Abstract
University nursing students have been shown to experience psychological stress. A mindfulness-based intervention (MBI) may be a helpful tool for stress management. The aim of this study was to examine the effects of a MBI on improving mindfulness and reducing perceived stress in nursing students. A quasi-experimental study was conducted between July 2021 and February 2022. The intervention group participated in an 8-week mindfulness awareness course, which included 50 min of training and practice in mindfulness meditation techniques each week. Over the same 8 weeks, the control group watched a 50-min film each week. The mindful attention awareness scale (MAAS) and perceived stress scale (PSS) were administered before the intervention, intervention completion, and 2 and 6 months after the intervention. Data were analyzed using t test and generalized estimating equation. Overall, that the MBI showed a substantial effect on felt stress in comparison to the control group. When compared to the control group, the MBI showed a substantial impact on trait mindfulness. The MBI was beneficial for nursing students and could be considered a viable approach in nursing education to enhance mental wellbeing. It could be an effective method of relieving stress in a high-stress population.
Similar content being viewed by others
Introduction
Mindfulness is an approach to the experience of everyday life that involves the nonjudgmental bringing of attention and awareness to the present moment1. It provides individuals with insight and knowledge about their present experiences, including their feelings, thoughts, physical states, consciousness, and environments, while encouraging openness, curiosity, and acceptance2,3. Mindfulness can reduce negative thoughts and those about the past and future, and is thought to relieve stress and anxiety and to improve individuals’ resilience3,4,5. The mindfulness-based intervention (MBI) created by Kabat-Zinn6 is an 8-week evidence-based program that aims to develop mindfulness, reduce stress, and, overall, improve mental functioning and health2,5,7,8,9. MBIs have been shown to effectively address a wide range of conditions and outcomes, including anxiety, depression, stress, disordered eating, chronic pain, quality of life, and psychological and emotional distress, in diverse populations10,11,12. Loucks et al.13 confirmed that MB-College establishes a groundwork of mindfulness abilities, including meditation, yoga, self-awareness, attention control, and emotion regulation, and offers recordings of varying lengths: 10, 20, 30, and 45 min. Students are encouraged to choose the duration that best suits them each day. Growing evidence indicates that MBIs help nurses to reduce stress, and they have been applied in nursing education14,15. However, evidence regarding their effectiveness for nursing students is scarce16.
Academic stress is the main stress type experienced by nursing students17. Due to its potential to affect academic achievement, stress has been recognized as a crucial psycho-social element in the educational process18. Students who participate in MBIs report experiencing less stress, more mindfulness, and/or greater empathy19. In a review, Chiodelli et al.20 confirmed that MBIs were beneficial to undergraduate students overall, findings on the effect of session length (45–120 min) and intervention duration (3–20 weeks) were not consistent. MBIs may be beneficial for nursing students, who according to the transactional analysis theory need to appraise how to manage their stress and emotions when confronting stressful events21,22. These students have limited opportunities to cope with various situations during their practice23, and they need to continually enrich their knowledge and experience over time to help them reduce stress23,24. Developed approach known as Mindfulness-Based Transactional Analysis (MBTA) integrates TA principles with encouraging mindful adult thinking, the authors describe the integration of mindfulness and transactional analysis theory into Mindfulness-Based Transactional Analysis (MBTA). This is an 8-week psychoeducational program that invites participants to cultivate full presence in everyday life, focusing on developing mindfulness capacity25,26. In a review, MBIs Transactional Analysis (TA) is applied in drug addiction, where craving beliefs are alleviated through a mindfulness-based TA intervention model. The efficacy of mindfulness-based transactional analysis group therapy in reducing craving beliefs among inpatients at the Indian Noida De-Addiction Center has been demonstrated27. The development team needs essential areas of knowledge to create effective Mindfulness-Based Programs tailored to particular populations or contexts. This suggests that mindfulness influences three aspects of self-regulation: attention control, self-awareness, and emotion regulation. Based on MBIs, MBSR, or MB-College, customization and responsive adjustments are continually made according to individual, group, and environmental needs. Teachers are constantly formulating and reformulating content to support participant learning, fine-tuning their teaching to ensure inclusivity and support the needs of individual participants and the entire group (e.g., The Mindfulness-Based Intervention (MBIs) is an evidence-based program lasting for 8 weeks, MBSR suggests the body scan is a 45-min exercise in which attention is directed to any areas of the body while lying down; MB-College offers recordings of varying lengths: 10, 20, 30, and 45 min. Students are encouraged to choose the duration that best suits them each day13,22,28. Therefore, nursing students in this study conform to other research suggesting that engaging in 45 min of mindfulness meditation followed by 5 min of physical recovery can achieve overall effectiveness.
