Abstract
In cases after pancreas transplantation (PTx), the pancreas graft might be lost for various reasons, including a pancreatoduodenal graft-related complication or patient death with a functioning graft. Although the causes seem to have distinct characteristics, the causes of pancreas graft loss have not been characterized. This study aimed to characterize the causes of pancreas graft loss by analyzing data from a Japanese nationwide registry. This study included 391 patients who received simultaneous pancreas-kidney transplantation among 461 patients with PTx during the study period in approved institutions in Japan. We characterized each cause in terms of the timing of the cause-specific graft loss and preoperative factors associated with graft loss based on nationwide data from a Japanese nationwide registry. Among the 391 cases, 113 lost the pancreas graft due to patient death with a functioning graft (DWFG; n = 34, 44.2%), graft thrombus (n = 22, 28.6%), or chronic rejection (CR; n = 7, 9.1%). Average (± standard deviation) time from PTx to graft loss due to DWFG, graft thrombus, and CR was 3.70 ± 4.36, 0.02 ± 0.01, and 2.37 ± 2.08 years, respectively. Duration of type 1 diabetes mellitus and donor body mass index were significantly associated with pancreas graft loss due to DWFG and graft thrombus, respectively. This characterization showed that the timing and preoperative factors associated with pancreas graft loss were significantly different for different causes of graft loss. These results may inform PTx follow-up protocols to ensure that appropriate care is based on the cause of graft loss.
Similar content being viewed by others
Introduction
Pancreas transplantation (PTx), which was first performed to treat type 1 diabetes mellitus in 1966, is an established therapeutic procedure for patients with diabetes mellitus1,2,3. When successfully performed, PTx can restore endogenous insulin secretion, which results in normal glucose metabolism in patients with diabetes. Due to the therapeutic effects of insulin on glucose metabolism, PTx can reduce diabetes-related complications, such as retinopathy, nephropathy, neuropathy, gastroparesis, and cardiovascular diseases. Furthermore, considering that the complications can lead to impaired quality of life and the occurrence of life-threatening events, the clinical benefit of PTx is evident for patients with diabetes mellitus4,5,6,7,8. However, the outcomes of PTx remain unsatisfactory. For example, in Japan, the 5- and 10-year survival rates for post-transplant pancreas grafts are 76.2% and 67.4%, respectively9,10. These post-transplant survival rates are comparable to outcomes reported in other countries11, and this universal problem of unsatisfactory PTx outcomes is thought to be due to post-transplant pancreas graft loss. Several causes of pancreas graft loss have been reported, including pancreatoduodenal graft-related complications and death with a functioning graft (DWFG). The complications include a graft thrombus, duodenal graft perforation, immunological rejection, and recurrence of type 1 diabetes mellitus. DWFG can be caused by cerebrovascular disease, cardiovascular disease, infection, or malignancy. Thus, pancreas graft loss has a variety of causes9,10. Each cause is likely to exhibit different clinical characteristics, including the frequency of the cause, the timing of the occurrence, and influencing factors. To the best of our knowledge, this is the first study to describe pancreas graft loss by etiology and clinical characteristics. We hope that investigations of the clinical characteristics influencing pancreas allograft failure may enhance our understanding of pancreas graft loss and improve management and outcomes. Thus, the present study aimed to characterize the specific causes of pancreas graft loss after PTx, including predictive preoperative factors for cause-specific pancreas graft loss based on data from a Japanese nationwide registry.
Materials and methods
Patients
This study included 461 recipients of PTx from a deceased donor after brain death (DBD) or a deceased donor after circulatory death (DCD). The 461 procedures were performed between 2000 and 2021 to treat type 1 diabetes mellitus at 19 institutions approved by the Japanese Pancreas and Islet Transplant Association. For the present study, we extracted anonymized clinical data for the 461 cases from the Japan Pancreas Transplant Registry of the Japanese Pancreas and Islet Transplant Association. Among the 461 PTx cases, including 458 from DBD and 3 from DCD, 391 underwent simultaneous pancreas-kidney transplantation (SPK), 51 received a pancreas after kidney transplantation (PAK), and 19 underwent PTx alone (PTA). To simplify the study model, the 391 cases with SPK, the predominant category of PTx, were included in this study. Clinical data were analyzed to identify perioperative factors and post-transplant outcomes.
