Abstract
In the United States (US), chlamydia is the most frequently reported sexually transmitted infection that is nationally notifiable. We examined trends in chlamydia prevalence in the US in 2011–2016 compared with 2005–2010. Cross-sectional, nationally representative surveys, National Health and Nutrition Examination Surveys (NHANES), were used to compare national chlamydia prevalence estimates from 2011 to 2016 with those from 2005 to 2010, and changes in prevalence since 1999–2004 were also reviewed. Persons aged 18–39 years were included in these analyses. Prevalence of chlamydia was based on results from urine specimens. Results were weighted to represent the U.S. civilian, noninstitutionalized population. The baseline characteristics of the study population were similar in gender, age and race/ethnicity between the two groups (P > 0.05). The overall chlamydia prevalence was 1.88% (95% confidence interval [CI] 1.55–2.22%) in 2011–2016 and 1.57% (95% CI 1.27–1.87%) in 2005–2010, a relative increase of 19.7% (95% CI 0.2–39.2%; P < 0.05) between the two surveys. Increases in chlamydia prevalence was especially concentrated in persons who were male, aged 18 to 29 years, had > high school educational level, never married, age at first sex < 18 years, had 2–5 sexual partners in lifetime and had no past sexually transmitted diagnosis between 2005 and 2016 (P < 0.05). Multivariable logistic regression analysis demonstrated that chlamydia was more prevalent in those aged 18–29 years, being non-Hispanic Blacks, had high school educational level, being widowed/divorced/separated and had > 5 sexual partners. The chlamydia prevalence had an increasing trend from 2005–2010 to 2011–2016. Those with high chlamydia prevalence such as sexually active young adults and Non-Hispanic Black should be screened annually so that infected persons can be diagnosed and they and their sex partners can be treated promptly.
Similar content being viewed by others
Introduction
Caused by the infection with Chlamydia trachomatis, chlamydia is the leading notifiable disease in the United States (US). It ranks among the most widespread sexually transmitted infection (STI), with the highest proportion of reported STI cases to CDC since 19941. Chlamydial infections commonly show no symptoms in men and women2. However, if left untreated, these infections can lead to acute urogenital diseases like urethritis, vaginitis, cervicitis, and genital ulceration in men or women3,4. Similar to other inflammatory STI, chlamydial infection can increase the risk of HIV transmission5. Moreover, newborns with congenital chlamydial infection via in utero transmission had increased risk of ophthalmia neonatorum, a condition that can result in blindness, as well as pneumonia6.
Chlamydia infection imposes a substantial cost burden on medical care in the United States. In the study conducted by Owusu-Edusei Jr. and colleagues, the total direct medical costs for chlamydia in 2008 were estimated to be $516.7 million for individuals aged 15–39 years7. The study further revealed that among nonviral STI, chlamydia was the most expensive infection. It emphasized that the burden would be even higher in the absence of efforts for STI prevention and control.
There have been two studies that showed the high prevalence of chlamydial infections in the general, non-institutionalized population of the United States, with a particular emphasis on young women8,9. Datta et al. reported that the prevalence of Chlamydia infection was 2.2% in 1999–2002 among persons aged 14–39 years about two decades ago and Torrone et al. reported a relative decreased prevalence of Chlamydia infection in 2007–2012, with an estimate of 1.7% about a decade ago. However, the recent prevalence and trends of chlamydia infection in US remain unclear. We used nationally representative data from the National Health and Nutrition Examination Survey (NHANES) to evaluate the prevalence and trends of chlamydia infection in 2005–2010 and 2011–2016 among US adults and to further determine the correlates of chlamydia infection.
Methods
Study population and survey design
The NHANES is a program of surveys conducted by the National Center for Health Statistics (NCHS) to collect health-related data from the civilian noninstitutionalized population in the US. These surveys use a complex and multistage probability sample design to establish a representative sample of the population. The aim is to obtain comprehensive information on health and nutrition status through interviews and examinations. The detailed information of study design, protocol, and data collection for NHANES are described in existing publications10. From 1999 to March 2020, there were a total of ten cycles for NHANES surveys, consisting of nine 2-year cycles spanning from 1999 to 2016 and one combined cycle from 2017 to March 2020, which was impacted by the COVID-2019 pandemic11. Chlamydia prevalence was surveyed from 1999 to 2016 including nine cycles. The present study included adult population aged ≥ 18 years and who had complete data for chlamydia laboratory test and focused on the chlamydia prevalence of last three cycles 2011–2016 and previous three cycles 2005–2010. The unweighted total response rates ranged from 61.3 to 80.5% for the interviewed samples and from 58.7 to 77.4% for the examined samples12. All participants included in this study were interviewed and medically examined with CT lab results. For this study, the NHANES protocol obtained approval from the National Center for Health Statistics Ethics Review Board, and all participants provided informed consent.
