Abstract
Unplanned hospital readmission is a safety and quality healthcare measure, conferring significant costs to the healthcare system. Elderly individuals, particularly, are at high risk of readmissions, often due to issues related to medication management. Pharmacists play a pivotal role in addressing medication-related concerns, which can potentially reduce readmissions. This retrospective single-centre cohort study, conducted from November 2022 to February 2023 in an emergency department, aimed to determine if integrating emergency medicine pharmacists into Emergency Department care models reduces unplanned hospital readmissions within 28 days and to identify the interventions they employ. The inclusion criteria included patients aged ≥ 65, taking ≥ 3 medications, and presenting with falls, cognition changes, or reduced mobility and were planned for discharge to home from the emergency department. Collaborating with the Emergency Department Aged Care Service Emergency Team, a pharmacist provided comprehensive medication management consultations, discharge liaison services, and other pharmacy related interventions to eligible participants whenever the pharmacist was available. Patients who met the eligibility criteria but did not receive pharmacist interventions due to the pharmacist's unavailability served as the control group. This method was chosen to ensure that the control group consisted of comparable patients who only differed in terms of receiving the pharmacist intervention. The study included 210 participants, with 120 receiving pharmacist interventions and 90 acting as controls. The results revealed a significant reduction in unplanned hospital readmissions among participants who received pharmacist interventions (10.0%, n = 12) compared to controls (22.2%, n = 20), with a notable difference of 12.2% (95% confidence interval 2.4–23.4%, p = 0.01). A total of 107 interventions were documented, emphasising medication selection recommendations (28.0%) and identification of adverse drug reactions/drug-drug interactions (21.5%) as primary areas of focus. These findings suggest that integrating skilled pharmacists into Emergency Department Aged Care Service Emergency Team (ASET) lowered the rate of unplanned hospital readmission within 28 days resulting in improved hospital performance metric outcomes. This highlights the potential role of pharmacists in addressing medication-related issues and enhancing the quality and safety of healthcare delivery, particularly for elderly patients transitioning from the ED to home care settings.
Similar content being viewed by others
Introduction
In Australia, the rates at which patients are readmitted to the same facility within 28 days of discharge are a key performance indicator for safety and quality in healthcare1,2. Similar approaches for quantifying the performance of public health systems have been adopted in England, Scotland, the US and Canada3,4. Data from America5, France6, Belgium7, and Taiwan8 have reported readmission rates at 28 days to 6 weeks ranging from 10.7 to 23.6%. In 2015, the unplanned 28-day readmission rate from state health systems in Australia ranged from 3.29 to 10.9%2,3,10. Unplanned readmissions have a substantial financial burden on the healthcare system,3,4, estimated to cost Australia in the order of $1.5 billion annually11. Unplanned readmissions are also associated with overcrowding, hospitalisation-acquired complications and infections, iatrogenic harms, and poor health outcomes2,12.
Older patients are a high-risk group for hospital readmission13. The Australian Institute of Health and Welfare has estimated people aged 65 years and over accounted for 46% of all potentially preventable hospitalisations, and medication management was identified as a risk factor14.
Pharmacists are involved in medication history taking, medication reconciliation, and are in an optimal position to identify and address medication-related problems. They can identify and provide advice to manage polypharmacy, drug side-effects, drug interactions, identify deprescribing opportunities, and engage patients in medication education to improve knowledge and compliance, interventions that have been shown to reduce readmissions15,16.
In 2022, the Deeble Institute for Health Policy Research Queensland published a comprehensive review on strategies to mitigate unplanned hospital readmissions. The review concluded a model of care that employed multidisciplinary teams and multifaceted approaches resulted in improved patient care and were more successful in reducing unplanned readmissions12. Moreover, the tangible benefits of this approach have been exemplified in studies involving specific disease states, showcasing the efficacy of a collaborative strategy involving pharmacists in mitigating readmissions17,18,19.
In light of these insights, the concept of integrating emergency medicine pharmacists into allied healthcare teams within the Emergency Department (ED) emerges as a promising solution for reducing unplanned readmissions.
