Abstract
The differential effect of meteorological factors and air pollutants on pediatric epistaxis in younger and older children has not been evaluated. We evaluated the distribution of pediatric epistaxis cases between younger (0–5 years) and older children (6–18 years). Subsequently, we assessed and compared the effects of meteorological variables and the concentration of particulate matter measuring ≤ 10 μm in diameter (PM10) on hospital epistaxis presentation in younger and older children. This retrospective study included pediatric patients (n = 326) who presented with spontaneous epistaxis between January 2015 and August 2019. Meteorological conditions and PM10 concentration were the exposure variables, and data were obtained from Korea Meteorological Administration 75. The presence and cumulative number of epistaxis presentations per day were considered outcome variables. Air temperature, wind speed, sunshine duration, and PM10 concentration in younger children, and sunshine duration and air pressure in older children, significantly correlated with the presence of and cumulative number of epistaxis presentations per day. The PM10 concentration was not a significant factor in older children. Thus, meteorological factors and PM10 concentration may differentially affect epistaxis in younger (0–5-year-olds) and older (6–18-year-olds) children. Risk factors for pediatric epistaxis should be considered according to age.
Similar content being viewed by others
Introduction
Particulate matter (PM) is a complex mixture of organic and inorganic compounds found in the atmosphere, in the gas, liquid, and solid phases1. Owing to the genotoxic, mutagenic, and carcinogenic effects of PM, exposure to PM is a risk factor for various diseases such as cardiovascular disease, stroke, and airway diseases2. The size of PM determines the target organ that it penetrates. PM10 (≤ 10 μm, coarse particles) is known to settle in the upper airway tract and trigger allergenic and irritating responses. In South Korea, the PM10 concentration is higher than that in North America, Western Europe, and Japan, and reports of a spontaneous increase in PM10 concentration are of major concern3.
Epistaxis is a common symptom in children, and it is reported that up to 60% of children will have had at least one epistaxis event by 10 years of age4. Various conditions associated with pediatric epistaxis have been evaluated. In terms of individual patient factors, age and allergic rhinitis have been shown to be significantly associated with hospital epistaxis presentation in children5. Regarding environmental conditions, several meteorological factors have been suggested to be important in pediatric epistaxis. For example, temperature and air visibility have been reported as vital climate variables in pediatric epistaxis6. Humidity has likewise been linked to pediatric epistaxis7. In addition to meteorological factors, air pollutants such as PM10 have also been recently shown to be associated with the incidence of epistaxis in children4,8.
The daily lives of preschool children (0–5 years of age) differ from that of school-aged children (6–18 years) in this country. The life of younger children might be more dependent on the daily weather. Younger children might spend a considerable amount of time outdoors during days with fair weather but might spend more time indoors during days with bad weather. Furthermore, the daily life of school-aged children tends to be more constant, with them spending a considerable amount of time indoors regardless of the weather.
Objectives
We hypothesized that epistaxis, which is closely associated with meteorological factors and PM10, would show dissimilar patterns between younger and older children. This study aimed to evaluate the distribution of pediatric epistaxis cases among younger children aged 0–5 years and older children aged 6–18 years.
Methods
Study design
In this retrospective, single-center study, medical records of pediatric patients (age ≤ 18 years) who presented with spontaneous epistaxis at Chung-Ang University Hospital between January 2015 and August 2019 were reviewed. Patients who presented with secondary epistaxis due to bleeding disorders or a foreign body lodged in the nose were excluded from this study.
Exposure variables
Meteorological conditions and PM10 concentration were the exposure variables, and the data were obtained from Korea Meteorological Administration 75 (https://web.kma.go.kr/eng/index.jsp). Data on air pressure (hPa), wind speed (m/s), air temperature (°C), relative humidity (%), sunshine duration (h), amount of solar radiation (MJ/m2), number of clouds (cloud cover) (1/10), and PM10 concentration (μg/m3) are daily reported, and we collected these daily reported data from January 1, 2015, to August 31, 2019, were analyzed8.