Assessment and definition
Pancreas graft loss was defined as a return of serum C-peptide to < 0.3 ng/ml. Kidney graft loss was defined as a return to dialysis. In defining graft loss, DWFG was considered a graft failure. Expanded donor criteria were defined based on criteria reported by Kapur et al. and Troppmann et al.12,13.
Ethics and statistical analysis
Given the anonymization of the data, the study was exempt from approval by the Institutional Review Board of Osaka University Hospital based on the ethical guideline in Japan, "Ethical Guidelines for Medical and Biological Research Involving Human Subjects." Informed consent was waived for the same reason. This study was conducted in accordance with the Declaration of Helsinki. Measured data are described as the mean ± standard deviation for continuous variables, and as the number (%) for categorical variables. Differences between groups were assessed by chi-squared, Fisher’s exact test, or Mann–Whitney U test, as appropriate. The cumulative incidence of pancreas graft loss was assessed by the Kaplan–Meier method. Hazard rates were measured in terms of the number of events per the number of patients at risk over a 1-year interval. To visualize the hazard rate pattern, we created smoothed curves with a Kernel smoothing procedure. Univariate and multivariate analyses of Cox proportional hazards regression models were performed to identify preoperative factors that may affect pancreas graft loss. Multivariate analysis was performed using significant factors and those with a tendency toward significance in the univariate analyses. Statistical analyses were performed using JMP Pro 14 software (SAS Institute Inc., Cary, NC, USA). p-values < 0.05 were considered significant, and p-values < 0.1 were considered to trend towards significance.
Results
Incidence and causes of pancreas graft loss after PTx
Post-transplant pancreas graft loss was identified in 77 of the 391 SPK cases (19.7%). The cumulative incidence of pancreas graft loss 1, 3, 5, and 10 years after PTx was 12.5%, 15.2%, 17.2%, and 24.9%, respectively. The pancreas graft loss was caused by DWFG (n = 34, 44.2%), graft thrombus (n = 22, 28.6%), chronic rejection (CR; n = 7, 9.1%), duodenal graft perforation (n = 6, 7.8%), acute rejection (AR; n = 3, 3.9%), recurrence of type 1 diabetes mellitus (n = 3, 3.9%), and pancreatoduodenal graft-related complications other than graft thrombus or duodenal graft perforation (n = 2, 2.6%). DWFG was caused by infection (n = 13), cerebro-cardiac disease (n = 10), malignancy (n = 4), multiple organ failure (n = 3), renal deficiency (n = 1), graft versus host disease (n = 1), and unknown reasons (n = 2). These causes are summarized in Table 1.
Clinical background based on cause of pancreas graft loss
In the present study, we focused on the three major causes of post-PTx pancreas graft loss: DWFG, graft thrombus, and CR. First, we compared the clinical backgrounds of these three groups (Table 2). In regard to donor-related factors (age, sex distribution, proportions of deaths caused by cerebrovascular accident, hemodynamic stability, cardiopulmonary arrest episodes, and marginal donors as defined by Kapur et al. and Troppmann et al.12,13), there were no significant differences among the groups. In contrast, donor body mass index (BMI) was significantly higher in the graft thrombus group than the DWFG group (p = 0.0279). The number of human leukocyte antigen mismatches was comparable among the groups. With regard to recipient-related factors, sex distribution, the duration of type 1 diabetes mellitus, the proportion of patients that required dialysis, the duration of dialysis, and the time after the registration of PTx were also not significantly different among the groups, whereas recipient age tended to be older in the DWFG group than the CR group (p = 0.058) and recipient BMI tended to be higher in the graft thrombus group than the DWFG group (p = 0.0615). There were also no significant differences in PTx-related factors, such as the duration of pancreas or kidney graft ischemia, among the three groups.
