Abstract
There are inconclusive results available on the association between dietary fatty acid intake and the risk of hypertension (HTN) incident. In this study, we investigate the relationship between baseline dietary fatty acids intake including polyunsaturated fatty acid (PUFA), trans fatty acids (TFA), monounsaturated fatty acid (MUFA), and saturated fatty acid (SFA), and the risk of first incidence hypertension. The current prospective cohort study was carried out from the Ravansar Non-Communicable Diseases (RaNCD) cohort. A food frequency questionnaire (FFQ) with 118 items was used for the assessment of dietary data. Cox proportional hazards analyses were done to estimate hazard ratios (HR) and 95% confidence intervals (CIs) of the highest versus lowest quartile intake of SFA, PUFA, MUFA, and SFA and risk of HTN. Out of 7359 eligible participants, 597 new cases of HTN were identified over an average of 6.4 ± 1.33 years of follow-up. No significant relationship was observed between the fourth compared to the first categories of dietary SFA (HR: 0.82, 95% CI 0.55, 1.21; P trend: 0.476), MUFA (HR: 0.71, 95% CI 0.48, 1.06; P trend: 0.252), PUFA (HR: 0.86, 95% CI 0.62, 1.19; P trend: 0.315) and TFA (HR: 0.99, 95% CI 0.76, 1.27; P trend: 0.675), and risk of HTN. However, a significant inverse association between each 1 g per day increase in dietary MUFA intake during 6.4 years of follow up and HTN incident (HR: 0.97; 95% CI 0.94, 0.99; P 0.044) was observed. In brief, our study revealed that higher dietary MUFA intake was protectively associated with HTN incident. Dietary MUFA-rich foods should be encouraged to improve blood pressure.
Similar content being viewed by others
Introduction
Hypertension (HTN) is extensively associated with most of chronic disease such as cardiovascular disease (CVD), chronic kidney disease (CKD), end-stage renal disease (ESRD) and mortality1. The American Heart Association expected that the direct and indirect costs of HTN in the US population would rise to 240 billion USD by 20302. The prevalence of HTN is lower in high-income countries than in low and middle-income countries1. A meta-analysis conducted on Iranian population in 2019, reported that the prevalence of HTN is 22% among adults3.
Based on evidence, lifestyle factors like dietary habits, alcohol consumption, and physical inactivity are a main contributor to the high prevalence of this disease3. Preventing hypertension through dietary modification is a best solution for public health to promote the population`s well-being4. Although the effects of dietary sodium, potassium, fruit, vegetable and obesity on controlling blood pressure are well-established, the roles of dietary fatty acids are ambiguous5,6.
The macronutrient known as dietary fat plays a crucial role in providing energy for physical activities, as well as aiding in the transportation of fat-soluble vitamins and the construction of cell membranes4. However, overconsumption of dietary fat can lead to weight gain and an increased risk of developing various diseases4. Examples of dietary fats include saturated fatty acid (SFA), trans fatty acid (TFA), monounsaturated fatty acid (MUFA), and polyunsaturated fatty acid (PUFA)4. A cross-sectional analysis from 18 countries7 have revealed that dietary monounsaturated fatty acids (MUFA) intake was inversely related to HTN. Prospective cohort studies have reported mixed results8,9,10. A cohort study on US adults after four years of follow-up did not find any significant associations between dietary SFA or PUFA intake and risk HTN9. However, a trial study in the United State during six years of follow up reported that higher dietary intake of PUFA was related to lower blood pressure, while higher dietary SFA intake was associated with higher blood pressure8. Another prospective cohort study on 28,100 US women indicated that after considering all potential confounders monounsaturated fatty acids (MUFA), SFA, and PUFA were not associated with risk of HTN, whereas the highest versus lowest quintile of trans fatty acids (TFA) intake was significantly related to developing risk of HTN10.
Due to inconclusive results on the association of dietary fatty acids intake and risk of HTN, and also limited study on this relationship specially in developing countries, conducting a cohort study in this regard seems to be necessary. Therefore, we performed a prospective cohort study in the Kurdish adult population of Ravansar Non-Communicable Disease (RaNCD) cohort to determine the link between dietary intake of fatty acids including PUFA, SFA, MUFA, and TFA and the risk of first incidence hypertension.