Outcome variables
The presence of hospital epistaxis presentation and the cumulative number of epistaxis presentations per day were considered outcome variables.
Statistical analyses
Exposure variables are presented as means with a 95% confidence interval. Univariate and multivariate logistic regression analyses were performed to identify significant explanatory variables associated with hospital epistaxis presentation. Univariate and multivariate Poisson regression analyses were performed to identify significant explanatory variables associated with the cumulative number of hospital epistaxis presentations per day. The correlation was assessed using Pearson’s correlation analysis. A two-tailed p value of < 0.05 was considered to be indicative of statistical significance. Statistical analyses were performed using R version 3.6.2.
Ethics statement
This study was approved by the Institutional Review Board of Chung-Ang University College of Medicine (2002-013-19303), and the requirement for informed consent was waived.
Reporting guideline
This manuscript has been prepared in accordance with the STROBE guidelines for reporting observational studies.
Results
Summary characteristics of exposure and study population data
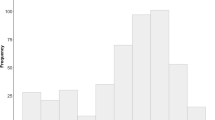
A total of 326 children were enrolled in this study. The mean age was 7.62 ± 4.92 years. The number of children in the 0–5- and 6–18-year age groups was 137 and 189, respectively (Table 1). The number of hospital epistaxis presentations per day showed a decreasing pattern with age, reaching a peak with 33 visitors at the age of 5 years and then gradually decreasing to 9 visitors at the age of 18 years (Fig. 1a). When the number of epistaxis cases was reviewed yearly, we found that the number of annual visits by patients with epistaxis was 81 in 2015, 100 in 2016, 70 in 2017, 38 in 2018, and 37 in 2019 (Fig. 1b). We divided pediatric patients into two groups aged 0–5 and 6–18 years and found a few more patients in the 6–18-year age group during summer; however, the difference was not statistically significant (Fig. 1c).
Supplementary Table S1 compares the monthly averages and 95% confidence intervals of explanatory variables (air temperature, wind speed, air pressure, humidity, sunshine duration, solar radiation amount, number of clouds, and PM10). All variables had seasonal fluctuations.
Factors associated with the presence of daily hospital epistaxis presentation according to age groups
The associations between meteorological factors, including PM10 concentration and daily hospital epistaxis presentation, are presented in Table 2. In the 0–5-year age group, minimum temperature, mean wind speed, sunshine duration, and PM10 concentration were positively associated with the presence of hospital epistaxis presentation per day. In the 6–18-year age group, sunshine duration was positively associated with the presence of hospital epistaxis presentation, whereas the mean air pressure was negatively associated. Additionally, PM10 concentration was not a significant factor in the 6–18-year age group.
Factors associated with the cumulative number of hospital epistaxis presentations per day according to age groups
Next, we evaluated the effects of meteorological factors, including PM10 concentration, on the cumulative number of hospital epistaxis presentations per day (Table 3). In the 0–5-year age group, maximum air temperature, mean wind speed, sunshine duration, and PM10 concentration were positively associated with the daily cumulative number of epistaxis presentations. In the 6–18-year age group, sunshine duration was positively associated with the daily cumulative number of epistaxis presentations, whereas the mean air pressure was negatively associated. However, PM10 concentration was not significantly associated with the daily cumulative number of epistaxis presentations in the 6–18-year age group.