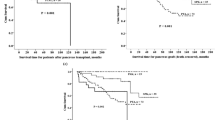
Timing of cause-specific pancreas graft loss
Next, we investigated the timing of graft loss due to the three major causes (Table 3). The average and median time from SPK to graft loss due to DWFG was 3.70 and 1.47 years [range 0.02 years (0.86 weeks) to 17.97 years], respectively. The 90th and 95th percentiles were 8.71 and 11.20 years, respectively. The loss occurred within the first postoperative month in 5.9%, within the first year in 47.1%, and within 5 years in 67.6%. In contrast, the average and median time from PTx to pancreas graft loss due to graft thrombus was 0.02 (0.86 weeks) and 0.01 years [0.57 weeks) (range 0.00 years (0.14 weeks) to 0.44 years (2.29 weeks)], respectively. The 90th and 95th percentiles were 0.40 years (2.00 weeks) and 0.40 years (2.29 weeks), respectively, and the loss occurred within the first postoperative month in 100.0%. The average and median time from PTx to the graft loss due to CR was 2.37 and 2.08 years [range 0.58 years (30.14 weeks) to 6.63 years], respectively. The 90th and 95th percentiles were 4.58 and 5.61 years, respectively. Though no cases developed CR within the first postoperative month, the loss occurred within the first year in 28.6% and within 5 years in 42.9%. Thus, the timing of pancreas graft loss was significantly different among the three causes. Notably, the time to graft loss was significantly shorter in the graft thrombus group than in the DWFG group and CR group (p = 0.0002 and p < 0.0001, respectively). The grafts in the DWFG group lasted longer than the grafts in the other groups. Although 47.1% were lost within the first year, 33.4% survived longer than 5 years, and two cases developed DWFG after more than 10 years. In the CR group, approximately 70.0% of the grafts lasted more than 1 year. The differences in the timing of pancreas graft loss were reflected in differences in the hazard rates of the three specific causes and the cumulative incidence of pancreas graft loss in the Kaplan–Meier curves (Fig. 1). Figure 2 shows the whole hazard rate of pancreas graft loss per year with the causes based on the timing. Thus, the timing of pancreas graft loss was significantly different among the causes. We also investigated the timing of DWFG-derived pancreas graft loss. The timing also varied among the causes of DWFG (Fig. 3).
Hazard rates and cumulative incidences of specific causes of pancreas graft loss in SPK cases. Upper panels: Hazard rates for graft loss within 10 years due to (A) DWFG, (B) graft thrombus, and (C) CR. Solid lines show smoothed curves obtained with a Kernel smoothing procedure based on the causes of the pancreas graft loss. The hazard rates were measured in terms of the number of events per the number of patients at risk over a 1-year interval. The smoothed curves were created to visualize the pattern of the hazard rates with a Kernel smoothing procedure. Lower panels: Cumulative incidences of post-transplant pancreas graft loss due to (A) DWFG, (B) graft thrombus, and (C) CR (solid lines). The cumulative incidence was assessed by the Kaplan–Meier method. CR chronic rejection, DWFG death with a functioning graft, SPK simultaneous pancreas-kidney transplantation.
Preoperative factors affecting cause-specific pancreas graft loss
Based on the results in the three groups, we investigated potential factors that might affect pancreas graft loss in univariate and multivariate Cox proportional hazards regression analyses. Preoperative factors associated with pancreas graft loss were significantly different among the three groups. The univariate analysis showed that, in the DWFG group, pancreas graft loss was significantly associated with recipient age [hazard ratio (HR) = 1.075, p = 0.0007], the duration of type 1 diabetes mellitus in the recipient (hazard ratio = 1.090, p = 0.0001), the duration of dialysis in the recipient (HR = 1.104, p = 0.0010), and the duration after the registration for PTx (HR = 1.102, p = 0.0399; Table 4). In the graft thrombus group, the univariate analysis showed that the donor BMI was significantly associated with pancreas graft loss (HR = 1.147, p = 0.0144). The recipient BMI tended to be associated (HR = 1.119, p = 0.0909). In the CR group, no preoperative factors were significantly associated with pancreas graft loss in the univariate analysis.
Finally, to identify independent preoperative factors significantly associated with pancreas graft loss, a multivariate analysis was performed using the significant factors and those with a tendency toward significance in the subgroups based on the causes of pancreas graft loss (Table 5). The analysis demonstrated that the duration of type 1 diabetes mellitus in the recipient was the only factor associated with DWFG-derived pancreas graft loss (HR = 1.064, p = 0.0276). As shown in Fig. 4A. The incidence of DWFG-derived pancreas graft loss was increased with the duration of type 1 diabetes mellitus. When the patients were divided into two groups based on the average (29.1 years) considering easy clinical application, a more than average duration was significantly associated with DWFG-related pancreas graft loss compared to less than average duration (HR = 2.458, p = 0.0134). In the graft thrombus group, donor BMI was the only factor that remained significantly associated with pancreas graft loss (HR = 1.147, p = 0.0160). The incidence of pancreas graft loss due to graft thrombus was increased based on the donor BMI (Fig. 4B). When the patients were divided into two groups based on the average (21.9 kg/m2), a more than average BMI was significantly associated with graft thrombus-related pancreas graft loss compared to less than average BMI (HR = 2.991, p = 0.0221). Thus, the significant preoperative factors independently associated with pancreas graft loss were different between the DWFG group and the graft thrombus group, and no preoperative factors were significantly associated with pancreas graft loss in the CR group.
