Abstract
There is a lack of research focused on understanding the different characteristics and healthcare utilization of metastatic breast cancer patients by palliative care use. This study aims to investigate trend of in-patient palliative care and its association with healthcare utilization among hospitalized metastatic breast cancer patients in the US. National Inpatient Sample (NIS) was used to identify nationwide metastatic breast cancer patients (n = 5209, weighted n = 25,961) from 2010 to 2014. We examined the characteristics of the study sample by palliative care and its association with healthcare utilization, measured by discounted hospital charges and length of stay. Multivariable survey regression models were used to identify predictors. Among 26,961 breast cancer patients, 19.0% had palliative care. Percentage of receiving palliative care during the period were gradually increased. Social factors including race, insurance types were also associated with a receipt of palliative care. Survey linear regression results showed that patients with palliative care were associated with 31% lower hospital charges, however, length of stays were not significantly associated. This study found evidence of who was associated with the receipt of palliative care and its relationship with healthcare utilization. This study also emphasizes the importance of receiving palliative care in patients with breast cancer, paving the way for future research into ways to improve palliative care in cancer patients. This study also found social differences and gave evidence of programs that could be used to help vulnerable groups in future health policy decisions.
Similar content being viewed by others
Introduction
Breast cancer is the most common cancer among women in the United States. Approximately 13% of women in the U.S. are diagnosed with breast cancer in their lifetime, and it is the cause of death for 3% of American women annually1. In 2019, an estimated 286,600 new breast cancer cases and 47,760 deaths were reported1,2. Furthermore, the incidence rate for invasive breast cancer has been steadily increasing over the last 15 years1. The majority of breast-cancer related deaths are a result of complications from recurrent or metastatic diseases3. Metastatic breast cancer is defined as breast cancer that has spread to another part of the body, such as the liver, brain, bones, or lungs4. With respect to new breast cancer cases, approximately 6% are metastatic when initially diagnosed3. Even when cases are diagnosed in early stages, 30% of these early-stage breast cancer cases will still become metastatic3.
Despite significant improvements in treatment, the 5-year relative survival rate for metastatic breast cancer is only 27%, with a median relative survival time of 25 months; significantly less than the 5-year relative survival rate for localized breast cancer of 99%1,5,6. The progression of metastatic breast cancer and its different cytotoxic treatments can cause patients to experience increased fatigue, stress, depression, anxiety, and social isolation. These manifestations significantly impact the patient’s psychological well-being and quality of life7,8. Metastatic breast cancer remains essentially incurable, and current therapy goals include: the palliation of symptoms, delaying disease progression, improving/maintaining quality of life, and prolonging overall survival9. According to a recent guideline by the American Society of Clinical Oncology (ASCO), it is recommended for patients with advanced cancer to receive interdisciplinary palliative care services with concurrent active treatment10.
Palliative care is an interprofessional discipline that utilizes a patient-centered approach to address the supportive care needs of patients with advanced cancer, and their families11. The clinical importance of palliative care for patients with metastatic breast cancer has been demonstrated in several previous studies that have shown that palliative care facilitates a higher quality of life, less aggressive end of life, lowers depression rate, and maintains or improves survival for patients with metastatic breast cancer12,13. Other studies have also demonstrated that integration of palliative care improves patient understanding of the disease, and promotes dialogue that encourages patient involvement in the treatment planning14. The European society of Medical Oncology's guidelines strongly recommend introduction of specialty palliative care in metastatic breast cancer, as adequate control of symptoms such as pain should be prioritized13. Other clinical benefits are well documented and it is suggested that healthcare professionals recognize their role in the patient's care, as well as end of life integration of palliative care into patient's treatment plans15,16.