The primary aim of this study was to determine whether integrating an emergency medicine pharmacist into existing ED care teams that manage older patients led to a reduction in unplanned hospital readmissions within 28 days. A secondary aim was to examine the types of interventions carried out by the ED pharmacist.
Method
Study design
This study involved collecting prospective data collected from the quality improvement initiative and then reviewing patients' electronic medical records 28 days later to assess if they had any readmissions. It was conducted at the St George Hospital ED in Sydney, Australia. The quality improvement initiative occurred over a four-month period from November 2022 to February 2023. The project plan was reviewed by the South Eastern Sydney Local Health District Human Research Ethics Committee, and advised that as this was a quality improvement initiative it was exempt from formal ethics committee review. Permission to conduct an interview with participants by the pharmacist was sought as part of the clinical practice interaction. Written informed consent was deemed unnecessary by the ethics committee. This study was carried out in accordance with the standards for quality improvement reporting excellence (SQUIRE 2.0)20.
Participants
Patients were eligible for the study if they were referred to the Aged Care Service Emergency Team and/or the quick response program and were taking at least three chronic disease medications. Aged Care Service Emergency Team is an allied health service that supports elderly patients transitioning back to their own homes after discharge from the ED. The Aged Care Services Emergency Team works collaboratively with ED staff, participating in patient assessment and treatment. Quick response program, is an extension of Aged Care Service Emergency Team, focuses on providing short-term services to promote safe and independent living at home, aiming to reduce readmissions. Quick response program ensures that any pharmacy recommendations made during the ED presentation are implemented at home. Referral criteria are aged 65 years or older who are in the ED, are being considered for discharge home, and have one or more of the following: falls within the past 12 months, changes in cognition or behaviour, or concerns regarding safe mobility. Patients admitted to the hospital or discharged to nursing homes were not assessed by Aged Care Service Emergency Team and were excluded from the study.
Study group allocation
Participants were assigned to either the intervention or control groups based on the order of their referral, following a first-referred, first-intervened basis. Allocation decisions were made on each study day, with assignments to the intervention and control groups determined by the pharmacist’s availability. This approach aimed to minimize potential biases by ensuring that external factors, such as changes in the emergency department's patient load or staffing levels, did not influence the assignment process.
Each day, as patients were referred to the study, decisions were promptly made regarding their inclusion in the intervention group. Patients who did not receive the intervention on the same day were placed in the control group. By making these allocation decisions simultaneously, we aimed to balance the groups with respect to time-related variables and external conditions, thus enhancing their comparability.
On average, six patients were referred daily. The pharmacist did not have time to see all patients but included an average of four patients daily based on the time of referral. Patients the pharmacist did not have time to see were included in the control group.
Pharmacy intervention group
Patients who met the above criteria and received the pharmacy intervention based on the pharmacist availability were assigned to the intervention group. The intervention was delivered opportunistically by a single part-time pharmacist when available during business hours to conduct a comprehensive medication management. The pharmacist was available Monday, Tuesday and Wednesday each week. All participants in this group underwent a thorough medication history, sourced from at least two reliable references and medication reconciliation upon admission. Additionally, their attitudes toward medications and health were assessed to ensure sound knowledge of medications and compliance. Moreover, pathology review (renal and hepatic) was conducted for potential dosing adjustments as needed.
Types of pharmacist-led interventions included:
-
(1)
Change medication order/clarify medicine Instances where adjustments were made to the prescribed medication or inquiries were made to ensure clarity regarding a particular medicine.
-
(2)
Medication selection recommendation Recommendations put forth by the pharmacist that are clinically appropriate for the patient.
-
(3)
Discharge liaison service Pharmacy related services provided that facilitates the transition of patients from the hospital back to their homes or alternative care settings.
-
(4)
Therapeutic duplication Identification and rectification of instances where patients were prescribed multiple medications with similar or same therapeutic class.
-
(5)
Overdose Instances where the prescribed dosage exceeded the recommended guidelines.
-
(6)
Subtherapeutic dose or duration Cases where the prescribed dosage or duration of medication was insufficient for optimal therapeutic effect as per recommended guidelines.
