Abstract
This study aimed to identify the prevalence of sarcopenia, obesity, and sarcopenic obesity and examine their association with radiographic knee osteoarthritis (OA) and knee pain in Korean postmenopausal women. This cross-sectional study utilized the data from Korean National Health and Nutrition Examination Surveys 2009–2011. The participants were categorized into 4 groups based on body composition: either sarcopenic (appendicular skeletal muscle < 23%) or not, either obese (body mass index ≥ 25.0 kg/m2) or not. The prevalence of radiographic knee OA and knee pain was calculated. The effect of hormone replacement therapy (HRT) was also evaluated. The prevalence of radiographic knee OA, knee pain, and both were all highest in the sarcopenic obese group and lowest in the control group (61.49% vs. 41.54%, 39.11% vs. 27.55%, 32.04% vs. 17.82%, all p < 0.001). Without sarcopenia, obese women showed significantly higher ratio of radiographic knee OA only (57.64% vs. 41.54%, p < 0.001). With sarcopenia, the coexistence of obesity presented higher ratio of radiographic knee OA, knee pain, and both compared to sarcopenia without obesity (61.49% vs. 41.82%, 39.11% vs. 27.61%, 32.04% vs. 17.60%, all p < 0.001). The use of HRT for more than 1 year was not associated with radiographic knee OA, knee pain, or both (p = 0.147, 0.689 and 0.649, respectively). Obesity with sarcopenia had greater effect on knee OA compared to obesity without sarcopenia. Moreover, HRT use for more than 1 year was not associated with the prevalence of knee OA. Therefore, more efforts should focus on reducing body fat and increasing muscle in postmenopausal women with knee OA.
Similar content being viewed by others
Introduction
Osteoarthritis (OA) is a common disease in the elderly population, affecting approximately 27 million adults in the United States1. OA often requires surgical treatment owing to pain and mobility restriction, and the social cost is high due to high postoperative morbidity2. Therefore, it is important to clarify the pathophysiology and reduce risk factors. OA and its various risk factors have been extensively studied in the general elderly population; however, studies in postmenopausal women are limited.
Menopause is a life event that greatly affects women through hormonal changes. The most well-known menopausal symptoms include vasomotor symptoms including hot flushes, atrophic vaginitis, psychological symptoms including depression, and cardiovascular symptoms3. Furthermore, temporomandibular joint disease, osteoporosis, and sarcopenic obesity have a significantly higher incidence in women than in men, suggesting a relationship between female hormones and these musculoskeletal ailments4,5,6. In addition, a change in hormonal status, especially a decrease in sex hormone levels, alters the body composition7. A decrease in bone mass density leads to osteoporosis, and the decrease in muscle mass leads to sarcopenia increases8. All these changes lead to a restricted life in postmenopausal women9.
Therefore, it is necessary to examine the relationship between body composition and OA in postmenopausal women. Previous studies primarily focused on the association between obesity and OA. Furthermore, the research was conducted based on anthropometric measures such as weight and BMI. However, BMI does not reflect body composition as do body fat mass and muscle mass10,11. Sarcopenia, which is characterized by a decrease in muscle mass, is a part of normal aging process but it results in functional impairment12. In postmenopausal women, it is rather necessary to utilize objective measures for relatively low muscle mass to study sarcopenia and sarcopenic obesity in relation to OA13.
Because low muscle mass may be owing to a deprivation of sex hormone levels in postmenopausal women, estrogen supplementation or hormone replacement therapy (HRT) is used to relieve various symptoms and to protect muscle mass and muscle strength14,15; however, a few studies showed that HRT did not show positive effect on muscle mass16,17. Furthermore, the effect of HRT on knee OA is controversial; although some observational studies showed positive effect of HRT on knee OA18,19, others showed no association of sex hormone replacement or knee arthroplasty20.
Therefore, this study aimed to identify the prevalence of sarcopenia, obesity, and sarcopenic obesity and examine their association with knee OA in Korean postmenopausal women and also the effect of HRT using data obtained during the 2009–2011 Korean National Health and Nutrition Examination Surveys (KNHANES).
