Abstract
We aimed to verify the combined use of two frailty tools in predicting mortality in older adults. We used the data of 10,276 Japanese older adults (aged ≥ 65 years) who provided valid responses to two frailty assessment tools in a mail survey in Japan’s Kyoto‒Kameoka Prospective cohort study. Frailty status was categorized into four groups depending on the validated frailty screening index and Kihon Checklist, respectively: Non-frailty (n = 5960), Physical frailty (n = 223), Comprehensive frailty (n = 2211), and Combination (n = 1882) groups. Mortality data were collected between July 30, 2011, and November 30, 2016. We assessed the relationship between frailty status and all-cause mortality risk using multivariate Cox proportional hazards models. During a median follow-up of 5.3 years, we recorded 1257 deaths. After adjusting for confounders, the Combination group had the highest mortality risk compared with the other groups [Non-frailty: reference; Physical frailty: hazards ratio [HR], 0.99 (95% confidence interval [CI] 0.58 to 1.70); Comprehensive frailty: 1.91 (1.63 to 2.23); Combination: 2.85 (2.44 to 3.22)]. People who are positive for frailty in both instruments have a higher risk of death than those who are positive to one model.
Similar content being viewed by others
Introduction
Frailty is a condition wherein multiple physiological reserves deteriorates because of decreased homeostasis ability to cope with stress1,2. Frailty, which is the antonym of “fit,”3,4 indicates biological aging5,6; as such, it is a public health problem among older adults worldwide7. Therefore, to extend the healthy longevity of older adults, the effect of frailty—with a focus on biological aging—on prognosis should be assessed.
Frailty can be broadly assessed using two models: the phenotype model by Fried et al.8 and the deficit accumulation model by Mitnitski and Rockwood et al.9,10. The phenotype model mainly assesses physical characteristics8, whereas the deficit accumulation model reflects the accumulation of multiple factors, including social, cognitive factors, and physical aspects9,10 that may induce adverse events. Individuals identified as frail based on the definitions of these models may not necessarily match11. However, frailty is related to mortality11,12,13,14 and the risk of disability in older adults11,13, regardless of the type of model used.
There are more than 20 methods for assessing frailty3, and these methods differ from one study to another. Consequently, there were reports of inconsistencies in the classification of frailty and in the predictive capacity depending on the frailty assessment method used11. Therefore, it is possible that the prognoses of older adults who qualified frail as defined by the combined use of multiple frailty and single frailty assessment tool may differ12. Nevertheless, to the best of our knowledge, combining both tools for assessing frailty to determine mortality risk in Japanese older adults has not yet been investigated. Disability complications of frailty are reversible since individuals can return to a healthy state through appropriate lifestyle intervention15,16; therefore, it is essential to identify high-risk older adults for early detection and treatment of frailty. In this study, we aimed to conduct a community-based longitudinal cohort study among older adults to investigate the combined use of two validated frailty assessment tools in determining the risk of all-cause mortality. We hypothesized that the combined use of the two models would lead to a stronger association between frailty and mortality risk than the use of either model individually.
Methods
Study population and assessment of baseline characteristics
The Kyoto-Kameoka study is a cohort study of older adults aged ≥ 65 years residing in Kameoka City, Kyoto Prefecture, Japan. The details of the Kyoto-Kameoka study have been published elsewhere17,18,19,20,21,22,23. A survey was conducted among the residents of Kameoka City, aged ≥ 65 years as of July 1, 2011. A municipal employee in charge of the survey selected qualified participants based on their name, sex, and date of birth, which were obtained from the Basic Resident Register maintained by Kameoka City Hall (Fig. 1). Finally, a total of 10,276 participants were included in this prospective study. We obtained informed consent from all participants upon receiving their responses to the mail-in survey. This study was conducted according to principles of the Declaration of Helsinki and all procedures involving research study participants were approved by the Research Ethics Committee of Kyoto Prefectural University of Medicine (RBMR-E-363), the National Institutes of Biomedical Innovation, Health and Nutrition (NIBIOHN-76-2), and Kyoto University of Advanced Science (No. 20-1). The reporting of this study conformed to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)24.
