Abstract
We aimed to investigate the alterations of thalamic nuclei volumes and intrinsic thalamic network in patients with primary restless legs syndrome (RLS) compared to healthy controls. Seventy-one patients with primary RLS and 55 healthy controls were recruited. They underwent brain MRI using a three-tesla MRI scanner, including three-dimensional T1-weighted images. The intrinsic thalamic network was determined using graph theoretical analysis. The right and left whole thalamic volumes, and the right pulvinar inferior, left ventral posterolateral, left medial ventral, and left pulvinar inferior nuclei volumes in the patients with RLS were lower than those in healthy controls (0.433 vs. 0.447%, p = 0.034; 0.482 vs. 0.502%, p = 0.016; 0.013 vs. 0.015%, p = 0.031; 0.062 vs. 0.065%, p = 0.035; 0.001 vs. 0.001%, p = 0.034; 0.018 vs. 0.020%, p = 0.043; respectively). There was also a difference in the intrinsic thalamic network between the groups. The assortative coefficient in patients with RLS was higher than that in healthy controls (0.0318 vs. − 0.0358, p = 0.048). We demonstrated the alterations of thalamic nuclei volumes and intrinsic thalamic network in patients with RLS compared to healthy controls. These changes might be related to RLS pathophysiology and suggest the pivotal role of the thalamus in RLS symptoms.
Similar content being viewed by others
Introduction
Restless legs syndrome (RLS) is the most significant of the sleep related movement disorders, causing significant health and personal morbidity, including chronic sleep deprivation, depression, and anxiety1,2. In studies, RLS of varying severity affects between 3.9% and 15% of adults, and females have a higher rate than males2,3,4,5. However, RLS has been not widely recognized, diagnosed, and treated.
Although the exact pathogenesis for RLS has not been clearly demonstrated, there have been many studies and various causes have been suggested. Among them, reduced regional brain iron stores6,7,8 and dopaminergic system dysfunction9,10 are the most consistently implicated central nervous system abnormalities. Lower peripheral iron status has been associated with an increased risk of developing and worsening RLS symptoms, and both brain magnetic resonance imaging (MRI) and ultrasound imaging studies have revealed iron deficiency in the region of the substantia nigra in patients with RLS6,7,8. The observation that dopaminergic therapy improves RLS symptoms strongly implicates the pivotal role of dopamine in the pathogenesis of RLS, and the dopamine transporter is decreased in the striatum of patients with RLS, demonstrated by positron emission tomography studies9,10.
RLS is defined by sensory symptoms, not movement, and is based on the essential characteristic of a frequently unpleasant or inconvenient urge to move the legs that occurs during periods of inactivity, particularly in the evenings, and is temporarily alleviated by movement1,2. Because the main features of RLS are sensory symptoms, we focused on the thalamus in this study, which is the most important sensory-associated structure in the brain. Previous studies have also frequently reported thalamic abnormalities in patients with RLS11. A study using proton magnetic resonance spectroscopy has demonstrated decreased metabolite activity in the medial thalamus with decreased N-acetyl aspartate to creatine ratio12. In a small pathologic study, the number of beta-endorphin and met-enkephalin positive cells in the thalamus was reduced in patients with RLS compared to healthy controls13. These studies suggest the association between the thalamus and RLS pathophysiology.
Recently, neuroimaging has been widely used to investigate the pathophysiologic mechanisms for various neurological diseases, with breakthrough developments of techniques for MRI scanning and analysis. A new technical tool generates a parcellation of the thalamus into 25 distinct nuclei using a probabilistic atlas constructed from histological data14. By utilizing this tool, it is possible to measure each individual thalamic nuclei volume, as well as the total volume of the thalamus. These MRI-based thalamic nuclei volume analysis has demonstrated a good agreement with histological findings and showed an excellent test–retest reliability14. The various thalamic nuclei have a distinct location and function, and each thalamic nuclei is connected differently to a specific brain regions. In addition, a graph theoretical analysis based on these thalamic nuclei volumes allows the calculation of the intrinsic thalamic network in subjects15,16,17. Graph theory metrics can provide a valuable assessments and sophisticated characterization of the intrinsic thalamic network. Thus, structural co-variance analysis based on the thalamic nuclei volumes with a graph theory could conceptualize how morphological properties of different thalamic nuclei relate to each other at the group level, which could be related with RLS pathophysiology. However, there have been no studies to investigate the change of thalamic nuclei volumes or intrinsic thalamic network in patients with RLS compared to healthy controls.