Generally, nursing students have higher levels of stress than do other college students, due primarily to the highly demanding and rigorous nature of their professional educational programs23,29,30,31. In addition, nursing students entering clinical practice face major challenges and pressures, such as the need to bridge the gap between theory and practice, the feeling of being underprepared and fear of making mistakes; the need to deal with death and dying and to witness pain and suffering; the need to communicate well with clinical staff, teachers, and patients; and the unfamiliarity of the hospital environment24,32,33. The turnover rate for newly graduated nursing staff is high due to the long-term pressure experienced by those in the nursing profession33. However, burnout is indeed becoming increasingly prevalent among professional healthcare students. Burnout syndrome can manifest in any environment characterized by chronic stress, including academic settings34. Furthermore, university studies in fields like Nursing or Psychology, which are related to the healthcare system, present additional risk factors for developing burnout syndrome, such as exposure to human suffering and the responsibility for others’ health35. The incidence of burnout syndrome is significant among university students, with main stressors identified including concerns about exam performance, adapting to the university environment, study demands, and uncertainty about the future (González Ramírez and Landero Hernández 2007). Comprehending the occurrence and impacts of burnout within graduate healthcare programs enables faculty and administration to design curricula and offer information to students, helping them understand, identify, and seize opportunities to mitigate burnout, thereby fostering the development of enduring, high-quality clinicians36. This study was to test the efficacy of a mindfulness-based training program on reducing stress and increasing positive thinking of nursing students. Similar to their U.S. counterparts, nursing students in Taiwan experience stress and mindfulness, which may affect their academic and clinical performance. Therefore, this study was designed to examine the effects of the program on stress and mindfulness of nursing students in Taiwan.
Methods
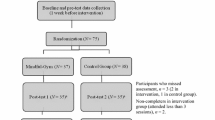
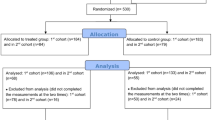
A longitudinal quasi‐experimental design, repeated-measures study was performed with a 6-month follow-up period to investigate the effects of an 8-week mindfulness awareness course on the mindfulness and perceived stress of nursing students before their clinical practice. Cluster randomization was employed to assign two classes to the experimental and control groups, mitigating the risk of contamination, as participants within clusters are likely to share experiences and similar learning environments.
Participants and setting
This study was approved by the Institutional Review Board (or Ethics Committee) of the Antai Medical Care Cooperation Antai-Tian-Sheng Memorial Hospital (protocol code, 21-045-B, and date of approval, 15 July 2021). This study followed the principles described in the Helsinki Declaration. All research activities were carried out in conformity with the applicable rules and regulations. The text includes a statement stating that all participants or their legal guardians provided informed consent. The recruitment period was July 2021–February 2022. Participants were third-year nursing students enrolled in the 5-year nursing program at a university, southern Taiwan. Eligible students spoke and read Mandarin or Taiwanese clearly; those who had taken a similar mindfulness course previously, regularly practiced mindfulness, or had completed their nursing practicum were excluded. All participants, and legal representatives of those aged < 20 years, provided written informed consent to study participation. The students received no credit for their participation.
The G*Power software (Ver. 3.1) was utilized to determine that the sample size was estimated to be 41 participants per group, with a power of 0.8, alpha of 0.05, and effect size of 0.25. This estimation was based on a repeated-measures between-factor analysis of variance of data collected from four assessment timepoints37.
Intervention
The intervention was based on the current MBI standard6 and the transactional theory concept that stress derives from relationships between people and their environments21. Participants in the experimental group took an 8-week mindfulness awareness course that included training and practice in mindfulness meditation techniques for 50 min/week. Those in the control group watched a 50-min film once a week for 8 weeks. An overview of the intervention content is provided in Table 1. The participants were taught by the first author who was trained to use mindfulness meditation techniques such as the body scan, a 30-min exercise in which the individual, while sitting in a relaxed position with the eyes closed, sequentially directs his or her attention to specific areas of the body and carefully observes how each area feels. Participants were instructed in meditation, with the direction of their attention to the sensations of breathing, tension, and relaxation. They also learned an exercise in which they focused on the feeling of rolling two wooden balls in the palm of the dominant hand for 15 min, repeating the movement dozens of times. They were taught to practice mindfulness skills in daily activities such as walking, standing, and eating. The participants were asked to practice the skills and techniques for 45 min/day, with a final 5-min period to return to the perception of all bodily sensations. After the completion of the course, the researchers used the LINE application38 to remind the participants in the intervention group to practice for at least one hour per week and during periods of low mood.