Covariates of chlamydia infection
To examine covariates possibly associated with chlamydia infection, we extracted data on gender (male and female), age (18–29 years and 30–39 years), race/ethnicity (Mexican American, other Hispanic, non-Hispanic White, non-Hispanic Black and other), education (< high school, high school and > high school), marital status (never married, widowed/divorced/separated and married/living with partner), family poverty ratio (<100% and ≥ 100%), age at first sex (< 18 years and ≥ 18 years, sex was defined as vaginal, oral, or anal), number of sexual partners in lifetime (0, 1, 2–5, > 5) and past STI diagnosis (participants who have been told by a doctor or other health care professional in the last 12 months that they had chlamydia or gonorrhea or genital herpes or genital warts).
Statistical analysis
Statistical analysis was performed with R version 4.3.1. Descriptive statistics were generated to show the demographic characteristics and other participants’ features, and the difference of NHANES 2005–2010 and 2011–2016 was compared using Wilcoxon rank-sum test. Estimates on weighted prevalence (95% confidence interval (CI)) of chlamydia were calculated in the two surveys. The percent change (95% CI) was calculated and the differences in prevalence between the surveys were considered to be statistically significant if χ2 test had a P value of less than 0.05. Additionally, estimates on weighted prevalence (95% CI) of chlamydia were further calculated by gender, age, race/ethnicity, education, marital status, family poverty ratio, age at first sex, lifetime no. sexual partners and past STI diagnosis group, the percent change (95% CI) was also calculated and the difference was also compared between the two surveys in each subgroup. Furthermore, we estimated and compared overall, gender-specific, age-specific and race/ethnicity-specific prevalence of chlamydia in 1999–2004, 2005–2010 and 2011–2016. Last, weighted logistic regressions were used to explore the risk factors of chlamydia infection by incorporating gender, age, race/ethnicity, education, marital status, family poverty ratio, age at first sex, lifetime no. sexual partners and past STI diagnosis by combining NHANES 2005–2010 and 2011–2016. All statistical tests were 2 sided, with P < 0.05 considered statistically significant.
Ethic statement
For this study, the NHANES protocol obtained approval from the National Center for Health Statistics Ethics Review Board, and all participants provided informed consent. All methods were carried out in accordance with relevant guidelines and regulations.
Results
Participant characteristics
Of the 60,936 individuals who participated in NHANES from 2005 to 2016, we excluded 24,649 participants who were younger than 18 years and 23,258 who had no chlamydia screening information. The final study population included 13,029 adults with complete data, 6651 in 2005–2010 and 6378 in 2011–2016. There was no significant difference of gender, age and race/ethnicity composition between the two surveys (P > 0.05). Detailed data on demographic characteristics and other participants’ features were shown in Table 1.
Prevalence and trends of chlamydia in 2005–2010 and 2011–2016
The overall chlamydia prevalence was 1.88% (95% CI 1.55%–2.22%) in 2011–2016 and 1.57% (95% CI 1.27%–1.87%) in 2005–2010, a relative increase of 19.7% (95% CI 0.2%–39.2%; P < 0.05) between the two surveys (Table 2). Additionally, an increasing trend was observed for male from 1.45% to 1.94% (percent change, 33.8% [95% CI (2.1%–65.4%)]; P < 0.05), for younger adults aged 18–29 years from 2.18% to 2.81% (percent change, 28.4% [95% CI (4.5%–52.2%)]; P < 0.05), for those who had > high school educational level from 0.94 to 1.34% (percent change, 42.2% [95% CI (2.9%–81.5%)]; P < 0.05), for those who were never married from 1.93% to 2.76% (percent change, 43.5% [95% CI (11.2%–75.7%)]; P < 0.05), for those aged < 18 years when had the first sex from 1.77% to 2.48% (percent change, 39.6% [95% CI (10.5%–68.7%)]; P < 0.05), for those who had 2–5 sexual partners in lifetime from 1.43% to 2.29% (percent change, 60.6% [95% CI (17.1%–104.0%)]; P < 0.05) and for those who had no past STI diagnosis from 1.40% to 2.07% (percent change, 47.9% [95% CI (20.6%–75.1%)]; P < 0.05).
