Abstract
The importance of integrated care for complex, multiple long term conditions was acknowledged before the COVID pandemic but remained a challenge. The pandemic and consequent development of Long COVID required rapid adaptation of health services to address the population’s needs, requiring service redesigns including integrated care. This Delphi consensus study was conducted in the UK and found similar integrated care priorities for Long COVID and complex, multiple long term conditions, provided by 480 patients and health care providers, with an 80% consensus rate. The resultant recommendations were based on more than 1400 responses from survey participants and were supported by patients, health care professionals, and by patient charities. Participants identified the need to allocate resources to: support integrated care, provide access to care and treatments that work, provide diagnostic procedures that support the personalization of treatment in an integrated care environment, and enable structural consultation between primary and specialist care settings including physical and mental health care. Based on the findings we propose a model for delivering integrated care by a multidisciplinary team to people with complex multisystem conditions. These recommendations can inform improvements to integrated care for complex, multiple long term conditions and Long COVID at international level.
Similar content being viewed by others
Introduction
Efforts to establish integrated care for people with complex, multiple long term conditions (also termed multimorbidity) have been made since the 1990s because of the rise of long term conditions in all age groups and the associated costs1,2. Integrated care pathways (ICPs) provide care for people who need input from a combination of providers, such as primary care and specialist general hospital care for long term conditions3,4. The NHS proposed to provide integrated care using structured, multidisciplinary care plans coordinated across specialties, investigations, treatments and rehabilitation to improve outcomes for patients with long term conditions and complex needs5. This was achieved through disease management and chronic care models such as collaborative care for single disease models or care pathways for conditions such as diabetes, cardiovascular disease, chronic obstructive pulmonary disease (COPD) or rheumatoid conditions6,7,8,9,10,11.
More recent efforts aimed to incorporate integrated approaches into the care of complex, multiple long term conditions. These are chronic conditions affecting multiple systems and have a significant impact on life, requiring stepwise approaches to interventions and subsequent monitoring. Those treatments encompass a range of interventions such as medications, surgical interventions, psychotherapy, education about the condition and self-management as well as lifestyle interventions, delivered by a multidisciplinary team12,13. Initially they were especially developed for older people14, but evolved towards developing integrative approaches to care management including for comorbid somatic and mental disorders15,16,17,18,19,20,21,22,23,24. The COVID-19 pandemic resulted in a surge in new long term conditions which placed additional strain on health services worldwide, combined with service provision for pre-existing conditions having to be maintained2. This has reinforced the ongoing and urgent need for integrated care.
Long COVID is a new long term condition, which has been defined by the World Health Organization as ‘the continuation or development of new symptoms 3 months after the initial SARS-CoV-2 infection, with these symptoms lasting for at least 2 months with no other explanation’25. Long COVID cannot, at present, be cured, but is controlled by medication or other treatments26,27. It affected 2 million people in the UK in 202328 and at least 65 million globally29. It is a complex, heterogeneous, multisystem condition which significantly impacts the lives of those affected. Research indicates that 57% of people with Long COVID experience at least one persistent symptom 12 months post-infection30. Since 2020, the NHS has set up more than 100 Long COVID services across England31,32. Combined with the recent establishment of integrated care boards aiming to improve the quality of care and support for those with complex multiple long term conditions3, the development of Long COVID services provides a timely opportunity to inform the optimal set-up of ICPs for complex multiple long term conditions, incorporating learning from the establishment of Long COVID care pathways. An example of potential models for ICPs managing recovery in Long COVID and other LTCs is shown in Table 1 below33.
The approach that was taken in the Long COVID clinics enforced many aspects of integrated care pathways that had been theoretically defined but rarely implemented before the pandemic. The sense of urgency and the need to work swiftly on this obviously multisystem condition forced the swift development of integrated care models in Long COVID clinics. The learning from this experience could provide insights for the development of integrated care pathways for other long term conditions, that had until then remained underdeveloped.
To-date, research has not considered learning from Long COVID health care systems development, to inform integrated care for complex, multiple long term conditions. Additionally, as the set-up of Long COVID clinics could differ by region, it would both be relevant to understand how to better manage Long COVID, and how to better use ICPs for all diseases.
Both the literature on Long COVID and on the importance of integrated care for long term conditions are limited. Moreover, how such care should be implemented depends on policies in the respective countries, that may differ. Therefore, a Delphi study to be conducted amongst experts in the domain of long term conditions, Long COVID and integrated care seemed the right way to proceed to develop priorities for integrated care pathways for Long COVID and long term conditions. Relevant experts were considered to be healthcare providers as well as care users with experience in the conditions of interest. A Delphi study uses a structured method for collecting the opinions of experts (called panelists), concerning a subject of their expertise. This is done anonymously, with each voice counting equally and not being subject to social pressure to adhere to a dominant vision. The essence is an exploration of expert views on a particular topic and then giving the option to the experts to react to the input of the other experts in an iterative procedure which can comprise several rounds of enquiry. Following an initial round of information gathering, a summary of expert opinions is provided to panelists to inform the next round, and so on until consensus is achieved34,35.
This article reports the findings of a Delphi consensus study which was conducted in line with the NHS England commitment to improve the involvement of patients in healthcare36. The Delphi research group believe that the patient viewpoint can enhance the quality of research and care provision; as such we chose a definition of integrated care that is close to the experience of patients with sometimes multiple long term conditions: “I can plan my care with people who work together to understand me and my carer(s), allow me control, and bring together services to achieve the outcomes important to me”37.
The aim of our study is to inform the optimal set-up of ICPs for complex multiple long term conditions, incorporating learning from the establishment of Long COVID care pathways, and how to better manage Long COVID. To this goal, we report the findings of a Delphi consensus study based on patient and health care provider experience.
We explored:
-
1.
Key enabling elements for effective ICPs for Long COVID and strengths of existing ICPs for long term conditions.
-
2.
Which part of an ICP model for Long COVID might be transferred to long term conditions without sufficiently developed care pathways, and how could they be integrated.