Methods
Study design and setting
This was a nationwide cross-sectional observational study. Data were extracted from the KNHANES conducted from 2009 to 201121. KNHANES is a national, population-based cross-sectional survey that collects data on the health and nutrition status of Koreans by sampling representative, noninstitutionalized Korean civilians. Every year, approximately 10,000 individuals were sampled. The survey is composed of health interviews, physical examinations, and nutrition surveys. All the components of the survey were conducted either at the mobile screening center or at the home of participants by trained medical staff, dieticians, health interviewers, and medical technicians. All participants provided written informed consent. The KNHANES were performed in accordance with the principles of the Declaration of Helsinki. For this study, we used the data from 2009 to 2011; the study was approved by the institutional review board of the Korea Centre for Disease Control and Prevention (2009-01CON-03-2C, 2010-02CON-21-C, 2011-02CON-06C).
Participants
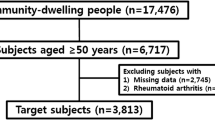
For KNHANES from 2009 to 2011, 28,009 individuals were enrolled. Of the participants, 4362 women answered as postmenopausal for the question about their menstruation status. We included only the participants who completed health interviews for sarcopenia, physical examination for BMI, knee joint radiography, and dual-energy X-ray absorptiometry (DXA). The exclusion criteria included diagnosis of surgical menopause, thyroid disease, end-stage renal disease, malignant tumor, or arthritis other than OA and missing variables for analysis. For sub-cohort analysis, we excluded women who did not respond to the questions regarding hormone replacement therapy (HRT). The participants were asked about the experience of HRT and the period of use in months. For this study, 4099 women were included in the final analysis. Among those who answered to have the history of HRT use, they were divided into the group who had used HRT for less than a year, whereas the other who had used it for longer than a year for sub-cohort analysis.
Definition of sarcopenia and obesity
Appendicular skeletal muscle (ASM) was defined as the sum of muscle mass in four limbs as measured by DXA (QDR 4500A; Hologic Inc., Bedford, MA). For the definition of sarcopenia, there is no single standardized diagnostic criterion. Based on a previous study that studied for sarcopenia and sarcopenic obesity using the KNHANES from 2010 to 2011, we used the value obtained by dividing ASM by body weight multiplied by 100 as the ASM index (%). Sarcopenia was defined as two standard deviations below the mean of the same gender, young standard group and the cutoff value was 23.0% for Korean women22. Obesity was defined as body mass index (BMI, kg/m2) more than or equal to 25.0 according to the guideline for the management of obesity in Korea23.
Measurements of variables
Current age, age at menarche and menopause, body mass index (BMI), past history of hypertension (HTN), diabetes mellitus (DM), osteoporosis, lifestyle such as alcohol consumption and smoking status, HRT, and lipid profile were considered as confounding variables.
All participants completed the physical examination and blood sampling either at the mobile screening center or at home. They wore light clothing without shoes while measuring the height, weight, and blood pressure. BMI was calculated from the measured height and weight. Blood sampling was done after overnight fasting of at least 8 h and the samples were analyzed on the same day (Neodin Medical Institute, Seoul, South Korea).
All participants completed the standardized questionnaire regarding their medical history and lifestyle. For medical history, prior to doctor’s diagnosis of HTN, DM, and osteoporosis were asked. For alcohol consumption, any previous experience was asked. A heavy drinker was defined as he/she who consumed more than 30 g of alcohol per day. For smoking, the participants were asked of any previous experience of smoking and the current status of smoking. Regular exercise was defined as walking for 30 min or more at a time, 5 days per week or more and muscle-strengthening exercise as anaerobic exercises such as push-ups, sit-ups, dumbbells, and barbells at least once a week. Regarding HRT, the history of drug use was asked. The duration was measured in months. If they had used HRT for less than a year, they were assigned to sub-cohort 1, and if they had used HRT for longer than a year, they were assigned to sub-cohort 2.
Knee radiography was performed for all participants and the results were analyzed based on the Kellgren-Lawrence (KL) Scale that assesses the severity of knee OA. A grade higher than or equal to 2 was considered as radiographic knee OA. In addition, knee pain was asked on the questionnaire as knee pain for 30 days over the previous 3 months.