In this study, we aimed to investigate the changes in thalamic nuclei volumes and the intrinsic thalamic network in patients with primary RLS compared to healthy controls. We hypothesized that there were significant changes in the thalamic nuclei volumes and intrinsic thalamic network in patients with RLS.
Results
Demographic and clinical characteristics
Table 1 reveals the demographic and clinical characteristics in patients with RLS and healthy controls. The ages and sex were not significantly different (age, 56.4 vs. 55.4 years, p = 0.415; males, 18/71 (25%) vs. females, 17/55 (30%), p = 0.491; respectively). However, the Pittsburgh sleep quality index, Insomnia severity index, Hospital anxiety scale, and Hospital depression scale were higher in patients with RLS than healthy controls (12 vs. 4, p < 0.001; 17 vs. 3, p < 0.001; 7 vs. 4, p < 0.001; 8 vs. 5, p = 0.001; respectively). Of the 71 patients with RLS, 21 patients (29.5%) were already taking medication to relieve RLS symptoms prior to MRI scanning (drug-treated state), whereas the 50 patients (70.5%) were drug-naïve state for RLS.
Whole thalamic volumes and individual thalamic nuclei volumes
Table 2 shows the difference of whole thalamic volumes and individual thalamic nuclei volumes between patients with RLS and healthy controls. There were significant differences in whole thalamic volumes and some thalamic nuclei volumes between the groups. The right and left whole thalamic volumes in the patients with RLS were lower than those in healthy controls (0.433 vs. 0.447%, p = 0.034; 0.482 vs. 0.502%, p = 0.016; respectively). Furthermore, the right pulvinar inferior, left ventral posterolateral, left medial ventral, and left pulvinar inferior nuclei volumes in the patients with RLS were lower than those in healthy controls (0.013 vs. 0.015%, p = 0.031; 0.062 vs. 0.065%, p = 0.035; 0.001 vs. 0.001%, p = 0.034; 0.018 vs. 0.020%, p = 0.043; respectively).
In the comparison of the RLS patients with drug-naïve state and healthy controls, the right and left whole thalamic volumes in the patients with RLS were also lower than those in healthy controls (0.431 vs. 0.447%, p = 0.006; 0.478 vs. 0.502%, p = 0.034; respectively). Additionally, the right pulvinar medial, right pulvinar inferior, left lateral posterior, left ventral posterolateral, left ventro-medial, left medial ventral, left medial geniculate, left pulvinar medial, and left pulvinar inferior nuclei volumes in the patients with RLS were lower than those in healthy controls (0.065 vs. 0.070%, p = 0.031; 0.013 vs. 0.023%, p = 0.012; 0.009 vs. 0.009%, p = 0.014; 0.061 vs. 0.065%, p = 0.012; 0.015 vs. 0.017%, p = 0.012; 0.001 vs. 0.001%, p = 0.010; 0.078 vs. 0.085%, p = 0.012; 0.079 vs. 0.085%, p = 0.016; 0.018 vs. 0.020%, p = 0.014; respectively).
In the comparison of the RLS patients with drug-treated state and healthy controls, the right and left whole thalamic volumes in the patients with RLS were not different from those in healthy controls. Furthermore, any of the thalamic nuclei volumes were not different between the groups.
Intrinsic thalamic network
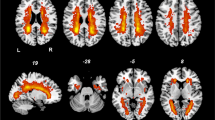
There was a significant difference in intrinsic thalamic network between patients with RLS and healthy controls (Table 3) (Fig. 1). The assortative coefficient in patients with RLS was higher than that in healthy controls (0.0318 vs. − 0.0358, p = 0.048). The other network measures, including characteristic path length, mean clustering coefficient, and small-worldness index were not different between the groups.