Results
In an 18-month process, following three conferences of the expert group and two surveys providing 461 patient and 180 health care professional experiences with long term conditions (n = 365) or Long COVID (n = 276), this study yielded priorities for integrated care for Long COVID and for long term conditions. Most patients reporting on long term conditions suffered from multimorbidity or complex multiple long term conditions.
Round one
Table 2 provides demographic characteristics for participants of Surveys 1 and 2. As round 1 was intended to gather information about important characteristics of integrated care pathways (ICPs) for Long COVID and for long term conditions, a detailed description of the responses from survey 1 and how they informed survey 2 questions is available via this link https://www.york.ac.uk/media/healthsciences/documents/research/mentalhealthresearch/STIMULATE-ICP%20Delphi%20Responses%20Table.pdf.
Round 2
In round 2 (Establishing consensus and ranking), Survey 2 findings identified ten statements which achieved 80% consensus; these were the same for both Long COVID and long term conditions and are presented in Table 3. Color coding illustrates the similarities and differences in rank order between statements for Long COVID care and long term condition care.
The top two statements for both Long COVID and long term conditions were:
-
1.
Ensure the person is listened to, acknowledged, supported and believed, thus validating their experience and knowledge.
-
2.
Provide appropriate diagnostic assessment, which is person-centered, to rule out other conditions, aiming to confirm a diagnosis.
The following three statements were ranked between 3 and 5 for Long COVID and other long term conditions:
-
3.
Provide evidence-based treatment and recommendations
-
4.
Ensure services have sufficient and appropriate resources, including funding
-
5.
Ensure clinicians and services provide knowledge and understanding of symptoms and services available to patients
Numbers 6 and 7 are ranked the same for both conditions, and the last three are ranked between 8 and 10.
Round 3
Subsequently in round 3 (Developing policy recommendations), fifteen policy recommendations were developed based on the expert panel discussions about those ten statements. These recommendations concern four domains: diagnosis, resources, training and research. Recommendations, outlined in Table 4, include sufficient time with clinicians to assess the problem or condition and offer timely access to diagnostic investigations; research to provide evidence-based treatment and rehabilitation; appropriately resourced services with funded time for specialist consultant contributions to multidisciplinary care and routine follow-up appointments; and training to increase the knowledge and understanding of health care professionals, communities and employers.
Discussion
Key priorities identified in this work center around evidence-based support, provided by services with appropriate resources (including funding) and clinicians who are knowledgeable and understanding of symptoms and aware of the available services. Care should be offered in in a timely and consistent manner, with easy access through multi-disciplinary teams. Healthcare should include long term support, reviews, personalized care plans and a care coordinator. Self-management advice should be provided in line with individual needs, as should personalized evidence-based fatigue management. Personalized continuity of care was also prioritized. The findings of this Delphi study show that priorities identified for long term conditions are very similar to those for Long COVID, a recently established condition. Both patients and health care providers envisioned priorities with a high consensus rate of 80%. The two top priorities were to ensure the person is listened to, acknowledged, supported and believed, thus validating their experience and knowledge; and to provide appropriate diagnostic assessment, which is person centered, to rule out other conditions, aiming to confirm a diagnosis.
These findings indicate the importance of validating the patient experience and providing adequate diagnostics when planning care for complex conditions. The Health Committee of the House of Commons stated that in view of multimorbidity, the person should be treated, not the condition, and that the single-disease framework on which the NHS mainly operates is less successful in treating people with complex multiple long term conditions38. The patient and healthcare provider priorities which we identified led to the development of policy recommendations which resonate with this statement.
It is not surprising that priorities concerned with taking the patient seriously and performing adequate diagnostic assessments were important for Long COVID, as this is a new condition with many diagnostic uncertainties, and patients were actively discouraged from seeking help from their primary care physician in the initial phase of the pandemic to reduce cross-infection risks39,40,41. In contrast, the fact that patients and clinicians gave the same priority and ranking for other long term conditions was an unexpected and novel finding. The COVID-19 pandemic resulted in organizations struggling to meet previous objectives for long term condition management42. Therefore, these priorities could reflect the strain on current health care services. On the other hand, the wish to prioritize the validation of patient experiences and the provision of adequate diagnostics could indicate that the challenges of implementing integrated care into routine practice pre-dated the COVID-19 pandemic43. Given the level of importance placed on diagnosis by Delphi participants in this study, Box 1 shows an example of how a single response made by a participant with lived experience of Long COVID was categorized at each stage of this Delphi, and subsequently contributed to policy recommendations relating to Diagnosis.
The expert panel from this study recommended that the experiences with the newly formed Long COVID clinics could offer an opportunity to innovate integrated care within a complex care pathway. Long COVID clinics bring multiple providers together to meet needs broader than has historically been possible for many complex long term conditions, and evaluations of Long COVID clinics indicate that accessing a virtual multidisciplinary team without additional referrals has enhanced the ‘one team’ approach44. This has facilitated knowledge exchange and enhanced the integration of primary and specialist care for Long COVID; it also minimized referrals to single-specialty services. In addition, this approach is able to facilitate appropriate allocation of resources for further investigation, action plans for correct diagnosis provision and treatment for personalized complex care management45. The policy recommendations outlined in Table 4 reflect the agreed statements and concern four aspects of care: diagnostics, resources, training of health care providers, and research to develop evidence-based treatment and rehabilitation programs for Long COVID, and also to evaluate integrated care models and their cost-effectiveness for complex long term conditions. Consequently, in this paper we propose an overall model of care which could be replicated and further developed to ensure consistency in the delivery of services nationally, and to inform similar changes internationally.
This study suggests that more effective coordination and workforce planning, to support specialist input into care plans, should be prioritised in integrated care. There is a need to provide resources for the introduction of multi-disciplinary team case discussions and structurally embedding consultation with specialists into primary care, including for mental health. Introducing this for complex, multiple long term conditions would be novel and would reduce multiple onward referrals. Other innovative recommendations would be: (i) enhanced workforce training to support skills transference and interdisciplinary learning; (ii) support by local public health teams for public health campaigns; (iii) tracking access to services and patient outcomes of service provision; and (iv) benchmarking of quality of care and service improvement. Inclusion of public health contributions and workforce training is not typically incorporated into integrated care pathways; however, these align with the broader objectives of disease management programmes to improve health or prevent disease, and to enhance the cost effectiveness of an ICP.