Statistical analysis
Statistical analysis software (SAS) version 9.4 (SAS Inc., Cary, NC, USA) was used for all statistical analysis and the KNHANES data were analyzed according to the KNHANES data analysis guidelines. All analyses were two tailed, and a p-value of < 0·05 was considered significant.
Continuous variables were analyzed by one-way ANOVA considering the complex sample design to calculate the mean and standard errors (SE). Categorical variables were represented with raw percent with SEs and comparatively tested by Rao-Scott Chi-square test.
For the sub-cohort analysis, the participants were divided based on the period of HRT consumption. After adjusting for age and BMI, the continuous variable was represented with mean and SE, and analysis of covariance was applied to test statistical significance. The dichotomous variables were represented with ratio and standard deviation (SD), and logistic regression model was used to identify association.
Results
Subjects were divided into four groups based on their body composition: (1) control: did not meet the definition for obesity or sarcopenia; (2) sarcopenic: met definition for sarcopenia but not obesity; (3) obese: met definition for obesity but not sarcopenia; (4) sarcopenic obese: met definition for both sarcopenia and obesity.
Demographic characteristics of participants
From 2009 to 2011, 28,009 people participated in KNHANES, of which 4362 participants were postmenopausal. Our final cohort included 4150 subjects after excluding those who did not complete the survey. 1231 people were with normal body composition, 1379 were sarcopenic but not obese, 203 were obese but not sarcopenic, and 1337 were both sarcopenic and obese. The baseline characteristics of participants according to the body composition are presented in Table 1.
The mean age of the participants was 62.41 ± 0.25 years. The mean age at menopause and menarche was 48.40 ± 0.12 years and 13.96 ± 0.28 years, respectively. Only the mean age at menopause was significantly different among the groups (p = 0.012). The characteristics related to obesity such as weight, body mass index (BMI), and waist circumference, and ASM index presented significant difference among the four groups in the expected direction (p < 0.001).
For the past history, the prevalence of HTN and DM was significantly different among the four groups with the prevalence being the highest for the sarcopenic obese group for both HTN and DM (p < 0.001), while that of osteoporosis was not significantly different (p = 0.927).
In terms of lifestyle, smoking and alcohol consumption were not significantly different among the groups. The two obese groups tended to exercise regularly more than the non-obese women (p = 0.004). The previous use of HRT was not significantly different among the groups (p = 0.760).
Radiographic and clinical knee OA based on body composition
Table 2 shows the prevalence of radiographic knee OA and knee pain of the four groups. The ratio of radiographic knee OA, knee pain, and both radiographic knee OA and knee pain were analyzed. There was a significant difference among the four groups in all three variables (all p < 0.001).
Table 3 shows the p-value as a result of multiple groupwise comparisons among the four groups. Among the non-obese people, whether sarcopenic or non-sarcopenic did not show significant difference in the ratios of each and both radiographic OA and knee pain (p = 0.922, 0.981, and 0.932, respectively). Also, among the obese people, the ratios of each and both radiographic OA and knee pain did not show significant difference between the non-sarcopenic and the sarcopenic group (p = 0.467, 0.118, and 0.298, respectively).
However, among the people without sarcopenia, the obese people tended to show a higher ratio of radiographic OA significantly (57.64% vs. 41.54%, p < 0.001). Knee pain and both radiographic and clinical knee OA were not significantly different (p = 0.658 and 0.098, respectively). Finally, for people with sarcopenia, obesity increased the ratio of radiographic knee OA, knee pain, and both radiographic knee OA and knee pain. For radiographic knee OA, although the ratio was 41.82% for the sarcopenic group, that of the sarcopenic obese group was 61.49% (p < 0.001). The ratio of knee pain was also statistically different between the sarcopenic and sarcopenic obese groups (27.55% and 39.11%, respectively; p < 0.001). Lastly, the ratio of people with both radiographic knee OA and knee pain was 17.60% and 32.04% for sarcopenic and sarcopenic obese groups, respectively (p < 0.001).
