MCI were older; more likely to be female; less educated; had a higher systolic blood pressure and resting heart rate, lower eGFR and BMI, longer QTc, JT, and JTc intervals, shorter QRS interval; and had a higher prevalence of stroke (p < 0.05, Table 1).
In the MRI subsample, 236 (23.9%) of the 989 participants were defined with MCI. Individuals with MCI (vs. no MCI) had lower volumes of ICV, GM, and WM and greater volumes of total WMH and PWMH (p < 0.01), while people without and with MCI did not differ significantly in CSF and DWMH volumes (Table 1).
Association of ventricular ECG parameters with MCI, aMCI, and naMCI (n = 4328)
Logistic regression analysis suggested that longer QT, QTc, JT, and JTc intervals were significantly associated with an increased likelihood of MCI after adjusting for a wide range of demographic, lifestyle, and clinical factors (all p < 0.05, Model 2, Table 2). Similar results were obtained for the associations of QT, QTc, JT, and JTc intervals with aMCI, and the multivariable-adjusted odds ratio of aMCI associated with per 1-SD increment in QT interval was 1.13 (95% confidence interval [CI]: 1.03, 1.25), while there was no significant association of ECG parameters with naMCI. In addition, QRS interval was not significantly associated with MCI, aMCI, or naMCI (Table 2). In the sensitivity analysis, we repeated the analysis among participants who were free from atrial fibrillation or stroke. The findings remained generally consistent (Supplementary Tables 1 and 2).
Association of ventricular ECG parameters with structural brain measures (n = 989)
Longer QT interval was significantly associated with lower GM volume, with the multivariable-adjusted β coefficient (per 1-SD increment in QT interval) being -2.77 (95% CI: -5.23, -0.30) (Table 3). Besides, prolonged JT and JTc interval were marginally associated with decreased WM volume. Furthermore, prolonged QT, QTc, JT, and JTc intervals were significantly associated with increased WMH volume, with the β coefficient of cubic-rooted WMH volume associated with per 1-SD increment in QT interval and JT interval being 0.08 (0.03, 0.13, p = 0.002) and 0.06 (0.01, 0.12, p = 0.02), respectively. Analogous patterns were obtained for the association of ECG parameters with PWMH volume, but there was no significant association with DWMH volume in the multivariable-adjusted model. In addition, QRS interval was not related to any of the examined structural brain MRI measures (Table 3). The sensitivity analysis among participants who were from atrial fibrillation or stroke yielded the results that were overall similar to those from the main analysis (Supplementary Tables 3 and 4).
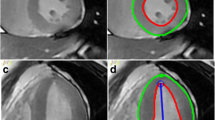
We detected statistical interactions of CHD and APOE ε4 allele with QT, JT, and JTc intervals on GM and CSF volumes (all p for interaction < 0.05). Stratified analysis showed prolonged QT interval was significantly associated with decreased GM volume and increased CSF volume among participants with CHD or those without APOE ε4 allele (p < 0.05), but not among those without the history of CHD or with APOE ε4 allele. The associations of GM volume with JT and JTc intervals stratified by history of CHD or APOE ε4 allele were overall comparable to those with QT interval (Fig. 2 and Supplementary Fig. 1).
Association of QT, JT, and JTc intervals with grey matter volume stratified by history of CHD and APOE genotype (n = 989). CHD, Coronary heart diseases; CI, Confidence interval. Models were adjusted for age, sex, education, heart rate (QT and JT intervals only), MRI center, total intracranial volume, smoking, alcohol intake, body mass index, dyslipidemia, hypertension, diabetes, APOE genotype (if applicable), CHD (if applicable), arrhythmia, heart failure, stroke, transient ischemic attack, and use of anti-thrombotic agents, cardiac agents, and QT prolonging agents.
