Abstract
Maternal mortality ratio (MMR) estimates have been studied over time for understanding its variation across the country. However, it is never sufficient without accounting for presence of variability across in terms of space, time, maternal and system level factors. The study endeavours to estimate and quantify the effect of exposures encompassing all maternal health indicators and system level indicators along with space–time effects influencing MMR in India. Using the most recent level of possible -factors of MMR, maternal health indicators from the National Family Health Survey (NFHS: 2019–21) and system level indicators from government reports a heatmap compared the relative performance of all 19 SRS states. Facet plots with a regression line was utilised for studying patterns of MMR for different states in one frame. Using Bayesian Spatio-temporal random effects, evidence for different MMR patterns and quantification of spatial risks among individual states was produced using estimates of MMR from SRS reports (2014–2020). India has witnessed a decline in MMR, and for the majority of the states, this drop is linear. Few states exhibit cyclical trend such as increasing trends for Haryana and West Bengal which was evident from the two analytical models i.e., facet plots and Bayesian spatio- temporal model. Period of major transition in MMR levels which was common to all states is identified as 2009–2013. Bihar and Assam have estimated posterior probabilities for spatial risk that are relatively greater than other SRS states and are classified as hot spots. More than the individual level factors, health system factors account for a greater reduction in MMR. For more robust findings district level reliable estimates are required. As evident from our study the two most strong health system influencers for reducing MMR in India are Institutional delivery and Skilled birth attendance.
Similar content being viewed by others
Introduction
A maternal death is “the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and site of pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes”1. The likelihood of a woman dying while pregnant is quantified by maternal mortality ratio (MMR), which is the number of maternal deaths per 100,000 live births within a given time period. Globally during 2017 about 295,000 women died during and following pregnancy and childbirth2. Most of these deaths occurred in low and middle-income countries (LMIC), and most could have been prevented.
Maternal mortality reduction has always been a global health priority. Sustainable Development Goals (SDG) target reduction of global MMR to less than 70 per 100,000 births, with no country having MMR more than twice the global average3. Achieving this SDG target would necessitate an average reduction of roughly three times the yearly rate reduction achieved during the (Millennium Development Goals) MDG era4. Despite a documented progress towards this SDG target5,6, a greater acceleration is warranted.
The "three delay" concept7 i.e., delays in making the decision to seek care, delays in getting to a health facility, and delays in health institutions providing proper care, has been the guiding framework behind formulating all policies and programs to reduce MMR. These critical time periods are predictive of most obstetric complications7. Most of the indicators for tracking such delays fall under the ambit of various demographic sample surveys; however, the inadequacy of data collection at smallest spatial unit makes it more difficult to gather routine and comprehensive information about the maternal death.
The Sample Registration system (SRS), a demographic sample survey in India uses nationally representative sample to offer reliable estimates of maternal mortality for major states8. National Family and Health Survey (NFHS) is another large-scale, multi-round survey conducted in a representative sample of households throughout states and districts of India. The survey offers information on fertility, infant and child mortality, family planning, maternal and child health, reproductive health, nutrition, anaemia, and the use and quality of health and family planning services for India at the national, state and district levels9.
India is a confederation of thirty-six (36) states/ union territories (UTs) having diverse and heterogenous culture, geographies, health infrastructure, and health indicators. It acknowledges the regional variations and inequalities and is cognizant of its commitment to cater to the needs of the entire people. Understanding variation for any event or a health outcome through one or two dimensions is never sufficient without accounting for presence of variability across in terms of space and time. We generally look upon the socio-economic exposures for explaining the outcome under study but seldom account for variation in spatial and temporal dimensions. Decline in maternal mortality is associated with ample of variates: socio-economic variables, increased government health expenditure, employment of government schemes, progress in institutional delivery, antenatal and postnatal care, nutrition, birth preparedness and contraception use are some of the indicators which have improved significantly over the years.
Emphasising on the reliability of data for major states from SRS we aim to evaluate evidence for spatio-temporal variations accounting for 45% decline in MMR since last decade across nineteen (19) SRS states. Thus, the study proposes to identify the time of the transition for significant decline in maternal mortality across 19 SRS states between 2000 and 2020 and to understand linear/cyclical declining pattern. The study also endeavours to estimate the spatial risk of individual states and later categorise states as hot spots based on posterior probabilities obtained through adopted model for selected states in India.