Hormone replacement therapy
Based on the answers to the use of HRT in the questionnaire, a sub-cohort analysis was done. Among the postmenopausal women who had used HRT before, 240 women used HRT for less than a year, whereas the other 398 used it for longer than a year. In Table 4, the mean ASM index of these two groups did not show a significant difference (24.47% and 24.80%, respectively, p = 0.181). The ratio of sarcopenia showed no significant association with the duration of HRT use (69.80% and 62.11%, respectively, p = 0.147). For the radiographic knee OA, knee pain, and both radiographic knee OA and knee pain, none of the ratios were significant between the two groups (p = 0.688, 0.634, and 0.649, respectively).
Table 5 shows the results after adjustment for age and BMI. The average ASM index was not significantly different between the two groups (p = 0.119), which was similar to the result before the adjustment. Both the ratio of sarcopenia and radiographic OA did not show a significant difference between the two groups (p = 0.082 and p = 0.506, respectively).
Discussion
Menopause, which involves a drastic change in hormonal status and results in a decrease in sex hormone levels, has a great effect on bone mass density and body fat distribution7. A decrease in bone mass density can lead to osteoporosis, an increase in body fat to obesity, and a decrease in body muscle to sarcopenia, which are all closely related to knee OA in postmenopausal women. Additionally, HRT after menopause, which keeps the estradiol level enough to relieve menopausal symptoms, is considered to be helpful in preventing knee OA18.
Although the association between knee OA and anthropometric measures such as BMI and weight have been studied well, there are few studies regarding the association of body composition with knee OA in literature. However, the results of the studies were not in the same trend because of their different study design, participants, measurement of body composition, and definition of obesity13,24,25,26. The longitudinal study conducted by Misra et al. showed that the risk of knee OA was increased in sarcopenic obese people, especially in women with statistical significance26. However, another study showed that body weight and BMI were more important factors associated with knee OA compared to body composition such as fat distribution or muscle mass as measured by DXA13. In a study by Suh et al. that also utilized data from KNHANES, obese people with low muscle mass, who were sarcopenic obese, presented greater odds of radiographic knee OA compared to the non-sarcopenic non-obese people, whereas obese people without low muscle mass showed no increased odds25.
This is the first cross-sectional study with a large number to present the association between knee OA and body composition acquired with DXA such as sarcopenia and sarcopenic obesity. Based on the body composition analyzed with DXA, the participants were categorized into four categories. For people without sarcopenia, the status of obesity only affected the prevalence of radiographic knee OA. However, for people with sarcopenia, the status of obesity affected the prevalence of not only radiographic knee OA but also knee pain. This emphasizes the fact that obesity may have more effect only when sarcopenia coexists, suggesting that the risk of knee OA in postmenopausal women is through both high fat mass and low muscle mass, not just one. The contrasting results of a previous study by Misra et al. can be explained by the fact that Misra et al. included both sexes in their study, whereas we analyzed only postmenopausal women26.
Aging causes many changes in body composition. Usually, muscle mass and bone mass decrease and fat mass increases. The increased fat mass infiltrates into muscle and bone. This can be observed more clearly in postmenopausal women, especially as central obesity increases as estrogen decreases. Central obesity also means an increase in visceral fat8,27,28. As aging progresses, osteoporosis, sarcopenia, and obesity increase all together. As a result, the quality of life of postmenopausal women or mortality increases29. Previous literature has shown that sarcopenia is more prevalent in older women with OA30. According to one review, these two diseases are closely related in both clinical and cellular ways31. Clinically, lower limb muscle weakness can lead to OA, and conversely. Poor muscle quality and low lean body mass mechanically contribute to the pathogenesis of OA and, the walking speed, one of the functional diagnostic criteria for sarcopenia, is slower in the OA group32,33. In cellular pathway, chondrocytes and skeletal muscle cells share common pathological pathway, thus, muscle mass in most OA patients is reduced31. Therefore, it can be considered that not simply the increase in fat mass, but the decrease in muscle mass accompanying the increase in fat mass has a significant effect on knee OA.
HRT is used by postmenopausal women to relieve various menopausal symptoms such as hot flushes. HRT affects not only the vasomotor symptoms but also the prevalence of OA19. Cirillo et al. showed that neither estrogen replacement nor estrogen plus progestogen therapy affected the need for knee joint replacement34. Our study also included a sub-cohort analysis to see the long-term effect of HRT and we divided the participants based on the use of HRT for longer than a year35. Different from the studies that presented that HRT relieved both the prevalence of radiographic knee OA and knee pain, our results showed no statistical significance in comparison based on HRT36,37. Confounding factors such as duration, dose, type of HRT used, lifestyle, and daily activity could explain the discordant results.