Discussion
In this cross-sectional study of rural-dwelling older adults in China, we investigated the association of ventricular ECG parameters with MCI, subtypes of MCI, and neuroimaging markers of brain lesions. Our main findings could be summarized as follows: (1) prolonged ventricular repolarization was independently associated with MCI, and aMCI in particular, but not with naMCI; (2) prolonged ventricular repolarization was independently associated with cortical atrophy and increased total WMH, and PWMH in particular, but not with DWMH; and (3) the associations of prolonged ventricular repolarization with atrophic brain measures varied by CHD and APOE gene, such that QT and JT intervals were associated with brain atrophy only among people with CHD or APOE ε4 non-carriers. Collectively, these results imply that prolonged ventricular repolarization is a valuable clinical marker for MCI, especially aMCI, and that altered ECG parameters and MCI may share common cerebral neuropathological lesions in a general population of rural older adults.
Previously, we reported that prolonged QT and JT intervals were associated with dementia and poor global cognitive function in older adults, even among those who were free of CVD11,13. Data from PROSPER study of older adults at high risk for cardiovascular events showed that prolonged ventricular repolarization was associated with poor function of several cognitive domains (e.g., attention and processing speed)12. Furthermore, other ventricular ECG parameters, such as the spatial QRS-T angle and left ventricular hypertrophy, have been associated with cognitive decline in older adults14,15. These studies support the view that abnormalities in ECG parameters is associated with cognitive phenotypes in older people. By contrast, participants in the Chicago Health and Aging Project (59% black) failed to show the association of QT prolongation with global cognitive performance, but other altered ventricular parameters (e.g., T wave nondipolar voltage) were associated with poor cognition16. Our current study revealed for the first time that prolonged ventricular repolarization was associated with MCI, and aMCI in particular, but not with naMCI, in a general population of rural older adults. Because individuals with aMCI were more likely to progress to dementia, especially AD, than those with naMCI2,17, these results imply that prolonged ventricular repolarization may be an early marker for prodromal dementia in older adults. Of note, the length of QRS interval was not associated with MCI and its subtypes in our study. Previous research has indicated that QRS prolongation, which is less common than QTc interval prolongation, was associated with increased long-term mortality18. Thus, the lack of cross-sectional association between QRS interval length and MCI in our study might be partially attributable to selective survival associated with QRS prolongation.
Evidence supporting the association of prolonged ventricular repolarization with brain MRI alterations is limited. The PROSPER study did not show any association of prolonged ventricular repolarization with structural brain MRI markers12. A possible explanation was that the PROSPER participants were relatively healthy in cognitive function (MMSE score ≥ 24), and thus, they might have fewer brain lesions. Indeed, the load of WMH in our study sample was about 3 times greater compared to that of the PROSPER participants. Our study further revealed the associations of prolonged ventricular repolarization with reduced GM volume and increased volumes of WMH, and PWMH in particular. Indeed, PWMH, but not DWMH, were associated with accelerated cognitive decline19, progression from aMCI to AD dementia20, and an increased risk of dementia21. In addition, we revealed the CHD- and APOE gene-varying associations between QT prolongation and brain atrophy, suggesting that CVD may be involved in the association of ECG markers with brain atrophic lesions, and that APOE ε4 allele may share a different pathophysiological process. This merits further investigation in future studies. Collectively, these results support the view that neuropathological alterations (e.g., cerebral microvascular and atrophic lesions) may be the common pathophysiological process linking prolonged ventricular repolarization with cognitive phenotypes.