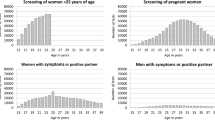
Chlamydia prevalence during 1999–2016
Overall, chlamydia prevalence decreased from 2.10% in 1999–2004 to 1.57% in 2005–2010 (P < 0.05) but re-increased to 1.88% in 2011–2016 (P < 0.05, Fig. 1A). A similar pattern was observed in younger adults, decreased from 2.87% in 1999–2004 to 2.18% in 2005–2010 (P < 0.05) but increased to 2.81% in 2011–2016 (P < 0.05). Although chlamydia prevalence had a continuous decrease from 1994–2004 to 2011–2016 in persons aged 30–39 years, the differences were not statistically significant. Additionally, chlamydia prevalence had a significant decrease from 2.32% in 1999–2004 to 1.70% (P < 0.05) in 2005–2010 and remained stable in 2011–2016 for female adults (Fig. 1B) and decreased from 1.44% in 1999–2004 to 0.75% (P < 0.05) in 2005–2010 and remained stable in 2011–2016 for non-Hispanic White (Fig. 1C). Chlamydia prevalence was stable for male, Mexican American and non-Hispanic Black across the three surveys.
Risk factors of chlamydia infection
In weighted multivariate logistic regression analysis, when compared to the counterparts in each of subgroup, the prevalence of chlamydia was significantly higher for younger adults (OR 3.28; 95% CI 2.01–5.35) and those who were Mexican American (OR, 2.85; 95% CI 1.72–4.72) or non-Hispanic Black (OR 5.01; 95% CI 3.14–8.01), had an educational level of high school (OR 1.90; 95% CI 1.31–2.77)) or < high school (OR 1.51;95% CI 0.92–2.48), were never married (OR 1.83; 95% CI, 1.17–2.86) or widowed/divorced/separated (OR 4.64; 95% CI 2.61–8.26), had one sexual partner (OR 1.16; 95% CI 0.14–9.46) or 2–5 sexual partners (OR 3.73; 95% CI 0.48–29.0) or > 5 sexual partners (OR 3.97; 95% CI 0.55–28.8) in lifetime (Table 3).
Discussion
A nationally representative population of US were included in the present study. Our data showed that the overall prevalence of chlamydia in 2011–2016 was 1.88% among adults aged 18–39 years, which was similar to previous studies that reported a high prevalence of chlamydia8,9. It had a significant relative increase of 19.7% from 2005 to 2010 in which chlamydia prevalence was 1.57%. However, a previous study indicated that there was an estimated 40% reduction from 1999 to 200813, our results suggested that chlamydia prevalence was 2.10% in 1999–2004, the highest among the three surveys, significantly decreased in 2005–2010, but had a re-increasing trend in recent years. Additionally, significant increases of chlamydia prevalence were observed in male and those aged 18–29 years, had > high school educational level, never married, age at first sex < 18 years, had 2–5 sexual partners in lifetime and had no past sexually transmitted diagnosis between 2005 and 2016. Multivariable logistic regression analysis demonstrated that chlamydia was more prevalent in those aged 18–29 years, being non-Hispanic Black, had high school educational level, being widowed/divorced/separated and had > 5 sexual partners.
Considerable prevalences of chlamydia infection have also been observed in other countries in recent years. Li et al. showed that chlamydia prevalence was 6.33% in female outpatients with genital tract infections based on a nationwide, multi-center and cross-sectional study between 2017 and 2018 in China14, and concluded chlamydia prevention strategies should incorporate both behavioral interventions and early screening programs to identify and treat individuals with genital tract infections, particularly those with risk factors. In addition, Campaner et al. performed a study of 11 years’ surveillance of chlamydia infection in Brazil and reported the overall prevalence was 2.2% in the study population15. Klavs et al. reported that the age-specific prevalence was the highest among individuals aged 18–24 years, 2.8% in men and 4.7% in women from a national survey in Slovenia between 2016 and 201716. Therefore, chlamydia infection with high prevalence was a globally noticeable sexually transmitted disease that required primary prevention, targeted testing and effective management.