This study has some strengths. First, this study utilized the standardized nationwide data with a great number of participants. Second, to see the effect of sarcopenia and obesity in relation to each other, we categorized the participants into four groups and performed group-to-group multiple comparisons. Third, considering the specificity of the participants, we also conducted a sub-cohort analysis to see the effects of HRT on both clinical and radiological knee OA.
However, this study has several limitations. First, the results of this comparative, cross-sectional study design cannot be interpreted as a causal relationship between body composition and knee OA. Second, the variables obtained by self-questionnaire are subject to information bias or recall bias. Third, sarcopenia was only defined with the low muscle mass. Although sarcopenia is now diagnosed with many functional values such as hand grip strength or physical performance, this study only utilized the muscle quantity. Because this study was planned before the consensus about the sarcopenia diagnosis and KNHANES only contained the data about muscle mass, further study with muscle quality should better support this result. Fourth, the type of HRT was not analyzed due to the lack of data. Further prospective studies with a large number of subjects are required for a more detailed explanation regarding the relationship between sarcopenic obesity and knee OA.
In conclusion, obesity in terms of sarcopenia has greater effect on knee OA compared to obesity without sarcopenia. Moreover, HRT use of longer than a year is not associated with the prevalence of knee OA. Therefore, in knee OA, more preventive efforts should focus on reducing body fat and increasing muscle in postmenopausal women.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Lawrence, R. C. et al. Estimates of the prevalence of arthritis and other rheumatic conditions in the United States. Part II. Arthritis Rheum. 58, 26–35. https://doi.org/10.1002/art.23176 (2008).
Singh, J. A., Kwoh, C. K., Richardson, D., Chen, W. & Ibrahim, S. A. Sex and surgical outcomes and mortality after primary total knee arthroplasty: A risk-adjusted analysis. Arthritis Care Res. (Hoboken) 65, 1095–1102. https://doi.org/10.1002/acr.21953 (2013).
Nelson, H. D. Menopause. Lancet 371, 760–770. https://doi.org/10.1016/S0140-6736(08)60346-3 (2008).
Abellan van Kan, G. Epidemiology and consequences of sarcopenia. J. Nutr. Health Aging. 13, 708–712. https://doi.org/10.1007/s12603-009-0201-z (2009).
Bagis, B., Ayaz, E. A., Turgut, S., Durkan, R. & Ozcan, M. Gender difference in prevalence of signs and symptoms of temporomandibular joint disorders: A retrospective study on 243 consecutive patients. Int. J. Med. Sci. 9, 539–544. https://doi.org/10.7150/ijms.4474 (2012).
O’Connor, M. I. Sex differences in osteoarthritis of the hip and knee. J. Am. Acad. Orthop. Surg. 15(Suppl 1), S22-25 (2007).
Carr, M. C. The emergence of the metabolic syndrome with menopause. J. Clin. Endocrinol. Metab. 88, 2404–2411. https://doi.org/10.1210/jc.2003-030242 (2003).
Cruz-Jentoft, A. J. et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 39, 412–423. https://doi.org/10.1093/ageing/afq034 (2010).
Riis, B. J., Hansen, M. A., Jensen, A. M., Overgaard, K. & Christiansen, C. Low bone mass and fast rate of bone loss at menopause: equal risk factors for future fracture: A 15-year follow-up study. Bone 19, 9–12. https://doi.org/10.1016/8756-3282(96)00102-0 (1996).
Felson, D. T., Anderson, J. J., Naimark, A., Walker, A. M. & Meenan, R. F. Obesity and knee osteoarthritis. The Framingham Study. Ann. Intern. Med. 109, 18–24. https://doi.org/10.7326/0003-4819-109-1-18 (1988).
Grotle, M., Hagen, K. B., Natvig, B., Dahl, F. A. & Kvien, T. K. Obesity and osteoarthritis in knee, hip and/or hand: An epidemiological study in the general population with 10 years follow-up. BMC Musculoskelet. Disord. 9, 132. https://doi.org/10.1186/1471-2474-9-132 (2008).