Materials and methods
Study population
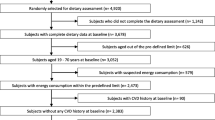
This population-based prospective cohort study was carried out from the Ravansar Non-Communicable Diseases (RaNCD) cohort. The inclusive details on the study have been published11,12. Overall, RaNCD cohort aims to examine the non-communicable diseases in Iranian Kurdish ethnicity in Ravansar city, Kermanshah Province, west of Iran. Ravansar city with a population of around 50,000 people located in the western part of Iran. The RaNCD cohort was one of 20 cores of the Prospective Epidemiological Research Studies in Iran (PERSIAN) cohort study which is approved by the ethics committees at the Ministry of Health and Medical Education of Iran. Baseline information of 10,025 adults ages of 35 and 65 was collected from October 2014 up to August 202211. Out of 10,025 participants at baseline, 2,666 participants were excluded according to the following reasons: 78 with cancer, 109 pregnant women, 1564 who had hypertension at baseline (prevalence case), 64 patients with known renal failure at baseline, 165 subjects with missing data, and 686 participants with calorie intake higher than 4200 kcal or lower than 800 kcal. Finally, 7359 were eligible for analysis and were included in the study (Fig. 1).
Assessment of dietary intake
Baseline dietary data of the study participants were collected by 118 items food frequency questioners (FFQ)11. This valid and reliable FFQ contains a list of usual and local food with normal service sizes that consumed by Iranian Kurdish population11. After fulfilling the FFQ by trained researchers, the reported food item frequency was converted to gram per day by considering the portion sizes of consumed foods13. Daily energy, nutrients, MUFA, PUFA, SFA and TFA intakes of each participant was calculated via Nutritionist IV software with a revised food composition dataset for Iranian foods according to the US Department of Agriculture14.
Assessment and definition of blood pressure
Blood pressure of participants was measured by a manometer (Reister) cuff and stethoscope (Reister) while people sit on a chair in relaxed position. The measurement was done from both right and left arm, then it was repeated 10 min later. To reduce the effects of diurnal variation, the blood pressure was measured in the morning. The average of all measurement was considered as the final blood pressure. Finally, based on the codes I10 of the International classification of diseases Tenth Edition (ICD-10), HTN incident was determined. Accordingly, HTN incident was diagnosis as either SBP/DBP ≥ 140/90 mmHg or taking anti-hypertensive medications in the during between baseline of cohort recrutment (2014) and follow up sessions (from 2015 to 2022)11.
Assessment of other factors
Face-to-face interviews and clinical examinations were conducted to examine all participants. Database applications were used to manage data and collect it. For instance, all questionnaires are fulfilled by the online application and controlled by evaluation teams. The Online electronic questionnaire system was used to register the information about living area (urban, rural), marital status, physical activity, age, education, sex, socioeconomic status (SES), smoking history, and history of chronic diseases. All contributors were requested to take off their shoes, heavy dresses, and accessories. Then, hip circumference, waist circumference (WC), and height were measured by skilled investigators. After that, body mass index (BMI) and body weight was calculated by an automated Bio-Impedance Analyzer BIA (Inbody 770, Inbody Co, Seoul, Korea)11. To calculate participants’ physical activity, the PERSIAN Cohort standard physical activity questionnaire which consisted of 22 items was applied. Then, participants were categorized into light, moderate, and high according to physical activity intensity. More details on the measurement standard protocols have been published elsewhere11.
Statistical analysis
Dietary fats including SFA, PUFA, MUFA and SFA were adjusted for total energy intake through residual method introduced by Willett15. Based in this model, energy-adjusted dietary fats are calculated from the regression model, while the dietary fats considered as a dependent variable and total dietary energy intake as an independent variable. All participants were categorized according to the quartile of energy-adjusted dietary fats and the first quartile were considered as reference. General characteristics of study subjects across the quartile categories of energy-adjusted dietary fats were compared using ANOVA analysis for continuous data and Chi-square analysis for categorical variables. All categorical data are shown as (%), and continuous data are depicted as mean ± standard deviation (SD). To examine the association between SFA, PUFA, MUFA and SFA and risk of HTN incident, Cox proportional hazards analyses were applied to estimate hazard ratios (HR) and 95% confidence intervals (CIs). The time covariate for each subject was defined as the time interval between the baseline entry of cohort data and the incidence of a HTN event. Three cox regression models were defined to adjust for protentional confounders. Model 1 was a crude model. In model 2, we controlled the association for sex (male/female) and age (years). In the third model, we additionally adjusting the association for residence type (rural/urban), marital status, BMI, smoking, SES, history of diabetes, cardiovascular diseases (CVD) history, tertiles of physical activity, tertiles of education, energy intake (kcal/d), sodium (g/d), magnesium (mg/d), carbohydrate (%), protein (%) and healthy eating index-2015 score. Subgroup analyses based on sex and resident type were also performed. All of the statistical analyses were analyzed using SPSS software (version 26). The significance level was set at a P value less than 0.05.