The surveillance data of CDC in the US finds higher rates of reported chlamydia among women from 2000 to 20181. However, our findings contrast this in the 2011–2016 with males having a higher prevalence than females. This pronounced increase among males could be attributed to either increased transmission or improved case identification (e.g., through intensified extra-genital screening efforts) among gay, bisexual, and other men who have sex with men (MSM)1. Additionally, a significant advantage of population-based prevalence studies of chlamydia, such as NHANES, is the ability to accurately assess the true burden of the disease by detecting infections, whether they present with symptoms or not. Limited research has been conducted to determine the proportion of asymptomatic chlamydial infections. However, data from community screening sites in New Orleans, Louisiana, revealed that up to 77% of chlamydial infections were asymptomatic17. Therefore, we can monitor the chlamydia prevalence fully and accurately by combining reportable surveillance and detecting disease. Although symptoms were not specifically inquired about, making it impossible to differentiate between symptomatic and asymptomatic infections, it is crucial to measure the burden of asymptomatic infections because they are less likely to receive treatment. Untreated chlamydial infections can persist for up to one to two years, and they can be transmitted to sexual partners, increasing the risk of long-term complications in women18.
The NHANES results demonstrated that chlamydial infections disproportionately affect young people and non-Hispanic Black individuals. These findings were consistent with previous surveillance data and results among subgroups of the U.S. population1,8,9. Young individuals may have an increased risk of infection due to biological, contextual, and behavioral factors. Racial and ethnic disparities in chlamydia prevalence may be attributed to differential exposure to the disease within sexual networks, as well as limited access to routine preventative care that includes chlamydia screening and effective partner treatment. Addressing these disparities will require targeted interventions, including federally-funded programs and initiatives such as the CDC’s Community Based Approaches to Reducing Sexually Transmitted Diseases (CARS) initiative, which seeks to promote prevention and control of sexually transmitted infections through interdisciplinary interventions and enhanced community-clinical linkages.
Consistent with other studies19,20, we found that participants with lower educational levels were at higher risk of incident chlamydia infection. This finding may be due to that those with a higher educational level had a better sexual education and tended to avoid high-risk sexual behaviors19,20. Additionally, our results showed that participants who were never married or widowed/divorced/separated had a higher prevalence of chlamydia19. This finding may be due to that unmarried individuals are more likely to have multiple partners21.
The analysis presented in this report have several limitations. Firstly, the data utilized are cross-sectional, it is not possible to capture newly developed cases of chlamydia or assess the duration of chlamydia. Second, it is important to note that the prevalence estimates provided in this report may not account for chlamydial infections occurring at non-genital sites, which can also be contracted through sexual contact, such as the rectum and oropharynx. Therefore, these estimates are likely to underestimate the true burden of sexually transmitted infections. Third, it is possible that some participants may have inaccurately reported their sexual activity status, either by falsely claiming to be sexually active or by denying their sexual activity. However, the present study provided crucial observations of current epidemiology of chlamydia infection, and disparities of chlamydia in sociodemographic and lifestyle factors, which may promote future studies and public health planning.
Conclusions
The overall chlamydia prevalence was 1.88% in 2011–2016 and 1.57% in 2005–2010, having a relative increase of 19.7% between the two surveys. Increases was especially concentrated in persons who were male, aged 18–29 years, had > high school educational level, never married, age at first sex < 18 years, had 2–5 sexual partners in lifetime and had no past sexually transmitted diagnosis. Those with high chlamydia prevalence such as sexually active young adults and Non-Hispanic Black should be screened annually so that infected persons can be diagnosed and they and their sex partners can be treated promptly.
Data availability
The datasets generated and/or analyzed during the current study are available in the open database NHANES website: https://wwwn.cdc.gov/nchs/nhanes/Default.aspx.
References
CDC. Sexually transmitted disease surveillance 2018. Atlanta, GA: US Department of Health and Human Services, CDC. 2019, accessed 1 August 2020); https://www.cdc.gov/std/stats18/STDSurveillance2018-full-report.pdf.
Stamm, W. E. Chlamydia trachomatis infections in the adult. In Sexually Transmitted Diseases 4th edn (eds Holmes, K. K., Sparling, P. F., Stamm, W. E. et al.) 575–606 (McGraw-Hill, 2008).
Hu, H. et al. Prevalence of syphilis and chlamydia trachomatis infection among men who have sex with men in Jiangsu province, China: A cross-sectional survey. Front Public Health. 11(10), 1006254 (2022).
Oakeschott, P. et al. Randomised controlled trial of screening for Chlamydia trachomatis to prevent pelvic inflammatory disease: The POPI (prevention of pelvic infection) trial. BMJ 340, c1642 (2010).
Fleming, D. T. & Wasserheit, J. N. From epidemiological synergy to public health policy and practice: The contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sex Transm. Infect. 75(1), 3–17 (1999).