Janssen, I., Heymsfield, S. B. & Ross, R. Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J. Am. Geriatr. Soc. 50, 889–896. https://doi.org/10.1046/j.1532-5415.2002.50216.x (2002).
Abbate, L. M. et al. Anthropometric measures, body composition, body fat distribution, and knee osteoarthritis in women. Obesity (Silver Spring) 14, 1274–1281. https://doi.org/10.1038/oby.2006.145 (2006).
Chen, Z. et al. Postmenopausal hormone therapy and body composition—A substudy of the estrogen plus progestin trial of the Women’s Health Initiative. Am. J. Clin. Nutr. 82, 651–656. https://doi.org/10.1093/ajcn.82.3.651 (2005).
Kim, S. W. & Kim, R. The association between hormone therapy and sarcopenia in postmenopausal women: The Korea National Health and Nutrition Examination Survey, 2008–2011. Menopause 27, 506–511. https://doi.org/10.1097/GME.0000000000001509 (2020).
Hansen, R. D., Raja, C., Baber, R. J., Lieberman, D. & Allen, B. J. Effects of 20-mg oestradiol implant therapy on bone mineral density, fat distribution and muscle mass in postmenopausal women. Acta Diabetol. 40(Suppl 1), S191-195. https://doi.org/10.1007/s00592-003-0063-5 (2003).
Kenny, A. M., Dawson, L., Kleppinger, A., Iannuzzi-Sucich, M. & Judge, J. O. Prevalence of sarcopenia and predictors of skeletal muscle mass in nonobese women who are long-term users of estrogen-replacement therapy. J. Gerontol. A Biol. Sci. Med. Sci. 58, M436-440. https://doi.org/10.1093/gerona/58.5.m436 (2003).
Jung, J. H. et al. Knee osteoarthritis and menopausal hormone therapy in postmenopausal women: A nationwide cross-sectional study. Menopause 26, 598–602. https://doi.org/10.1097/GME.0000000000001280 (2018).
Spector, T. D., Nandra, D., Hart, D. J. & Doyle, D. V. Is hormone replacement therapy protective for hand and knee osteoarthritis in women? The Chingford Study. Ann. Rheum. Dis. 56, 432–434. https://doi.org/10.1136/ard.56.7.432 (1997).
Hussain, S. M. et al. Incidence of total knee and hip replacement for osteoarthritis in relation to circulating sex steroid hormone concentrations in women. Arthritis Rheumatol. 66, 2144–2151. https://doi.org/10.1002/art.38651 (2014).
Kweon, S. et al. Data resource profile: The Korea National Health and Nutrition Examination Survey (KNHANES). Int. J. Epidemiol. 43, 69–77. https://doi.org/10.1093/ije/dyt228 (2014).
Kim, Y. S. et al. Prevalence of sarcopenia and sarcopenic obesity in the Korean population based on the Fourth Korean National Health and Nutritional Examination Surveys. J. Gerontol. A Biol. Sci. Med. Sci. 67, 1107–1113. https://doi.org/10.1093/gerona/gls071 (2012).
Seo, M. H. et al. 2018 Korean Society for the study of obesity guideline for the management of obesity in Korea. J. Obes. Metab. Syndr. 28, 40–45. https://doi.org/10.7570/jomes.2019.28.1.40 (2019).
Lee, S., Kim, T. N. & Kim, S. H. Sarcopenic obesity is more closely associated with knee osteoarthritis than is nonsarcopenic obesity: A cross-sectional study. Arthritis Rheum. 64, 3947–3954. https://doi.org/10.1002/art.37696 (2012).
Suh, D. H. et al. Body composition is more closely related to the development of knee osteoarthritis in women than men: A cross-sectional study using the Fifth Korea National Health and Nutrition Examination Survey (KNHANES V-1, 2). Osteoarthritis Cartilage 24, 605–611. https://doi.org/10.1016/j.joca.2015.10.011 (2016).
Misra, D. et al. Risk of knee osteoarthritis with obesity, sarcopenic obesity, and sarcopenia. Arthritis Rheumatol. 71, 232–237. https://doi.org/10.1002/art.40692 (2019).