In the comparison of the RLS patients with drug-naïve state and healthy controls, the assortative coefficient in patients with RLS was also higher than that in healthy controls (0.0374 vs. − 0.0358, p = 0.040). The other network measures were not different between the groups.
In the comparison of the RLS patients with drug-treated state and healthy controls, the intrinsic thalamic network between the patients with RLS and healthy controls was not different.
Correlation analysis between thalamic nuclei volumes and RLS severity, Pittsburgh sleep quality index, insomnia severity index, hospital anxiety scale and hospital depression scale
No individual thalamic nuclei volumes were significantly correlated with RLS severity (Supplementary Table 1). However, the right thalamic volume was correlated with the Insomnia severity index (r = − 0.281, p = 0.038).
Discussion
In this study, we newly found that (1) patients with RLS had decreased whole thalamic volumes and some thalamic nuclei volumes, especially the pulvinar inferior, ventral posterolateral, and medial ventral nuclei, compared to healthy controls; (2) there were alterations of the intrinsic thalamic network in patients with RLS; (3) these thalamic alterations were consistently observed even in RLS patients with drug-naïve state; and (4) the whole thalamic and thalamic nuclei volumes as well as the intrinsic thalamic network were not different between RLS patients with drug-treated state and healthy control. These changes might be related to RLS pathophysiology and suggest the pivotal role of the thalamus in RLS symptoms.
The thalamus serves a variety of functions, but it is most commonly thought to act as a hub for the sensory system, relaying information between various subcortical areas and the cerebral cortex18. The thalamus receives and transmits sensory signals to the associated primary cortex area. Furthermore, the thalamus has traditionally been thought of as simply a “relay” for signals to the cerebral cortex18. However, recent research indicates that the thalamus is more selective and performs a higher order relay function, which is a part of the cortico-thalamo-cortical route of communication19. In this study, we found that patients with RLS had lower whole thalamic volumes in both sides than healthy controls. The abnormal sensory processing by thalamic abnormalities reflected with decreased thalamic volumes might lead to sensory symptoms in patients with RLS. These findings are consistent with our previous study discussion of the role of “resting keeper” in the thalamus20,21, in which the thalamus could suppress symptoms during a resting state and play an important role in managing RLS symptoms.
Of the several thalamic nuclei, the volumes of the pulvinar inferior, ventral posterolateral, and medial ventral nuclei in patients with RLS were significantly lower than those in healthy controls. The pulvinar inferior thalamic nucleus has widespread connections with the visual cortex, and lesions of the pulvinar region result in visual deficits22. In addition, ischemic stroke to the pulvinar nucleus has been linked to the development of chronic pain22. The ventral posterolateral thalamic nucleus receives sensory information for the body from the spinothalamic tract and the posterior column-medial pathway’s lemniscus. This sensory information is then projected to the primary sensory cortex23. Thus, the decreased volumes in the pulvinar inferior and ventral posterolateral nuclei are related with the main sensory symptoms of RLS. Furthermore, RLS is a sleep related movement disorder characterized by a compulsive urge to move the legs (ie, akathisia). In addition, involuntary movements of the legs, known as periodic limb movements, are frequently present. These sensorimotor symptoms can be associated with decreased volume in the medial ventral thalamic nucleus, which receives afferents from the basal ganglia and communicates information to the cerebral cortex, including motor areas24. Thus, the medial ventral thalamic nucleus is associated with at least some aspects of motor function as well as other cortical functions24.