Ethical approval and consent to participate
The Ethics Committee of Kermanshah University of Medical Sciences approved the study (KUMS.REC. 1400.670). All methods were carried out in accordance with relevant guidelines and regulations. The study was conducted in accordance with International Conference on Harmonisation and the ethical principles of the Declaration of Helsinki. All the participants were provided written informed consent.
Result
Among 7359 participants free of HTN at baseline, a total of 597 (8.11%) new cases of HTN were diagnosed through an average of 6.4 ± 1.33 years of follow-up. Table 1 indicates the baseline characteristics of RaNCD participants by quartiles of dietary TFA, SFA, MUFA, and PUFA intakes. Subjects with the greatest intake of SFA were more likely to be female, residents in rural areas, low SES, educated, and less likely to be a smoker and married. Also, these subjects have lower SBP and DBP. Participants with higher dietary intake of MUFA were more likely to be younger, have lower SBP, female, residents in urban areas, higher SES, and less likely to be educated and physically active. Concerning dietary PUFA intake, subjects consuming higher amounts were younger, and heavier, more likely to be female, urban residents, and higher SES, while less likely to be smokers, physically active, and educated. Participants at the top quartile of TFA intake had younger, lower SBP and DBP, were more likely to be female, urban residents, and higher SES, while less probable to be physically active, educated, smokers, and had CVD or diabetes history.
Dietary nutrient intake of the study participants across quartile categories of dietary fatty acids is shown in Table 2. Participants at the highest quartile of SFA intake had a lower intake of energy, carbohydrate, protein, potassium, fiber, and magnesium, and also had a higher intake of dietary fat, sodium, and calcium. Subjects in the top quartile of MUFA intake consume a greater amount of fat and potassium while consuming a lower amount of energy, carbohydrate, protein, fiber, sodium, and magnesium. Dietary intake of energy, carbohydrate, sodium, and calcium declined with increasing intake of PUFA. However, dietary intake of fat, fiber, protein, potassium, and magnesium increased with rising dietary PUFA intake. Concerning dietary TFA intake, participants at the fourth quartile had a lower intake of energy, carbohydrate, fiber, sodium, potassium calcium, and magnesium.
HR and 95% CI of HTN according to dietary fatty acids quartile categories are given in Table 3. In model 1 (crude) and model 2 (controlled for age and sex), no significant link was observed between the top vs. bottom quartile of dietary SFA, MUFA, PUFA, and TFA and the risk of HTN. In model 3, after adjusting for all confounders including residence type (rural/urban), marital status, BMI, smoking, SES, history of diabetes, and cardiovascular diseases (CVD), tertiles of physical activity, tertiles of education, energy intake (kcal/d), sodium (g/d), magnesium (mg/d), carbohydrate (%), protein (%) and healthy eating index-2015 score, we did not find any significant link of the fourth compared to the first categories of dietary SFA (HR: 0.82, 95% CI 0.55, 1.21; P trend: 0.476), MUFA (HR: 0.71, 95% CI 0.48, 1.06; P trend: 0.252), PUFA (HR: 0.86, 95% CI 0.62, 1.19; P trend: 0.315) and TFA (HR: 0.99, 95% CI 0.76, 1.27; P trend: 0.675), and HTN risk. However, continuous analysis revealed that each gram per day increase in dietary MUFA intake was associated with lower risk of HTN (HR: 0.97; 95% CI 0.94, 0.99; P: 0.044).
Subgroup analyses for sex and resident type by dietary fatty acids intake and risk hypertension are depicted in Table 4. No significant relationship was observed between dietary SFA, MUFA, PUFA, and TFA intakes and HTN risk across subgroups of sex and resident type.
Discussion
The current prospective cohort study on Iranian Kurdish adults revealed that higher dietary MUFA intake was protectively associated with HTN risk, while dietary SFA, TFA, and PUFA intakes were not related to the risk of HTN. The associations were independent of age, gender, residence type, marital status, BMI, smoking, SES, history of diabetes and CVD, physical activity, education, energy intake, sodium, magnesium, carbohydrate, protein and healthy eating index-2015 score. As far as we know, there is a limited cohort study available on the association between dietary fatty acid intake and HTN in the middle east countries.