Definition of frailty
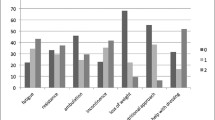
We used two frailty assessment tools, namely, self-administered frailty screening index (FSI), with five previously validated question items20,25, and self-administered Kihon Checklist (KCL), with 25 previously validated question items20,26,27 (Supplementary Tables 1 and 2). The FSI is based on the phenotype model, which mainly assesses frailty from the perspective of physical aspects (physical frailty); meanwhile, KCL is based on the accumulation of the deficit model, which assesses frailty from multidimensional perspectives (comprehensive frailty), including social, cognitive factors, and physical aspects. Physical frailty based on the FSI is defined as three or more of the five items25. Comprehensive frailty based on the KCL is defined as seven or more of the 25 items20,26,27. The seven subdomains included in the KCL (instrumental activities of daily living, physical function, nutritional status, oral function, social status, cognitive status, and depression) have been assessed in accordance with a previous study28.
Outcomes
The survival status of the cohort participants during the follow-up period was assessed using the data from the Basic Resident Register maintained by Kameoka City Hall. These data were collected between July 30, 2011, and November 30, 2016. We performed censoring of residents who lost their official resident status, left the country, or moved to another municipality.
Statistical analysis
The participants were assigned to one of the four groups: Non-frailty, when unqualified with either physical nor comprehensive frailty (n = 5960, 58.0%); Physical frailty, when unqualified with comprehensive frailty (n = 223, 2.2%); Comprehensive frailty, when unqualified with physical frailty (n = 2211, 21.5%); and Combination group, when qualified with both physical and comprehensive frailty (n = 1882, 18.3%).
Descriptive statistics for continuous variables are shown as the mean and standard deviation, and intergroup comparisons were performed using analysis of variance. Categorical variables are shown as number of people and percentage, and intergroup comparisons were performed using Pearson’s chi-square test. Where covariate information pertaining to the family structure (n = 675, 6.6%); socioeconomic status (n = 395, 3.8%); education (n = 1139, 11.0%); smoking status (n = 257, 2.5%); alcohol status (n = 230, 2.2%); sleep time (n = 536, 5.2%); and medications (n = 657, 6.4%) was missing, we imputed data using the five data sets created using multiple imputation by chained equation (MICE)29 package using R statistical software (process: m [number of imputed datasets] = 5; predictorMatrix = predmtx1; maxit [a scalar giving the number of iterations] = 50; meth [imputation method] = predictive mean matching [pmm], logreg, or polr 500 seed). The imputation method for continuous, binary, and ordered categorical variables used the pmm, logreg, and polr, respectively. To impute the missing data, the predictors used all Model 2 variables and variables that were associated with missingness21. The integrated parameter was calculated by arithmetic mean for the data sets. All missing values were assumed to be missing at random. It has been suggested that 5% missing data is the upper threshold for which multiple imputations provide a benefit in large data sets; if the missing values exceed 10%, it is stated that bias is likely in the analyses30. The details of the missing data pattern for covariates are shown in Supplementary Fig. 1. The number of complete cases without missing values was 7520 (73.2%). Furthermore, we compared the characteristics of the individuals who participated in this study with those who were excluded.