Integrated care has previously been located in primary care or the hospital setting46,47. New post-pandemic aspects of integrated care, indicated by the expert panel and based on the findings of this work, include resource provision for better integration of specialist care relevant to multiple conditions within primary care, such as the structural embedding of secondary care consultation specialists without the need for separate referrals. Additionally, the innovation of virtual multidisciplinary teams supported by primary, secondary, tertiary, community, physical and mental health care specialists and their subsequent implementation offers an opportunity to broaden the number of integrated care pathways beyond Long COVID to other complex conditions and to provide care to community-managed patients without requiring multiple referrals48,49. The leading principle should be that access to care is not enough; people need access to effective care and treatments which could be attained by personalization of care within a model of vertical integration between primary and specialist care, the support of multidisciplinary teams and monitoring by a care manager with expertise relevant to the care of complex multiple long term conditions.
The health economic impacts of implementing our proposed solutions require further evaluations to determine the value of having the necessary expertise available in meetings, compared with the cost of consultant time, multiple referrals and discharges, opportunity costs for staff and associated societal costs for fragmented care like loss of productivity and travel. To prioritize a person’s comprehensive needs in a single ICP requires broadening the available options and incorporating integrated psychiatric treatment and vocational rehabilitation. This must balance with competing costs and workforce demands. The current crisis in health care and the increasing burden of complex, multiple long term conditions demands urgent solutions, which may mean increasing resources. However, given the limited resources and the challenges to dealing with complex, multiple long term conditions that have become apparent, it should maximize the use of current resources towards integrating services, avoiding stacking treatment for each condition by making lean, personalized treatment programs. In addition, diagnostic centers available for some health conditions could be expanded to cater for a wider variety of complex conditions; better links between these centers and the broader health care environment could be made.
This work was completed in the UK; but, given the pandemic context and international efforts to establish integrated care, we deem the results to be relevant internationally. Our findings align with international recommendations for multiple long term condition care since the start of the COVID-19 pandemic. In Australia, increased primary care funding has been identified to increase the length of consultations to enable Primary Care Physicians to fully understand the presenting problem(s)50. In the USA, 40 Long COVID clinics were established and calls for changes to service configuration have been made to support the care of people with complex multiple long term conditions, integrating appropriate services to provide coordinated patient-centered care23,51. In Europe, studies have reported some of the logistical adaptations needed to provide these services in the context of the pandemic, both for comorbid mental disorders in the general hospital setting52 and for the diagnosis of Long COVID in the primary care setting53,54. In Africa, health care organization, delivery system design, a clinical information system, self-management support, community linkages, and trained educators and decision support to link informed, activated patients and prepared proactive teams are identified as critical components of collaborative care for complex multiple long term conditions55. However, it should be noted that these studies were performed from the researchers’ and providers’ perspective and did not include patients’ views. Our study now presents the view of patients and health care providers working across primary, secondary and acute specialty care including specialty mental health care on priorities for integrated care.
This study is of great clinical need; Long COVID is a major problem for health care systems and societies following the COVID-19 pandemic. Representation of patient and health care providers’ views is a novelty, and the study’s large sample size and high consensus rates are strengths. The Delphi consensus method we adopted incorporated data from a diverse sample of patients and clinicians with a wide range of Long COVID and long term condition experiences from all devolved nations of the UK. It combined more than 1400 responses from nearly 500 survey participants and was supported by patients, clinicians, and charitable and professional organisations across the UK. This enabled the integration of views from different stakeholder groups, going beyond similar research where patients’ involvement was not incorporated at all or any stages52. Incorporating views relevant to Long COVID and complex multiple long term conditions and the findings highlighting the similarities in health care priorities is novel and another strength of the study. The 80% level of consensus, which identified the same top 10 statements as priorities for long term condition care as for Long COVID care, is very high when compared to consensus levels in most Delphi studies indicating substantial agreement that the prioritised statements are essential to address during ICP development which is another strength.
Limitations are that despite efforts to recruit a diverse sample, the vast majority of respondents to survey 1 were female and of white ethnicity, similar to other UK health-related research56 and to the demographics of people attending Long COVID clinics. It is thus possible that priorities pertinent to individuals from alternative backgrounds may not have been reflected in the statements presented. For survey 2, we took more measures to guarantee a diverse sample regarding ethnicity and gender by additional purposive sampling57. Nevertheless, our sample was only drawn from the UK and mainly, but not exclusively, recruited the public respondents via online systems, which may introduce bias relating to the digital divide and health pressure groups. In contrast, digital access for health care providers should be less of a distorting factor. Despite these limitations regarding the generalizability of the findings, we believe the findings can be relevant to health care systems internationally.
Given the paucity of integrated care guidelines for complex, multiple long term conditions, this study reinforces the need to continue striving to provide care which is patient-centred, ongoing and supported by evidence. This paper starts to meet this need by offering concrete recommendations to support the implementation of interdisciplinary care for complex long term conditions and Long COVID in routine practice; for example, by the inclusion of multidisciplinary teams to provide interventions, and by coordinated, integrated plans for treatment and long term support.
In the context of integrated care for Long COVID and complex, multiple long term conditions, people need access to care and treatments that work, not just more access. They need diagnostic procedures that support the personalization of treatment in an integrated care environment, avoiding stacking treatment for each condition by making lean, personalized treatment programs supported by a care manager, a virtual multidisciplinary team and specialist consultants as needed. This model for delivering integrated care can be attained by vertical integration between primary and relevant specialist care, delivered by a multidisciplinary team including physical and mental health care, that may convene virtually. Actioning the policy recommendations from this research may help ensure appropriate care provision for the growing number of people with complex, multisystem long term conditions requiring management. With a gap in health care provision for Long COVID in many countries, and the similar problems identified by this study for complex multiple long term conditions, our recommendations offer guidance for international communities to develop similar integrated care approaches appropriate both for Long COVID and for refining health care provision for complex multiple long term conditions.