-
(7)
Adverse drug reactions or drug–drug interaction Identification and management of adverse reactions.
-
(8)
Administrative issues Addressing administrative challenges related to medication dosage forms and providing appropriate dosage form alternatives.
-
(9)
Medication education Provision of education and information to patients regarding their medications, including dosage, administration, and potential side effects.
-
(10)
Deprescribing Initiatives aimed at reducing or discontinuing medications that are no longer clinically necessary or may pose risks when used long term.
On discharge, the medication reconciliation review included the following (focusing on new therapy):
-
Accuracy and completeness of the clinical provider completed discharge medication reconciliation by comparing home medications with new orders at discharge.
-
Review financial barriers of certain medications to ensure compliance after discharge.
-
Arrange a supply of discharge medication where needed
-
Identify drug interactions of newly commenced medications with home medications
-
Counselling patients/caregivers on the purpose and appropriate doses of medications. Provide written treatment plan and written information about the medications.
-
If there were changes to medications for a patient who had a dose administration aid, the ED pharmacist would follow-up with the patient’s local pharmacy to ensure that change to medication was communicated.
The quick response program team ensured that patients who were discharged had their pharmacy recommendations implemented.
Pharmacist documentation was a part of the intervention. Upon admission, the ED pharmacist would create a comprehensive medication list, which the ED medical officer would then use to reconcile medications. Following the completion of the medication management process, a detailed summary of the patient, including identified issues, recommendations, medication compliance review, and the updated medication list, would be documented in the patient's electronic medical record, and identifiable by the title 'Pharmacy Progress Note'. This documentation was accessible to all hospital clinical providers.
Control group
Control participants were patients referred to Aged Care Service Emergency Team on Mondays, Tuesdays and Wednesdays during the pharmacist’s working hours during the study period. However, they were not seen by the pharmacist as they presented at a time when the pharmacist’s services was not available due to competing demands.
Outcomes
The primary outcome was unplanned readmission to the ED within 28 days. Secondary outcomes included examining the types of interventions carried out by the ED pharmacist.
Data collection
The Aged Care Service Emergency Team maintained a record of all referrals made to the service as part of routine care. Participants were identified from this list. The ED Pharmacist maintained a record of those who received the intervention, as well as the type of interventions conducted. All other data were collected retrospectively from the electronic medical record, including the date of presentation, sex, age, degree of dependency (lives alone or with support), the reason for initial presentation, number of chronic medications on presentation, number of comorbidities, readmission within 28 days, and reason for readmission.
Statistical analysis
Descriptive categorical data are presented as total counts and proportions, while continuous variables are nonparametric and are presented as medians with interquartile ranges (IQRs). The primary outcome was presented as a difference in proportions with a 95% confidence interval and compared using the chi-square test. This analysis was performed using Microsoft Excel.
Ethics approval
The SESLHD Research Ethics Committee has confirmed that no ethical approval is needed.
Results
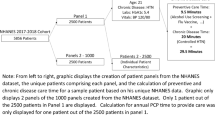
During the study period, Aged Care Service Emergency Team received 282 referrals, and 218 met the eligibility criteria. Pharmacy interventions were conducted on 128 patients; however, eight were subsequently admitted after review and excluded. This left 120 participants in the intervention group and 90 in the control group, as illustrated in Fig. 1. Table 1 shows the characteristics of the study participants. Unplanned hospital readmission occurred in 12 participants (10.0%) in the intervention group and 20 participants (22.2%) in the control group, a difference of 12.2% (95% confidence interval 2.4–23.4%, p = 0.01).
For those with a primary outcome event, the median time from first presentation to readmission was 14 days (IQR 7–22.5) in the intervention group and 16 days (IQR 8–22) in the control group. Table 2 presents reasons for initial presentation and subsequent readmission.
The study’s primary outcome, the risk ratio, was calculated to be 0.45 with a 95% confidence interval of 0.233–0.871. This indicates that the risk of unplanned hospital readmission within 28 days is approximately 45% lower in the intervention group compared to the control group. Additionally, the number needed to treat (NNT) to prevent one older adult from being readmitted within 28 days was estimated to be 8.17. This means that for every eight patients receiving the intervention, one fewer readmission would be expected within 28 days.