The absolute risk of all-cause mortality in each of the four groups in accordance with the degree of frailty is shown as the number of events per 1000 person-years. To adjust for confounding factors in the relationship between frailty and the risk of all-cause mortality, we used multivariate Cox proportional hazards analysis that included the baseline covariates. The Schoenfeld residuals test was performed to confirm the assumptions of the Cox proportional-hazard model. Proportional hazard conditions were assumed because the test did not reject the data (p = 0.173). We conducted multivariate analysis using the following two models: Model 1 was adjusted for age (continuous), sex (female or male), and population density (≥ 1000 or < 1000 people/km2), and Model 2 was further adjusted for the following factors in Model 1: living alone (yes or no), socioeconomic status (high or low), educational attainment (< 9, 10–12, or ≥ 13 years), smoking status (never smoker, past smoker, or current smoker), alcohol drinker (yes or no), sleep time (continuous), medication use (continuous), and number of chronic diseases (continuous). These adjustment factors were decided with reference to covariates used in previous studies that examined the association between frailty11,31, KCL27, or FSI25 and mortality or factors associated with prevalence of frailty17,18,23 before performing the statistical analysis. The results of these analyses are shown as hazards ratio (HR) and 95% confidence interval (CI), and HRs were calculated with the non-frailty group as the reference group. The interaction between physical and comprehensive frailty regarding the risk of mortality was assessed with relative excess risk due to interaction (RERI) as an additive interaction. We performed sensitivity analyses using the following two methods: (1) to remove the possibility of a causal reversal relationship, we excluded mortality events (males: 244, females: 169) that were recorded during the first two years of the follow-up survey19; (2) we performed the same analyses using complete case datasets that included no missing values32. We examined the relationship between the subdomains included in the FSI and KCL, which were used for assessing frailty, and the risk of all-cause mortality in the same way. In addition, we constructed adjusted Kaplan–Meier survival curves using the inverse probability weighting including the variables of adjustment Model 233.
To assess the curvature of the relationship between the FSI and KCL scores and the risk of all-cause mortality, we used the restricted cubic spline model with three data points (5th, 50th, and 95th percentiles) based on the score distributions for these two assessments22,23. The results are shown as HR and 95% CI, with HR being calculated based on FSI and KCL scores of 0 points (no frailty).
The significance for all statistical analyses was set at < 5% on both sides. All statistical analyses were performed using STATA MP version 15.0 (StataCorp LP, College Station, TX, USA), and/or R software 3.4.3 (R Core Team, Vienna, Austria).
Results
Population and exposure characteristics
The characteristics of the participants in each of the four or two groups corresponding to the frailty status are shown in Table 1 and Supplementary Table 3. When compared to the Non-frailty group, the Combination group participants were older, predominantly women, and had a lower level of educational attainment. The prevalence rates of Physical and Comprehensive frailty were 20.5% and 39.8%, respectively (Supplementary Table 4). Participants in the Combination group had a higher prevalence of the subdomains of KCL and FSI than individuals with only one of those conditions (Supplementary Table 5). Meanwhile, the individuals excluded from this study were older, and the majority were women compared to those included in this study (Supplementary Table 6).
Combined use of two frailty concept models in mortality
The relationships between frailty status and the risk of all-cause mortality are shown in Fig. 2 and Table 2. The median follow-up period was 5.3 years (50,984 person-years). During the follow-up period, 1257 individuals (12.2%) died. Even after adjusting for confounding factors, the Combination group had the highest risk for all-cause mortality relative to the other groups [Non-frailty group: reference; Physical frailty: HR, 0.99 (95% CI 0.58–1.70); Comprehensive frailty: HR, 1.91 (95% CI 1.63–2.23); Combination: HR, 2.85 (95% CI 2.44–3.22), p < 0.001]. The interaction between Physical and Comprehensive frailty accounted for 51.3% relative excess risk of mortality in the Combinations group. Several of the sensitivity analyses also yielded the same results but the sensitivity analysis after excluding participants with an event in the first two years of follow-up was not significant for the RERI using a categorical frail/non-frail variable for KCL and FSI (Supplementary Tables 7 and 8). In addition, these findings were similar to the results using frailty defined by FSI of ≥ 2 points (Supplementary Table 9). The same results were observed even when the samples were stratified by age or sex, with more pronounced results obtained for men and individuals aged ≥ 75 years (Supplementary Tables 10 and 11). Moreover, there was a relationship between all subdomains included in the FSI and KCL and the risk of all-cause mortality (Supplementary Table 12).
Multivariate adjusted Kaplan–Meier survival curves using inverse probability weighting for all-cause mortality according to frailty status among older adults. (a) Four groups stratified by frailty screening index (FSI) and Kihon Checklist (KCL); (b) two groups stratified by FSI; (c) two groups stratified by KCL. Nf, non-frailty; Ph, physical frailty; Ch, comprehensive frailty; Cb, combinations. The adjustment factors are age, sex, population density, family structure, economic status, educational attainment, smoking status, alcohol consumption status, sleep time, medication use, and number of chronic diseases.