Measurements
Mindful attention awareness scale (MAAS)
The 15-item MAAS, developed by Brown and Ryan39, is used to determine the degree of individuals’ mindfulness. Respondents score items about inattentive states on a Likert scale ranging from 1 (almost always) to 6 (almost never). Participants were asked how frequently you currently had experienced. Higher scores reflect greater mindfulness39. The Cronbach’s α value for the original MAAS was 0.8139, and it was 0.83 in our study.
Perceived stress scale (PSS)
The 14-item PSS was developed by Cohen et al.40. It was used to measure the level of unpredictable, uncontrollable and overloaded stress experienced by the respondents in the past month. Responses are structured by a 5-point Likert scale (0 = never, 4 = always). Total scores range from 0 to 56, with higher scores reflecting more perceived stress40. The concurrent validity of the original scale was tested and Cronbach’s α values were 0.84–0.8640, and it was 0.79 in our study.
Data collection
Classes were randomly assigned to experimental and control groups due to the possibility of contamination. whereby participants within clusters are likely to have shared experiences and similar learning environments41. Before the start of the intervention (T0), the researcher explained the study purpose and procedures to the students and asked them to provide consent and to take 20–30 min to complete a questionnaire (the content of which was explained). At T0, items soliciting data on students’ gender (female or male), age, religious beliefs (yes or no), monthly family income (20,000–59,999 or > 60,000 NTD), and personality (e.g., extroverted, easy-going, conscientious, gentle, open-minded), and their parents’ teaching style (democratic, authoritative, permissive, uninvolved, or inconsistent) were included. The Mindful Attention Awareness Scale (MAAS) and Perceived Stress Scale (PSS) were administered at T0, upon completion of the intervention (T1), and at 2 (T2) and 6 (T3) months after the intervention.
Data analysis
The data were analyzed using SPSS 24.0 (IBM Corporation, Armonk, NY, USA). Categorical variables are reported as frequency and percentages and continuous variables are reported as mean and standard deviations. Differences between groups at the same timepoint were assessed using the t test. Considering time effects, a generalized estimating equation (GEE) was used to examine differences on MASS and PSS between groups at different time points42,43,44.
Ethical committee approval
This study was approved by the Institutional Review Board (or Ethics Committee) of the Antai Medical Care Cooperation Antai-Tian-Sheng Memorial Hospital (protocol code, 21-045-B, and date of approval, 15 July 2021). Additionally, we also registered our study on the ISRCTN registry with study registration number ISRCTN13821133 on May 24, 2024.
Results
An 8-week course on mindfulness-awareness, comprising weekly 50-min sessions of instruction and practice in mindfulness meditation techniques, was administered to participants in the experimental group. Meanwhile, participants in the control group watched a 50-min movie once a week for 8 weeks during the same period. Each participant was evaluated four times using the MASS and PSS scales: before the intervention (T0), immediately following the intervention (T1), 2 months after the intervention (T2), and 6 months after the intervention (T3). By comparing score differences at the four time points and changes in scores over time between the control and intervention groups, we assessed the intervention’s impact on MASS and PSS measures.
Mean MASS and PSS scores were plotted to illustrate group differences at the four assessment times. Baseline scores (T0) were similar between groups for all measurements. Over time, participants in the intervention group showed an increase in mean MASS scores (Fig. 1) and a decrease in mean PSS scores (Fig. 2). No adverse events or unexpected issues occurred during the intervention.
Participant characteristics
All of the 94 students (10 males, 84 females) whose eligibility was evaluated participated in this study and completed all procedures. The 49 participants, with mean age 18.22 (SD = 0.42) years old, were allocated to the intervention group, while the 45 participants, with mean age 18.27 (SD = 0.45) years old, were allocated to the control group. Their baseline characteristics are summarized in Table 2. More than 80% of the participants reported having religious beliefs and 34 students reported family incomes > $60,000 NTD. The participant characteristics did not differ between groups. No adverse event or unexpected issue occurred during the intervention.