The secondary aim was to examine the types of clinical interventions made by the pharmacist’s participants in the intervention group. A total of 107 interventions were recorded and are shown in Table 3. Among these, medication selection recommendations were the most common, at 28.0% (n = 30), followed by adverse drug reactions and drug‒drug interaction recognition, at 21.5% (n = 23). Over 93% of the recommendations were proposed and implemented by the ED physician.
Discussion
In this study, we integrated a pharmacist into current Aged Care Service Emergency Team. The pharmacist’s primary focus was on optimising all aspects of patient medication management. While pharmacist interventions are not novel, what distinguishes our study is the strategic placement of a pharmacist within the Aged Care Service Team model and multifaceted pharmaceutical intervention, including medication review and interview. It's important to note that many studies on readmissions tend to focus on patients admitted to the hospital rather than those seen solely in the emergency department. However, the increasing trend of readmissions to the emergency department within one month, rising from 2.4% in 2010 to 3.1% in 2014, is concerning 21. Additionally, the elderly cohort represents the highest proportion of these readmission with statistics revealing a 6.2% per annum rise in readmission rates among those over 85 years of age 21, emphasising the urgent need for improved streaming processes within the hospital system to prevent these patients from being repeatedly assessed in the ED.
Potential solutions may include implementing multidisciplinary assessment areas, or enhancing geriatric outreach services. Our study contributes to this conversation by demonstrating that proactive interventions, such as integrating pharmacists into the Aged Care Service Emergency Team, can effectively reduce unplanned hospital readmissions. This highlights the potential benefits of such strategies in improving patient care and alleviating burdens on the healthcare system.
We found that the intervention was associated with a reduction in unplanned hospital readmissions within 28 days. This suggests that integrating pharmacists into models for managing older patients can optimise medication management and address potential issues that may lead to readmissions.
Several studies have examined the role of pharmacists within other interdisciplinary and multidisciplinary teams and have demonstrated reductions in hospital readmissions which aligns with our study17,18,19,22,23. These investigations have highlighted a diverse range of interventions orchestrated by pharmacists, who collaboratively engage with medical specialists, consultant nurses, and allied health professionals.
For example, several chronic obstructive pulmonary disease (COPD) specific care bundles that have investigated the inclusion of pharmacists as a strategy to decrease readmissions, with varying degrees of success reported in the literature. In a study by Gentene et al., it was found that pharmacists play a pivotal role in hospital-based transitions of care to lower COPD readmissions 18. The integration of a multidisciplinary team incorporating pharmacists into the care plan led to a reduction in COPD hospital 30-day readmission rates, from 22.7 to 14.7%18.
Similarly, Thurston et al. found that adding a pharmacist to the transitional care team that managing heart failure patients decreased the readmission rate from 33.7 to 21.3% in the intervention group17. The intervention group received the pharmacist-led intervention during their hospital stay and post discharge. The study also found an increase in self-reported patient medication adherence17.
Our study found that the Number Needed to Treat (NNT) is 8, meaning that for every 8 patients receiving our intervention, one fewer readmission would be expected. This indicates a potential benefit of our intervention in reducing hospital readmissions within 28 days.
According to the National Hospital Cost Data Collection (NHCDC), the average cost per emergency department presentation in 2020–21 is $78924. Therefore, if we effectively reduce readmissions within this cohort, the potential cost savings would be substantial.
Contributions from the pharmacist’s interventions may have influenced patients' initial presentation or, if left unidentified, could have potentially exacerbated their conditions, necessitating further medical attention. This demonstrates that the role of pharmacy practice extends beyond merely compiling medication histories and conducting patient interviews. However, as an integral component in preventing readmissions and highlighting the proactive stance in recognising medication-related issues may avert potential harm that could lead to repeat presentations.