Dose-response relationships
We assessed the curvature relationship of the FSI and KCL scores with the risk of mortality using the restricted cubic spline model (Fig. 3). Even after adjusting for baseline confounding factors, there was a strong log linear relationship between both scores and the risk of all-cause mortality in a dose–response-dependent manner (did not show a linear relationship for FSI ≤ 2 points). Multivariate-adjusted HR (95% CI) of all-cause mortality for each one-point increment was 1.36 (1.29–1.42) for FSI and 1.10 (1.09–1.11) for KCL.
Restricted cubic spline regression model between KCL (a) and FSI (b) score and risk of all-cause mortality. The Kihon Checklist (KCL) and Frailty Screening Index (FSI) received a point by every problem with activity or function, and the higher the total score, the greater the difficulty in daily functioning (high frailty). Solid lines represent hazard ratios, and dashed lines represent 95% confidence intervals (CI), and the hazard ratio based on 0 point of both KCL and FSI as reference was calculated. We estimated that p < 0.05 when the 95% CI of the hazard ratio exceeded 1.00, and p ≥ 0.05 when the 95% CI of the hazard ratio did not exceed 1.00. The adjustment factors are age, sex, population density, family structure, economic status, educational attainment, smoking status, alcohol consumption status, sleep time, medication use, and number of chronic diseases.
Discussion
Main findings
In this population-based cohort study of older adults, we examined the combined use of two verified frailty assessment tools in assessing the risk of mortality. After adjusting for confounders, we found that the Combination group had the strongest association with the risk of all-cause mortality compared with the other groups. To the best of our knowledge, this is the first study to verify the combined use of two frailty tools to assess the relationship between frailty status and mortality risk in Japanese individuals. Our results suggest that frailty assessed by the combined use of multiple frailty assessment tools may have a higher predictive ability for prognosis than frailty assessed using any single tool.
Prevalence of physical and comprehensive frailty
Our results showed that the prevalence of Comprehensive frailty (39.8%) was higher than that of Physical frailty (20.5%), which is consistent with the findings of previous studies21,23. These prevalence of frailty is relatively higher than what was reported in other well-established cohorts34. This could be attributed to the fact that the prevalence of frailty assessed using KCL was higher than those assessed using commonly used screening instruments26. Comprehensive frailty, as defined using the KCL, included multiple components such as cognitive, social, and other factors. In contrast, physical frailty, as defined using the FSI, focuses mainly on the physical aspects. Thus, consideration must be given to the possibility that the pathologies resulting from comprehensive and physical frailty may differ35. However, approximately 90% of the people with physical frailty in our study had comprehensive frailty. Therefore, it is important to assess the prognosis of those with both physical and comprehensive frailty and those with a single type of frailty.
Main outcomes
A previous study that followed-up 4721 older adults aged ≥ 65 years for four years found that individuals who were deemed to be frail based on both phenotype and deficit accumulation model had the highest risk of mortality12. In our study, we found the same results when we used the data of more than 10,000 individuals (50,984 person-years), which is more than double the size of that of the previous study. Previous studies that compared comprehensive frailty, considering multiple factors, and physical frailty, which focuses on physical factors only, reported that comprehensive frailty had higher accuracy in predicting the risk of mortality12,14. This could be due to the fact that comprehensive frailty indices, which assess frailty using a multi-faceted model have a linear positive correlation with age, and thus reflect biological aging5,6. Furthermore, middle-aged and older adults with both sarcopenia and frailty have a higher rate of all-cause mortality36,37 and a higher risk of cardiovascular and respiratory diseases36 than individuals with only one of those conditions. Findings of previous studies corroborates our results. Therefore, frailty defined through the combined use of two frailty tools may better identify the high-risk group than only either of the assessment models. However, a previous study concluded that combining different screening instruments does not improve predictive power of dependency, mortality, and hospitalization38. The study included only pre-frail and frail patients and did not include non-frail individuals. Our study population consisted of both frail and non-frail individuals as our sample was from the general population. We recommend further exploration of other combinations of instruments among other study populations because these differences might have affected the results. In addition, these detailed mechanisms need to be elucidated through interventional and basic research35. The data shown in our study may be helpful in identifying those with poorer prognoses of older adults.