We also demonstrated that there were alterations of the intrinsic thalamic network in patients with RLS. Although this is the first study to analyze the intrinsic thalamic network using the covariance analysis method by applying the thalamic nuclei volume-based graph theory, thalamic network alteration has been proven in previous studies using resting state functional MRI (rs-fMRI). Ku et al. enrolled patients with RLS and healthy controls who had undergone rs-fMRI25. They discovered that patients with RLS had decreased thalamic connectivity to the parahippocampal, precentral, and lingual gyri, but increased connectivity to the superior temporal, middle temporal, and medial frontal gyri. Additionally, the severity of RLS was negatively correlated with the thalamic-parahippocampal gyrus connection25. This finding that RLS is a disorder of the thalamic network was later confirmed in another follow-up study26. The study used rs-fMRI on patients with RLS and healthy controls, and assessed functional connectivity changes in the subjects using a seed-based technique utilizing the bilateral ventral and posterolateral thalamic nuclei, and decreased functional connectivity was observed in the bilateral lingual gyri26. Our present study revealed that the assortative coefficient in patients with RLS was higher than that in healthy controls. Interestingly, patients with RLS had positive values of assortative coefficients, which is called an assortative network, whereas healthy controls had negative value of assortative coefficient, defined as a disassortative network27,28. In an assortative network, a node with many links, that is a hub, is clustered with hubs, whereas nodes with few links are grouped with similar nodes with few links27,28. However, in a disassortative network, nodes with many links and nodes with few links are connected. The assortative coefficient quantifies assortativity, or the proclivity of nodes sharing similar properties to connect. Numerous technological and biological networks serve as models for a disassortative network29. Additionally, we discovered that healthy controls had a disassortative intrinsic thalamic network in this study. However, in patients with RLS, the intrinsic thalamic network was assortative, which appears to be more difficult to synchronize than a disassortative network30. We could assume that less synchronization of the thalamus is associated with dysfunction of the thalamus.
In this study, we firstly investigated the alterations of thalamic nuclei volumes and intrinsic thalamic network in patients with RLS compared to healthy controls, and we enrolled a relatively large sample size of participants. However, there were several limitations. First, less than one-third of the patients with RLS were already taking medication to relieve RLS symptoms prior to MRI scanning. These medications may have affected the volume of the thalamic nuclei. Thus, we additionally analyzed the thalamic changes in RLS patients with drug-naïve state, and we confirmed the alterations of thalamic nuclei volumes and intrinsic thalamic network compared to healthy controls. The whole thalamic and thalamic nuclei volumes as well as the intrinsic thalamic network were not different between RLS patients with drug-treated state and healthy control, which could suggest that thalamic function could return to normal condition by RLS treatment. However, since this study had a cross-sectional design, it was not possible to prove it, and this assumption could be confirmed through the further study with design of longitudinal follow-up MRI scan before and after RLS treatment. Second, our results could not be generalized because the patients were enrolled at a sleep specialist center in one tertiary hospital. Third, because this study was conducted by cross-sectional design, it is difficult to know the causal relationship. Fourth, we could not analyze thalamic changes according to which leg had the dominant RLS symptoms. Lastly, although we measured thalamic nuclei volumes by structural imaging, it is difficult to rule out the possibility that the results may vary depending on the time of MRI scan, because RLS symptoms are more severe at night. In the future, further longitudinal studies with multicenter considering the time of MRI scanning are needed to confirm our findings.
In this study, we demonstrate the alterations of thalamic nuclei volumes and intrinsic thalamic network in patients with RLS compared to healthy controls. These changes might be related with RLS pathophysiology and suggest the pivotal role of the thalamus in RLS symptoms.
Methods
Participants: patients with RLS and healthy controls
Seventy-one patients with primary RLS and 55 healthy controls were recruited at a sleep center in a tertiary hospital. This study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The study was approved by the institutional review board of the Keimyung University Dongsan Hospital. Informed consent was obtained from all participating subjects. All methods were carried out in accordance with relevant guidelines and regulations. We enrolled patients with RLS who met the following criteria: (1) primary RLS diagnosed by a certified Korean neurologist (YWC) who is an expert in RLS using the International RLS/WED Study Group (IRLSSG) criteria1; (2) no structural lesions on the brain MRI; and (3) no other medical or neurological conditions, except RLS. Patients with secondary RLS due to iron deficiency anemia, pregnancy, chronic kidney disease, or peripheral neuropathy were excluded from the study. Additionally, we recruited healthy subjects as a control group, whose age and gender were comparable to those of the RLS patients. The healthy controls all answered “no” to the RLS diagnostic questionnaire’s initial questions; they had normal brain MRI scans and were free of any medical or neurological conditions.