Within-group changes in MAAS and PSS scores
The mean MAAS score increased and the PSS score decreased over time in the intervention group (Figs. 1, 2). The MAAS score was significantly higher at T2 and T3 than at T0 (t = 3.51, p = 0.001 and t = 4.17, p < 0.001, respectively); no significant difference was observed between T1 and T0 (Table 3). The PSS score was significantly lower at T3 than at T0 (t = − 3.52, p = 0.001), but did not differ from baseline at T1 or T2 (Table 3). No significant change in the MAAS or PSS score was observed in the control group (Table 3).
Between-group differences in MAAS and PSS scores at different timepoints
GEE modeling revealed between-group differences in the MAAS and PSS scores over time (Table 4). Group and time had no main effect on either score, but significant (group × time) interaction was found for the difference at T3 in the MAAS (Wald χ2 = 8.71, p = 0.003) and PSS (Wald χ2 = 4.84, p = 0.028) scores, reflecting improvements in the intervention group between T0 and T3. The difference in the MAAS and PSS scores between T0 and T3 were 0.51 and 3.32 points greater, respectively, in the intervention group than in the control group.
Correlations between the difference scores of MAAS and PSS at each stage compared to T0 in intervention group
We observed correlations between the increase in specific items of MAAS and the decrease in PSS at different time points (Table 5). The correlation coefficients between MAAS (T1 vs T0) and PSS (T1 vs T0), PSS (T2 vs T0), and PSS (T3 vs T0) were − 0.651 (p < 0.001), − 0.572 (p < 0.001), and − 0.551 (p < 0.001), respectively. For MAAS (T2 vs T0) and PSS (T2 vs T0), and PSS (T3 vs T0), the correlation coefficients were − 0.673 (p < 0.001) and − 0.648 (p < 0.001), respectively. Finally, the correlation coefficient between MAAS (T3 vs T0) and PSS (T3 vs T0) was − 0.759 (p < 0.001).
Discussion
Our findings supported our hypothesis that participants in the experimental group significantly increase mindfulness and decrease perceived stress over 6 months follow-up. Significantly differences were found on mindfulness and perceived stress for participants between two groups after 6 months follow-up. Our intervention was an 8-week mindfulness-based intervention and combined the LINE software to remind participants self-practice every day. Song and Lindquist22 MBSR program were the standard elements of yoga, sitting, walking, breath-work, body scan, and eating meditation.
One of the unique aspects of this study was that we scheduled an 8-week, 50-min weekly mindfulness meditation skill instruction and practice course. The course can be replicated in other ethnic groups and clinical units. The main technique is to use two mindfulness meditation techniques: The first is to conduct a 30-min body scanning technique practice through the instructor, allowing participants to scan the body during meditation and carefully observe every aspect of the body. Feel in each area, and focus on the awareness of breathing, walking, tension, and relaxation. The second is to use a 15-min wooden ball focus training, allowing participants to focus on the feeling of rolling the ball on the palm, teaching the body to focus on mindfulness, and guiding participants to apply it to daily activities, such as walking, standing and eating. In addition, the line software is another feature that continuously remind participants to practice daily life for the 6 months follow-up.