Several possible mechanisms may underlie the observed associations. First, prolonged ventricular repolarization may be linked with cerebral hypoperfusion, and thus affecting cognitive function. Indeed, large-scale prospective studies showed that QT prolongation was a risk factor for incident stroke7,22. Second, prolonged ventricular repolarization is known to be associated with CVD (e.g., CHD and heart failure)7,23, which might further lead to cognitive impairment. Third, previous studies from the US and our own project have indicated that prolonged ventricular repolarization were associated with elevated serum inflammatory cytokines (e.g., IL-6) and adhesion molecules (e.g., ICAM-1 and VCAM-1)11,24. Inflammatory cytokines could lead to long-QT syndrome either directly through membrane ion channels modulation or indirectly through the reduction of testosterone levels or bioavailability of QT-prolonging drugs25,26. Thus, systemic inflammation may play an important role in linking prolonged ventricular repolarization with WMH and MCI. Fourth, altered ECG parameters may be related to autonomic dysfunction, which was common in patients with MCI27. Previous research reported a correlation between QT prolongation and dorsal vagal nucleus infarction28, which might affect the parasympathetic pathway and dysregulate the automatic neural control of cardiac function29. This indicates that prolonged ventricular repolarization may be cerebrogenic arrhythmia. Finally, given that WMH were associated with cerebral amyloid angiopathy and aMCI and AD30,31, prolonged ventricular repolarization could be linked with aMCI and AD partially via cerebral microvascular lesions. Indeed, previous research has linked prolonged QT, JT, and JTc intervals with plasma AD-related biomarkers (e.g., a decreased Aβ42/Aβ40 ratio and increased plasma neurofilament light chain protein)13.
Our study showed that prolonged ventricular repolarization was associated with MCI, subtypes of MCI, and MRI markers of brain microvascular and atrophic lesions in older adults. Many medications could affect QT intervals, such as Alzheimer’s drugs (e.g., galantamine and donepezil), cardiovascular agents (e.g., amiodarone and nicardipine), and antipsychotic agents (e.g., clozapine, escitalopram, and amantadine)32,33. Besides, previous studies showed that QT prolongation was associated with an increased risk of stroke and cardiac mortality22,34. Therefore, it is of clinical importance to recognize the prolonged QT intervals for older adults when taking these medications, and cognitive assessments and brain MRI examination may be considered for older adults with prolonged QT intervals.
This large-scale study engaged rural-dwelling Chinese older adults who had relatively low income and received no or very limited education (83.1% had no formal school education or only attended primary school). Given that most studies of this topic in the current literature have been carried out among urban populations in high-income countries, findings from our study could contribute to health equity across ethnically, socioeconomically, and demographically diverse populations. In addition, by integrating structural brain MRI data with extensive epidemiological, clinical, neuropsychological, and pharmacological profiles, we were able to explore the underlying neuropathologies linking prolonged ventricular repolarization with MCI and subtypes of MCI. However, our study also has limitations. First, we were not able to determine the causality due to the nature of cross-sectional study and the cross-sectional design also limited the investigation of the possible mechanisms underlying the observed associations and the interpretation of the research findings. Future prospective longitudinal studies are warranted to help clarify the potential causal relationship of prolonged ventricular repolarization with cognitive phenotypes and the underlying neuropathological mechanisms. Second, although we have controlled for extensive possible confounders, we cannot rule out the potential impact of residual confounding due to imperfect measurements of some confounders (e.g., self-reported lifestyle factors and health history). Finally, participants in the MRI subsample were younger, healthier, and more educated compared to those in the MIND-China total sample35. This should be kept in mind when generalizing these findings to other populations.
Our cross-sectional study revealed associations of prolonged ventricular repolarization with MCI, especially aMCI, but not with naMCI, in older adults. Furthermore, altered ECG parameters were associated with reduced GM volume and increased WMH volume, and increased PWMH volume in particular, but not with DWMH volume. The associations of ECG parameters with structural brain MRI markers varied by CHD and APOE gene, such that prolonged QT and JTs interval were associated with brain atrophy only among individuals who had CHD or did not carry the APOE ε4 allele. These findings suggest that prolonged ventricular repolarization is a valuable marker for prodromal dementia and vascular brain pathology in older adults, and that cognitive assessment and brain MRI examination may be important for older adults with QT prolongation.