Dose-response relationships
Furthermore, we found a log linear positive dose–response relationship between the mortality risk and the FSI and KCL scores, which are used to assess frailty (did not show a linear relationship for FSI ≤ 2 points). This observation concurs with the phenotypic definition of frailty12. No previous studies have investigated the dose–response relationship between FSI/KCL scores and mortality risk25,27. Considering that the frailty is understood to exist on a spectrum from fit to frail3,4, our results appear to appreciate this with the identification of a dose-response with each of the two frailty instruments, whereas the use of sequential frailty categorization to define frailty populations will lead to loss of information value from each of these tools that are under and over this categorization threshold. Therefore, it is likely to be useful in the early prediction of the prognosis of older adults by spectrum from fit to frail using these indices with continuous variables.
Strengths and limitations
The strength of this study is that we investigated the relationship of the risk of all-cause mortality with physical and comprehensive frailty defined using two validated assessment tools in a large-scale cohort study of community-dwelling older adults. Nevertheless, this study had several methodological limitations. First, although we used the validated frailty assessment tools, there may have been a self-reporting bias since our survey was based on a self-administered questionnaire. Two tools developed in the Japanese population were applied in defining frailty. This may be limited in its generalizability to other populations. There is need to re-evaluate using the most commonly used instruments for frailty assessment (Fried’s Phenotype model and the Rockwood’s Frailty Index)3 because our results may vary depending on the tool used to determine frailty. Although frailty status has an intermediate pre-frailty category, frailty assessments were dichotomized as frail or non-frail in this study. The dichotomization of frailty status is an over-simplification of the concept of frailty and the results may lead to misclassification of frailty status due to the dependence on the cut-off value used to determine frailty. This kind of misclassification in the exposure assessments might have weakened the relationship between mortality risk and frailty. Despite this, our study confirmed the relationship between mortality risk and frailty. Second, the observation period in our study was relatively short. This may have affected the relationship between frailty and mortality risk. In addition, because we could not obtain data on the cause of death, we did not examine whether frailty might have been linked to various causes of death. Furthermore, there is the possibility of selection bias due to different participant characteristics such as age and sex between participants included and excluded from this study. Third, physical frailty, as assessed using the FSI, is not perfectly consistent with the phenotype model advocated by Fried et al.8. The phenotype model includes grip strength (weakness)8, but because this index requires actual measurements, FSI utilizes cognitive function instead of referencing several frailty assessment questionnaires25. However, we confirmed the good predictivity of KCL and FSI against frailty defined by the revised Japanese version of the Cardiovascular Health Study criteria according to the Fried phenotype model in the sub-cohort of Kyoto-Kameoka study, which measured grip strength and gait speed20. In addition, we have previously reported that FSI can predict disability in older Japanese adults25. Fourth, although we found nearly no difference in the overall results of our observational study even after adjusting for several participant characteristics of participants and lifestyle-related factors, there may still be remaining confounding factors linked to frailty and the risk of all-cause mortality. Finally, although we imputed data using the multiple imputation method for missing data, the choices of the imputation methods, predictors, and the number of imputations (number of imputed datasets), among others, could have a significant impact on the quality of imputation. These limitations may make it difficult to generalize the study results.
Perspective
In recent years, there has been a paradigm shift from a focus on individual diseases to a perception that multiple chronic diseases have common risk factors39 and that the simultaneous presence of multiple pathological conditions has a powerful influence over people’s health trajectory, disabilities, and the complexity of the care they require40. Frailty occurs because of complex interactions between various factors41. Thus, assessing frailty from a multifaceted perspective through the use of multiple frailty assessment indices may allow more sensitive identification of older adults with poor prognoses, including mortality. Considering that the degree of frailty observed across most adult age groups increased in the United States during 1999–201842, our results may provide useful clues that can be used to identify high-risk older adults.
Conclusion
Our results suggested that the combined use of tools to assess frailty was more strongly linked to the risk of mortality among older adults. These results suggest that assessment of frailty from a multifaceted approach using multiple frailty assessment indices may allow high-sensitive identification of older adults with poor prognoses and increased risk of mortality.