Time-lag effect between hospital epistaxis presentation per day and meteorological factors
Finally, we analyzed the number of hospital epistaxis presentations per day and meteorological factors, including PM10 concentration, as measured during the previous 7 days to evaluate the time-lag effect (Table 4). In the 0–5-year age group, the presence of epistaxis was positively associated with air temperature on the day of the medical visit and during the previous 7 days (p < 0.05). The maximum value of correlation was 0.12 between the 5-day lagged epistaxis presentation and mean temperature. The presence of epistaxis was negatively associated with air pressure. The maximum air pressure was -0.08 for the 7-day lagged epistaxis presentation (p < 0.05) in the 0–5-year age group. In the 6–18-year age group, the presence of epistaxis was positively associated with temperature and solar radiation. The mean air temperature showed the highest correlation at 0.1 for the 1-day lagged epistaxis presentation (p < 0.05). Solar radiation also had the highest correlation of 0.1 with the 0-day lagged epistaxis presentation (p < 0.05). The presence of epistaxis was negatively associated with air pressure, and the maximum amount was −0.11 (Pearson’s correlation coefficient) at the 1-day lagged epistaxis presentation (p < 0.05) in the 6–18-year age group. PM10 concentration did not show any significant time-lag effect in either group.
Discussion
Our study evaluated the differential effects of meteorological factors and PM10 concentration on hospital epistaxis presentation in younger and older children. To the best of our knowledge, this is the first study to compare the differential effects of meteorological factors, including PM10, on epistaxis between younger and older children.
Among the studied meteorological factors, air temperature and wind speed were significant factors for epistaxis in younger children, while air pressure was an important factor for older children. Sunshine duration was positively associated with hospital epistaxis presentation in both groups. Regarding the differential effects of meteorological factors, we believe that as younger children spend more time outdoors than older children who regularly go to school, they would be more severely affected by the daily weather. Therefore, it would be natural to expect that temperature, rain, and wind would be more strongly associated with epistaxis in younger children than older children. However, contrary to our expectations, humidity was not a significant factor for younger or older children in our study. Although the reported effect of humidity on epistaxis was not consistent in previous studies, several studies have indicated humidity to be an important factor in epistaxis6,9,10. Therefore, the role of humidity needs to be further evaluated in future studies based on a larger population.
PM10 is associated with many adverse health effects, such as increased mortality, hospitalization, emergency care, and outpatient rate, owing to the damage to the respiratory system11,12. Children are a susceptible population, and existing studies have found increased adverse effects on children’s respiratory systems13. Although meteorological factors have been considered important in the pathogenesis of epistaxis, PM10 has not been extensively evaluated, especially in children. Several mechanisms may explain why the increase in PM10 concentration is associated with the risk of pediatric epistaxis. Components of PM10 could stimulate the upper airway mucosa, leading to inflammatory responses such as cytokine release14. The nasal mucosa of children persistently exposed to PM10 exhibited basal cell hyperplasia, reduced number of ciliated and goblet cells, and neutrophilic epithelial infiltration, which could result in epistaxis15.
This study was conducted in South Korea, which has a relatively higher concentration of PM10 than other countries, and PM10 concentration is seen as an important social issue. In addition, we enrolled subjects with epistaxis before the emergence of the coronavirus disease to exclude the effect of wearing masks on the results. Our findings suggest that the effects of PM10 on children not wearing masks are different between younger and older children.
When compared with other meteorological factors, PM10 concentration did not show any time-lag effect in younger or older children. Temperature and air pressure showed a time-lag effect during the previous 7 days in the 0–5-year age group. Temperature, solar radiation, and air pressure showed a time-lag effect during the previous 0–1 day in the 6–18-year age group. However, PM10 did not show a significant time-lag effect in either group. A previous study found some correlation between air pollutants and the incidence of pediatric epistaxis; however, it did not show any obvious delayed effect4. No conclusive data have yet been published on the time-lag effect of PM10 concentration, and further study is warranted.
Our study has some limitations. First, the survey was based in a single institute, which is a tertiary referral center, and the generalizability of our findings might be limited. A large population-based multicenter study is needed in the future to confirm our findings. Second, this is a retrospective study, and we could not collect further specific information that might be associated with pediatric epistaxis. The presence of allergic rhinitis or acute respiratory infections and the effects of confounders such as traffic, which may lead patients to go to medical centers other than the hospital, were not evaluated.