Methods
Design
Since the invention of the Delphi method in the 1950s58 a commonly used variation of the Delphi method is the estimate-talk-estimate Delphi method that combines assembling of expert opinions on an anonymous basis during surveys with open exchange during workshops by a facilitator or moderator panel59; this approach was adopted for the current project. This Delphi consensus study involved two surveys: an exploratory survey followed by a consensus and ranking survey, alternating with expert panel meetings from February 1 2022 to March 30 2023. It sought to identify integrated care priorities and to inform policy recommendations. We report the findings following the Guidance on Conducting and REporting DElphi Studies (CREDES)34 and a checklist outlining where they can be found (Supplementary Information).
Scope
The plan and scope of the work was discussed and agreed with expert panel members at the first meeting. Adults (aged ≥ 18 years) residing in the UK were eligible to participate. Following input from the STIMULATE-ICP Patient and Public Involvement (PPI) group33, regarding the definition of complex multiple long term conditions for consideration in the IC priorities, input in the survey on fatigue, as a symptom, was in scope. However, given an ongoing discussion between patient groups on whether Long COVID would or would not differ from myalgic encephalomyelitis or chronic fatigue syndrome (ME/CFS), and the wish of the PPI group to focus on Long COVID, ME/CFS was considered out of scope.
Delphi team
This work involved a research team, a moderator panel and an expert panel.
-
The research team (n = 4) consisted of academic researchers (JS, FT, CFC) and a coordinator (NS). This group worked across all aspects of the project.
-
The moderator panel included two General Practitioners and two PPI members (MG, GA, EA, LH) drawn from the STIMULATE-ICP consortium. This group met with the research team on 20 occasions (typically fortnightly) throughout the project to oversee all aspects of the research.
-
Expert panel members were selected by the moderator panel and research team. The aim for this group was to include people with clinical expertise as Health Care Providers (HCP) or lived experience as patients, of Long COVID, other LTCs such as cardiovascular disorders, type 2 diabetes, mental disorders and MNYES, or multi-morbidity; 5 of each group with a minimum of 25.
A snowballing method and a maximum variation approach to selection were followed to recruit expert panel members. Patient expert panel members were recruited from peer support groups, previous research project PPI groups, charities relating to health conditions (including Diabetes UK, Guts UK, British Pain Society, Epilepsy Action, British Thyroid Foundation, Graham Hughes International Charity-antiphospholipid syndrome) and NHS trust patient involvement networks. Based on self-reported diagnosis, fifteen people with lived experience of Long COVID or long term conditions such as cardiovascular disorders, type 2 diabetes, mental disorders and medically not yet explained symptoms (MNYES), or multi-morbidity were included (total n = 15: Long COVID experience = 9, long term condition experience = 10). Six patient expert panel members had only Long COVID experience, 12 had only (diverse) long term condition experiences and 11 had both Long COVID and long term conditions. Patient expert panel members included people who lived with single and multiple long term conditions. Overall, the patient expert panel members had experience of the following long term conditions: fibromyalgia, POTS, diabetes, endometriosis, psoriatic arthritis, cluster headaches, asthma, COPD and mental disorders including anxiety, depression, bipolar disorder, Functional Neurological Disorder and PTSD.
HCP expert panel members were medics recruited from professional clinical networks, medical trusts and the Royal College of General Practitioners, as well as contacts from the STIMULATE-ICP consortium (total n = 14: working with Long COVID = 8, working with long term condition = 14). Specialties included Primary Care (n = 4), Psychiatry (n = 3), Cardiology (n = 2), Diabetes (n = 1), Geriatrics (n = 1), Rehabilitation medicine (n = 1), Stroke (n = 1) and COPD (n = 1).
Data collection and analysis
Round 1: gathering information
Survey 1 collected anonymous electronic data using the Qualtrics survey platform60. Based on input from the expert panel and the moderator panel, the survey included questions about (1) demographic factors (age, gender, ethnicity), (2) relevant disease experience as patient or clinician; (3) experiences of initiating care, referrals, treatment(s) offered and received; (4) challenges and advances for clinical care, (5) knowledge gaps and policies, (6) possible improvements to services, and (7) the transferability of care models to other conditions. These topics were explored for Long COVID and for long term condition integrated care pathways (ICPs). Questions were presented to participants in blocks, depending on their self-reported experience as a person with lived or professional experience of Long COVID or long term conditions. Participants were able to respond to multiple question blocks if they self-reported multiple experiences. Questions were similar in each block but differed slightly between patients and HCPs. They are available via this link: https://www.york.ac.uk/media/healthsciences/documents/research/mentalhealthresearch/STIMULATE-ICP%20Delphi%20Survey%20Questions.pdf.
The research team initially organized responses (n = 283; responses = 1447) into four groups based on who made the statements: patients with experience of Long COVID (19 statements), patients with experience of long term conditions (10 statements), HCP with experience of Long COVID (14 statements) and HCP with experience of long term conditions (12 statements). This was reviewed and revised by small groups of expert panel members to ensure similar responses were grouped together and suggest summary statements which reflected the survey responses. To ensure all perspectives were considered in this process, each group meeting involved patient and clinician expert panel members, was chaired by a moderator panel clinician and observed by a moderator panel PPI representative. Feedback was gathered from the panels during meetings that were audio-recorded, with notes taken by an observer. Consensus discussions took place, the outcomes were recorded, and minutes circulated.
Round 2: establishing consensus and ranking
As the first round aimed at amassing as many relevant statements as possible, consensus was not calculated in round one. We calculated consensus levels on the statements in round 2 and defined consensus as at least 50% agreement in the response category. In case of lack of consensus, further rounds for achieving consensus were planned.