Methods
The study used secondary data available in public domain viz SRS and NFHS. The sampling design adopted for SRS is a unit-stage stratified simple random sample without replacement except in stratum II (larger villages) of rural areas, where two stage stratification has been applied10. Total sample units covered by SRS (2018–2020) is 8841 and total population covered is 83,10,00011.
NFHS-5 used a multistage stratified sampling, as part of which the census enumeration blocks (CEBs) in urban areas and villages in rural areas were selected as the primary sampling units (PSUs) based on Probability Proportional to Size (PPS) sampling. It covers 636,699 households, 724,115 women (15–49 years) and 101,839 men (15–54 years)9.
To explore the trends of MMR, data were taken from SRS published reports for 19 states for five time periods 2014–1612, 2015–1713, 2016–1814, 2017–1911 and 2018–2011. Spatial categorisation of 19 SRS states is visualised in supplementary Fig. 1. In order to explore the spatial risk of different states, we retrieved maternal health related indicators from the most recent NFHS-5 (2019–21) survey.
The analysis includes health system level or macro level indicators such as Health index, Government Health Expenditure (GHE), Out of Pocket Expenditure (OOPE), Janani Suraksha Yojna (JSY) beneficiary, Number of Accredited Hospitals, Number of National Quality Assurance Standards (NQAS) certified hospitals. The case definitions of these factors are described in Supplementary table 1. Apart from the above indicators, various health systems centric maternal health indicators were also considered such as percentage of women receiving antenatal care (ANC), percentage of women receiving postnatal care (PNC) within 48 h of delivery, percentage of women with birth order greater than 3, percentage of women with birth interval less than two years, percentage of children who were delivered with skilled birth attendance (either from doctor or auxiliary nurse mid-wife or from any health professional), percentage of women using any contraception method, percentage of women with body mass index (BMI) less than 18.5 kg/m2, percentage of women with anaemia, proportion of women who delivered through caesarean section were considered for analysis15.
Geo-statistical models focus on the response-determinant dynamics to visualize the extent of uncertainty or the degree of regularity for the underlying physical process. These hidden uncertainties might be associated with the data, the underlying spatio-temporal process or with the model parameters which are accounted for by assigning probability distributions to them. A section under the model will explain utility of spatial and spatio-temporal effects in explaining MMR across 19 SRS states of India.
Individual trend of MMR for states was analysed through simple linear regression visualisation using ggplot216 package in R which provides a useful collection of tools to partition the data using "facets"17, which separate the data frame based on the values of specific columns. We obtained graphs each with a separate linear regression line with 95% Confidence Interval for coefficients of indicators fitted against time.
By summarizing massive data sets, the data visualisation approach known as the heatmap enhances descriptive analysis and enhances visualisation, specifically when there is a wealth of data available for many time periods, locations, or qualities. Each data point received after standardisation is given a relative score, and each score is then further assigned to a colour based on our preference. Heatmap scales down each feature under study by standardisation over the span where span can be in years or set of places depending on the data. Scaling in heatmap is done by standardizing the observations in a particular column. The mathematical formula for standardizing is same as standardizing a normal variable to standard normal variable.
The notations \({\text{O}}_{\text{it}}\) and \({\text{E}}_{\text{it}}\) denote observed and expected maternal mortality ratio in area i = 1,2,3…. N (N is the number of states as in SRS report; N = 19 at time t = 1,…,T. In this study T = 5 (SRS-2014–2016, SRS-2015–17, SRS-2016–18, SRS-2017–19 and SRS-2018–20).
where \({\uprho }_{\text{it}}\) represent risk of maternal mortality in district i at time t. \({\text{E}}_{\text{it}}\) can be computed as follows.
\({\text{E}}_{{{\text{it}}}} = \mathop \sum \limits_{{{\text{t}} = 1}}^{{\text{T}}} {\text{P}}_{{{\text{it}}}} \times {\text{~}}\frac{{\mathop \sum \nolimits_{{{\text{i}} = 1}}^{{\text{N}}} {\text{O}}_{{{\text{it}}}} }}{{\mathop \sum \nolimits_{{{\text{i}} = 1}}^{{\text{N}}} {\text{P}}_{{{\text{it}}}} }}\) where \({\text{P}}_{\text{it}}\) is the population under study for state i at time t.
Since MMR is number of maternal deaths per lakh live births, it is standardised with respect to population in each state; therefore, we took E as 1 for each state.