Data availability
The datasets used and/or analysed during the current study available from the corresponding author (d2watanabe@nibiohn.go.jp), TY (t-yoshida@nibiohn.go.jp), and YY (yamaday@nibiohn.go.jp) on reasonable request.
References
Clegg, A., Young, J., Iliffe, S., Rikkert, M. O. & Rockwood, K. Frailty in elderly people. Lancet 381, 752–762. https://doi.org/10.1016/S0140-6736(12)62167-9 (2013).
Hoogendijk, E. O. et al. Frailty: Implications for clinical practice and public health. Lancet 394, 1365–1375. https://doi.org/10.1016/S0140-6736(19)31786-6 (2019).
Dent, E. et al. The Asia-Pacific clinical practice guidelines for the management of frailty. J. Am. Med. Dir. Assoc. 18, 564–575. https://doi.org/10.1016/j.jamda.2017.04.018 (2017).
Romero-Ortuno, R. & O’Shea, D. Fitness and frailty: opposite ends of a challenging continuum! Will the end of age discrimination make frailty assessments an imperative?. Age Ageing 42, 279–280. https://doi.org/10.1093/ageing/afs189 (2013).
Hamczyk, M. R., Nevado, R. M., Barettino, A., Fuster, V. & Andres, V. Biological versus chronological aging: JACC focus seminar. J. Am. Coll. Cardiol. 75, 919–930. https://doi.org/10.1016/j.jacc.2019.11.062 (2020).
Rockwood, K., Rockwood, M. R. & Mitnitski, A. Physiological redundancy in older adults in relation to the change with age in the slope of a frailty index. J. Am. Geriatr. Soc. 58, 318–323. https://doi.org/10.1111/j.1532-5415.2009.02667.x (2010).
Morley, J. E. et al. Frailty consensus: A call to action. J. Am. Med. Dir. Assoc. 14, 392–397. https://doi.org/10.1016/j.jamda.2013.03.022 (2013).
Fried, L. P. et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 56, M146-156. https://doi.org/10.1093/gerona/56.3.m146 (2001).
Mitnitski, A. B., Mogilner, A. J. & Rockwood, K. Accumulation of deficits as a proxy measure of aging. ScientificWorldJournal 1, 323–336. https://doi.org/10.1100/tsw.2001.58 (2001).
Rockwood, K. & Mitnitski, A. Frailty in relation to the accumulation of deficits. J. Gerontol. A Biol. Sci. Med. Sci. 62, 722–727. https://doi.org/10.1093/gerona/62.7.722 (2007).
Lin, S. M. et al. Comparison of 3 frailty instruments in a geriatric acute care setting in a low-middle income country. J. Am. Med. Dir. Assoc. 19, 310–314. https://doi.org/10.1016/j.jamda.2017.10.017 (2018).
Kulminski, A. M. et al. Cumulative deficits better characterize susceptibility to death in elderly people than phenotypic frailty: lessons from the Cardiovascular Health Study. J. Am. Geriatr. Soc. 56, 898–903. https://doi.org/10.1111/j.1532-5415.2008.01656.x (2008).
Malmstrom, T. K., Miller, D. K. & Morley, J. E. A comparison of four frailty models. J. Am. Geriatr. Soc. 62, 721–726. https://doi.org/10.1111/jgs.12735 (2014).
Rockwood, K., Andrew, M. & Mitnitski, A. A comparison of two approaches to measuring frailty in elderly people. J. Gerontol. A Biol. Sci. Med. Sci. 62, 738–743. https://doi.org/10.1093/gerona/62.7.738 (2007).
Gill, T. M. et al. A program to prevent functional decline in physically frail, elderly persons who live at home. N. Engl. J. Med. 347, 1068–1074. https://doi.org/10.1056/NEJMoa020423 (2002).
Gill, T. M., Gahbauer, E. A., Allore, H. G. & Han, L. Transitions between frailty states among community-living older persons. Arch. Intern. Med. 166, 418–423. https://doi.org/10.1001/archinte.166.4.418 (2006).