Expert panel members reviewed summary statements developed from Survey 1 responses during the second full expert panel meeting to remove any overlaps. In all rounds, feedback was gathered from the expert panel during expert panel meetings that were audio-recorded, with notes taken by an observer. Consensus discussions took place, the outcomes were recorded, and minutes circulated. The final list of 15 summary statements were presented as statements relevant to ICP for Long COVID and long term conditions in the second anonymous online survey. Survey participants were asked to respond to questions about health care priorities for Long COVID and long term conditions separately in blocks of questions so that all questions about Long COVID were together and all questions about long term conditions were together. To minimise response bias, these question blocks about Long COVID and long term conditions were presented in a random order; the list of statements within questions were also presented in a random order. Survey 2 asked participants to rate their level of agreement with each of the statements about Long COVID and long term condition care using a 5-point Likert scale (1. Strongly Agree, 5. Strongly Disagree). After this, participants were asked to prioritise the statements in order of importance (1 = most important, 15 = least important).
Median values were calculated to aid interpretation of the response category selected by survey participants. Interquartile deviation (IQD) values61 were used to ascertain consensus agreement from Survey 2 data (n = 197). IQD represent the spread of responses, with smaller values indicating greater consensus. Initially IQDs were calculated using a 50% threshold by determining the distance between the 25th and 75th percentiles (> 50% of individuals responded using the same category). IQD ≤ 1 was considered to indicate consensus as this indicates that cases fall within one response category from each other. Following discussion with the moderator panel who considered a Top-10 priority list to be optimal, statements which achieved 80% consensus (> 80% of individuals responded using the same category; n = 10 items) were included in prioritization. All response options were considered relevant for inclusion in this study. This means that items which achieved consensus for negative response options (Strongly disagree/Disagree) would be incorporated into the study results in the same way as positive response options (Strongly agree/Agree) were included; however, in this case consensus for all items were around positive response categories. Respondents were asked to prioritize all 15 summary statements in order of importance, placing the most important statement against the value of 1 and the least important statement against the value of 15. The sum of prioritization responses was used to establish the order of statements; the item with the lowest sum value was considered to have the highest priority.
Round 3: developing policy recommendations
Ten statements achieved 80% consensus after Survey 2; these were the same for both Long COVID and long term conditions. Further surveys to establish consensus were therefore not necessary. Full consensus and prioritization results are shown in Table 3.
The results of Survey 2 were presented in IQD format and discussed with the moderator panel in relation to Long COVID initially, and then in relation to long term conditions. Following this, the team decided to consider the recommendations together due to the similarities in priorities and rank order for both groups. The research team and moderator panel then worked together to develop the key domains relevant to the ten identified priorities and the statements which underpinned them. During these discussions, draft policy recommendations from the ten statements which achieved consensus were developed. The process of understanding the Survey 2 findings were then discussed with the expert panel in a final expert panel meeting. Priorities for Long COVID and their ranking were presented in IQD format, and then for long term conditions before discussion about the similarities and differences between the priorities and rank order. The research team and moderator panel process of developing the key domains and the draft policy recommendations was then also discussed with expert panel members. The scope of recommendations, appropriate stakeholders to share these with and co-signatories who may be interested in supporting the recommendations were also included in this discussion. The final recommendations from this work are organized into the four key domains: Diagnosis, Research, Resources and Training. Dissemination strategies for these recommendations were discussed with expert panel members and moderator panel members. Feedback was gathered from the expert panel during this meeting that was audio-recorded, with notes taken by an observer. Consensus discussions took place, the outcomes were recorded, and minutes circulated. The discussion continued until consensus was reached.
In addition to the expert panel and moderator panel members, representatives of relevant long term condition charities attended the second half of the final expert panel meeting. These representatives contributed to discussions concerning approaches to dissemination.
Priorities for health care of Long COVID and of long term conditions were initially examined independently, and then compared. The research team and moderator panel considered the priorities and underlying statements for these two groups, identifying key themes across all areas in order to develop key domains across all priorities. Draft policy recommendations were developed for the identified key domains using the same approach, prior to consultation with the expert panel members.
Survey participants
Snowball sampling was used to recruit participants for both surveys. Existing clinical, patient support and social media networks shared the information to generate diverse samples with a variety of clinical experiences relevant to ICPs. To ensure diversity of sex and ethnicity, purposive sampling through the research platform PROLIFIC was incorporated into Survey 2 recruitment57.
Survey 1 (n = 283) focused on patient or health care professional experience of Long COVID or long term conditions. Questions for patients and HCPs differed slightly as indicated in the pdf via this link https://www.york.ac.uk/media/healthsciences/documents/research/mentalhealthresearch/STIMULATE-ICP%20Delphi%20Survey%20Questions.pdf.
Initially 328 people consented to complete Survey 1, however 45 were excluded for the following reasons: incomplete responses to eligibility items (n = 11), residing outside of the UK (n = 20), out of scope experiences (n = 14). Data presented for Survey 1 therefore relate to priorities for integrated care for Long COVID and long term conditions from 283 respondents (1447 suggestions). These did not reflect current clinical care provision but what respondents considered to be the most important aspects of care for these patient groups. Responses for Long COVID and long term conditions were organized separately initially, but due to the high level of overlapping themes, a single list of 15 statements was included in Survey 2. Survey 2 participants were asked to prioritize and rank from this list for both Long COVID and long term condition care independently.
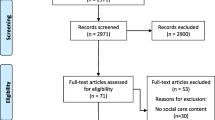
All UK-based adults were eligible to participate in Survey 2 (n = 197). Initially 485 people consented to complete Survey 2, however 288 were excluded for the following reasons: no response at all (n = 173), no demographic data to assess eligibility (n = 76), residing outside of the UK (n = 5), out of scope experiences (n = 34). Despite this, Survey 2 recruited a large sample (n = 197) diverse in terms of gender, age and ethnicity for consensus and prioritization of statements. Table 2 shows demographic characteristics for Surveys 1 and 2. The flow of participants through the study is shown in Fig. 1.
Patient and public involvement (PPI)
Patients were involved in discussions and shaping of this work at all stages. PPI members were included in the expert panel and the moderator panel incorporating the experiences of people with a variety of Long COVID symptoms and long term conditions, and assisted with formulation of policy suggestions and dissemination of the results.
Ethics
This research was conducted in accordance with the Declaration of Helsinki and was reviewed and approved by the University of York Health Sciences Research Governance Committee on 17·12·2021 (HSRGC/2021/478/A: STIMULATE). All survey participants provided informed consent.