Previous studies suggested that palliative care was associated with lower costs, and economic benefits of palliative care for metastatic cancer patients were very clear17,18,19,20,21 where more end-of life cancer patients are seeking various aggressive treatments17,18,22. Administering unnecessary end-of-life care can hinder discussions about proper symptom relief and palliative care. Furthermore, as new anti-cancer treatments are continuously being developed, it is common for palliative care to become delayed for metastatic breast cancer patients until they are very close to end-of-life15. In the era of rapid growing cancer patient, understanding of various characteristics for palliative care utilization is very critical23, however, evidence of economic benefit regarding with metastatic breast cancer patients have not been reviewed well. There is a lack of previous studies focusing on the aspects of palliative care using a representative population sample24,25 and its association with healthcare utilization measured by hospital charges and length of stays (LOS) among metastatic breast cancer patients, it is very crucial to investigate the issue.
Despite numerous studies demonstrating the benefits of palliative care for metastatic breast cancer patients, little is known regarding the pattern of palliative care utilization among metastatic breast cancer patients in the United States. The primary objective of this study is to examine the recent trends of palliative care utilization to identify the various factors associated with the use of palliative care among hospitalized women with metastatic breast cancer. This study will also assess how palliative care was associated with hospital length of stay and hospital charges among women hospitalized with metastatic breast cancer. This study will finally look at these factors and compare them to findings in previous studies on palliative care in other cancers and conditions.
Materials and method
Data collection
The 2010–2014 National Inpatient Sample (NIS) database was used to obtain a population based estimate for women with metastatic breast cancer. NIS data is obtained by Agency for Healthcare Research and Quality (AHRQ)’s Healthcare Cost and Utilization Project (HCUP) and it is not only one of the largest publicly available healthcare dataset but also contains all payer US hospital inpatients records. Among all 2010–2014 NIS sample (N = 37,312,324), as shown in Fig. 1, we first identified primary diagnosis of breast cancer (total n = 76,140) using the International Classification of Diseases, Ninth revision, Clinical Modification (ICD-9-CM) codes for breast cancer. Metastatic stage was determined as the ICD-9 code indicated metastatic disease to other organs (196.0–196.2, 196.5–196.9, 197.0–197.8, 198.80–198.89 and 199.00–199.18). After cleaning the missing other variables, we finally obtained women patients with diagnosis of metastatic stage (N = 5209).
Variables
The main objective of this study was to investigate the characteristics of palliative care utilization and its association with in-hospital death, length of stay, and hospital charges. The main interesting variable was a receipt of palliative care and we used the ICD-9-CM code of V66.7 in order to identify palliative care for hospitalized patients. The V66.7 code is defined as an encounter for palliative care when hospitalized patients received palliative care consultation. Further, it is used in situations of “palliative care,” “end-of-life care,” “hospice care,” or “terminal care”26. Total hospital charges were calculated after adjusting for the annual inflation rate using Centers for Medicare and Medicaid Services estimates27. Due to the skewing of distribution for hospital charges and length of stay, we calculated the natural log of those variables. In this study, we adjusted patient-level and hospital-level confounders. Patient level characteristics included: age, race, annual median household income based on ZIP code, primary payer (Medicare, Medicaid, Self-Pay/No Charge, Other, Private insurance), number of comorbidities, severity of illness using all-patient refined diagnosis-related group (APRDRG), and whether patients received surgery, radiation, or chemotherapy. Hospital attributes included information concerning teaching status, location, and bed-size. We defined our variables based on previous literatures using NIS samples23,28,29.
Statistical analysis
To represent the entire population of patients with metastatic stage breast cancer, sampling weights were used for all statistical analyses. We used a sampling weights approach that was employed in previous research28. We first examined the characteristics of the final dataset which included patient and hospital characteristics by palliative care use. The patient and hospital characteristics were presented as weighted frequency (percentage) or means (SD). To investigate group differences (whether receiving palliative care), Rao-Scott Chi-Square tests were used for categorical variables.