Methods
Study design and participants
This is a cross-sectional study. We used data collected from the baseline assessments of the Multimodal INterventions to delay Dementia and disability in rural China (MIND-China) project, which is part of the World-Wide FINGERS Network36,37. MIND-China targeted at people who were aged ≥ 60 years by the end of 2017 and living in the 52 villages of Yanlou town, Yanggu County, western Shandong province. In March-September 2018, 5,765 participants (74.9% of all eligible persons) underwent the baseline assessments. Participants who were aged 60–64 years (n = 519) were excluded because a considerable proportion of people in this age group were working as rural migrant workers, and thus they could not attend the assessments. Of the 5,246 participants who were aged ≥ 65 years, we further excluded 918 persons due to prevalent dementia (n = 302), severe mental health problems (e.g., depressive symptoms and schizophrenia, n = 46), and missing information on MCI diagnosis (n = 329), ECG parameters (n = 12), or covariates (n = 229), leaving 4328 participants for the analysis of ECG parameters in relation to MCI (analytical sample 1). Using the cluster (village)-randomized sampling approach, a subsample of 1,034 participants were selected from 26 villages and invited for structural brain magnetic resonance imaging (MRI) scans, of these, 45 persons were excluded due to suboptimal MRI quality, leaving 989 individuals for the analysis involving MRI markers (analytical sample 2). Figure 1 shows the flowchart of the study participants.
The Ethics Committee at Shandong Provincial Hospital approved the protocol of MIND-China study. Prior to data collection, written informed consent was obtained from all participants or their guardians in the case of persons with severe cognitive impairment. The MIND-China study was registered in the Chinese Clinical Trial Registry (registration no.: ChiCTR1800017758). Research within MIND-China has been conducted in full compliance with the ethical principles expressed in the Declaration of Helsinki.
Data collection and assessments
Data were collected following the structured questionnaire via face-to-face interviews, clinical and neurological examination, neuropsychological testing, and laboratory tests, as previously described36. In brief, we collected data on demographic features (age, sex, and education), lifestyle factors (e.g., smoking and alcohol consumption), genetic markers (e.g., APOE gene), health history (e.g., body mass index [BMI], dyslipidemia, hypertension, diabetes, CHD, arrhythmia, heart failure, stroke, and transient ischemic attacks [TIAs]), and administered drugs (anti-thrombotic agents, cardiac agents, and QT prolonging agents), which were considered potential confounders. Education was categorized into no formal education, primary school (1–5 years), and middle school or above (≥ 6 years). Smoking and alcohol intake were categorized into never, former, and current smoking or drinking alcohol. Apolipoprotein E (APOE) genotype was dichotomized into carriers vs. non-carriers of the ε4 allele. Information on the current use of medications was collected via in-person interviews, and whenever available, drug prescriptions and containers were checked to verify the information. All medications were classified and coded according to the Anatomical Therapeutic Chemical (ATC) classification system38. Diabetes mellitus, dyslipidemia, and hypertension were defined by integrating self-reported history of respective disorders, clinical examination, blood tests (i.e., fasting blood glucose and serum lipids), and current use of respective mediations (i.e., antihypertensive, blood glucose-lowering, and lipids-lowering drugs), as previously described36. BMI, CHD, heart failure, stroke, TIAs, and arrhythmia were ascertained following the approaches as previously reported11,36. Antithrombotic agents (e.g., acetylsalicylic acid, clopidogrel, and warfarin), cardiac agents (e.g., amiodarone, digoxin, propafenone, isosorbide mononitrate, glyceryl trinitrate, and trimetazidine), and QT prolonging drugs (e.g., alprazolam, olanzapine, perphenazine, sulpiride, and tamoxifen) were considered potential confounders because use of these drugs might affect ECG parameters and might be associated with cognitive impairment as well4,32.
Electrocardiogram (ECG) was recorded in a resting supine position using a 12-lead CM 300 electrocardiograph (Comen Corp., Shenzhen, Guangdong, China). Resting heart rate, QT interval, and QRS interval were obtained from an automated analysis program in the device. JT interval was defined as the length of QT interval minus QRS interval. QTc and JTc intervals were the heart rate-corrected QT and JT intervals, respectively, and were calculated using the Bazett’s formula:39 QTc = QT/(60/[heart rate])1/2; JTc = JT/(60/[heart rate])1/2.