Mindfulness
The mindfulness significantly increased over time in the experimental group. Although no significantly improved after intervention immediately, it significantly increased at 2 months and 6 months after the intervention exception in intervention group. Additionally, significant differences of mindfulness were found between two groups after participants had received an 8 weeks intervention after 6 months. Our findings were confirmed as a 8 weeks mindfulness-based intervention was shown to be significantly beneficial to the nursing students. Our findings were similar to Horrillo Álvarez et al.45, but were not consistent with previous studies16,22. In Horrillo Álvarez et al.45 study, after 47 voluntary participants aged 20–60 received 8 weeks (total 8 h) of mindfulness training, there was no significant difference in mindfulness between the two groups after 8 weeks. However, the immediate effects were found in other two studies16,22. The possible reasons might be: (1) higher does and intensity training. In Song and Lindquist22 study, they provided 2 h per week and continued for 8 weeks (total 16 h). In Cheli et al.16 pre-post study design, the intervention was composed of five 3-hs sessions and 4.5 h (total 19.5 h). The dose provided by Cheli et al.16 is 2.44 times than ours (the total dose of this study is 8 h), and the interventions are all completed within 6 weeks. In Martínez-Rubio et al.36 study, they offered abbreviated programs (under 8 weeks), shorter sessions (90 min), brief practices (15 min or less), and prioritized training through informal practice. Furthermore, there was a significant emphasis on the effectiveness of mindfulness practice, particularly informal practice, as the primary means for personal transformation. In this program, participants were allocated 9 h for formal at-home practice, with sessions lasting 15 min each. Overall, the program is distinguished by its emphasis on short practice sessions and underscores the significance of informal practice in integrating mindfulness into daily routines. The current standard of mindfulness-based interventions, designed by Kabat-Zinn6, involves 26 h of session time consisting of eight weekly classes of 2.5 h each and an all-day 6-h class during sixth week46. According to the systematic review: the duration of mindfulness-based interventions is between 3 and 20 weeks, and the time of each section is diverse (40–120 min)20. More researches are needed to clarity this phenomenon. (2) Participants come from self-selection process that causes a biased sample to enhance the treatment effect in above studies. Thus, future intervention research should consider these issues to improve the outcomes.
In a review, Berghoff et al.47 confirmed that assessed the relationships among adherence, meditation practice time, and psychiatric symptoms following two 2-week mindfulness meditation interventions: one prescribing 10 min of daily meditation and another prescribing 20 min of daily meditation. The findings revealed no significant group difference in total days of meditation or overall meditation time. However, stress levels decreased and mindfulness increased over the 2-week period for both groups. Despite similar adherence rates, participants in the 20-min group reported greater increases in self-compassion compared to those in the 10-min group. Ma et al.48 programs like MBSR, MBCT, and their derivatives typically require a significant commitment to program sessions (usually eight weekly sessions of 2 h each) and home practice (45 min of daily practice), which may not resonate with university students and often leads to high dropout rates. This contradicts our research. The possible reasons might be: (1) Due to the younger age and higher compliance of our nursing students, we chose to follow Kabat-Zinn6 is an 8-week evidence-based program, which entails 50 min of training and practice. (2) During the long-term follow-up, there was no loss of our case count. Researchers used the LINE application to remind students to practice daily and record their progress.
Perceived stress
The results of this study show that the perceived pressure reached a significant difference at the 6th month (T3) after the intervention between two groups, indicating that the significant differences were found after participants practicing for 6 months. The perceived pressure did not decrease immediately after the intervention that were similar to the previous studies (Horrillo Alvarez et al. 2022)49, but not found in Kang et al.50, and Burger and Lockhart51. Our study did not show an immediate effect after the intervention. The reasons for this may include: (1) varied training time, such as the 17.5 h reported in the study by Kang et al.50 or 10 min of online videos per day for more than 4 weeks of practice in the study by Burger and Lockhart51. (2) According to the transactional model of stress and coping21, individuals, after assessing their stress levels, may make cognitive or behavioral adjustments to reduce the stress. In this study, the mindfulness scores in the experimental group increased over time and showed a significant increase at 2 months after the intervention. Additionally, perceived stress also exhibited a significant difference between the two groups at 6 months post-intervention. It is possible that participants gradually increased their mindfulness, leading to a reduction in perceived stress. Our findings revealed that mindfulness practice needs to be continued over a long period to achieve the expected benefits. This study confirmed that mindfulness practice can enhance self-awareness to help individuals adapt to stress4, and reduces stress among nursing students52,53. Therefore, our intervention, an 8-h training course before nursing practice, can be utilized to help nursing students continuously practice mindfulness skills on their own, enhancing mindfulness and reducing stress.
Therefore, regardless of the length or intensity of mindfulness practice, each study has its limitations. In the future, we must address and overcome these research challenges. The goal is to equip students with effective self-healing and stress-reducing techniques, enabling them to handle various clinical pressures. Our aim is to strengthen and empower students to become more resilient.
Conclusions
This study showed that an 8-h mindfulness-based training program for nursing students increased mindfulness and reduced perceived stress at 6 months after program completion. Thus, such training should be promoted for nursing students, with the recognition that continual practice over time is needed to fully integrate mindfulness skills. Our findings show that mindfulness practice needs to be continued for 6 months period to achieve the expected benefits, and confirm that mindfulness practice enhances self-awareness to adapt to stress and reduces stress among nursing students. Thus, our intervention can be feasibly implemented before nursing students enter their practice, followed by the continuous practice of the skills learned to enhance mindfulness and reduce stress.