Using the survey logistic regression analysis, the odds ratios and 95% confidence interval (ORs and 95% CI) for receiving palliative care for metastatic breast cancer patients were calculated (Table 2). Via multivariable survey linear regression analysis, the effect of palliative care on both lengths of stay and hospital charges was also examined (Table 3). All analyses were conducted by using SAS statistical software (version 9.4; SAS Institute Inc., Cary, NC, USA). The statistical tests utilized in this study were all two-sided and statistical significance was calculated at p value < 0.05.
This study adhered to the Declaration of Helsinki, and the data we used in this study was secondary data in which all patient data were encrypted and unable to identify. This study was approved for waiver from the Institutional Review Board of Soonchunhyang University (202109-SB-083).
Results
Patient characteristics
A total 5209 hospital discharges of women with metastatic breast cancer were identified in the 2010–2014 NIS data (weighted n = 25,961) (Fig. 1). Among them, 991 (weighted n = 4934, 19.0%) had palliative care. The general characteristics of patient and hospital characteristics are presented in Table 1. Among metastatic breast cancer patients who died during hospitalization, over half of them received palliative care (55.4%). Among those who did not die, 12.7% received palliative care. The mean LOS and hospital charges were 6.46 days (SD = 7.44 days) and $37,807 (SD = $80,564) for those who received palliative care and 5.74 days (SD = 6.71 days) 43,906 (SD = 53,775) for those who did not receive palliative care.
Patterns of palliative care use
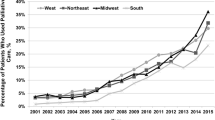
Figure 2 shows the trends in palliative care use among hospitalized patients with metastatic breast cancer between 2010 and 2014. The rate at which palliative care were increased from 14.3 to 21.9% during the study period (CAGR—Compound Annual Growth Rate = 11.13%, p < 0.001).
The ORs of receiving palliative care from multiple regression model is shown in Table 2. Metastatic breast cancer patients who died during their hospitalization were more likely to receive palliative care compared to those who did not die after controlling for all other variables (OR: 6.59, 95% CI: 5.50–7.90). Black patients were associated with fewer odds of using palliative care compared with White; patients with Medicare were less likely to use palliative care, while patients with other types of insurance were associated with higher odds of using palliative care. Additionally, palliative care was significantly less likely used in patients receiving surgery (OR: 0.07, 95% CI: 0.04–0.12) or chemotherapy (OR: 0.69, 95% CI: 0.50–0.94) during the same admission. The use of palliative care was significantly higher in urban teaching hospitals compared to rural hospitals (OR: 1.38, 95% CI: 1.09–1.74).
Association of palliative care with hospital charges and LOS
The association of hospital palliative care with hospital charges and LOS is shown in Table 3. Receiving palliative care while in the hospital was significantly associated with lower hospital charges (β = − 0.31, p < 0.001).The results also revealed that younger age groups, minority populations, and lower income groups were associated with statistically significant higher hospital charges.
Discussion
This study a retrospective cohort study by selecting metastatic stage breast cancer patients who were hospitalized between 2010 and 2014. Metastatic breast cancer patients that received palliative care increased by 7.6% from 2010 to 2014. The increased utilization of palliative care from year-to-year among metastatic breast cancer patients was consistent with previous American studies on the utilization of palliative care in patients with other medical issues such as chronic obstructive pulmonary disease (COPD)29, multiple sclerosis30, and a study inclusive of all cancers11. Among metastatic breast cancer patients discharged from American hospitals, 19.0% received palliative care, an increase from 14.3% in 2010 to 21.9% in 2014. In comparison to previous studies from 2005 to 2014 that demonstrated 30.0% of patients with COPD received palliative care29. The percentage of patients with multiple sclerosis who received palliative care increased from 0.2% in 2005 to 6.1% in 201430. Among all cancer patients, 9.9% received palliative care, and those specifically with advanced stage cancers experienced an increase in palliative care from 3.0% in 2005 to 15.5% in 201411. Rubens et al. found that 4.3% of all breast cancer patients received palliative care; however, their data did not make a distinction between the subjects’ stages of cancer11. Though palliative care uptake percentage increased in this study as years progressed, majority of the patients with metastatic breast cancer did not receive palliative care. According to the third edition of the Clinical Practice Guidelines for Quality Palliative Care (NCP guidelines) drafted by the National Consensus Project for Quality Palliative Care in 2013, seriously or terminally ill patients with cancer who are not likely to recover should be considered for palliative care. Palliative care should be delivered by an able interdisciplinary team who can focus on different aspects of a patient’s quality of life and provide care in conjunction with the patient’s and their family’s preferences, beliefs and preferences. Provision of physical comfort, pain and symptom management, psychological assessment, patient education, grief and bereavement services, inclusive healing environment, culturally and linguistically competent care, and coping tools, understanding patient’s social structure and spiritual needs, promoting a peaceful and dignified death and having access to legal and ethical palliative care-based expertise together form the cornerstone of a multi-dimensional palliative care intervention31. The NCP guidelines stress the importance of ensuring that in the future, all women with metastatic breast cancer get access to palliative care. Palliative care utilization among metastatic breast cancer patients was significantly higher in urban teaching hospitals, compared to rural hospitals. This is in concurrence with previous studies that have shown that the general practice of palliative care is utilized more often in urban hospitals and teaching hospitals32,33.