We propose the model18 for explaining Maternal Mortality risk variation across 19 SRS states
#SPTM.
Both spatially structured random effect (\({\text{s}}_{\text{i}}\)) and spatio-temporal effect (\({\updelta }_{\text{i}}\)) are assigned as Conditionally Autoregressive (CAR) Distribution18 as a prior distribution. Model (1) is the baseline model for our study and is described as a model with purely spatial and spatio-temporal random effects. In model 1, estimated log-relative risk is given by \(\text{log}{(\uprho }_{\text{it}})\) at base e and is explained by an overall global risk (given by \(\alpha\)); a risk related to the spatial location (\({\text{s}}_{\text{i}}\)) that can be attributed to factors associated to particular region; a temporal risk trend common to all areas \((\upgamma )\) that can be attributed to changes in coding the underlying factors, policies affecting the whole country and finally an indicator of adjusted area specific trend \(({\updelta }_{\text{i}}\)) that reflect particular effects of each state. More specifically, \({\updelta }_{\text{i}}\) is difference between area specific trend and overall trend \(\upgamma\). Adjusted area specific trends are usually of more interest in planning government intervention strategies as their probability of being greater or smaller than some threshold indicates hot-spots and cold spots respectively. The Poisson distribution is the fundamental distribution when discussing discrete events. Spatial random effects when captured through CAR distribution handles both overdispersion and spatial autocorrelation when counts are modelled through Poisson distribution18.
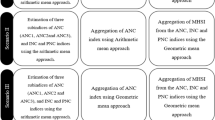
In order to adjust all the 17 exposures discussed as indicators along with the space–time effects we constructed and analysed two different models separated based on health system level factors and individual maternal health factors.
#Maternal Health factors + SPTM.
#Health system level Indicators + SPTM.
Model 2 explains MMR risk through maternal health indicators along with spatial and spatio-temporal effects. Model 3 explains MMR risk through health system level indicators along with spatial and spatio-temporal effects.
Relative risks computed as spatial risk for each areal unit is calculated as \({\widehat{\uprho }}_{\text{i}}=\text{exp}\left({\widehat{\text{s}}}_{\text{i}}\right)\) associated to region \(\text{i}.\) Posterior probability that the spatial risk for MMR is greater than 1, i.e., \({\text{p}}={\text{P}}({\widehat{\uprho }}_{\text{i}}>1/ {\text{Y}}_{\text{it}})\).
All the parameters based on model 1, 2 and 3 are estimated and analysed through Integrated Nested Laplace Approximation (INLA) and the goodness and complexity of different models is assessed and compared through Deviance Information Criterion19 (DIC).
Integrated nested Laplace approximation
An alternate method for approximating Bayesian estimates apart from Monte Carlo Markov Chain (MCMC) technique that is faster and more computationally efficient was introduced20 in 2009 with the name of Integrated Nested Laplace Approximation (INLA). Computing high-dimensional integrals is the main step in Bayesian inference and in our adpated model we estimate our posterior marginals through R-INLA. Analysis for estimates of MMR and covariates have handled in R version 4·1·3. Bayesian estimates have been computed through R-INLA. Facet plots and Heatmaps are obtained in R version 4·1·3.
Results
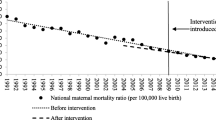
Facet plots for trend of MMR from 2016 to 2020 across 19 SRS states in India (Fig. 1) shows an overall declining trend for all states except for Haryana and West Bengal. States of northern part of the country like Punjab, Uttarakhand, Jharkhand, Haryana, Chhattisgarh, Madhya Pradesh, and Uttar Pradesh exhibit larger variation in MMR as indicated be grey scales representing 95% C.I. in comparison to other states. Southern states like Andhra Pradesh, Tamil Nadu, Kerala and Karnataka are amongst better performing States in context with the MMR as compared to other SRS states.
Heatmap in Fig. 2 represent the scaled estimates of MMR from 2001 to 2020 for 19 SRS states. This reiterates that there is considerable decline in MMR over the years. It can be inferred that the period of major transition for decline in MMR was from 2010 to 2013 and from 2015–2017 is common for all states. During 2016–2020, few states have shown a slight increase in MMR relative scale such as Haryana and West Bengal.