A survey in 2010 estimated that out of 1.39 billion adults with HTN worldwide, 1.04 billion live in low and middle-income countries16. Higher blood pressure is strongly and independently associated with the risk of CVD, ESRD, and mortality1. Therefore, reductions in HTN risk factors are suggested for the prevention and control of this disease1. In our study, dietary MUFA intake was protectively related to HTN incidence, whereas dietary SFA, TFA, and PUFA intakes did not significantly relate to HTN. In line with the findings, a randomized controlled parallel trial in five European countries indicated that SBP and DBP were significantly decreased by following a high MUFA diet but did not change by adherence to a high SFA diet17. Moreover, two other RCTs in a population at risk of CVD showed high MUFA diet compared to a high carbohydrate diet could significantly reduce blood pressure18,19. A cross-sectional survey in the USA revealed that after controlling for all protentional covariates dietary MUFA intake was inversely associated with systolic and diastolic blood pressure20. Similar to our results, two prospective cohort studies on US men9 and women21 adults after four years of follow-up did not find any significant relationships between dietary SFA or PUFA intake and HTN risk. In the same way, a cross-sectional analysis conducted on 18 countries in North America, Asia, Europe, South America, and Africa showed that dietary MUFA intake was inversely related to the odds of HTN, while dietary SFA intake was not associated with HTN7. In contrast to our results, in a prospective cohort study on 11 342 US adults, PUFA intake was inversely related to blood pressure, while SFA intake was positively associated with blood pressure8. Finding from another prospective cohort study on 28,100 US women, indicated that TFA intake was significantly related to developing risk of HTN, while MUFA, SFA, and PUFA intakes were not associated10. It is worth noting that the inconsistency in the association between dietary fatty acids intake and hypertension risk could be attributed to variations in the study region, the demographics of the population (age, gender), the type of dietary questionnaire, and the consideration of the energy adjustment of fatty acid intake. Although studies reported mixed results, it seems dietary MUFA intake might have a protective association with HTN.
The beneficial effect of MUFA intake on blood pressure might be due to improvement on the coronary vascular function by increased high-density lipoprotein (HDL) and reduced low-density lipoprotein (LDL) and22. Second plausible mechanism is that MUFA by decreasing the inflammatory markers, atherosclerotic lesions, levels of non-esterified fatty acids and trimethylamine-N-oxide level could improve endothelial function23. Insulin sensitivity improvement is another suggested mechanism of MUFA which may reduce sympathetic nervous system, sodium retention, and peripheral resistance24,25.
Strengths of the current study included the large population in the middle-east country and detailed information over 6.4 years follow up. However, some limitations are unavoidable. First, although we adjusted dietary intake for total energy, measurement errors may still be probable for the dietary assessment. Second, residual confounding factors likely remained even after controlling the association for all covariates. Because our study conducted on Iranian Kurdish ethnicity, generalizing our results to other populations with different demographic characteristics should be done with caution.
Conclusions
In conclusion, our findings demonstrated that higher dietary MUFA intake was protectively related with HTN risk. Other dietary fatty acids including PUFA, SFA, and TFA were not related to HTN incident. Dietary MUFA rich foods such as canola oil, peanut oil, nuts, olive oil, vegetables, and fruits should be encouraged to improve blood pressure.
Data availability
All data generated and analyzed during this study are included in the manuscript.
Abbreviations
- BMI:
-
Body mass index
- WHR:
-
Waist-to-hip ratio
- DBP:
-
Diastolic blood pressure
- SBP:
-
Systolic blood pressure
- SES:
-
Socioeconomic status
- CVD:
-
Cardiovascular disease
- HTN:
-
Hypertension
- SFA:
-
Saturated fatty acid
- MUFA:
-
Monounsaturated fatty acid
- TFA:
-
Trans fatty acids
- PUFA:
-
Polyunsaturated fatty acid
References
Mills, K. T., Stefanescu, A. & He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 16, 223–237 (2020).
Heidenreich, P. A. et al. Forecasting the future of cardiovascular disease in the United States: A policy statement from the American Heart Association. Circulation 123, 933–944 (2011).
Afsargharehbagh, R. et al. Hypertension and pre-hypertension among Iranian adults population: A meta-analysis of prevalence, awareness, treatment, and control. Current Hypertens. Rep. 21, 1–13 (2019).
Liu, Q. Impact of different dietary fat sources on blood pressure in Chinese adults. PLoS ONE 16, e0247116 (2021).
Hall, W. L. Dietary saturated and unsaturated fats as determinants of blood pressure and vascular function. Nutr. Res. Rev. 22, 18–38 (2009).
Nestel, P. J. Dietary fat and blood pressure. Current Hypertens. Rep. 21, 1–6 (2019).
Mente, A. et al. Association of dietary nutrients with blood lipids and blood pressure in 18 countries: A cross-sectional analysis from the PURE study. Lancet Diabetes Endocrinol. 5, 774–787 (2017).