Incidence of pancreas graft loss due to each cause based on the independent factor associated with the graft loss. (A) Incidence of DWFG-derived pancreas graft loss based on the duration of type 1 diabetes mellitus. (B) Incidence of graft thrombus-derived pancreas graft loss based on donor BMI. BMI Body mass index, DWFG death with a functioning graft.
Discussion
In the present study, we characterized three major specific causes of pancreas graft loss after SPK based on the nationwide PTx registry in Japan. The three causes were selected based on the frequency of occurrence in anticipation of the potential clinical applications of our results. We found that the timing of pancreas graft loss and associated preoperative factors were remarkably different for the three causes in the SPK cases.
Previous studies have discussed factors that significantly influence PTx outcomes in patients with type 1 diabetes mellitus, such as the ages of the recipient and donor, PTx category, pancreas graft preservation time, and immunosuppressive regimen14,15,16,17,18. However, these analyses included the entire PTx cohort without focusing on the causes of graft loss, even including PAK and PTA cases with considerably varied characteristics. Considering the potentially different characteristics of the causes, some significant factors associated with prognosis may have been masked in previous studies that included an entire population. Furthermore, due to the pooling of the various causes of pancreas graft loss, the statistical analyses may have overestimated the significance of certain factors. Ito et al. demonstrated that no factors significantly influenced pancreatic graft survival in a multivariate analysis of post-PTx outcomes based on the Japanese database19. If they had performed the analysis based on cause-specific subgroups, their results would have been similar to those reported in the present study.
The present study focused on the three major causes of pancreas graft loss and provided several new findings in the SPK cases. First, in the DWFG group, the timing of graft loss was not limited to a certain period, but varied widely. Moreover, the duration of type 1 diabetes mellitus was the only factor associated with graft loss due to DWFG. To date, no studies have investigated DWFG in post-PTx cases; however, considering the nature of DWFG, and particularly the causes of DWFG, our results were considered realistic. On the other hand, the predominant timing of each cause of DWFG may be different; in other words, infection-derived DWFG may develop early after PTx, whereas DWFG due to malignancy may occur long time after PTx (Fig. 3). In contrast, the timing of the development of cerebro-cardiac disease-derived DWFG seems to vary widely. Further investigation of trends in the timing of the DWFG-derived pancreas graft loss in larger studies would be expected. Second, unlike DWFG, pancreas allograft thrombosis has been discussed traditionally, particularly concerning the factors associated with graft loss. For example, factors associated with the donor, recipient, and surgery, including intraoperative hemodynamic state and organ preservation solutions, were previously reported to be risk factors for graft thrombosis20,21,22,23,24,25. Our results revealed that, in the presence of graft thrombus, the pancreas graft is lost very early after PTx. We also found that the donor BMI is a risk factor for graft loss due to graft thrombus. The timing of graft loss in the graft thrombus group was consistent with previous studies22,26,27. Our finding that the donor BMI is a risk factor for graft thrombus is consistent with previous findings22,25,27,28,29. Finally, no preoperative factors significantly associated with CR-derived graft loss were detected in SPK patients. However, more cases with CR-derived graft loss are required for the analysis than are included in this study. Considering that a solitary PTx (PAK or PTA) increased the risk of CR compared to an SPK, the case accumulation would not be easily completed.