Matkovic, V. et al. Timing of peak bone mass in Caucasian females and its implication for the prevention of osteoporosis Inference from a cross-sectional model. J. Clin. Invest. 93, 799–808. https://doi.org/10.1172/JCI117034 (1994).
Kelly, T. L., Wilson, K. E. & Heymsfield, S. B. Dual energy X-ray absorptiometry body composition reference values from NHANES. PLoS ONE 4, e7038. https://doi.org/10.1371/journal.pone.0007038 (2009).
Ilich, J. Z. et al. Interrelationship among muscle, fat, and bone: Connecting the dots on cellular, hormonal, and whole body levels. Ageing Res. Rev. 15, 51–60. https://doi.org/10.1016/j.arr.2014.02.007 (2014).
Kemmler, W. et al. Prevalence of sarcopenia in Germany and the corresponding effect of osteoarthritis in females 70 years and older living in the community: Results of the FORMoSA study. Clin. Interv. Aging 10, 1565–1573. https://doi.org/10.2147/CIA.S89585 (2015).
De Ceuninck, F., Fradin, A. & Pastoureau, P. Bearing arms against osteoarthritis and sarcopenia: When cartilage and skeletal muscle find common interest in talking together. Drug Discov. Today 19, 305–311. https://doi.org/10.1016/j.drudis.2013.08.004 (2014).
Conroy, M. B. et al. Muscle strength, mass, and quality in older men and women with knee osteoarthritis. Arthritis Care Res. (Hoboken) 64, 15–21. https://doi.org/10.1002/acr.20588 (2012).
Toda, Y., Segal, N., Toda, T., Kato, A. & Toda, F. A decline in lower extremity lean body mass per body weight is characteristic of women with early phase osteoarthritis of the knee. J. Rheumatol. 27, 2449–2454 (2000).
Cirillo, D. J., Wallace, R. B., Wu, L. & Yood, R. A. Effect of hormone therapy on risk of hip and knee joint replacement in the Women’s Health Initiative. Arthritis Rheum. 54, 3194–3204. https://doi.org/10.1002/art.22138 (2006).
Marjoribanks, J., Farquhar, C., Roberts, H., Lethaby, A. & Lee, J. Long-term hormone therapy for perimenopausal and postmenopausal women. Cochrane Database Syst. Rev. 1, CD004143. https://doi.org/10.1002/14651858.CD004143.pub5 (2017).
Dawson-Basoa, M. E. & Gintzler, A. R. Estrogen and progesterone activate spinal kappa-opiate receptor analgesic mechanisms. Pain 64, 608–615. https://doi.org/10.1016/0304-3959(96)87175-2 (1996).
Smith, Y. R. et al. Pronociceptive and antinociceptive effects of estradiol through endogenous opioid neurotransmission in women. J. Neurosci. 26, 5777–5785. https://doi.org/10.1523/JNEUROSCI.5223-05.2006 (2006).
Acknowledgements
We would like to thank members of the Department of Obstetrics and Gynecology, Yonsei University College of Medicine for their generous support of this research.
Author information
Authors and Affiliations
Contributions
H.I.K.: conceptualization, methodology and investigation, writing-original draft preparation, visualization; S.H.A.: methodology and investigation, visualization; Y.K.: formal analysis, data curation; J.E.L.: formal analysis, data curation; E.C.: revision, data curation; S.S.K.: conceptualization, supervision, project administration.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, H.I., Ahn, S.H., Kim, Y. et al. Effects of sarcopenia and sarcopenic obesity on joint pain and degenerative osteoarthritis in postmenopausal women. Sci Rep 12, 13543 (2022). https://doi.org/10.1038/s41598-022-17451-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-17451-1
- Springer Nature Limited
This article is cited by
-
Infrapatellar fat pad size and subcutaneous fat in knee osteoarthritis radiographic progression: data from the osteoarthritis initiative
Arthritis Research & Therapy (2024)
-
The role of obesity and adipose tissue dysfunction in osteoarthritis pain
Nature Reviews Rheumatology (2024)
-
Association between sarcopenia and osteoarthritis among the US adults: a cross-sectional study
Scientific Reports (2024)