Preprint
A previous version of this manuscript was published as a preprint62
Data availability
Responses from Survey 1 data and the way these were organised and translated into Survey 2 statements are publicly available on website https://www.york.ac.uk/healthsciences/research/mental-health/projects/stimicp/. A minimal dataset from Survey 2 can be made available to interested parties upon request to the principal investigator. Researchers can submit a research plan, which describes the background and methods of a proposed research question, and a request for specific data of the database used for this study to answer the research question. Requests to access the datasets should be directed to christina.vanderfeltz-cornelis@york.ac.uk. The study protocol is available online33.
References
Vos, T. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. The Lancet 396, 1204–1222 (2020).
Palmer, K. et al. The potential long-term impact of the COVID-19 outbreak on patients with non-communicable diseases in Europe: Consequences for healthy ageing. Aging Clin. Exp. Res. 32, 1189–1194 (2020).
Goodwin, N. Understanding integrated care. Int. J. Integr. Care 16(4), 6 (2016).
NHS. Guidance to clinical commissioning groups on preparing integrated care board constitution. www.england.nhs.uk/publication/integrated-care-systems-guidance/ (2023).
NHS England. NHS five year forward view. www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf (2014).
Sather, E. W., Iversen, V. C., Svindseth, M. F., Crawford, P. & Vasset, F. Exploring sustainable care pathways-a scoping review. BMC Health Serv. Res. 22(1), 1595 (2022).
Ratti, M. et al. The determinants of expert opinion in the development of care pathways: Insights from an exploratory cluster analysis. BMC Health Serv. Res. 23(1), 211 (2023).
Button, K., Morgan, F., Weightman, A. L. & Jones, S. Musculoskeletal care pathways for adults with hip and knee pain referred for specialist opinion: A systematic review. BMJ Open 9(9), e027874 (2019).
Lip, G. Y. & Ntaios, G. Novel clinical concepts in thrombosis: Integrated care for stroke management—easy as ABC. Thrombos. Haemost. 122(03), 316–319 (2022).
Field, M. et al. Integrated care systems and the aortovascular hub. Thrombos. Haemost. 122(02), 177–180 (2022).
Buckley, B. J. Integrated care for atrial fibrillation: What’s the recipe for success? Eur. J. Cardiovasc. Nurs. 23(4), 36–36 (2024).
J. Flowers Health Staff. What is a complex medical condition? An informative guide. https://jflowershealth.com/what-is-a-complex-medical-condition/ (2024).
Social Care Institute for Excellence. Multidisciplinary teams working for integrated care. https://www.scie.org.uk/integrated-care/research-practice/activities/multidisciplinary-teams/ (2023)
Béland, F. & Hollander, M. J. Integrated models of care delivery for the frail elderly: International perspectives. Gac. Sanit. 25, 138–146 (2011).
Camacho, E. M. et al. Long-term clinical and cost-effectiveness of collaborative care (versus usual care) for people with mental–physical multimorbidity: Cluster-randomised trial. Br. J. Psychiatry 213(2), 456–463 (2018).
Chwastiak, L., Vanderlip, E. & Katon, W. Treating complexity: Collaborative care for multiple chronic conditions. Int. Rev. Psychiatry 26(6), 638–647 (2014).
Ivbijaro, G. O., Enum, Y., Khan, A. A., Lam, S. S. & Gabzdyl, A. Collaborative care: Models for treatment of patients with complex medical-psychiatric conditions. Curr. Psychiatry Rep. 16, 1–2 (2014).
Thornicroft, G. et al. Integrated care for people with long-term mental and physical health conditions in low-income and middle-income countries. The Lancet Psychiatry 6(2), 174–186 (2019).
Doornebosch, A. J., Smaling, H. J. & Achterberg, W. P. Interprofessional collaboration in long-term care and rehabilitation: A systematic review. J. Am. Med. Dir. Assoc. 25(5), 764–777 (2022).
Huffman, J. C., Niazi, S. K., Rundell, J. R., Sharpe, M. & Katon, W. J. Essential articles on collaborative care models for the treatment of psychiatric disorders in medical settings: A publication by the academy of psychosomatic medicine research and evidence-based practice committee. Psychosomatics 55(2), 109–122 (2014).
Coventry, P. et al. Integrated primary care for patients with mental and physical multimorbidity: Cluster randomised controlled trial of collaborative care for patients with depression comorbid with diabetes or cardiovascular disease. BMJ https://doi.org/10.1136/bmj.h638 (2015).
Wallace, E. et al. Managing patients with multimorbidity in primary care. BMJ https://doi.org/10.1136/bmj.h176 (2015).
Rijken, M. et al. Managing multimorbidity: Profiles of integrated care approaches targeting people with multiple chronic conditions in Europe. Health policy 122(1), 44–52 (2018).
van der Feltz-Cornelis, C. M., Van Os, T. W., Van Marwijk, H. W. & Leentjens, A. F. Effect of psychiatric consultation models in primary care. A systematic review and meta-analysis of randomized clinical trials. J. Psychosom. Res. 68(6), 521–33 (2010).
World Health Organization. Post COVID-19 condition (Long COVID). https://www.who.int/europe/news-room/fact-sheets/item/post-covid-19-condition#:~:text=Definition,months%20with%20no%20other%20explanation (2024).
NHS England. Post-COVID syndrome (long COVID). https://www.england.nhs.uk/coronavirus/post-covid-syndrome-long-covid/ (2024).
NHS. Long-term effects of COVID-19 (long COVID). https://www.nhs.uk/conditions/covid-19/long-term-effects-of-covid-19-long-covid/ (2023).
ONS. Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK: 2 February 2023. www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/bulletins/prevalenceofongoingsymptomsfollowingcoronaviruscovid19infectionintheuk/2february2023 (2023).
Davis, H. E., McCorkell, L., Vogel, J. M. & Topol, E. J. Long COVID: Major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 21(3), 133–146 (2023).
Mudgal, S. K. et al. Pooled prevalence of long COVID-19 symptoms at 12 months and above follow-up period: A systematic review and meta-analysis. Cureus 15(3), e36325 (2023).