Stamler, J., Caggiula, A., Grandits, G. A., Kjelsberg, M. & Cutler, J. A. Relationship to blood pressure of combinations of dietary macronutrients: Findings of the Multiple Risk Factor Intervention Trial (MRFIT). Circulation 94, 2417–2423 (1996).
Ascherio, A. et al. A prospective study of nutritional factors and hypertension among US men. Circulation 86, 1475–1484 (1992).
Wang, L. et al. Dietary fatty acids and the risk of hypertension in middle-aged and older women. Hypertension 56, 598–604 (2010).
Pasdar, Y. et al. Cohort Profile: Ravansar non-communicable disease cohort study: The first cohort study in a Kurdish population. Int. J. Epidemiol. 48, 682–683f. https://doi.org/10.1093/ije/dyy296 (2019).
Hamzeh, B. et al. Predicting metabolic syndrome by anthropometric measures among adults 35–65 years in the west of Iran; a cross sectional study from an Iranian RaNCD cohort data. Diabetes Metab. Syndr. 14, 1293–1298. https://doi.org/10.1016/j.dsx.2020.07.017 (2020).
Lopez-Garcia, E. et al. Major dietary patterns are related to plasma concentrations of markers of inflammation and endothelial dysfunction. Am. J. Clin. Nutr. 80, 1029–1035 (2004).
Azar, M. & Sarkisian, E. Food Composition Table of Iran: National Nutrition and Food Research Institute (Shaheed Beheshti University, 1980).
Willett, W. C., Howe, G. R. & Kushi, L. H. Adjustment for total energy intake in epidemiologic studies. Am. J. Clin. Nutr. 65, 1220S-1228S (1997).
Mills, K. T. et al. Global disparities of hypertension prevalence and control: A systematic analysis of population-based studies from 90 countries. Circulation 134, 441–450 (2016).
Rasmussen, B. M. et al. Effects of dietary saturated, monounsaturated, and nJ3 fatty acids on blood pressure in healthy subjects1–3. Am. J. Clin. Nutr. 83, 221–226 (2006).
Appel, L. J. et al. Effects of protein, monounsaturated fat, and carbohydrate intake on blood pressure and serum lipids: Results of the OmniHeart randomized trial. Jama 294, 2455–2464 (2005).
Shah, M. et al. Effect of a high-carbohydrate versus a high—Cis-Monounsaturated fat diet on blood pressure in patients with type 2 diabetes. Diabetes Care 28, 2607–2612 (2005).
Williams, P. T. et al. Associations of dietary fat, regional adiposity, and blood pressure in men. Jama 257, 3251–3256 (1987).
Witteman, J. et al. A prospective study of nutritional factors and hypertension among US women. Circulation 80, 1320–1327 (1989).
Vafeiadou, K. et al. Replacement of saturated with unsaturated fats had no impact on vascular function but beneficial effects on lipid biomarkers, E-selectin, and blood pressure: Results from the randomized, controlled Dietary Intervention and VAScular function (DIVAS) study. Am. J. Clin. Nutr. 102, 40–48 (2015).
Tsutsumi, R. et al. Long-chain monounsaturated fatty acids improve endothelial function with altering microbial flora. Transl. Res. 237, 16–30. https://doi.org/10.1016/j.trsl.2021.03.016 (2021).
Vessby, B. et al. Substituting dietary saturated for monounsaturated fat impairs insulin sensitivity in healthy men and women: The KANWU Study. Diabetologia 44, 312–319 (2001).
Visioli, F. & Galli, C. Biological properties of olive oil phytochemicals. Crit. Rev. Food Sci. Nutr. 42, 209–221 (2002).
Acknowledgements
The authors thank the PERSIAN cohort Study collaborators and of Kermanshah University of Medical Sciences. The Iranian Ministry of Health and Medical Education has also contributed to the funding used in the PERSIAN Cohort through Grant no 700/534.
Funding
This research was supported by the Kermanshah University of Medical Sciences (Grant Number: 4010177).
Author information
Authors and Affiliations
Contributions
E.S.H., F.N., Y.P., M.H.S.H. and J.N. contributed to design the study. AB analyzed the data and wrote the manuscript. E.S.H., F.N. and M.M.N. extensively reviewed and edited the manuscript. All authors support the submission to this journal.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Shakiba, E., Najafi, F., Pasdar, Y. et al. A prospective cohort study on the association between dietary fatty acids intake and risk of hypertension incident. Sci Rep 13, 21112 (2023). https://doi.org/10.1038/s41598-023-48256-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-48256-5
- Springer Nature Limited