Considering the potential clinical applications of our results, our findings will increase our understanding of the main causes of pancreas graft loss. For example, the timing of DWFG (causing 44.2% of pancreas graft loss) does not take into regard the length of the post-transplant period. In addition, increased understanding of the risk of pancreas graft loss associated with each cause may reduce delays in diagnosis and performing the post-transplant follow-up. In turn, this information may lead to improvements in the PTx outcome. For example, in patients with long-term type 1 diabetes mellitus who exhibit a high risk of DWFG (with an increasing rate of 6% per year), the clinician should closely check, before and after PTx, for systemic diseases that can cause DWFG, such as cerebro- or cardiovascular diseases, infection, or malignancy. For patients at high risk of graft thrombus, more careful postoperative management, such as more frequent checking of the blood flow by ultrasonography and administration of anti-thrombotic therapy, may be helpful for prevention. Thus, based on our results, clinicians can perform careful follow-ups, keeping in mind the specific characteristics of each cause, particularly the timing and factors associated with pancreas graft loss, which would in turn lead to earlier examinations and treatment for each cause, especially in cases at high risk for each cause. The present study results are somewhat novel in the field of PTx.
The present study has several limitations. First, the study was based on a database analysis; we searched the data for specific causes of pancreas graft loss. However, we might have missed some cases in which the pancreas graft was lost due to multiple causes. For example, in some cases, the database might have recorded pancreas graft loss due to a duodenal graft perforation, but CR may have caused the perforation. Ideally, a closer investigation of the causes is required. However, due to the retrospective study design, closer investigation was not possible. Therefore, this limitation may have affected the study results. Second, the definitions of some events, such as AR and CR, are not fixed in this database. Information regarding whether the diagnosis is based on the result of a biopsy of the pancreas graft is also not included in the database. These findings imply not only the existence of certain bias, especially among the institutions, but also room for improvement in the database. Third, this study is based on a nationwide registry in Japan, where the criteria for pancreatic graft loss is strictly determined as a return of serum C-peptide to < 0.3 ng/ml. In this context, it might be difficult to apply our results in some countries. The last limitation was the small number of SPK cases, even though the database included nationwide PTx cases. In particular, each of the three cause groups comprised low numbers of patients. If the number had been more, we could investigate factors associated with each cause of DWFG. Including more PTx cases would have enabled a closer investigation of factors that affected the outcome.
In summary, our results highlight different characteristics of the specific causes of pancreas graft loss, including the timing and associated preoperative factors after PTx. To the best of our knowledge, this study is the first to address this issue. In particular, DWFG occurred in 44.2% of the post-transplant cases, with the risk increasing at a rate of 6% per year of type 1 diabetes mellitus duration, and its timing has no regard for the length of the post-transplant period. These findings have increased our understanding of the specific causes of pancreas graft loss. Moreover, our results demonstrate the clinical utility of analyzing the specific causes of pancreas graft loss in patients undergoing PTx for type 1 diabetes mellitus.
Data availability
The data underlying this study cannot be shared publicly and restrictions apply to the availability of the data, which were used under license for the current study. However, data are available from the authors upon reasonable request and with permission from the Japan Society for Transplantation.
References
Gruessner, A. C., Sutherland, D. E. & Gruessner, R. W. Pancreas transplantation in the United States: A review. Curr. Opin. Organ. Transplant. 15, 93–101. https://doi.org/10.1097/MOT.0b013e32833552d2 (2010).
White, S. A., Shaw, J. A. & Sutherland, D. E. Pancreas transplantation. Lancet 373, 1808–1817. https://doi.org/10.1016/S0140-6736(09)60609-7 (2009).
Kelly, W. D., Lillehei, R. C., Merkel, F. K., Idezuki, Y. & Goetz, F. C. Allotransplantation of the pancreas and duodenum along with the kidney in diabetic nephropathy. Surgery 61, 827–837 (1967).
Jiang, A. T., Rowe, N., Sener, A. & Luke, P. Simultaneous pancreas-kidney transplantation: The role in the treatment of type 1 diabetes and end-stage renal disease. Can. Urol. Assoc. J. 8, 135–138. https://doi.org/10.5489/cuaj.1597 (2014).
Lerner, S. M. Kidney and pancreas transplantation in type 1 diabetes mellitus. Mt. Sinai J. Med. 75, 372–384. https://doi.org/10.1002/msj.20056 (2008).
Parajuli, S. et al. Outcomes of simultaneous pancreas and kidney transplants based on preemptive transplant compared to those who were on dialysis before transplant—A retrospective study. Transpl. Int. 33, 1106–1115. https://doi.org/10.1111/tri.13665 (2020).