Figure 3 presents the scaled level MMR and associated maternal and health systems level covariates in India. It gives us an essence of performance of the associated covariates with MMR among 19 SRS states. The government health expenditure is relatively lower for states like Madhya Pradesh, Uttar Pradesh, Bihar, Chhattisgarh, and Punjab. Out of pocket expenditure is relatively higher for states like Kerala, West Bengal, Punjab, Maharashtra, Andhra Pradesh and Uttar Pradesh. There seems to be a poor corelation between the percentage of women receiving any money through JSY and proportion of institutional deliveries. States where both JSY beneficiaries and institutional deliveries are low includes Jharkhand and West Bengal. Southern states have fared better in terms of accreditation and NQAS certification of health facilities.
Utilization of ANC services are relatively better in most of the states except Bihar, Jharkhand and Uttarakhand. PNC services remains poorer in many states like Bihar, Assam, Jharkhand, Uttar Pradesh and West Bengal. These states also lag behind in skilled attendance at birth.
Table 1 presents posterior summaries of all parameters investigated under three scenarios i.e., model 1, 2 and 3. We found evidence for significant decline in terms of overall mean time trend from 2014 to 2020 whose posterior mean was estimated as − 0·121 and is significant as per 95% credible interval (C.I.) Estimates for model adequacy and model complexity i.e., DIC of model 3 being lowest is claiming to be best fit among all the three models. Model 2 gives the posterior estimates of maternal health indicators and the intensity of their influence on MMR. Positive posterior estimates in Table 1 indicate increase in MMR and negative posterior estimates indicate decrease in MMR. For example, proportion of women having birth interval less than two years or proportion of low birth interval in any SRS state have higher likelihood of MMR with relative risk of \(\text{exp}(\widehat{{\upbeta }_{3})}=1.638695\). Similarly, proportion of women with birth order greater than 3 or higher birth order has quite similar effect on MMR i.e., \(\text{exp}\left(\widehat{{\upbeta }_{6}}\right)=\) 1.499003. The two health system influencers of MMR which are responsible to decrease MMR strongly are institutional delivery and Skilled birth attendance with relative risk \(\text{exp}(\widehat{{\upbeta }_{9})}=0.4867523\) and \(\text{exp}(\widehat{{\upbeta }_{17})}=0.379842\) respectively. Increase in health system indicators like NQAS with exp \(\left(\widehat{{\upbeta }_{12}}\right)=\) 0.82037, accreditation status with exp (\(\widehat{{\upbeta }_{11})}=\) 0.959829, Health Index with \(\text{exp}(\widehat{{\upbeta }_{10})}=\) 0.615082 and GHE with \(\text{exp}(\widehat{{\upbeta }_{13}})=\) 0.920351 indicate decrease in MMR. OOPE has relative risk \(\text{exp}(\widehat{{\upbeta }_{14})}=\) 1.29706 and JSY has \(\text{exp}(\widehat{{\upbeta }_{15})}=\) 1.386247. The implementation of JSY was on high focus states which is the reason for higher likelihood of MMR in states where larger proportion of women received JSY.
Spatial risk of mortality associated with each state is computed based on model 1 and is presented in Fig. 4. Spatial risk greater than 1 for a state means relative risk of MMR is high than national average level of MMR which is common to all states. Further, in order to categorise states which, have spatial risk close to 1 and might have high probability of MMR risk greater than 1, we evaluated probability of spatial risk greater than 1 for each state as depicted in Fig. 5. The spatial and spatio-temporal effects have been depicted in Figs. 4, 5 and 6 and represent the spatial variation in MMR highlighting individual impact of states in explaining MMR.
Figure 5 depicts the probability such that \({\widehat{\uprho }}_{\text{i}}>1\) is greater than or less than 0·5 i.e., if \(\text{p}=\text{P}({\widehat{\uprho }}_{\text{i}}>1/ {\text{Y}}_{\text{it}})\); then we have mapped for different values of p. States for which \(\text{p}>0\cdot 5\) are classified as hot-spots because they have higher likelihood of having high MMR as compared to others which have \(\text{p}<0\cdot 5\). The latter are qualified as cold spots.
Figure 6 displays the posterior mean for spatio-temporal interaction effect for each SRS state. Since \({\updelta }_{\text{i}}\) is difference between area specific trend and overall mean time trend \((\upgamma )\), \({\updelta }_{\text{i}}\) provides evidence for spatial patterns because of time21. Positive posterior mean for \({\updelta }_{\text{i}}\) indicate risk of maternal mortality has increased over the five time periods from 2014–16 to 2018–20. Negative posterior mean indicates for declining risk of maternal mortality.