In conclusion, the effect of meteorological factors and PM10 concentration on epistaxis was different between younger (0–5 years) and older (6–18 years) children. Our results suggests that environmental factors could differentially affect younger and older children. More attention must be paid to PM10 concentration in younger children, who are more vulnerable to adverse health effects than older children, to reduce cases of hospital epistaxis presentation.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Bray, D., Monnery, P. & Toma, A. G. Airborne environmental pollutant concentration and hospital epistaxis presentation: A 5-year review. Clin. Otolaryngol. Allied Sci. 29, 655–658 (2004).
Arias-Pérez, R. D. et al. Inflammatory effects of particulate matter air pollution. Environ. Sci. Pollut. Res. Int. 27, 42390–42404 (2020).
The World Bank [Internet]. Washington DC, USA: The World Bank; 2016 May 20. PM2.5 air pollution, mean annual exposure (micrograms per cubic meter); 2016 May 20 [cited 2021 Sep 14]; [about 12 pages]. Available from: https://data.worldbank.org/indicator/EN.ATM.PM25.MC.M3
Lu, Y. X., Liang, J. Q., Gu, Q. L., Pang, C. & Huang, C. L. Pediatric epistaxis and its correlation between air pollutants in Beijing from 2014 to 2017. Ear Nose Throat J. 99, 513–517 (2020).
Yang, L., Hur, K., Koempel, J. & Ference, E. H. Epistaxis health disparities in the United States pediatric population. Int. J. Pediatr. Otorhinolaryngol. 114, 20–25 (2018).
Yu, G., Fu, Y., Dong, C., Duan, H. & Li, H. Is the occurrence of pediatric epistaxis related to climatic variables?. Int. J. Pediatr. Otorhinolaryngol. 113, 182–187 (2018).
Akdoğan, M. V. et al. The role of meteorologic factors and air pollution on the frequency of pediatric epistaxis. Ear Nose Throat J. 97, E1–E5 (2018).
Kim, K., Kwak, I. Y. & Min, H. Particulate matter 10 (PM10) is associated with epistaxis in children and adults. Int. J. Environ. Res. Public Health 18, 4809 (2021).
Qureishi, A. & Burton, M. J. Interventions for recurrent idiopathic epistaxis nosebleeds in children. Cochrane Database Syst. Rev. 9, CD004461 (2012).
Purkey, M. R., Seeskin, Z. & Chandra, R. Seasonal variation and predictors of epistaxis. Laryngoscope 124, 2028–2033 (2014).
Zhang, Y. et al. The association of ambient PM2.5 with school absence and symptoms in schoolchildren: A panel study. Pediatr. Res. 84, 28–33 (2018).
Orellano, P., Quaranta, N., Reynoso, J., Balbi, B. & Vasquez, J. Effect of outdoor air pollution on asthma exacerbations in children and adults: Systematic review and multilevel meta-analysis. PLoS ONE 12, e0174050 (2017).
Roy, A. et al. Ambient particulate matter and lung function growth in Chinese children. Epidemiology 23, 464 (2012).
Thompson, J. E. Airborne particulate matter: Human exposure and health effects. J. Occup. Environ. Med. 60, 392–423 (2018).
Calderon-Garciduenas, L. et al. Nasal biopsies of children exposed to air pollutants. Toxicol. Pathol. 29, 558–564 (2001).
Acknowledgements
The authors received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
I.Y.K. performed the statistical analysis and initial drafting of the manuscript. K.S.K. collected the data and reviewed the manuscript. H.J.M. participated in study conceptualization, data collection, initial writing of the manuscript, and final submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kwak, IY., Kim, K.S. & Min, H.J. Differential effect of meteorological factors and particulate matter with ≤ 10-µm diameter on epistaxis in younger and older children. Sci Rep 12, 21029 (2022). https://doi.org/10.1038/s41598-022-25630-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-25630-3
- Springer Nature Limited