Fridell, J. A. et al. The survival advantage of pancreas after kidney transplant. Am. J. Transplant. Off. J. Am. Soc. Transplant. Am. Soc. Transplant Surg. 19, 823–830. https://doi.org/10.1111/ajt.15106 (2019).
Ito, T. et al. Impact of pancreas transplantation on the patient survival-an analysis of the Japanese pancreas transplants registry. J. Clin. Med. https://doi.org/10.3390/jcm9072134 (2020).
Tomimaru, Y., Eguchi, H., Doki, Y., Ito, T. & Kenmochi, T. Current state of pancreas transplantation in Japan based on the nationwide registry. Ann. Gastroenterol. Surg. 5, 494–501. https://doi.org/10.1002/ags3.12423 (2021).
Tomimaru, Y., Ito, T. & Kenmochi, T. The registry of Japanese pancreas and islet transplantation 2020. Ishoku 55, 277–283 (2020).
Gruessner, A. C. & Gruessner, R. W. Pancreas transplantation of US and non-US cases from 2005 to 2014 as reported to the United Network for Organ Sharing (UNOS) and the International Pancreas Transplant Registry (IPTR). Rev. Diabet. Stud. 13, 35–58. https://doi.org/10.1900/RDS.2016.13.e2016002 (2016).
Kapur, S., Bonham, C. A., Dodson, S. F., Dvorchik, I. & Corry, R. J. Strategies to expand the donor pool for pancreas transplantation. Transplantation 67, 284–290. https://doi.org/10.1097/00007890-199901270-00017 (1999).
Troppmann, C. et al. Delayed endocrine pancreas graft function after simultaneous pancreas-kidney transplantation. Incidence, risk factors, and impact on long-term outcome. Transplantation 61, 1323–1330. https://doi.org/10.1097/00007890-199605150-00007 (1996).
Ayami, M. S., Grzella, S., Kykalos, S., Viebahn, R. & Schenker, P. Pancreas donor risk index but not pre-procurement pancreas allocation suitability score predicts pancreas graft survival: A cohort study from a large german pancreas transplantation center. Ann. Transplant. 23, 434–441. https://doi.org/10.12659/AOT.910014 (2018).
Zhou, J. et al. Influence of duration of type 1 diabetes on long-term pancreatic transplant outcomes. J. Hepatobiliary Pancreat. Sci. 26, 583–592. https://doi.org/10.1002/jhbp.677 (2019).
Gruessner, A. C. & Gruessner, R. W. Long-term outcome after pancreas transplantation: A registry analysis. Curr. Opin. Organ. Transplant. 21, 377–385. https://doi.org/10.1097/MOT.0000000000000331 (2016).
Gruessner, A. C., Sutherland, D. E. & Gruessner, R. W. Long-term outcome after pancreas transplantation. Curr. Opin. Organ. Transplant. 17, 100–105. https://doi.org/10.1097/MOT.0b013e32834ee700 (2012).
Sousa, M. G. et al. Risk factors of pancreatic graft loss and death of receptor after simultaneous pancreas/kidney transplantation. Transplant. Proc. 46, 1827–1835. https://doi.org/10.1016/j.transproceed.2014.05.048 (2014).
Ito, T., Kenmochi, T., Aida, N., Kurihara, K. & Asaoka, T. Are the outcomes of Japanese pancreas transplantation utilizing extended-criteria donors acceptable? A propensity score matching analysis for donors <50 or >/=50 years old. Transpl. Int. https://doi.org/10.1111/tri.13636 (2020).
Ciancio, G., Cespedes, M., Olson, L., Miller, J. & Burke, G. W. Partial venous thrombosis of the pancreatic allografts after simultaneous pancreas-kidney transplantation. Clin. Transplant. 14, 464–471. https://doi.org/10.1034/j.1399-0012.2000.140504.x (2000).
Ciancio, G., Julian, J. F., Fernandez, L., Miller, J. & Burke, G. W. Successful surgical salvage of pancreas allografts after complete venous thrombosis. Transplantation 70, 126–131 (2000).
Farney, A. C., Rogers, J. & Stratta, R. J. Pancreas graft thrombosis: Causes, prevention, diagnosis, and intervention. Curr. Opin. Organ. Transplant. 17, 87–92. https://doi.org/10.1097/MOT.0b013e32834ee717 (2012).