Diagnosis of MCI, aMCI, and naMCI
MCI was diagnosed following the Peterson’s criteria that were operationalized in the same way as used in the Mayo Clinic Study of Aging, as previously described in detail37,40. Briefly, the criteria for defining MCI included: (1) subjective cognitive concern by subjects or informants; (2) objective cognitive impairment evidenced in at least one of the four cognitive domains; (3) essentially preserved functional activities; and (4) absence of dementia diagnosed according to the DSM-IV criteria41. The final judgment was based on both neuropsychological test scores and a consensus agreement among neurologists specialized in cognitive disorders. MCI was further categorized into aMCI if the memory domain was impaired or naMCI if there was no impairment in memory function40.
MRI data acquisition and processing
All eligible participants were scanned on either the Philips Ingenia 3.0 T MR scanner in Shandong Southwestern Lu Hospital (n = 896) or the Philips Archiva 3.0 T MR scanner in Liaocheng People's Hospital (n = 93). The detailed parameters and processing procedure of the core MRI sequences are described previously36,42. We spatially normalized and segmented T1-weighted images and then automatically estimated the total intracranial volume (ICV), volumes of grey matter (GM), white matter (WM), and cerebrospinal fluid (CSF) via the Computational Anatomy Toolbox running on MATLAB (http://dbm.neuro.uni-jena.de/cat12/). ICV and MRI center were considered as potential confounders in the analysis involving brain MRI metrics. T2-FLAIR images were processed in AccuBrain® (BrainNow Medical Technology Ltd., Shenzhen, Guangdong, China) to acquire the volume of WMH42. We further categorized WMH into periventricular WMH (PWMH) and deep WMH (DWMH) according to continuity to ventricles.
Statistical analysis
We reported mean (standard deviation, SD) for continuous variables, and frequency (%) for categorical variables. We compared characteristics of the study participants by MCI status using chi-squared test for categorical variables and Mann–Whitney U test for continuous variables with skewed distribution. ECG parameters (i.e., QT, QTc, JT, JTc, and QRS intervals) were transformed into standardized z-score12. We used multinomial logistic regression models to estimate the associations of QT, QTc, JT, JTc, and QRS intervals with MCI, aMCI, and naMCI. In the MRI subsample, we investigated the associations of ventricular ECG parameters with structural brain MRI metrics using general linear regression models. Owing to right-skewed distribution, WMH, PWMH, and DWMH volume variables were cubic-root transformed42. Statistical interactions were assessed by simultaneously incorporating the independent variables and their cross-product term into the same model. When a statistical interaction was detected (p for interaction < 0.05), stratified analysis was further performed to assess the magnitude and direction of the interaction.
We reported the main results from two models: Model 1 was adjusted for age, sex, education, and resting heart rate (only for QT, JT, and QRS intervals); and Model 2 was additionally adjusted for smoking, alcohol intake, BMI, dyslipidemia, hypertension, diabetes, APOE genotype, CHD, arrhythmia, heart failure, stroke, TIA, anti-thrombotic agents, cardiac agents, and QT prolonging drugs.
R version 3.6.2 (R Core Team: R Project for Statistical Computing, Vienna, Austria. http://www.r-project.org) was used for all statistical analyses. A two-tailed p < 0.05 was considered statistically significant.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Mitchell, A. J. & Shiri-Feshki, M. Rate of progression of mild cognitive impairment to dementia–meta-analysis of 41 robust inception cohort studies. Acta Psychiatr. Scand. 119(4), 252–265. https://doi.org/10.1111/j.1600-0447.2008.01326.x (2009).
Jungwirth, S., Zehetmayer, S., Hinterberger, M., Tragl, K. H. & Fischer, P. The validity of amnestic MCI and non-amnestic MCI at age 75 in the prediction of Alzheimer’s dementia and vascular dementia. Int. Psychogeriatr. 24(6), 959–966. https://doi.org/10.1017/S1041610211002870 (2012).