It may thus be interpreted that the states like Punjab, Haryana, Uttarakhand, UP, Rajasthan, MP, Chhattisgarh, Bihar, Jharkhand, Odisha West Bengal, and Assam have MMR more than the national average. However, the two states that should deserve focussed attention in terms of MMR reduction includes Bihar and Assam. Bihar exhibits relatively poor maternal health indicators than others which is also in line with estimate of spatial risks and computed probability. When we compare the MMR of each state relative to itself, many states including Punjab, Haryana, UP, MP, Chhattisgarh, West Bengal and Assam demonstrates higher risk over the past five years. For more robust findings district level reliable estimates are required.
Discussion
The present study appraises spatial and spatio-temporal effects for explaining variation in MMR across 19 SRS states. India has witnessed a significant decline in MMR over the past ten years, although there are disparities between states. Most of the decline seems to be attributable to the improvement in health systems indicators across the country, as evident from Bayesian spatio-temporal analysis.
Our analysis demonstrates that the period of major transition for decline in MMR was between 2010 and 2013 and that is common for all states. This period coincides with the implementation of government initiatives such as National Health Mission in 2005 and monetary benefit schemes like JSY and JSSK to cater to the needs of pregnant women and promote institutional deliveries22,23. Institutional deliveries markedly increased after the implementation of JSY22,24,25. Reduction in maternal mortality is most sensitive to access to emergency services in equipped health facilities26,27.
The second transition occurred after 2015, that further coincides with the launch of various breakthrough schemes like Dakshta28 and Labour Room Quality Improvement Initiative (LaQshya) which is a strategic intervention to improve quality of care during and around childbirth. The National Health Mission's Pradhan Mantri Surakshit Matritva Abhiyan (PMSMA)29 was introduced in 2016. The programme seeks to offer guaranteed, thorough, and high-quality antenatal care to all pregnant women on the ninth of every month, free of charge. It is difficult to infer whether these transitions were strictly due to the introduction of specific large scale public health interventions, since a more granular analysis of the determinants indicate the differential uptake of services across the states.
Variation in MMR and the associated maternal level and system level influencers are computed and visualised together in one frame through heatmap. The differential decline is in line with the literature highlighting the poor performance of EAG states30. However, it is pertinent to note that states such as Bihar and Assam would have considerably higher MMR as compared to other states in India as evident from probabilities of spatial risk of individual states. This calls for urgent attention and better implementation of programs in these states for desired results at the national level.
Our study provides geographical and temporal perspectives of explaining variation in MMR using the Bayesian spatio-temporal approach making it one of its own kind. The study has evaluated and quantified the spatial risk, probability of spatial risk and estimate of spatio-temporal effect for each SRS state with respect to MMR for last five time periods making it more robust and generalizable.
Sufficient studies leverage spatial and spatio-temporal methods as indispensable tool for identifying inequalities in access for maternal health services and disparities in utilization31. Classical statistical algorithms such as Spatial autocorrelation32, Geographically weighted regression33, Local Indicators of Spatial Autocorrelation34 have been employed frequently for understanding maternal health and MMR integrated through panel data models in China, Ethiopia and fifty four (54) African countries respectively. Inverse distance weighted method of interpolation method has been used to assess spatial patterns of maternal mortality in Tanzania35. Poisson regression was utilised in understanding spatial distribution of maternal deaths in Brazil36. Studies done under Bayesian formulation for explaining maternal deaths and MMR are very few but have gained popularity recently due to the ease of MCMC and INLA as hassle-free convenient routes for statistical computations. Bayesian multivariable regression32 was employed recently to understand trends of MMR and its cause pattern in 34 Chinese provinces while a Brazilian study used Bayesian empirical model37 to assess covid deaths in obstetric population. The present study combines the essence of Poisson regression handled through Conditional Autoregressive distribution which counters extra-poisson variation38 forms the basis to proposed Bayesian spatio-temporal modelling approach.