NHS England. Long COVID patients to get help at more than 60 clinics www.england.nhs.uk/2020/12/long-covid-patients-to-get-help-at-more-than-60-clinics/ (2020).
NHS England. National commissioning guidance for post COVID services 2022 www.england.nhs.uk/publication/national-commissioning-guidance-for-post-covid-services/ (2022).
van der Feltz-Cornelis, C. M. et al. STIMULATE-ICP-Delphi (symptoms, trajectory, inequalities and management: Understanding long-COVID to address and transform existing integrated care pathways delphi): Study protocol. Plos One 17(11), e0277936 (2022).
Jünger, S., Payne, S. A., Brine, J., Radbruch, L. & Brearley, S. G. Guidance on Conducting and REporting DElphi Studies (CREDES) in palliative care: Recommendations based on a methodological systematic review. Palliat. Med. 31(8), 684–706 (2017).
Adler, M. & Ziglio, E. Gazing into the oracle: The Delphi method and its application to social policy and public health (Jessica Kingsley Publishers, 1996).
NHS England. Involving people in their own care. https://www.england.nhs.uk/ourwork/patient-participation/ (2024).
Lewis, R.Q., Rosen, R., Goodwin, N. & Dixon, J. Where next for integrated care organisations in the English NHS. London: The Nuffield Trust. 2017–01 (2010).
House of Commons Health Committee. Managing the care of people with long-term conditions (2014).
Turk, F. et al. Accessing care for Long Covid from the perspective of patients and healthcare practitioners: A qualitative study. Health Expect, 27(2), e14008 (2024).
Ladds, E. et al. Persistent symptoms after Covid-19: Qualitative study of 114 “long Covid” patients and draft quality principles for services. BMC Health Serv. Res. 20(1), 1–3 (2020).
NHS England. COVID-19: Summary of infection prevention and control guidance and information for healthcare settings. https://www.england.nhs.uk/coronavirus/documents/covid-19-summary-of-infection-prevention-and-control-guidance-and-information-for-healthcare-settings/ (2022).
Kaye, A. D. et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems: International perspectives. Best Pract. Res. Clin. Anaesthesiol. 35(3), 293–306 (2021).
Maruthappu, M., Hasan, A. & Zeltner, T. Enablers and barriers in implementing integrated care. Health Syst. Reform 1(4), 250–256 (2015).
van der Feltz-Cornelis, C., Attree, E., Heightman, M., Gabbay, M. & Allsopp, G. Integrated care pathways: A new approach for integrated care systems. Br. J. Gen. Pract. 73(734), 422 (2023).
van der Feltz-Cornelis, C. M., Heightman, M. & Allsopp, G. Learning from long COVID: Integrated care for multiple long-term conditions. Br. J. Gen. Pract. 73(730), 196–197 (2023).
Martínez-González, N. A., Berchtold, P., Ullman, K., Busato, A. & Egger, M. Integrated care programmes for adults with chronic conditions: A meta-review. Int. J. Qual. Health Care 26(5), 561–570 (2014).
Baxter, S. et al. The effects of integrated care: A systematic review of UK and international evidence. BMC Health Serv. Res. 18, 1–3 (2018).
Rajasekaran, R. B., Whitwell, D., Cosker, T. D., Gibbons, C. L. & Carr, A. Will virtual multidisciplinary team meetings become the norm for musculoskeletal oncology care following the COVID-19 pandemic?-experience from a tertiary sarcoma centre. BMC musculoskelet. Disord. 22, 1–7 (2021).
Sidpra, J. et al. Virtual multidisciplinary team meetings in the age of COVID-19: an effective and pragmatic alternative. Quant. Imaging Med. Surg. 10(6), 1204 (2020).
RACGP. More than 8m Australians have a long-term health condition: Census https://www1.racgp.org.au/newsgp/clinical/more-than-8m-australians-have-a-long-term-health-c (2022).
Owen, N., Dew, L., Logan, S., Denegri, S. & Chappell, L. C. Research policy for people with multiple long-term conditions and their carers. J. Multimorb. Comorbidity 12, 26335565221104410 (2022).
Schaefert, R. et al. COVID-19-related consultation-liaison (CL) mental health services in general hospitals: A perspective from Europe and beyond. J. Psychosom. Res. 167, 111183 (2023).
Parker, A. M. et al. Addressing the post-acute sequelae of SARS-CoV-2 infection: A multidisciplinary model of care. The Lancet Respir. Med. 9(11), 1328–1341 (2021).
Nurek, M. et al. Recommendations for the recognition, diagnosis, and management of long COVID: A Delphi study. Br. J. Gen. Pract. 71(712), e815–e825 (2021).
Highton, P. J. et al. Cardiometabolic disease and multiple long-term condition healthcare provision in Sub-Saharan Africa: Opportunities for new models of care in the post-COVID era. Diabetes Metab. Syndr. 17(1), 102681 (2022).
Smart, A. & Harrison, E. The under-representation of minority ethnic groups in UK medical research. Ethnic. Health 22(1), 65–82 (2017).
Prolific. A higher standard of online research. www.prolific.co/ (2023).
Dalkey, N. & Helmer, O. An experimental application of the Delphi method to the use of experts. Manag. Sci. 9(3), 458–467 (1963).
Rowe, G. & Wright, G. Expert opinions in forecasting: The role of the Delphi technique. In Principles of forecasting: A handbook for researchers and practitioners 125–44 (Springer, 2001).
Qualtrics. Qualtrics. Provo, Utah, USA (2020).
Rayens, M. K. & Hahn, E. J. Building consensus using the policy Delphi method. Policy, Politics Nurs. Pract. 1(4), 308–315 (2000).
Sweetman, J. et al. Integrated care priorities for complex, multi-system, long-term conditions and for long COVID: Results of the STIMULATE-ICP-Delphi study among UK patients and healthcare providers. Preprint at https://doi.org/10.2139/ssrn.4498395 (2023).