Type of hospital and geographical location are important factors related to the availability of palliative care. A study examining availability of palliative care in U.S. hospitals found that non-profit hospitals were more likely to have palliative care compared to for-profit hospitals and same holds true for metropolitan areas compared to rural areas34. Our study results also showed that a very small number of hospitalized patients undergoing surgery and chemotherapy were less likely to receive palliative care. Patients with metastatic breast cancer have four patterns of clinical progression: smoldering, gradual, rapid and de novo poor condition. Each pattern of progression has an acute and a stable phase. Provision of and the need for palliative care are determined based on the progression status and the phase experienced by the patient35. Our study findings highlight a gap in cancer care management and stress the importance of starting palliative care therapy early on, right after metastatic cancer diagnosis, given its beneficial nature as shown by previous research14.
Among metastatic breast cancer patients, we identified disparities regarding the receipt of palliative care. Patients with Medicare and black patients were less likely to use palliative care than white patients. Previous studies reveal that lack of awareness, lack of knowledge, fear that may hasten death, and doubt that might cause providers to deliver inadequate care might be associated with lower care for black patients36,37. Further, the study suggested the expansion of palliative care programs because this service is underutilized among Medicare beneficiaries38. This study also showed that receiving palliative care was associated with lower in-hospital mortality (OR = 6.59), which is consistent with previous studies on different cancers and conditions11,30, where palliative care is more likely recommended to patients who are terminally ill or as a last resort11. Palliative care has proven to be beneficial for patients with earlier-stage cancers or in combination with traditional treatment11,29,30. Many studies regarding this topic show that palliative care is commonly reserved for the elderly. This perpetuates the underutilization of palliative care in patients that can significantly benefit from it. Not having better opportunities to utilize palliative care can subsequently have a negative impact on their health-related quality of life (HRQoL)39.
Hospital charges were significantly lowered by $6,099 for metastatic breast cancer patients receiving palliative care, compared to those who were not. The lower hospital charges are consistent with previous studies, which have shown a decrease of $2,261 in MS patients receiving palliative care30. COPD patients receiving palliative care experienced a 28.7% decrease in hospital charges, compared to those who did not. Palliative care that is introduced sooner and used in conjunction with treatment has been shown to improve health outcomes and lower hospital charges when compared to palliative care that is introduced later29. A study on the use of palliative care in children found that using palliative care was associated with significantly lower overall and daily hospital costs40. Mulvey et al. discovered similar results, concluding that patients with head and neck cancer who received palliative care had significantly lower hospital-related charges, but there was no effect on length of stay39. In this study, we don’t see statistical significance for length of stay (LOS), which contradicts other studies, such as that of Cheng et al., where it was found that in hospitalized children with cancer, use of palliative care was associated with a shorter length of stay39. The study results are mixed depending on the diseases; further study should be conducted to determine how palliative care is associated with LOS.