The International RLS scale was used to assess the severity of RLS symptoms in the study group31,32. Additionally, the following scales were assessed with validated Korean-language versions of sleep questionnaires: (1) the Restless Legs Syndrome Quality of Life Questionnaire32,33; (2) the Insomnia Severity Index34; (3) the Pittsburgh Sleep Quality Index35; and (4) the Hospital Anxiety and Depression Scale36.
MRI acquisition: T1-wighed imaging
Patients with RLS and the healthy controls underwent brain MRI using a three-tesla MRI scanner equipped with a 32-channel head coil. Three-dimensional T1-weighted images were acquired using a turbo-field echo sequence with the following parameters: TI = 1300 ms; TR/TE = 8.6/3.96 ms; flip angle = 8°; and isotropic voxel size of 1 mm3.
Obtaining individual thalamic nuclei volumes
We obtained whole thalamic volumes and individual thalamic nuclei volumes using the FreeSurfer program (version 7.0). We used the “recon-all” and “segmentThalamicNuclei.sh” functions to automatically obtain the right and left whole thalamic volumes and individual thalamic nuclei volume, respectively14. An example of segmentation of thalamic nuclei is demonstrated in Fig. 2. The individual thalamic nuclei included:
-
Right and left anteroventral nuclei in the anterior group.
-
Right and left laterodorsal and lateral posterior nuclei in the lateral group.
-
Right and left ventral anterior, ventral anterior magnocellular, ventral lateral anterior, ventral lateral posterior, ventral posterolateral, and ventromedial nuclei in the ventral group.
-
Right and left central medial, central lateral, paracentral, centromedian, and parafascicular nuclei in the intralaminar group.
-
Right and left paratenial, medial ventral, mediodorsal medial magnocellular, and mediodorsal lateral parvocellular nuclei in the medial group.
-
Right and left lateral geniculate, medial geniculate, suprageniculate, pulvinar anterior, pulvinar medial, pulvinar lateral, pulvinar inferior nuclei in the posterior group.
Example of thalamic nuclei segmentation. Segmentations and labels of thalamic nuclei in the coronal (a) and axial (b) plane generated by FreeSurfer (not all segmentations are shown). The segmentations are overlaid on the T1-weighted scan. This figure is generated from our previous study17. MDl Mediodorsal lateral parvocellular nucleus, MDm Mediodorsal medial magnocellular nucleus, VLa Ventral lateral anterior nucleus, VLp Ventral lateral posterior nucleus, VPL Ventral posterolateral nucleus, VA Ventral anterior nucleus.
Then, we corrected the whole thalamic volumes and individual thalamic nuclei volumes by the total intracranial volume. Finally, we investigated the differences in whole thalamic volumes and individual thalamic nuclei volumes between patients with RLS and the healthy controls. In addition, we analyzed the differences in whole thalamic volumes and individual thalamic nuclei volumes between RLS patients with drug-naïve state and the healthy controls, and between RLS patients with drug-treated state and the healthy controls.
Calculation of intrinsic thalamic network using graph theory and correlation analysis
We previously described the detailed procedure to compute the intrinsic thalamic network using graph theoretical analysis in the BRAPH version 1.0 program15,16,17,37. Graph theory was used to analyze the network’s nodes and edges. We defined nodes as the individual thalamic nuclei volumes, and edges as the partial correlation between the individual thalamic nuclei volumes, while accounting for the effects of age and sex. We created a weighted connectivity matrix from nodes and edges in patients with RLS and healthy controls. Binary links denote the presence or absence of connections, whereas weighted links contain information about connection strength with respective magnitudes of correlational interactions. We subsequently calculated network measures, including characteristic path length, mean clustering coefficient, assortative coefficient, and small-worldness index from the connectivity matrix. The characteristic path length represents the shortest path length between the nodes, which is associated with global integration of the network. The mean clustering coefficient is a measure for the tendency of network elements to form local clusters, and the assortative coefficient is the values for degree of connections between nodes with similar degrees. The small-worldness index describes the balance between local connectedness and global integration in the network38,39. These are the most commonly used measures to analyze network topology in graph theory38,39. We then analyzed the differences in the network measures between patients with RLS and healthy controls, between RLS patients with drug-naïve state and healthy controls, and between RLS patients with drug-treated state and the healthy controls. We also performed a correlation analysis between individual thalamic nuclei volumes and the RLS severity, the Pittsburgh Sleep Quality Index, the Insomnia Severity Index, and the Hospital Anxiety and Depression Scale in patients with RLS.