In the future, more nursing students can benefit from mindfulness skills exercises, allowing them to feel more at ease during clinical practice. This approach may also help reduce the turnover rate among clinical nursing staff.
Limitations
This study was limited by the inclusion only of participants from the nursing program of a single technological university, which reduces the generalizability of the findings. Additionally, to accurately ascertain the effects of MBIs, studies conducted with larger and more diverse participant samples are needed. Despite these limitations, however, we provide a structured 8-h mindfulness-based course for nursing students that had measurable beneficial effects.
Data availability
It was not publicly available for the dataset during the current study since they contain potentially identifiable information for each participant; however, it is available from the corresponding author upon reasonable request.
References
Grossman, P. Defining mindfulness by how poorly I think I pay attention during everyday awareness and other intractable problems for psychology’s (re)invention of mindfulness: Comment on Brown et al. (2011). Psychol. Assess. 23(4), 1034–1040 (2011).
Hofmann, S. G. & Gomez, A. F. Mindfulness-based interventions for anxiety and depression. Psychiatr. Clin. N. Am. 40(4), 739–749. https://doi.org/10.1016/j.psc.2017.08.008 (2017).
Tai, Y. M., Yang, S. N. & Cheng, S. L. Effect of mindfulness training (body scan) on the five-item brief symptom rating scale of depressive inpatients of military personnel: A pilot study. Taiwan. J. Psychiatry 32(5), 306–313 (2018).
Kabat-Zinn, J. Mindfulness-based interventions in context: Past, present, and future. Clin. Psychol. Sci. Pract. 10, 144–156. https://doi.org/10.1093/clipsy/bgp016 (2003).
Koren, M. E. Mindfulness interventions for nursing students: Application of modelling and role modelling theory. Int. J. Caring Sci. 10(3), 1710–1716 (2017).
Kabat-Zinn, J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. Gen. Hosp. Psychiatry 4(5), 33–47 (1982).
Crane, R. S. et al. Development and validation of the mindfulness-based interventions—Teaching assessment criteria (MBI:TAC). Assessment 20(6), 681–688. https://doi.org/10.1177/1073191113490790 (2013).
Gu, J., Strauss, C., Bond, R. & Cavanagh, K. How do mindfulness-based cognitive therapy and mindfulness-based stress reduction improve mental health and wellbeing? A systematic review and meta-analysis of mediation studies. Clin. Psychol. Rev. 37, 1–12. https://doi.org/10.1016/j.cpr.2015.01.006 (2015).
Scheepers, R. A., Emke, H., Epstein, R. M. & Lombarts, K. The impact of mindfulness-based interventions on doctors’ well-being and performance: A systematic review. Med. Educ. 54(2), 138–149. https://doi.org/10.1111/medu.14020 (2019).
Baer, R. A. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clin. Psychol. Sci. Pract. 10(2), 125–143. https://doi.org/10.1093/clipsy.bpg015 (2003).
Simpson, R. et al. Mindfulness-based interventions for mental well-being among people with multiple sclerosis: A systematic review and meta-analysis of randomised controlled trials. J. Neurol. Neurosurg. Psychiatry 90(9), 1051–1058. https://doi.org/10.1136/jnnp-2018-320165 (2019).
Zhang, D., Lee, E. K. P., Mak, E. C. W., Ho, C. Y. & Wong, S. Y. S. Mindfulness-based interventions: An overall review. Br. Med. Bull. 138(1), 41–57. https://doi.org/10.1093/bmb/ldab005 (2021).
Loucks, E. B. et al. Mindfulness-based college: A stage 1 randomized controlled trial for emerging adult well-being. Psychosom. Med. 83(6), 602–614. https://doi.org/10.1097/PSY.0000000000000860 (2021).
Chen, X. et al. The effects of mindfulness-based interventions on nursing students: A meta-analysis. Nurse Educ. Today 98, 1–8. https://doi.org/10.1016/j.nedt.2020.104718 (2021).
McVeigh, C. et al. Mindfulness-based interventions for undergraduate nursing students in a university setting: A narrative review. Healthcare 9, 11. https://doi.org/10.3390/healthcare9111493 (2021).