Qiu, C. & Fratiglioni, L. A major role for cardiovascular burden in age-related cognitive decline. Nat. Rev. Cardiol. 12(5), 267–277. https://doi.org/10.1038/nrcardio.2014.223 (2015).
Ding, M. et al. Atrial fibrillation, antithrombotic treatment, and cognitive aging: a population-based study. Neurology 91(19), e1732–e1740. https://doi.org/10.1212/WNL.0000000000006456 (2018).
Imahori, Y. et al. Association of ischemic heart disease with long-term risk of cognitive decline and dementia: a cohort study. Alzheimers Dement. https://doi.org/10.1002/alz.13114 (2023).
Ding, M. et al. Cerebral small vessel disease associated with atrial fibrillation among older adults: a population-based study. Stroke 52(8), 2685–2689. https://doi.org/10.1161/STROKEAHA.120.031573 (2021).
Maebuchi, D. et al. QT interval prolongation and the risks of stroke and coronary heart disease in a general Japanese population: the Hisayama study. Hypertens Res. 33(9), 916–921. https://doi.org/10.1038/hr.2010.88 (2010).
Robison, L. B., Brady, W. J., Robison, R. A. & Charlton, N. QT interval prolongation and the risk of malignant ventricular dysrhythmia and/or cardiac arrest: Systematic search and narrative review of risk related to the magnitude of QT interval length. Am. J. Emerg. Med. 49, 40–47. https://doi.org/10.1016/j.ajem.2021.05.032 (2021).
Rich, J. D. et al. QTc prolongation is associated with impaired right ventricular function and predicts mortality in pulmonary hypertension. Int. J. Cardiol. 167(3), 669–676. https://doi.org/10.1016/j.ijcard.2012.03.071 (2013).
Imahori, Y., Vetrano, D. L., Ljungman, P. & Qiu, C. Electrocardiographic predictors of cognitive decline and dementia: a systematic review. J. Alzheimers Dis. 84(3), 1303–1322. https://doi.org/10.3233/JAD-210606 (2021).
Wang, C. et al. Associations of cardiac ventricular repolarization with serum adhesion molecules and cognitive function in older adults: the MIND-China study. J Alzheimers Dis. 92(1), 273–283. https://doi.org/10.3233/JAD-220874 (2023).
Zonneveld, M. H. et al. Ventricular repolarization is associated with cognitive function, but not with cognitive decline and brain magnetic resonance imaging (MRI) measurements in older adults. J. Clin. Med. 9(4), 911. https://doi.org/10.3390/jcm9040911 (2020).
Mao, M. et al. Ventricular electrocardiographic signatures associated with dementia and plasma Alzheimer’s disease biomarkers in older adults: a population-based study. J. Alzheimers Dis. 94(4), 1515–1526. https://doi.org/10.3233/JAD-230056 (2023).
Mahinrad, S. et al. Left ventricular hypertrophy and cognitive decline in old age. J. Alzheimers Dis. 58(1), 275–283. https://doi.org/10.3233/JAD-161150 (2017).
Mahinrad, S. et al. Spatial QRS-T angle and cognitive decline in older subjects. J. Alzheimers Dis. 67(1), 279–289. https://doi.org/10.3233/JAD-180633 (2019).
Lucas, B. P., de Leon, C. F., Prineas, R. J., Bienias, J. L. & Evans, D. A. Relation of cardiac ventricular repolarization and global cognitive performance in a community population. Am. J. Cardiol. 106(8), 1169–1173. https://doi.org/10.1016/j.amjcard.2010.06.031 (2010).
Glynn, K. et al. Clinical utility of mild cognitive impairment subtypes and number of impaired cognitive domains at predicting progression to dementia: a 20-year retrospective study. Int. J. Geriatr. Psych. 36(1), 31–37. https://doi.org/10.1002/gps.5385 (2021).