Hammerschlag, M. R. et al. Longitudinal studies of chlamydial infection in the first year of life. Pediatr. Infect. Dis. 1(6), 395–401 (1982).
Owusu-Edusei, K. Jr. et al. The estimated direct medical cost of selected sexually transmitted infections in the United States, 2008. Sex. Transm. Dis. 40(3), 197–201 (2013).
Datta, S. D. et al. Gonorrhea and chlamydia in the United States among persons 14 to 39 years of age, 1999 to 2002. Ann. Intern. Med. 147(2), 89–96 (2007).
Torrone, E., Papp, J., Weinstock, H., Centers for Disease Control and Prevention (CDC). Prevalence of Chlamydia trachomatis genital infection among persons aged 14–39 years--United States, 2007–2012. MMWR Morb Mortal Wkly Rep. 2014 63(38):834–838.
National Center for Health Statistics. NHANES survey methods and analytic guidelines. 2022, (accessed February 27, 2023); https://wwwn.cdc.gov/nchs/nhanes/analyticguidelines.aspx#sample-design.
National Center for Health Statistics. NHANES 2017-March 2020 pre-pandemic. 2022, (accessed May 23, 2023); https://wwwn.cdc.gov/nchs/nhanes/continuousnhanes/default.aspx?Cycle=2017-2020.
National Center for Health Statistics. NHANES response rates and population totals. 2022, (accessed February 27, 2023); https://wwwn.cdc.gov/nchs/nhanes/ResponseRates.aspx.
Datta, S. D. et al. Chlamydia trachomatis trends in the United States among persons 14 to 39 years of age, 1999–2008. Sex. Transm. Dis. 39(2), 92–96 (2012).
Li, T. et al. Prevalence of and risk factors for chlamydia in female outpatients with genital tract infections: a nationwide multi-center, cross-sectional study in China. Front. Public Health. 11, 1182108 (2023).
Campaner, A. B., de Castro, M. A. & Lucarelli, A. P. Chlamydia trachomatis prevalence in females in São Paulo, Brazil: 11 years’ surveillance of the infection. Braz. J. Microbiol. 54(1), 151–158 (2023).
Klavs, I. et al. Prevalence of sexually transmitted infections with Chlamydia trachomatis, Neisseria gonorrhoeae, Mycoplasma genitalium and Trichomonas vaginalis: findings from the National survey of sexual lifestyles, attitudes and health, Slovenia, 2016 to 2017. Euro. Surveill. 27(14), 2100284 (2022).
Farley, T. A., Cohen, D. A. & Elkins, W. Asymptomatic sexually transmitted diseases: The case for screening. Prev. Med. 36(4), 502–509 (2003).
Golden, M. R., Schillinger, J. A., Markowitz, L. & St Louis, M. E. Duration of untreated genital infections with chlamydia trachomatis: A review of the literature. Sex. Transm. Dis. 27(6), 329–337 (2000).
Wang, H. et al. High chlamydia infection and its associated factors among patients seeking clinic-based STI services in Southern China: A preliminary cross-sectional study. Front. Public Health. 10, 1005334 (2022).
Skjeldestad, F. E., Marsico, M. A., Sings, H. L., Nordbø, S. A. & Størvold, G. Incidence and risk factors for genital Chlamydia trachomatis infection: A 4-year prospective cohort study. Sex. Transm. Dis. 36(5), 273–279 (2009).
Maurya, C., Muhammad, T. & Thakkar, S. Examining the relationship between risky sexual behavior and suicidal thoughts among unmarried adolescents in India. Sci. Rep. 13(1), 7733 (2023).
Funding
National Nature Science Foundation of China (82260598), Jiangxi Provincial academic and technical leaders training program (20225BCJ22009), Educational Commission of Jiangxi Province (gjj210169) and Health Commission of Jiangxi Province (202310034).
Author information
Authors and Affiliations
Contributions
Study concept and design: Y.C., T.Z.. Acquisition of data: Y.C., G.Z., T.Z. Analysis and interpretation of data: Y.C., Z.S., T.Z. Drafting of the manuscript: Y.C., G.Z., T.Z. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: Y.C., X.R., T.Z. Administrative, technical, or material support: T.Z. Supervision: Z.S., T.Z.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cheng, Y., Zheng, G., Song, Z. et al. Trends in chlamydia prevalence in the United States, 2005–2016. Sci Rep 14, 11825 (2024). https://doi.org/10.1038/s41598-024-61818-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-61818-5
- Springer Nature Limited