This study’s findings show the importance of early integration of palliative care and its impact on length of stay, hospital charges. Although there are mixed conclusions surrounding the impact of palliative care on length of stay, it can be inferred that current literature supports the conclusion that palliative care is associated with decreased hospital charges. A small number of studies have focused on palliative care in patients with metastatic breast cancer. This study centers on palliative care utilization in metastatic breast cancer patients and may therefore prove useful in providing insight on the consequences of both late integration, or choosing not to integrate this health-care service. Clinicians providing care to cancer patients and extremely ill patients should evaluate the benefits of palliative care utilization in accordance with patient needs, expectations, and treatment goals41. Additional research needs to be conducted on this topic, as its findings have the potential to promote better health outcomes and better experiences for cancer patients.
Limitations
There are some limitations in our study. A universal ICD-9 V66.7 code is used to identify palliative care services. Hua et al. show that the usage of this code to identify patients that have received palliative care had poor sensitivity and high specificity26. Although in patients with metastatic cancer, sensitivity was considerably high (66.3%). Conversely, in patients that died in the hospital, the sensitivity was lower (53.9%). Age should also be considered when using ICD code V66.7, as sensitivity was improved with age restrictions26. Validity of the ICD-9 code V66.7 has been shown in other subgroups such as in hospitalized patients with heart failure, but one should evaluate patient characteristics to determine the validity of ICD-9 code in a specific patient population42. Also, ICD-9 code V66.7 does not include specific service information such as an expert palliative care team approach or primary physicians prescribing opioids, etc. More research should be done using detailed palliative care information. In this study, we controlled variables for patient and hospital characteristics based on previous literatures. However, confounding factors still exist even though we controlled for patient and hospital characteristics, and it may or may not differentiate the results of this study. Furthermore, our study findings suggest that palliative care patients stayed longer, however, some women with metastatic disease were unpredictable for their survival. Last, due to the nature of NIS data variables, we won’t be able to include very important variables such as chemo given prior to death, ICU admissions, reason for hospitalization etc. for an analysis. Despite these potential limitations due to using an administrative dataset, this study is meaningful to examine nationwide hospital palliative care and its associations with healthcare utilization for breast cancer patients, for which very limited number of studies have been conducted so far. It might provide some insights and will be useful for health policy development, epidemiology research, and/or clinical settings as well.
Conclusion
This study found evidence that the use of palliative care was significantly associated with decreased hospital charges. This study highlights the impact of receiving palliative care in the breast cancer patients and leads to further studies that identify ways to improve end-of-life care in this patient population. Also, this study found social disparities including race, insurance type, etc. and provide evidence of targeted programs, future health policy consideration for those vulnerable populations.
Data availability
All data generated or analysed during this study are included in this published article.
References
American Cancer Society. Breast Cancer Facts & Figures 2019–2020. Atlanta: American Cancer Society, Inc. (2019). https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/breast-cancer-facts-and-figures-2019-2020.pdf
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2019. CA Cancer J Clin. 69(1), 7–34 (2019).
O’Shaughnessy, J. Extending survival with chemotherapy in metastatic breast cancer. Oncologist 10(Suppl 3), 20–29 (2005).
Breastcancer.org. Metastatic Breast Cancer (2022). https://www.breastcancer.org/symptoms/types/recur_metast
Cancer.org. Survival Rates for Breast Cancer (2022). https://www.cancer.org/cancer/breast-cancer/understanding-a-breast-cancer-diagnosis/breast-cancer-survival-rates.html
Mariotto, A. B., Etzioni, R., Hurlbert, M., Penberthy, L. & Mayer, M. Estimation of the number of women living with metastatic breast cancer in the United States. Cancer Epidemiol. Biomarkers Prev. 26(6), 809–815 (2017).
Cherny, N. I., Paluch-Shimon, S. & Berner-Wygoda, Y. Palliative care: Needs of advanced breast cancer patients. Breast Cancer 3(10), 231–243 (2018).