Cheli, S., De Bartolo, P. & Agostini, A. Integrating mindfulness into nursing education: A pilot nonrandomized controlled trial. Int. J. Stress Manag. 27(1), 93–100. https://doi.org/10.1037/str0000126 (2020).
Ali, A. M. & El-Sherbini, H. H. Academic stress and its contributing factors among faculty nursing students in Alexandria. Alexand. Sci. Nurs. J. 20(1), 163–181 (2018).
Jimenez, C., Navia-Osorio, P. M. & Diaz, C. V. Stress and health in novice and experienced nursing students. J. Adv. Nurs. 66(2), 442–455 (2010).
Drew, B. L. et al. Care for the caregiver: Evaluation of mind-body self-care for accelerated nursing students. Holistic Nurs. Pract. 30(3), 148–154. https://doi.org/10.1097/HNP.0000000000000140 (2016).
Chiodelli, R. et al. Mindfulness-based interventions in undergraduate students: A systematic review. J. Am. Coll. Health 70(3), 791–800. https://doi.org/10.1080/07448481.2020.1767109 (2022).
Lazarus, R. S. & Folkman, S. Stress, Appraisal and Coping (Springer, 1984).
Song, Y. & Lindquist, R. Effects of mindfulness-based stress reduction on depression, anxiety, stress and mindfulness in Korean nursing students. Nurse Educ. Today 33, 86–90 (2015).
Evans, W. & Kelly, B. Pre-registration diploma student nurse stress and coping measures. Nurse Educ. Today 24(5), 473–482. https://doi.org/10.1016/j.nedt.2004.05.004 (2004).
Yildiz Findik, U., Ozbas, A., Cavdar, I., Yildizeli Topcu, S. & Onler, E. Assessment of nursing students’ stress levels and coping strategies in operating room practice. Nurse Educ. Pract. 15(3), 192–195. https://doi.org/10.1016/j.nepr.2014.11.008 (2015).
Žvelc, G., Černetič, M. & Košak, M. Mindfulness-based transactional analysis. Trans. Anal. J. 41(3), 241–254. https://doi.org/10.1177/036215371104100306 (2011).
Sheoherd, G. “Normally I’d get really agitated, but I just laughed!”: What do participants reflect upon in a transactional analysis/mindfulness based anger management programme? Br. J. Guid. Counsel. 48(4), 537–551 (2020).
Khurana, U., Hai, K. & Nayar-Akhtar, M. Effects of mindfulness based transactional analysis on craving belief: An interventional plan. Boletín De Literat. Oral 11, 2633–2640 (2023).
Loucks, E. B. et al. Mindfulness-based programs: Why, when, and how to adapt? Glob. Adv. Health Med. 11, 1–12. https://doi.org/10.1177/21649561211068805 (2022).
Chernomas, W. M. & Shapiro, C. Stress, depression, and anxiety among undergraduate nursing students. Int. J. Nurs. Educ. Scholarship 10(5), 255–266. https://doi.org/10.1515/ijnes-2012-0032 (2013).
Labrague, L. J. et al. A literature review on stress and coping strategies in nursing students. J. Mental Health 26(5), 471–480. https://doi.org/10.1080/09638237.2016.1244721 (2017).
Timmins, F. & Kaliszer, M. Aspects of nurse education programmes that frequently cause stress to nursing students fact-finding sample survey. Nurse Educ. Today 22(3), 203–211 (2002).
Labrague, L. J. et al. Stress and coping strategies among nursing students: An international study. J. Mental Health 27(5), 402–408. https://doi.org/10.1080/09638237.2017.1417552 (2018).
Turner, K. & McCarthy, V. L. Stress and anxiety among nursing students: A review of intervention strategies in literature between 2009 and 2015. Nurse Educ. Pract. 22, 21–29. https://doi.org/10.1016/j.nepr.2016.11.002 (2017).
Caballero, D. C. C., Breso, É. & Gutiérrez, O. G. Burnout en estudiantes universitarios. Psicol. Desde El Caribe 32(3), 424–441 (2015).
Bullock, G. et al. The prevalence and effect of burnout on graduate healthcare students. Can. Med. Educ. J. 8(3), 90–108 (2017).
Martinez-Rubio, D. et al. Protective role of mindfulness, self-compassion and psychological flexibility on the burnout subtypes among psychology and nursing undergraduate students. J. Adv. Nurs. 77(8), 3398–3411. https://doi.org/10.1111/jan.14870 (2021).