We have attempted to explore most probable covariates for MMR. SRS and Health Management Information Systems (HMIS) are the two major data bases that provide information pertaining to maternal deaths and related indicators in India. Both these databases encompass major limitations, but we have used Bayesian methods and model parameters, which accounts for less challenges39, which arises when unstable estimates happen because of low counts of events in areas and high sampling variation40,41,42. This makes this study more unique in its true sense. In this study we have addressed variation in estimates of MMR at different time points. Studies in past tried to estimate district wise maternal mortality ratio through data triangulation43 but robust and reliable district level estimates for MMR from government of India are awaited. The presently reported HMIS data suffers from lack of quality44, manipulation and misreporting45 and hence should be refrained from use in scientific deliberations or should be used with enough caution.
Very few studies have synthesised MMR explanations across space and time in India, and it is extremely uncommon to explain MMR using the broadest range of maternal health markers. For the first time in an Indian study, evaluation of 17 maternal and health system markers that may have an impact on MMR, as well as effects of pure spatial and spatiotemporal interactions, is carried out (Fig. 4, Models 2 and 3 Table 1). Model 2 and Model 3 were designed to analyse maternal level effects and health system effects separately. Health system factors were found to explain risk of MMR better than maternal level factors (Table 1, DIC = 1781).
Despite the fact that our study has numerous methodological and conceptual strengths, it also has certain limitations. The first limitation was the use of data from varied sources viz. SRS and NFHS in the same analysis. This was owing to unavailability of maternal health indicators in SRS data and unavailability of mortality rates in NFHS-5 (2019–2021) data. Even if sampling and random errors are likely to occur because of differential sources, the sources were consistent for all units analyzed, states in this case. The analysis was aggregated at the state level and risk of MMR was adjusted for the population, geographical variation and the proportions of maternal health indicators from NFHS-5 (2019–2021) data which enabled the adopted model to produce robust and reliable results. In order to strengthen the utility of statistical models, a single data source with comprehensive indicators although considered ideal is seldom available. The spatial analysis was undertaken at the state level as the availability of data on maternal mortality in India at district level has been the key barrier for quantitative research for policy formulation for preventing maternal deaths in India. With the progress made thus far, we need to identify districts that are lagging. The findings presented in this study are based on the analysis of aggregated data for 19 SRS states. With the availability of district level estimates of MMR in future, the present study may be extended to districts level analysis for identifying the effect of individual districts within states as hot-spots and cold-spots for explaining variation in MMR and associated maternal and health system level indicators. Association of age, socio-economic factors and educational status with MMR is well explored and hence we refrained from considering these factors in our analysis.
To conclude, although India has made significant progress, we need to accelerate our pace to achieve the SDG goal. Better implementation of national programs in Assam, Bihar, and Jharkhand, calls for innovative approaches to improve coverage. States such as Haryana and West Bengal, which shows rising MMR trends and the Bayesian estimation of spatio-temporal effect, need to analyze their programs more deeply. We should gear up to having region specific and district specific strategies to take the interventions to the last mile. Effective monitoring mechanisms and implementation strategies needs to be relooked in the light of these findings.
Data availability
Data is available from link: https://censusindia.gov.in/nada/index.php/catalog/42687. Govt of India. Ministry of Health and Family Welfare. Report 2019; 13: 315–322. National Health Accounts Technical Secretariat N. National Health Account Estimates for India, 2018–19. The Healthcare Manager: NABH accreditation statistics, https://expresshealthcaremanagement.blogspot.com/2019/06/nabh-accreditation-statistics.html. https://dhsprogram.com/data/available-datasets.cfm. https://qps.nhsrcindia.org/national-quality-assurance-standards.
Code availability
Code for the analysis was built in R version 4.3.2. Code will be shared as per personal request.
References
Hunt P, Gray T. Maternal mortality, human.
World Health Organisation. Trends in maternal mortality 2000 to 2017. (2019).
WHO. Key Facts - Maternal Mortality [Internet]. 2023. https://www.who.int/news-room/fact-sheets/detail/maternal-mortality.
WHO WHO. Trends in Maternal Mortality: 1990 to 2013 [Internet]. 2014. https://apps.who.int/iris/bitstream/handle/10665/112697/WHO_RH?sequence=1.
Hogan, M. C. et al. Maternal mortality for 181 countries, 1980–2008: A systematic analysis of progress towards Millennium Development Goal 5. Lancet 375, 1609–1623 (2010).
Wilmoth, J., Mathers, C., Say, L. & Mills, S. Maternal deaths drop by one-third from 1990 to 2008: A United Nations analysis. Bull. World Health Organ. 88, 718–718a (2010).