Grewal, H. P. et al. Risk factors for postimplantation pancreatitis and pancreatic thrombosis in pancreas transplant recipients. Transplantation 56, 609–612. https://doi.org/10.1097/00007890-199309000-00021 (1993).
Stockland, A. H. et al. Pancreas transplant venous thrombosis: Role of endovascular interventions for graft salvage. Cardiovasc. Interv. Radiol. 32, 279–283. https://doi.org/10.1007/s00270-009-9507-9 (2009).
Blundell, J., Shahrestani, S., Lendzion, R., Pleass, H. J. & Hawthorne, W. J. Risk factors for early pancreatic allograft thrombosis following simultaneous pancreas-kidney transplantation: A systematic review. Clin. Appl. Thromb. Hemost. 26, 1076029620942589. https://doi.org/10.1177/1076029620942589 (2020).
Delis, S. et al. Vascular complications of pancreas transplantation. Pancreas 28, 413–420. https://doi.org/10.1097/00006676-200405000-00010 (2004).
Patel, S. R. & Hakim, N. Prevention and management of graft thrombosis in pancreatic transplant. Exp. Clin. Transplant. 10, 282–289. https://doi.org/10.6002/ect.2012.0003 (2012).
Humar, A. et al. The impact of donor obesity on outcomes after cadaver pancreas transplants. Am. J. Transplant. Off. J. Am. Soc. Transplant. Am. Soc. Transplant. Surg. 4, 605–610. https://doi.org/10.1111/j.1600-6143.2004.00381.x (2004).
Sampaio, M. S. et al. Obesity was associated with inferior outcomes in simultaneous pancreas kidney transplant. Transplantation 89, 1117–1125. https://doi.org/10.1097/TP.0b013e3181d2bfb2 (2010).
Acknowledgements
We thank Dr. Masaaki Watanabe and Dr. Yasuyuki Koshizuka (Hokkaido University Hospital), Dr Shigehito Miyagi and Dr. Kazuaki Tokodai (Tohoku University Hospital), Dr. Ryo Okada and Dr. Akira Kenjo (Fukushima Medical University Hospital), Dr. Yukihiro Iso and Dr. Keiichi Kubota (Dokkyo Medical University Hospital), Dr. Hiroto Egawa and Dr. Yoshihito Kotera (Tokyo Women’s Medical University Hospital), Dr. Shigeyuki Kawachi and Dr. Hitoshi Iwamoto (Tokyo Medical University Hachioji Medical Center), Dr. Toshifumi Wakai and Dr. Takashi Kobayashi (Niigata University Hospital), Dr. Shunji Narumi and Dr. Takahisa Hiramitsu (Japanese Red Cross Aichi Medical Center Nagoya Daini Hospital), Dr. Taihei Ito (Fujita Health University Hospital), Dr. Hidetaka Ushigome and Dr. Shuji Nobori (Kyoto Prefectural University Hospital), Dr. Takayuki Anazawa and Dr. Hideaki Okajima (Kyoto University Hospital), Dr. Hirochika Toyama and Dr. Yoshihide Nanno (Kobe University Hospital), Dr. Hideki Ohdan and Dr. Hiroyuki Tahara (Hiroshima University Hospital), Dr. Keiichi Okano and Dr. Minoru Oshima (Kagawa University Hospital), Dr. Keizo Kaku and Dr. Yasuhiro Okabe (Kyushu University Hospital), Dr. Tomohiko Adachi and Dr. Hajime Matsushima (Nagasaki University Hospital), and Dr. Yoshifumi Beck and Dr. Akira Maki (Saitama Medical Center, Saitama Medical University) for their cooperation with the Japan Pancreas Transplant Registry of The Japanese Pancreas and Islet Transplant Association.
Author information
Authors and Affiliations
Contributions
Y.T., S.K., T.I., and H.E. designed the study. Y.T. drafted the manuscript. S.K., T.I., and H.E. contributed to analysis and interpretation of the study. K.S., Y.I., D.Y., T.N., H.T., T.K., and Y.D. supervised the analysis and interpretation. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tomimaru, Y., Kobayashi, S., Ito, T. et al. Different timing and risk factors of cause-specific pancreas graft loss after simultaneous pancreas kidney transplantation. Sci Rep 12, 17666 (2022). https://doi.org/10.1038/s41598-022-22321-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-22321-x
- Springer Nature Limited