Acknowledgements
This research has been conducted as part of the STIMULATE-ICP consortium, with valuable contributions being made by academic and PPI group members. An up-to-date list of Consortium members can be found: https://www.stimulate-icp.org/team. STIMULATE-ICP can be contacted at: info@stimulate-icp.org. MG is part-funded by National Institute for Health Research (NIHR) Applied Research Collaboration North West Coast (NIHR ARC NWC). KK is supported by the National Institute for Health Research (NIHR) Applied Research Collaboration East Midlands (NIHR ARC EM) and the NIHR Leicester Biomedical Research Centre (BRC). Our Moderator Panel members made significant contributions to the methods and focus for this work, including Dr Gail Allsopp, Dr Emily Attree, Professor Mark Gabbay (MG) and Lyth Hishmeh. We would also like to thank the Expert Panel members who contributed to this work, including Dr Robert Bell, Dr Philippa Bolton, Dr Anna Bristow, Dr Abigail Carey, Sakina Chandoo, Andrew Clark, Harriet Collett, Dr Michael Crooks, Katherine Francis, Jackie Harrison, Lisa Holden, Nicky Hughes-Evans, Danielle Knott, Helen Marshall, Dr David Mummery, Ritesh Patel, Dr Mark Rickenbach, Dr Abayomi Salawu, Dr Thozhukat Sathyapalan, Annie Shaw, Dr Gemma Smith, Dr Katherine Wildon. We thank the PPI group of STIMULATE-ICP, especially Dr Emily Attree, Lyth Hishmeh and Antony Loveless for their contribution to the research. In addition, the following charities and other organizations have supported the recruitment of expert panel members and/or survey participants: British Thyroid Foundation, Diabetes UK, Epilepsy Action, Graham Hughes International Charity, Guts UK, LYPFT, TEWV, The British Pain Society.
Funding
National Institute of Health Research grant (COV-LT2-0043) as part of the STIMULATE-ICP study (AB). This study was funded by the NIHR (COV-LT2-0043) as part of the STIMULATE-ICP study. The views expressed in this publication are those of the author(s) and not necessarily those of the National Institute for Health Research or the Department of Health and Social Care.
Author information
Authors and Affiliations
Contributions
Conceptualization: C.F.C., J.S., G.A., M.G., A.B.; methodology: C.F.C., J.S., G.A., M.G., A.B.; funding acquisition: A.B., C.F.C., G.A., M.G., K.K., N.W., H.M., M.H., G.Y.H.L., M.G.C., W.D.S., A.L., L.H.; ethics: C.F.C., A.B.; project administration: C.F.C.; data curation and analysis: J.S., F.T., G.A., M.G., L.H., N.S., C.F.C.; writing—original draft: J.S., C.F.C.; writing—review & editing: C.F.C., J.S., F.T., G.A., M.G., K.K., N.W., H.M., M.H., G.Y.H.L., M.G.C., W.D.S., A.L., L.H., N.S., A.B.; patient and public involvement: A.L., L.H.
Corresponding author
Ethics declarations
Competing interests
This research was funded by the National Institute for Health and Care Research (NIHR) (COV-LT2-0043). This work is independent research funded as part of the STIMULATE-ICP study. The views expressed in this publication are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. Unless otherwise stated, funding for this project was paid to author institutions. In addition, GA has held leadership roles with the Royal College of General Practitioners and National Institute for Health and Care Excellence during the timeframe of the STIMULATE-ICP Delphi project. MG has had recent or current involvement with NIHR and UKRI research grants. MG has been involved in SDL learning as academic director (payment to institution) and as a tutor (payment to MG). He has been appointed as faculty provost for the Royal College of General Practitioners and has small holdings from demutualization with Lloyds bank, ABRDN and Aviva. MG is part-funded by NIHR applied Research Collaboration North West Coast. KK is supported by the National Institute for Health Research (NIHR) Applied Research Collaboration East Midlands (ARC EM) and the NIHR Leicester Biomedical Research Centre (BRC). KK is Chair of UKRI/NIHR Long-Covid studies and reports to the Chief Medical Officer. NW is Deputy chair of NIHR HTA Programme Funding Committee for commissioned research and is a GP partner in Plas Menai Health Centre, Llanfairfechan. HM has received consultation fees from Astra Zeneca and has participated on a Data Safety Monitoring Board or Advisory Board relating to prevention and treatment of COVID-19 (not Long COVID issues specifically), and has received consultation fees from Axcella Therapeutics relating to a possible new Long COVID therapeutic. HM has also received payment from the Law Society for Education on Long COVID. MH is National Specialty Advisor for Long Covid, NHS England. As PPI members of STIMULATE-ICP, AL and LH have received funding from NIHR (COV-LT2-0043) for reimbursement for attendance and travel for research meetings. AB is the Chief Investigator of the STIMULATE-ICP (COV-LT2-0043) and is part of the BigData@Heart Consortium, funded by the Innovative Medicines Initiative-2 Joint Undertaking under grant agreement No. 116074. This Joint Undertaking receives support from the European Union’s Horizon 2020 research and innovation programme and EFPIA; it is chaired, by DE Grobbee and SD Anker, partnering with 20 academic and industry partners and ESC. In addition, AB has had recent or current involvement with NIHR, BMA, Astra Zeneca and UKRI research grants. AB is an unpaid Trustee for the South Asian Health Foundation. CFC has had recent or current involvement with grants from the BMA (CANDO Study), EU Horizon (EMPOWER Study), the Netherlands Organisation for Health Research and Development (Regional systems intervention for suicide prevention (SUPREMOCOL) in Noord -Brabant, the Netherlands), and NIHR HS&DR (Frequent Users of the Emergency Department: Improving and Standardising Services-a mixed methods study). CFC has received royalties for books on Psychiatry, an honorarium payment related to a lecture at the Big Questions in Neuroscience Annual meeting from Janssen UK, and has received travel and accommodation in the UK for a lecture from The Lloyd Register Foundation. All other authors have no conflicts of interest to report.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
van der Feltz-Cornelis, C.M., Sweetman, J., Turk, F. et al. Integrated care policy recommendations for complex multisystem long term conditions and long COVID. Sci Rep 14, 13634 (2024). https://doi.org/10.1038/s41598-024-64060-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-64060-1
- Springer Nature Limited