Central European Cooperative Oncology Group (CECOG) et al. Third consensus on medical treatment of metastatic breast cancer. Ann. Oncol. 20(11), 1771–1785 (2009).
Reiser, V., Rosenzweig, M., Welsh, A., Ren, D. & Usher, B. The support, education, and advocacy (SEA) program of care for women with metastatic breast cancer: A nurse-led palliative care demonstration program. Am. J. Hosp. Palliat. Care. 36(10), 864–870 (2019).
Ferrell, B. R. et al. Integration of palliative care into standard oncology care: American society of clinical oncology clinical practice guideline update. J. Clin. Oncol. 35(1), 96–112 (2017).
Rubens, M. et al. Palliative care consultation trends among hospitalized patients with advanced cancer in the United States, 2005 to 2014. Am. J. Hosp. Palliat Care 36(4), 294–301 (2019).
Rugno, F. C., Paiva, B. S. & Paiva, C. E. Early integration of palliative care facilitates the discontinuation of anticancer treatment in women with advanced breast or gynecologic cancers. Gynecol. Oncol. 135(2), 249–254 (2014).
Rabow, M. et al. The value of embedding: Integrated palliative care for patients with metastatic breast cancer. Breast Cancer Res. Treat. 167(3), 703–708 (2018).
Kain, D. A. & Eisenhauer, E. A. Early integration of palliative care into standard oncology care: Evidence and overcoming barriers to implementation. Curr. Oncol. 23(6), 374–377 (2016).
Leadbeater, M. The role of a community palliative care specialist nurse team in caring for people with metastatic breast cancer. Int. J. Palliat. Nurs. 19(2), 93–97 (2013).
Greer, J. A. et al. Randomized trial of a palliative care intervention to improve end-of-life care discussions in patients with metastatic breast cancer. J. Natl. Compr. Cancer Netw. 20(2), 136–143 (2022).
Huo, J. et al. Utilization pattern and service settings of palliative care for patients with metastatic non-small cell lung cancer. Cancer 125(24), 4481–4489 (2019).
Yadav, S. et al. The health care cost of palliative care for cancer patients: A systematic review. Support Care Cancer 28(10), 4561–4573 (2020).
Taylor, D. H. Jr. The effect of hospice on Medicare and informal care costs: The U.S. experience. Pain Symptom Manag. 38(1), 110–114 (2009).
Higginson, I. J. et al. Do hospital-based palliative teams improve care for patients or families at the end of life?. J. Pain Symptom Manag. 23(2), 96–106 (2002).
Zhang, B. et al. Health care costs in the last week of life: Associations with end-of-life conversations. Arch. Intern Med. 169(5), 480–488 (2009).
Earle, C. C. et al. Aggressiveness of cancer care near the end of life: Is it a quality-of-care issue?. J. Clin. Oncol. 26(23), 3860–3866 (2008).
Chang, J., Han, K. T., Medina, M. & Kim, S. J. Palliative care and healthcare utilization among deceased metastatic lung cancer patients in U.S. hospitals. BMC Palliat. Care 21(1), 136 (2022).
Morrison, R. S., Maroney-Galin, C., Kralovec, P. D. & Meier, D. E. The growth of palliative care programs in United States hospitals. J. Palliat. Med. 8(6), 1127–1134 (2005).
Dumanovsky, T. et al. The growth of palliative care in USS hospitals: A status report. J. Palliat. Med. 19(1), 8–15 (2016).
Hua, M., Li, G., Clancy, C., Morrison, R. S. & Wunsch, H. Validation of the V66.7 code for palliative care consultation in a single academic medical center. J. Palliat. Med. 20(4), 372–377 (2017).
SAMHSA Spending Estimates Team et al. Trends in spending for substance abuse treatment, 1986–2003. Health Aff. 26(4), 1118–1128 (2007).