Thaddeus, S. & Maine, D. Too far to walk: Maternal mortality in context. Soc. Sci. Med. Pergamon 38, 1091–1110 (1994).
Office of the Registrar General. Sample Registration System: Maternal Mortality in India, 1997–2003: Trends, Causes and Risk Factors. Office of the Registrar General India, in collaboration with Centre for Global Health Research, University of Tor. (2006).
International Institute for Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-5), 2019–21. Mumbai. (2022).
Census of India. Sample Registration System Statistical Report 2014. Off Regist Gen Census Com India Minist Home Aff Gov India [Internet]. 2016;11–28. http://www.censusindia.gov.in/vital_statistics/SRS_Report/9Chap2-2011.pdf.
Of O, Registrar THE. SPECIAL BULLETIN ON. 2022;1–4.
Of O, General R. SPECIAL BULLETIN ON MATERNAL MORTALITY IN INDIA 2014–16 SAMPLE REGISTRATION SYSTEM. 2018;16–8.
Of O, General R. SPECIAL BULLETIN ON MATERNAL MORTALITY IN INDIA 2015–17 SAMPLE REGISTRATION SYSTEM. 2019;17–9.
Sample Registration System Office of the Registrar General I. Special Bulletin on Maternal Mortality in India 2016–18. Sample Regist Syst. 2020;1–4.
The DHS Program - India: Standard DHS, 2019-21 Dataset [Internet]. [cited 2023 Feb 2]. https://dhsprogram.com/data/dataset/India_Standard-DHS_2020.cfm?flag=0.
ggplot2 package - RDocumentation [Internet]. [cited 2023 Feb 2]. https://rdocumentation.org/packages/ggplot2/versions/3.4.0.
Facet_grid function - RDocumentation [Internet]. [cited 2023 Feb 2]. https://www.rdocumentation.org/packages/ggplot2/versions/3.4.0/topics/facet_grid.
Adhikari, T. et al. Spatio-temporal modeling for malnutrition in tribal population among states of India a Bayesian approach. Spat. Spatiotemp. Epidemiol. 40, 100459 (2022).
Spiegelhalter, D. J., Best, N. G., Carlin, B. P. & Van Der Linde, A. Bayesian measures of model complexity and fit. J. R. Stat. Soc. Ser. B Stat. Methodol. 64, 583–616 (2002).
Rue, H., Martino, S. & Chopin, N. Approximate Bayesian inference for latent Gaussian models by using integrated nested Laplace approximations. J. R. Stat. Soc. Ser. B Stat. Methodol. 71, 319–92. https://doi.org/10.1111/j.1467-9868.2008.00700.x (2009).
Law, J., Quick, M. & Chan, P. Bayesian spatio-temporal modeling for analysing local patterns of crime over time at the small-area level. J. Quant. Criminol. 30, 57–78 (2014).
Gupta, S. K. et al. Impact of Janani Suraksha Yojana on institutional delivery rate and maternal morbidity and mortality: An observational study in India. J. Health Popul. Nutr. 30, 464–471 (2012).
Lim, S. S. et al. India’s Janani Suraksha Yojana, a conditional cash transfer programme to increase births in health facilities: An impact evaluation. Lancet 375, 2009–2023 (2010).
Carvalho, N. & Rokicki, S. The impact of India’s Janani Suraksha Yojana conditional cash transfer programme: A replication study. J. Dev. Stud. 55, 989–1006. https://doi.org/10.1080/00220388.2018.1506578 (2019).
Ng, M. et al. An assessment of the impact of the JSY cash transfer program on maternal mortality reduction in Madhya Pradesh, India. Glob. Health Action 7, 24939. https://doi.org/10.3402/gha.v7.24939 (2014).
Ahmed S, Creanga AA, Gillespie DG, Tsui AO. Economic Status, Education and Empowerment: Implications for Maternal Health Service Utilization in Developing Countries. [cited 2023 Feb 28]; www.plosone.org.
Bauserman, M. et al. Risk factors for maternal death and trends in maternal mortality in low- and middle-income countries: A prospective longitudinal cohort analysis. Reprod. Health https://doi.org/10.1186/1742-4755-12-S2-S5 (2015).
Maternal Health Division, Ministry of Health and Family Welfare. Government of India. DAKSHATA: Empowering Providers for Improved MNH Care during Institutional Deliveries. A strategic initiative to strengthen quality of intra- and immediate postpartum care. Operational Guidelines. (2015).