Statistical analysis
Categorical variables were expressed as frequency with percentages, while continuous variables were expressed as mean value with standard deviation (SD) or median value with interquartile range, depending on the normal distribution. In the comparison of the clinical characteristics, the Chi-square test was used to analyze categorical variables, and the independent samples t-test or Mann–Whitney test was used to analyze continuous variables according to the normal distribution. In the comparison of the whole thalamic volumes and thalamic nuclei volumes between the groups, we used an analysis of covariance (ANCOVA) with covariates of age and sex. Pearson’s correlation analysis was used for correlation analysis. We compared network measures using nonparametric permutation tests with 1,000 permutations because we could obtain network measures at the group level. Permutation tests were conducted with the BRAPH program. Multiple false discovery rate corrections (Benjamini–Hochberg procedure)40 were used in the comparisons of differences for whole thalamic volumes, individual thalamic nuclei volumes, and network measures between the groups, and in the correlation analysis. MedCalc® Statistical Software version 20.014 (MedCalc Software Ltd, Ostend, Belgium; https://www.medcalc.org; 2021) was used to conduct the statistical analyses. The adjusted p value was then displayed. Statistical significance was defined as p values less than 0.05.
Data availability
All data generated or analyzed during this study are included in this published article (and its Supplementary Information files).
References
Allen, R. P. et al. Restless legs syndrome/Willis-Ekbom disease diagnostic criteria: Updated International Restless Legs Syndrome Study Group (IRLSSG) consensus criteria–history, rationale, description, and significance. Sleep Med. 15, 860–873. https://doi.org/10.1016/j.sleep.2014.03.025 (2014).
Yeh, P., Walters, A. S. & Tsuang, J. W. Restless legs syndrome: A comprehensive overview on its epidemiology, risk factors, and treatment. Sleep Breath 16, 987–1007. https://doi.org/10.1007/s11325-011-0606-x (2012).
Cho, Y. et al. Epidemiology of restless legs syndrome in Korean adults. Sleep 31, 219–223 (2008).
Berger, K., Luedemann, J., Trenkwalder, C., John, U. & Kessler, C. Sex and the risk of restless legs syndrome in the general population. Arch. Intern. Med. 164, 196–202. https://doi.org/10.1001/archinte.164.2.196164/2/196[pii] (2004).
Ohayon, M. M., O’Hara, R. & Vitiello, M. V. Epidemiology of restless legs syndrome: A synthesis of the literature. Sleep Med. Rev. 16, 283–295. https://doi.org/10.1016/j.smrv.2011.05.002 (2012).
Allen, R. P., Barker, P. B., Wehrl, F. W., Song, H. K. & Earley, C. J. MRI measurement of brain iron in patients with restless legs syndrome. Neurology 56, 263–265. https://doi.org/10.1212/wnl.56.2.263 (2001).
Godau, J., Klose, U., Di Santo, A., Schweitzer, K. & Berg, D. Multiregional brain iron deficiency in restless legs syndrome. Mov. Disord. 23, 1184–1187. https://doi.org/10.1002/mds.22070 (2008).
Allen, R. P., Earley, C. J., Jones, B. C. & Unger, E. L. Iron-deficiency and dopaminergic treatment effects on RLS-Like behaviors of an animal model with the brain iron deficiency pattern of the restless legs syndrome. Sleep Med. 71, 141–148. https://doi.org/10.1016/j.sleep.2020.01.024 (2020).
Earley, C. J. et al. The dopamine transporter is decreased in the striatum of subjects with restless legs syndrome. Sleep 34, 341–347. https://doi.org/10.1093/sleep/34.3.341 (2011).
Lv, Q., Wang, X., Asakawa, T. & Wang, X. P. Pharmacologic treatment of restless legs syndrome. Curr. Neuropharmacol. 19, 372–382. https://doi.org/10.2174/1570159X19666201230150127 (2021).