Faul, F. & Erdfeler, E. G*power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical science. Behav. Res. Methods 39(2), 175–191 (2007).
LINE Corporation. https://Careers.Linecorp.com/ (2003).
Brown, K. W. & Ryan, R. M. The benefits of being present: Mindfulness and its role in psychological well-being. J. Person. Soc. Psychol. 84(4), 822–848. https://doi.org/10.1037/0022-3514.84.4.822 (2003).
Cohen, S., Kamarck, T. & Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 24, 385–396 (1983).
Cook, A. J., Delong, E., Murray, D. M., Vollmer, W. M. & Heagerty, P. J. Statistical lessons learned for designing cluster randomized pragmatic clinical trials from the NIH Health care systems collaboratory biostatistics and design core. Clin. Trials 13(5), 504–512. https://doi.org/10.1177/1740774516646578 (2016).
Ballinger, G. A. Using generalized estimating equations for longitudinal data analysis. Organ. Res. Methods 7(2), 127–150 (2004).
Hanley, J. A., Negassa, A., Edwardes, M. D. D. & Forrester, J. E. Statistical analysis of correlated data using generalized estimating equations: An orientation. Am. J. Epidemiol. 157(4), 364–375. https://doi.org/10.1093/aje/kwf215 (2003).
Wang, M. Generalized estimating equations in longitudinal data analysis: A review and recent developments. Adv. Stat. 2014, 1 (2014).
Horrillo Álvarez, B., Marin Martin, C., Rodriguez Abuin, M. & Orio Ortiz, L. Short mindfulness meditation training: Does it really reduce perceived stress? Cogn. Process. 23(5), 559–568. https://doi.org/10.1007/s10339-022-01108-y (2022).
Kabat-Zinn, J. Full Catastrophe Living: Using the Wisdom of Your Body and Mind to Face Stress, Pain and Illness (Delacorte, 1990).
Berghoff, C. R., Wheeless, L. E., Ritzert, T. R., Wooley, C. M. & Forsyth, J. P. Mindfulness meditation adherence in a college sample: Comparison of a 10-min versus 20-min 2-week daily practice. Mindfulness 8, 1513–1521 (2017).
Ma, L., Zhang, Y. & Cui, Z. Mindfulness-based interventions for prevention of depressive symptoms in university students: A meta-analytic review. Mindfulness 10, 2209–2224 (2019).
Bultas, M. W., Boyd, E. & McGroarty, C. Evaluation of a brief mindfulness intervention on examination anxiety and stress. J. Nurs. Educ. 60(11), 625–628. https://doi.org/10.3928/01484834-20210913-04 (2021).
Kang, Y. S., Choi, S. Y. & Ryu, E. The effectiveness of a stress coping program based on mindfulness meditation on the stress, anxiety, and depression experienced by nursing students in Korea. Nurse Educ. Today 29(5), 538–543. https://doi.org/10.1016/j.nedt.2008.12.003 (2009).
Burger, K. G. & Lockhart, J. S. Meditation’s effect on attentional efficiency, stress, and mindfulness characteristics of nursing students. J. Nurs. Educ. 56(7), 430–434 (2017).
Pipe, T. B. et al. Nurse leader mindfulness meditation program for stress management: A randomized controlled trial. J. Nurs. Admin. 39, 130–137 (2009).
van der Riet, P., Rossiter, R., Kirby, D., Dluzewska, T. & Harmon, C. Piloting a mindfulness program for undergraduate nursing students: Student feedback and lessons learned. Nurse Educ. Today 35, 44–49. https://doi.org/10.1016/j.nedt.2014.05.003 (2015).
Acknowledgements
The authors thank all the participants and co-investigator involved with this study. Additionally, all the authors thank the students who generously gave of their time to complete the questionnaire. They gratefully acknowledge the participants for their participants and their valuable information.
Author information
Authors and Affiliations
Contributions
Y.L.L.: Conceptualization, Methodology, Data collection, Formal analysis, Writing Original Draft. L.M.W.: Methodology, Validation, Formal analysis, Writing-Review & Editing. C.H.L.: Methodology, Formal analysis. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liu, YL., Lee, CH. & Wu, LM. A mindfulness-based intervention improves perceived stress and mindfulness in university nursing students: a quasi-experimental study. Sci Rep 14, 13220 (2024). https://doi.org/10.1038/s41598-024-64183-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-64183-5
- Springer Nature Limited