Limitations
There are several limitations that need to be considered when interpreting the results of this study. This was a relatively small study, with an intervention carried out in a single institution by a single pharmacist, which limits the generalisability to other institutions and pharmacists. The data collected focused solely on readmissions within the hospital where the study was conducted, disregarding occurrences at other hospitals. Consequently, the data might underestimate the actual rates of readmissions.
This retrospective cohort study involved participants selected for the intervention on an opportunistic basis. It is acknowledged that the allocation method of first-referred, first-intervened is not equivalent to random allocation and may introduce selection bias. Specifically, this opportunistic selection process may have resulted in systematic differences between the intervention and control groups. Participants chosen to receive the intervention might have differed in their characteristics, reasons for hospital admission, and potential for having a medication-related reason for presentation or representation. Consequently, observed differences in outcomes may partly reflect these underlying differences rather than the effect of the intervention itself. To address this limitation, we have described the allocation process in detail in the method section. Despite these efforts, it is possible that selection bias influenced our findings, and this should be considered when interpreting the results.
Future studies should aim to use random allocation methods to more robustly assess the impact of pharmacist interventions. Randomised controlled trials would provide stronger evidence by minimising selection bias and ensuring comparable groups.
Conclusion
In this retrospective cohort study, the inclusion of a pharmacist in the Aged Care Service Emergency Team, responsible for managing older patients being discharged from the ED, was associated with a reduction in unplanned hospital readmissions within 28 days following discharge from the ED. These findings suggest that a collaborative intervention between healthcare professionals may have a positive impact on patient-centred care. To further validate and generalise these findings, a larger randomised multicenter study is necessary.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author upon reasonable request.
References
Australian Institute of Health and Welfare (AIHW). Australia’s hospitals 2016–17 at a glance (Australian Institute of Health and Welfare; Canberra, Australia, 2017).
Considine, J. et al. Factors associated with unplanned readmissions in a major Australian health service. Aust. Health Rev. 43, 1–9 (2019).
Australian Commission on Safety and Quality in Healthcare Avoidable Hospital Readmissions June https://www.safetyandquality.gov.au/sites/default/files/2019-08/d198961_acsqhc_avoidable_hospital_readmissions_literature_review_on_australian_and_international_indicators_july_2019.pdf. (Accessed 31 January 2023).
NSW Ministry of Health 20 March 2015. Unplanned Hospital Remissions, where to from here? https://www.health.nsw.gov.au/Performance/Documents/201503-unplanned-readmissions.pdf. (Accessed 31 January 2023).
Fethke, C. C., Smith, I. M. & Johnson, N. “Risk” factors affecting readmission of the elderly into the health care system. Med. Care 24, 429–437 (1986).
Lanièce, I. et al. Incidence and main factors associated with early unplanned hospital readmission among French medical inpatients aged 75 and over admitted through emergency units. Age Ageing 37(4), 416–422. https://doi.org/10.1093/ageing/afn093 (2008).
Comette, P. et al. Differential risk factors for early and later hospital readmission of older patients. Aging Clin. Exp. Res. 17(4), 322–328. https://doi.org/10.1007/BF03324617 (2005).
Lotus Shyu, Y. I., Chen, M. C. & Lee, H. C. Caregiver’s needs as predictors of hospital readmission for the elderly in Taiwan. Soc. Sci. Med. 58(7), 1395–1403. https://doi.org/10.1016/S0277-9536(03)00334-4 (2004).
WA Country Health Service Annual Report 2014–15. WA Country Health Service. Available at https://www.health.wa.gov.au/~/media/Files/Corporate/Reports-and-publications/Annual-reports/12856-wachs-annual-report-2015.pdf. (Accessed 09 September 2023).
Li, J. Y. Z., Yong, T. Y., Hakendorf, P., Ben-Tovim, D. I. & Thompson, C. H. Identifying risk factors and patterns for unplanned readmission to a general medical service. Aust. Health Rev. 39, 56–62 (2015).
Sahli, D. A new focus is needed on preventing unplanned hospital readmissions. Linked in. Available at: https://www.linkedin.com/pulse/new-focus-needed-preventing-unplanned-hospital-daryl-sahli?trk=hb_ntf_MEGAPHONE_ARTICLE_POST. (Accessed 17 May 2023). (2015).