Rizzo, G., Li, X., Galantucci, S., Filippi, M. & Cho, Y. W. Brain imaging and networks in restless legs syndrome. Sleep Med. 31, 39–48. https://doi.org/10.1016/j.sleep.2016.07.018 (2017).
Rizzo, G. et al. Abnormal medial thalamic metabolism in patients with idiopathic restless legs syndrome. Brain J. Neurol. 135, 3712–3720. https://doi.org/10.1093/brain/aws266 (2012).
Walters, A. S., Ondo, W. G., Zhu, W. & Le, W. Does the endogenous opiate system play a role in the Restless Legs Syndrome? A pilot post-mortem study. J. Neurol. Sci. 279, 62–65. https://doi.org/10.1016/j.jns.2008.12.022 (2009).
Iglesias, J. E. et al. A probabilistic atlas of the human thalamic nuclei combining ex vivo MRI and histology. Neuroimage 183, 314–326. https://doi.org/10.1016/j.neuroimage.2018.08.012 (2018).
Cho, K. H. et al. Intrinsic thalamic network in temporal lobe epilepsy with hippocampal sclerosis according to surgical outcomes. Front. Neurol. 12, 721610. https://doi.org/10.3389/fneur.2021.721610 (2021).
Park, J. et al. An investigation of thalamic nuclei volumes and the intrinsic thalamic structural network based on motor subtype in drug naive patients with Parkinson’s disease. Parkinsonism Relat. Disord. 81, 165–172. https://doi.org/10.1016/j.parkreldis.2020.10.044 (2020).
Shin, K. J., Lee, H. J. & Park, K. M. Alterations of individual thalamic nuclei volumes in patients with migraine. J. Headache Pain 20, 112. https://doi.org/10.1186/s10194-019-1063-3 (2019).
Steriade, M. & Llinas, R. R. The functional states of the thalamus and the associated neuronal interplay. Physiol. Rev. 68, 649–742. https://doi.org/10.1152/physrev.1988.68.3.649 (1988).
Sherman, S. M. The thalamus is more than just a relay. Curr. Opin. Neurobiol. 17, 417–422. https://doi.org/10.1016/j.conb.2007.07.003 (2007).
Ku, J. et al. Default mode network disturbances in restless legs syndrome/Willis-Ekbom disease. Sleep Med. 23, 6–11. https://doi.org/10.1016/j.sleep.2016.05.007 (2016).
Ku, J. et al. Diurnal variation of default mode network in patients with restless legs syndrome. Sleep Med. 41, 1–8. https://doi.org/10.1016/j.sleep.2017.09.031 (2018).
Vartiainen, N. et al. Thalamic pain: Anatomical and physiological indices of prediction. Brain J. Neurol. 139, 708–722. https://doi.org/10.1093/brain/awv389 (2016).
Bornschlegl, M. & Asanuma, H. Importance of the projection from the sensory to the motor cortex for recovery of motor function following partial thalamic lesion in the monkey. Brain Res. 437, 121–130. https://doi.org/10.1016/0006-8993(87)91533-2 (1987).
Kuramoto, E. et al. Ventral medial nucleus neurons send thalamocortical afferents more widely and more preferentially to layer 1 than neurons of the ventral anterior-ventral lateral nuclear complex in the rat. Cereb. Cortex 25, 221–235. https://doi.org/10.1093/cercor/bht216 (2015).
Ku, J. et al. Functional connectivity alternation of the thalamus in restless legs syndrome patients during the asymptomatic period: A resting-state connectivity study using functional magnetic resonance imaging. Sleep Med. 15, 289–294. https://doi.org/10.1016/j.sleep.2013.09.030 (2014).
Lee, Y. S. et al. Resting-state connectivity and the effects of treatment in restless legs syndrome. Sleep Med. 67, 33–38. https://doi.org/10.1016/j.sleep.2019.10.014 (2020).
Newman, M. E. Mixing patterns in networks. Phys. Rev. E Stat. Nonlinear Soft Matter Phys. 67, 026126. https://doi.org/10.1103/PhysRevE.67.026126 (2003).