Breidthardt, T. et al. QRS and QTc interval prolongation in the prediction of long-term mortality of patients with acute destabilised heart failure. Heart 93(9), 1093–1097 (2007).
van den Heuvel, D. M. J. et al. Increase in periventricular white matter hyperintensities parallels decline in mental processing speed in a non-demented elderly population. J. Neurol. Neurosurg. Psych. 77(2), 149–153 (2006).
van Straaten, E. C. W. et al. Periventricular white matter hyperintensities increase the likelihood of progression from amnestic mild cognitive impairment to dementia. J. Neurol. 255(9), 1302–1308. https://doi.org/10.1007/s00415-008-0874-y (2008).
Hu, H.-Y. et al. White matter hyperintensities and risks of cognitive impairment and dementia: a systematic review and meta-analysis of 36 prospective studies. Neurosci. Biobehav. Rev. 120, 16–27. https://doi.org/10.1016/j.neubiorev.2020.11.007 (2021).
Soliman, E. Z. et al. Prolongation of QTc and risk of stroke: The REGARDS (REasons for Geographic and Racial Differences in Stroke) study. J. Am. Coll. Cardiol. 59(16), 1460–1467. https://doi.org/10.1016/j.jacc.2012.01.025 (2012).
O’Neal, W. T. et al. Electrocardiographic predictors of heart failure with reduced versus preserved ejection fraction: the multi-ethnic study of atherosclerosis. J. Am. Heart Assoc. 6(6), e006023. https://doi.org/10.1161/JAHA.117.006023 (2017).
Lazzerini, P. E. et al. Elevated interleukin-6 levels are associated with an increased risk of QTc interval prolongation in a large cohort of US veterans. J. Am. Heart Assoc. 13(4), e032071. https://doi.org/10.1161/JAHA.123.032071 (2024).
Lazzerini, P. E., Abbate, A., Boutjdir, M. & Capecchi, P. L. Fir(e)ing the rhythm: inflammatory cytokines and cardiac arrhythmias. JACC Basic Transl. Sci. 8(6), 728–750. https://doi.org/10.1016/j.jacbts.2022.12.004 (2023).
Lazzerini, P. E. et al. Transient hypogonadism is associated with heart rate-corrected QT prolongation and torsades de pointes risk during active systemic inflammation in men. J. Am. Heart Assoc. 11(1), e023371. https://doi.org/10.1161/JAHA.121.023371 (2022).
Collins, O., Dillon, S., Finucane, C., Lawlor, B. & Kenny, R. A. Parasympathetic autonomic dysfunction is common in mild cognitive impairment. Neurobiol. Aging. 33(10), 2324–2333. https://doi.org/10.1016/j.neurobiolaging.2011.11.017 (2012).
Je, G., Sun, Y., Keyhanian, K., Yaghi, S. & Henninger, N. Dorsal vagal nucleus involvement relates to QTc-prolongation after acute medullary infarction. Acta Neurol. Scand. 144(3), 283–287. https://doi.org/10.1111/ane.13445 (2021).
Scheitz, J. F., Nolte, C. H., Doehner, W., Hachinski, V. & Endres, M. Stroke-heart syndrome: clinical presentation and underlying mechanisms. Lancet Neurol. 17(12), 1109–1120. https://doi.org/10.1016/S1474-4422(18)30336-3 (2018).
Luchsinger, J. A. et al. Subclinical cerebrovascular disease in mild cognitive impairment. Neurology 73(6), 450–456. https://doi.org/10.1212/WNL.0b013e3181b1636a (2009).
Garnier-Crussard, A. et al. White matter hyperintensity topography in Alzheimer’s disease and links to cognition. Alzheimers Dement. 18(3), 422–433. https://doi.org/10.1002/alz.12410 (2022).
Nielsen, J. B. et al. Risk prediction of cardiovascular death based on the QTc interval: evaluating age and gender differences in a large primary care population. Eur. Heart J. 35(20), 1335–1344. https://doi.org/10.1093/eurheartj/ehu081 (2014).