Chua D., Johnson T. Evidence Brief. Avoiding hospital readmissions: the models and the role of primary care. Deeble Institute for Health Policy Research. no: 24, 19 May 2022. Available from https://ahha.asn.au/system/files/docs/publications/hospital_readmissions_reduction_primary_care_role_0.pdf. (Accessed 01 February 2023).
Franchi, C. et al. REPOSI investigators. Risk factors for hospital readmission of elderly patients. Eur. J. Intern. Med. 24(1), 45–51. https://doi.org/10.1016/j.ejim.2012.10.005 (2013).
Jencks, S. F., Williams, M. V. & Coleman, E. A. Rehospitalizations among patients in the medicare fee-for-service program. N. Engl. J. Med. 360(14), 1418–1428. https://doi.org/10.1056/NEJMsa0803563 (2009) (Erratum in: N Engl J Med.2011Apr21;364(16):1582).
Gallagher, D. et al. Inpatient pharmacists using a readmission risk model in supporting discharge medication reconciliation to reduce unplanned hospital readmissions: A quality improvement intervention. BMJ Open Qual. 11(1), e001560. https://doi.org/10.1136/bmjoq-2021-001560 (2022).
Lázaro Cebas, A. et al. Intervention by a clinical pharmacist carried out at discharge of elderly patients admitted to the internal medicine department: influence on readmissions and costs. BMC Health Serv. Res. 22, 167 (2022).
Thurston, M. M., Liao, T.-cV., Lim, T., Pounds, T. & Moye-Dickerson, P. M. Utilization of a multidisciplinary team to reduce the rate of hospital readmissions in high-risk heart failure patients at a community teaching hospital: The pharmacist’s role in transitions of care. J. Am. Coll. Clin. Pharm. 2(3), 281–287 (2019).
Gentene, A. J. et al. Multidisciplinary team utilizing pharmacists in multimodal, bundled care reduce chronic obstructive pulmonary disease hospital readmission rates. J. Pharm. Pract. 34(1), 110–116 (2021).
Blee, J. et al. Dispensing inhalers to patients with chronic obstructive pulmonary disease on hospital discharge: Effects on prescription filling and readmission. Am. J. Health Syst. Pharm. 72(14), 1204–1208 (2015).
Ogrinc, G. et al. SQUIRE 2.0 (standards for quality improvement reporting excellence): Revised publication guidelines from a detailed consensus process. BMJ Qual. Saf. 25(12), 986–992 (2016).
Dinh, M. M. et al. Trends and characteristics of short-term and frequent representations to emergency departments. Emerg. Med. Aust. 28, 307–312 (2016).
Eisenhower, C. Impact of pharmacist-conducted medication reconciliation at discharge on readmissions of elderly patients with COPD. Ann. Pharmacother. 48(2), 203–208 (2014).
Jack, B. W. et al. A reengineered hospital discharge program to decrease rehospitalization: A randomized trial. Ann. Intern Med. 150(3), 178–187 (2009).
National Hospital Cost Data Collection: Public sector report, 2020–21 financial year—June 2023. Accessed on 1 May 2023. Available from https://www.ihacpa.gov.au/sites/default/files/2023-06/national_hospital_cost_data_collection_report_public_sector_2020-21_0.pdf.
Acknowledgements
The authors also thank the members of the Aged Care Service Emergency Team and Quick Response Program Teams and the Emergency Department at St George for all their support in performing this research.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
S.T.N. had full access to all aspects of the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. S.T.N. and S.E.A. participated in the research design. S.T.N. and S.E.A. participated in the statistical analysis. S.T.N. and S.E.A. Participated in the writing of the paper. S.T.N supervised the study process and engaged key stakeholders including ASET, QRP and Emergency Department teams.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tran-Nguyen, S., Asha, S.E. A collaborative pharmacist-led intervention to prevent hospital readmissions among elderly patients discharged from the emergency department: a retrospective cohort study. Sci Rep 14, 15285 (2024). https://doi.org/10.1038/s41598-024-64968-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-64968-8
- Springer Nature Limited