Newman, M. E. Assortative mixing in networks. Phys. Rev. Lett. 89, 208701. https://doi.org/10.1103/PhysRevLett.89.208701 (2002).
Eguiluz, V. M., Chialvo, D. R., Cecchi, G. A., Baliki, M. & Apkarian, A. V. Scale-free brain functional networks. Phys. Rev. Lett. 94, 018102. https://doi.org/10.1103/PhysRevLett.94.018102 (2005).
Albert, R., Jeong, H. & Barabasi, A. L. Error and attack tolerance of complex networks. Nature 406, 378–382. https://doi.org/10.1038/35019019 (2000).
Walters, A. S. et al. Validation of the International Restless Legs Syndrome Study Group rating scale for restless legs syndrome. Sleep Med. 4, 121–132. https://doi.org/10.1016/s1389-9457(02)00258-7 (2003).
Yang, J.-G. et al. The reliability and validity of the Korean versions of the international restless legs scale and the restless legs syndrome quality of life questionnaire. J. Korean Neurol. Assoc. 263–269 (2010).
Abetz, L. et al. Evaluating the quality of life of patients with restless legs syndrome. Clin. Ther. 26, 925–935. https://doi.org/10.1016/s0149-2918(04)90136-1 (2004).
Cho, Y. W., Song, M. L. & Morin, C. M. Validation of a Korean version of the insomnia severity index. J. Clin. Neurol. 10, 210–215. https://doi.org/10.3988/jcn.2014.10.3.210 (2014).
Sohn, S. I., Kim, D. H., Lee, M. Y. & Cho, Y. W. The reliability and validity of the Korean version of the Pittsburgh Sleep Quality Index. Sleep Breath 16, 803–812. https://doi.org/10.1007/s11325-011-0579-9 (2012).
Zigmond, A. S. & Snaith, R. P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 67, 361–370. https://doi.org/10.1111/j.1600-0447.1983.tb09716.x (1983).
Mijalkov, M. et al. BRAPH: A graph theory software for the analysis of brain connectivity. PLoS ONE 12, e0178798. https://doi.org/10.1371/journal.pone.0178798 (2017).
Farahani, F. V., Karwowski, W. & Lighthall, N. R. Application of graph theory for identifying connectivity patterns in human brain networks: A systematic review. Front. Neurosci. 13, 585. https://doi.org/10.3389/fnins.2019.00585 (2019).
Thomas, J., Seo, D. & Sael, L. Review on graph clustering and subgraph similarity based analysis of neurological disorders. Int. J. Mol. Sci. https://doi.org/10.3390/ijms17060862 (2016).
Green, G. H. & Diggle, P. J. On the operational characteristics of the Benjamini and Hochberg False Discovery Rate procedure. Stat. Appl. Genet. Mol. Biol. 6, Article 27, https://doi.org/10.2202/1544-6115.1302 (2007).
Acknowledgements
This work was supported by the Ministry of Science and ICT of the Republic of Korea (NRF-2021R1F1A1049605).
Author information
Authors and Affiliations
Contributions
K.M.P. and K.T.K., these two authors equally contributed to paper writing and data analysis as the first author. K.T.K. and Y.W.C. participated in recruiting patients and controls and organizing data. Y.W.C. supervised the paper writing. K.M.P. and D.A.L. wrote the manuscript. All the authors participated in the analysis and interpretation of data. All the authors revised the manuscript critically and approved the manuscript in its final form.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Park, K.M., Kim, K.T., Lee, D.A. et al. Alterations of the thalamic nuclei volumes and intrinsic thalamic network in patients with restless legs syndrome. Sci Rep 13, 4415 (2023). https://doi.org/10.1038/s41598-023-31606-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-31606-8
- Springer Nature Limited
This article is cited by
-
Regional structural abnormalities in thalamus in idiopathic cervical dystonia
BMC Neurology (2024)
-
Difference in functional connectivity between end-stage renal disease patients with and without restless legs syndrome: A prospective study
Sleep and Breathing (2024)
-
Multilayer network analysis in patients with juvenile myoclonic epilepsy
Neuroradiology (2024)