Kho, J. et al. Long term use of donepezil and QTc prolongation. Clin. Toxicol. (Phila). 59(3), 208–214. https://doi.org/10.1080/15563650.2020.1788054 (2021).
Straus, S. M. J. M. et al. Prolonged QTc interval and risk of sudden cardiac death in a population of older adults. J. Am. Coll. Cardiol. 47(2), 362–367 (2006).
Song, L. et al. Thalamic gray matter volume mediates the association between KIBRA polymorphism and olfactory function among older adults: a population-based study. Cereb Cortex. 33(7), 3664–3673. https://doi.org/10.1093/cercor/bhac299 (2023).
Wang, Y. et al. Health status and risk profiles for brain aging of rural-dwelling older adults: data from the interdisciplinary baseline assessments in MIND-China. Alzheimers Dement (N Y). 8(1), e12254. https://doi.org/10.1002/trc2.12254 (2022).
Cong, L. et al. Mild cognitive impairment among rural-dwelling older adults in China: a community-based study. Alzheimers Dement. 19(1), 56–66. https://doi.org/10.1002/alz.12629 (2023).
Cong, L. et al. Use of cardiovascular drugs for primary and secondary prevention of cardiovascular disease among rural-dwelling older Chinese adults. Front. Pharmacol. 11, 608136. https://doi.org/10.3389/fphar.2020.608136 (2020).
Bazett, H. An analysis of the time-relations of electrocardiograms. Heart 7, 353–370 (1920).
Petersen, R. C. Mild cognitive impairment as a diagnostic entity. J. Intern Med. 256(3), 183–194 (2004).
Diagnostic and statistical manual of mental disorders : DSM-IV. Fourth edition. Washington, DC : American Psychiatric Association, [1994] ©1994; 1994.
Dong, Y. et al. Anosmia, mild cognitive impairment, and biomarkers of brain aging in older adults. Alzheimers Dement. 19(2), 589–601. https://doi.org/10.1002/alz.12777 (2023).
Acknowledgements
The authors would like to thank all the study participants as well as medical staff at the Yanlou Town Hospital and the Shandong Provincial Hospital for their contributions in data collection and management.
Funding
Open access funding provided by Karolinska Institute. This work was supported in part by grants from the National Natural Science Foundation of China (grants no.: 81861138008), the Alzheimer’s Association Grant (grant no.: AACSFD-22–922844), the National Key R&D Program of China Ministry of Sciences and Technology (grant no.: 2017YFC1310100), the Natural Science Foundation of Shandong Province (grant no.: ZR2021MH005), and the Brain Science and Brain-like Intelligence Technology Research Projects of China (2021ZD0201801 and 2021ZD0201808). C.Q. received grants from the Swedish Research Council (grants no.: 2017–05819 and 2020–01574), the Swedish Foundation for International Cooperation in Research and Higher Education (grant no.: CH2019-8320), and Karolinska Institutet, Stockholm, Sweden. The funding agency had no role in the study design, data collection and analysis, the writing of this manuscript, and in the decision to submit the work for publication.
Author information
Authors and Affiliations
Contributions
Ming Mao, Yongxiang Wang, Yifeng Du, and Chengxuan Qiu: study concept and design; Ming Mao, Yiran Wei, Chaoqun Wang, Xiaolei Han, Rui Liu, Yi Dong, Lin Cong: data collection and assessments; Ming Mao, Yiran Wei: data analysis; Ming Mao: draft of the manuscript; Yongxiang Wang, Yifeng Du, and Chengxuan Qiu: supervision of the study; all authors: critical revision of the manuscript for important intellectual content.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mao, M., Wei, Y., Wang, C. et al. Prolonged ventricular repolarization associated with mild cognitive impairment and white matter hyperintensities: a cross-sectional study. Sci Rep 14, 15162 (2024). https://doi.org/10.1038/s41598-024-65364-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-65364-y
- Springer Nature Limited