Watanabe, D. et al. A U-shaped relationship between the prevalence of frailty and body mass index in community-dwelling Japanese older adults: The Kyoto-Kameoka study. J. Clin. Med. https://doi.org/10.3390/jcm9051367 (2020).
Watanabe, D. et al. Diet quality and physical or comprehensive frailty among older adults. Eur. J. Nutr. 61, 2451–2462. https://doi.org/10.1007/s00394-022-02819-w (2022).
Watanabe, D. et al. Dose-response relationship between life-space mobility and mortality in older Japanese adults: a prospective cohort study. J. Am. Med. Dir. Assoc. https://doi.org/10.1016/j.jamda.2022.04.017 (2022).
Watanabe, D. et al. Validation of the Kihon Checklist and the frailty screening index for frailty defined by the phenotype model in older Japanese adults. BMC Geriatr. 22, 478. https://doi.org/10.1186/s12877-022-03177-2 (2022).
Yamada, Y. et al. Prevalence of frailty assessed by fried and kihon checklist indexes in a prospective cohort study: Design and demographics of the Kyoto-Kameoka longitudinal study. J. Am. Med. Dir. Assoc. 18(733), e737–e733. https://doi.org/10.1016/j.jamda.2017.02.022 (2017).
Watanabe, D. et al. Objectively measured daily step counts and prevalence of frailty in 3,616 older adults. J. Am. Geriatr. Soc. 68, 2310–2318. https://doi.org/10.1111/jgs.16655 (2020).
Watanabe, D. et al. Association between the prevalence of frailty and doubly labeled water-calibrated energy intake among community-dwelling older adults. J. Gerontol. A Biol. Sci. Med. Sci. 76, 876–884. https://doi.org/10.1093/gerona/glaa133 (2021).
von Elm, E. et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. PLoS Med. 4, e296. https://doi.org/10.1371/journal.pmed.0040296 (2007).
Yamada, M. & Arai, H. Predictive value of frailty scores for healthy life expectancy in community-dwelling older Japanese adults. J. Am. Med. Dir. Assoc. 16(1002), e1007-1011. https://doi.org/10.1016/j.jamda.2015.08.001 (2015).
Ambagtsheer, R. C. et al. Commonly used screening instruments to identify frailty among community-dwelling older people in a general practice (primary care) setting: A study of diagnostic test accuracy. J. Gerontol. A Biol. Sci. Med. Sci. 75, 1134–1142. https://doi.org/10.1093/gerona/glz260 (2020).
Satake, S., Shimokata, H., Senda, K., Kondo, I. & Toba, K. Validity of total kihon checklist score for predicting the incidence of 3-year dependency and mortality in a community-dwelling older population. J. Am. Med. Dir. Assoc. 18(552), e551-552. https://doi.org/10.1016/j.jamda.2017.03.013 (2017).
Watanabe, D. et al. Association between mixing ability of masticatory functions measured using color-changing chewing gum and frailty among Japanese older adults: The Kyoto-Kameoka study. Int. J. Environ. Res. Public Health https://doi.org/10.3390/ijerph17124555 (2020).
Buuren, S. V. & Groothuis-Oudshoorn, K. Mice: Multivariate imputation by chained equations in R. J. Stat. Softw. 45, 1–67 (2011).
Madley-Dowd, P., Hughes, R., Tilling, K. & Heron, J. The proportion of missing data should not be used to guide decisions on multiple imputation. J. Clin. Epidemiol. 110, 63–73. https://doi.org/10.1016/j.jclinepi.2019.02.016 (2019).
Hoogendijk, E. O. et al. Frailty combined with loneliness or social isolation: An elevated risk for mortality in later life. J. Am. Geriatr. Soc. 68, 2587–2593. https://doi.org/10.1111/jgs.16716 (2020).
Sterne, J. A. et al. Multiple imputation for missing data in epidemiological and clinical research: Potential and pitfalls. BMJ 338, b2393. https://doi.org/10.1136/bmj.b2393 (2009).
Xie, J. & Liu, C. Adjusted Kaplan-Meier estimator and log-rank test with inverse probability of treatment weighting for survival data. Stat. Med. 24, 3089–3110. https://doi.org/10.1002/sim.2174 (2005).