Pradhan Mantri Surakshit Matritva Abhiyan | PMSMA [Internet]. [cited 2023 Mar 1]. https://pmsma.nhp.gov.in/.
Horwood, G., Opondo, C., Choudhury, S. S., Rani, A. & Nair, M. Risk factors for maternal mortality among 1.9 million women in nine empowered action group states in India: Secondary analysis of Annual Health Survey data. BMJ Open 10, e038910 (2020).
Kpienbaareh, D. et al. Spatio-temporal disparities in maternal health service utilization in Rwanda: What next for SDGs?. Soc. Sci. Med. Pergamon 226, 164–175 (2019).
Li, J. et al. Spatiotemporal trends and ecological determinants in maternal mortality ratios in 2205 Chinese counties, 2010–2013: A Bayesian modelling analysis. PLoS Med. 17, 2010–3. https://doi.org/10.1371/journal.pmed.1003114 (2020).
Kurji, J. et al. Spatial variability in factors influencing maternal health service use in Jimma Zone, Ethiopia: A geographically-weighted regression analysis. BMC Health Serv. Res. 21, 1–14 (2021).
Yaya, S., Anjorin, S. S. & Adedini, S. A. Disparities in pregnancy—related deaths: Spatial and Bayesian network analyses of maternal mortality ratio in 54 African countries. BMJ Glob. Health https://doi.org/10.1136/bmjgh-2020-004233 (2021).
Manyeh, A. K., Nathan, R. & Nelson, G. Maternal mortality in Ifakara health and demographic surveillance system: Spatial patterns, trends and risk factors, 2006–2010. PLoS One 13, 2006–2010 (2018).
Carreno, I., Bonilha, A. L. L. & da Costa, J. S. D. Temporal evolution and spatial distribution of maternal death. Rev. Saude Publica 48, 662–70 (2014).
Siqueira, T. S. et al. Spatial clusters, social determinants of health and risk of maternal mortality by COVID-19 in Brazil: A national population-based ecological study. Lancet Reg. Health Am. 3, 100076. https://doi.org/10.1016/j.lana.2021.100076 (2021).
Haining, R., Law, J. & Griffith, D. Modelling small area counts in the presence of overdispersion and spatial autocorrelation. Comput. Stat. Data Anal. 53, 2923–37. https://doi.org/10.1016/j.csda.2008.08.014 (2009).
Gelman, A. & Price, P. N. All maps of parameter estimates are misleading. Stat. Med. 18, 3221–3234 (1999).
Congdon, P. Monitoring suicide mortality: A Bayesian approach. Eur. J. Popul. 16, 251–284 (2000).
Bernardinelli, L. et al. Bayesian analysis of space—Time variation in disease risk. Stat. Med. 14, 2433–43. https://doi.org/10.1002/sim.4780142112 (2007).
Knorr-Held, L. Bayesian modelling of inseparable space-time variation in disease risk. Stat. Med. 19, 2555–2567 (2000).
Goli, S., Puri, P., Salve, P. S., Pallikadavath, S. & James, K. S. Estimates and correlates of district-level maternal mortality ratio in India. PLOS Glob. Public Health 2, e0000441 (2022).
State, H., Sharma, A., Rana, S. K., Prinja, S. & Kumar, R. Quality of health management information system for maternal & child health care in Haryana state, India. PLoS ONE 11, e0148449 (2016).
Meghani, A., Rodríguez, D. C., Peters, D. H. & Bennett, S. Understanding reasons for and strategic responses to administrative health data misreporting in an Indian state. Health Policy Plann. 38, 150–60 (2023).
Author information
Authors and Affiliations
Contributions
SBN conceptualized, provided skeleton and supervised the overall study. HT reviewed the literature, compiled the data, developed methods, did the data analysis and prepared the first draft of the manuscript. AKP provided critical inputs during study implementation, reviewed literature on implementation of government schemes. PKK reviewed the literature and provided inputs for data analysis and reporting of study findings. SSM provided inputs for the manuscript and reviewed the manuscript. HT, SBN, AKP, PKK and SSM critically reviewed and approved the version of submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tolani, H., Neogi, S.B., Pandey, A.K. et al. Contributing factors for reduction in maternal mortality ratio in India. Sci Rep 14, 14883 (2024). https://doi.org/10.1038/s41598-024-65009-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-65009-0
- Springer Nature Limited