Hwang, J. et al. Ten-year trends of utilization of palliative care services and life-sustaining treatments and hospital costs associated with patients with terminally ill lung cancer in the United States from 2005 to 2014. Am. J. Hosp. Palliat. Care 36(12), 1105–1113 (2019).
Kim, S. J. et al. Life-sustaining procedures, palliative care, and cost trends in dying COPD patients in U.S. hospitals: 2005–2014. J. Hosp. Palliat. Care 21, 23–32 (2018).
Lee, Y. J. et al. Ten-year trends of palliative care utilization associated with multiple sclerosis patients in the United States from 2005 to 2014. J. Clin. Neurosci. 58, 13–19 (2018).
National Consensus Project for Quality Palliative Care. Clinical Practice Guidelines for Quality Palliative Care, 3rd edn. Pittsburgh, PA: National Consensus Project for Quality Palliative Care Task Force (2013). https://www.nationalcoalitionhpc.org/wp-content/uploads/2017/04/NCP_Clinical_Practice_Guidelines_3rd_Edition.pdf
Chen, Y. et al. Prevalence, trend and disparities of palliative care utilization among hospitalized metastatic breast cancer patients who received critical care therapies. Breast 54, 264–271 (2020).
Mazzone, E. et al. Temporal trends and social barriers for inpatient palliative care delivery in metastatic prostate cancer patients receiving critical care therapies. Prostate Cancer Prostatic Dis. 23(2), 260–268 (2020).
Rogers, M., Meier, D. E., Morrison, R. S., Moreno, J. & Aldridge, M. Hospital characteristics associated with palliative care program prevalence. J. Palliat. Med. 23(10), 1296–1299 (2020).
Kida, K., Olver, I., Yennu, S., Tripathy, D. & Ueno, N. T. Optimal supportive care for patients with metastatic breast cancer according to their disease progression phase. JCO Oncol. Pract. 17(4), 177–183 (2021).
Bazargan, M., Cobb, S., Assari, S. & Kibe, L. W. Awareness of palliative care, hospice care, and advance directives in a racially and ethnically diverse sample of California adults. Am. J. Hosp. Palliat. Care 38(6), 601–609 (2021).
Rhodes, R. L. et al. The desires of their hearts: The multidisciplinary perspectives of African Americans on end-of-life care in the African American community. Am. J. Hosp. Palliat. Care 34(6), 510–517 (2017).
Taylor, D. H. Jr. et al. Paying for palliative care in medicare: Evidence from the four seasons/duke CMMI demonstration. J. Pain Symptom Manag. 58(4), 654–661 (2019).
Mulvey, C. L., Smith, T. J. & Gourin, C. G. Use of inpatient palliative care services in patients with metastatic incurable head and neck cancer. Head Neck 38(3), 355–363 (2016).
Cheng, B. T. & Wangmo, T. Palliative care utilization in hospitalized children with cancer. Pediatr. Blood Cancer 67(1), e28013 (2020).
Tometich, D. B. et al. Metastatic breast cancer patients’ expectations and priorities for symptom improvement. Support Care Cancer 26(11), 3781–3788 (2018).
Feder, S. L. et al. Validation of the ICD-9 diagnostic code for palliative care in patients hospitalized with heart failure within the veterans health administration. Am. J. Hosp. Palliat. Care 35(7), 959–965 (2018).
Acknowledgements
James Mills read and reviewed the manuscript.
Funding
This work was supported by the Soonchunhyang University Research Fund, BK21 FOUR (Fostering Outstanding Universities for Research, No.: 5199990914048, Korean Ministry of Education), and partially supported from the seed grant at Texas A&M university, Irma Lerma Rangel School of Pharmacy.
Author information
Authors and Affiliations
Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, S.J., Patel, I., Park, C. et al. Palliative care and healthcare utilization among metastatic breast cancer patients in U.S. Hospitals. Sci Rep 13, 4358 (2023). https://doi.org/10.1038/s41598-023-31404-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-31404-2
- Springer Nature Limited