O’Caoimh, R. et al. Prevalence of frailty in 62 countries across the world: a systematic review and meta-analysis of population-level studies. Age Ageing 50, 96–104. https://doi.org/10.1093/ageing/afaa219 (2021).
Fried, L. P. et al. The physical frailty syndrome as a transition from homeostatic symphony to cacophony. Nat. Aging 1, 36–46 (2021).
Petermann-Rocha, F., Gray, S. R., Pell, J. P., Ho, F. K. & Celis-Morales, C. The joint association of sarcopenia and frailty with incidence and mortality health outcomes: A prospective study. Clin. Nutr. 40, 2427–2434. https://doi.org/10.1016/j.clnu.2020.10.044 (2021).
Thompson, M. Q. et al. Frailty and sarcopenia in combination are more predictive of mortality than either condition alone. Maturitas 144, 102–107. https://doi.org/10.1016/j.maturitas.2020.11.009 (2021).
Op Het Veld, L. P. M. et al. Can the combined use of two screening instruments improve the predictive power of dependency in (Instrumental) activities of daily living, mortality and hospitalization in old age?. J. Frailty Aging 8, 180–185. https://doi.org/10.14283/jfa.2019.17 (2019).
Kaeberlein, M., Rabinovitch, P. S. & Martin, G. M. Healthy aging: The ultimate preventative medicine. Science 350, 1191–1193. https://doi.org/10.1126/science.aad3267 (2015).
Fried, L. P. & Rowe, J. W. Health in aging - past, present, and future. N. Engl. J. Med. 383, 1293–1296. https://doi.org/10.1056/NEJMp2016814 (2020).
Dent, E. et al. Management of frailty: Opportunities, challenges, and future directions. Lancet 394, 1376–1386. https://doi.org/10.1016/S0140-6736(19)31785-4 (2019).
Blodgett, J. M., Rockwood, K. & Theou, O. Changes in the severity and lethality of age-related health deficit accumulation in the USA between 1999 and 2018: a population-based cohort study. Lancet Healthy Longev. 2, e96-104 (2021).
Acknowledgements
We would like to express our appreciation to all participants of this study and to all individuals involved in the data collection. We acknowledge several administrative of Kameoka city and Kyoto prefecture. We would like to thank the Kyoto–Kameoka Study Group who contributed their resources to the development of this study. We would like to thank Editage (www.editage.jp) for the English-language editing. The Kyoto-Kameoka study was conducted with JSPS KAKENHI and was supported by a research grant provided to Misaka Kimura (24240091), Yosuke Yamada (15H05363), and Daiki Watanabe (21K17699); a grant and administrative support by the Kyoto Prefecture Community-based Integrated older adults Care Systems Promotion Organization since 2011; Kameoka City under the program of the Long-term Care Insurance and Planning Division of the Health and Welfare Bureau for the older adults, Ministry of Health, Labor, and Welfare and the World Health Organization (WHO) Collaborating Centre on Community Safety Promotion. The Article Processing Charges was supported by Health and Labor Sciences Research Grant provided to Motohiko Miyachi (22AC5004 and 21FA1004).
Author information
Authors and Affiliations
Contributions
Study concept and design: D.W., T.Y., and Y.Y. Acquisition of data: T.Y., Y.Y., Y.W., M.Y., and M.K. Analysis and interpretation of data: D.W., T.Y., M.M., and H.A. Drafting of the manuscript: D.W., T.Y., M.Y., and H.A. Critical revision of the manuscript for important intellectual content: D.W., M.M., and H.A. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Watanabe, D., Yoshida, T., Yamada, Y. et al. Combined use of two frailty tools in predicting mortality in older adults. Sci Rep 12, 15042 (2022). https://doi.org/10.1038/s41598-022-19148-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-19148-x
- Springer Nature Limited
This article is cited by
-
Dose-Response Relationships between Diet Quality and Mortality among Frail and Non-Frail Older Adults: A Population-Based Kyoto-Kameoka Prospective Cohort Study
The Journal of nutrition, health and aging (2023)