Abstract
Successful weaning from ventilators not only improves the quality of life of patients, but also reduces medical expenses. The aim of this study was to explore the association between nutritional provision and successful ventilator weaning. In this retrospective study data from the Respiratory Care Center of Chung Shan Medical University Hospital between October, 2017 and July, 2019 on patient characteristics, amount of nutrition delivered, and clinical outcomes were retrieved. A total of 280 ventilated patients were enrolled and divided into successful extubation and failed weaning groups. There were 178 males (63.6%) and 102 females (36.4%) with a mean age of 67.3 ± 16.9 years. The successful extubation group consisted of patients who tended towards ideal body weight during the weaning process (BMI 23.9 ± 5.0 versus 22.7 ± 4.8 kg/m2, p < 0.001). Patients from both groups initially received the same nutritional intervention, while patients of successful extubation received significantly more calories and protein after weaning (23.8 ± 7.8 kcal versus 27.8 ± 9.1 kcal, p < 0.001 and 0.97 ± 0.36 g versus 1.14 ± 0.42 g, p < 0.001). Successful weaning was associated with higher survival rate (p = 0.016), shortened hospital stay (p = 0.001), and reduced medical costs (p < 0.001). Overall, nutritional support with high calories and protein was associated with the probability of successful ventilator weaning in patients undergoing prolonged mechanical ventilation. Adequate nutrition is a determinant of successful ventilator weaning.
Similar content being viewed by others
Introduction
Previous studies have demonstrated that several factors are independently associated with extubation success, such as age, Glasgow coma score (GCS)1, and swallowing attempts2. Factors that can lead to failed weaning include increased respiratory load, timing of tracheotomy, and decreased neuromuscular competence3,4. From the results of the Large observational study to UNderstand the Global impact of Severe Acute respiratory FailurE (LUNG SAFE) and WorldwidE AssessmeNt of Separation of pAtients From Ventilatory assistancE (WEAN SAFE) studies, potential independent predictors of discontinuation or withdrawal of mechanical ventilation (MV) are: patient characteristics (age5,6,7,8,9, body mass index (BMI)10, geo-economic area11), comorbidities5,6,7,9,10,12, in-hospital treatment5, and severity of illness5,6,7,8. Successful ventilator weaning not only improves the quality of life of patients, but also reduces medical expenses.
Adequate nutritional provision is important for survival and shortens discharge time in the critically ill population. Recently, several global nutritional guidelines for critically ill patients have been published to inform practitioners of the best evidence-based therapies. The American Society for Parenteral and Enteral Nutrition (ASPEN) and the Society of Critical Care Medicine (SCCM) guidelines include energy requirements of 25–30 kcal/kg/day and protein requirements of 1.2–2.0 g/kg/day13. The European Society for Parenteral and Enteral Nutrition (ESPEN) guidelines are for 20–25 kcal/kg/day and 1.3 g/kg protein equivalents per day14. Achieving at least 80% of the prescribed protein intake is optimal15. In contrast, a research study has shown that caloric intake/target of more than 64.6% in an intensive care unit (ICU) for 7 days is associated with significantly higher mortality, ICU-acquired infections16,17,18,19,20,21, duration of MV, and length of stay (LOS) in hospital22. Underfeeding and overfeeding may increase the risk of infection of ventilated patients23 and prolong ventilator weaning time24. Therefore, nutrition intervention plays a key role in critical care.
information systems can assist decision-makers in improving performance and patient care, with which through integrating business intelligence (BI) and hospital information systems real-time big data analytics is possible. In the present study, we developed predictive models of ventilator weaning using BI system and large datasets in a medical university hospital respiratory care center (RCC). The aim of this study is the monitoring of ventilated patient nutritional status to determine its association with successful ventilator weaning.
Materials and methods
Establishment of the BI system
Since 2005, our hospital has applied BI to the evaluation of big data to understand the outcomes of medical treatments and to perform real-time monitoring. As of July 2019, 28 items have been completed, including medical management, quality control, response to overall operating conditions, and timely warning messages to facilitate preventive measures.
This is a retrospective analysis of existing data from the Healthcare/Hospital Information System (HIS) of Chung Shan Medical University Hospital (CSMUH). This study integrated several units, such as the information center, RCC, and departments of management and nutrition. As a first step, the department of management of CSMUH was informed of the indicators and purposes of nutritional analysis for ventilator weaning. Following discussions with the information center, and according to the studied indicators, the SharePoint platform of HIS was automatically uploaded. For the second step, we worked with nutrition department staff to write programs to classify data and map comparison charts for simple and easy presentation of results, applying BI to real-time monitoring of ventilated patient nutritional status and collecting anthropometric measurements, food-related history, biochemical data, and patient history. For the third step, a hospital-wide campaign was conducted to promote this system. After establishment of the BI system and simplification of the analytical process, we explored the indicators and predictive models of successful weaning.
Study population and setting
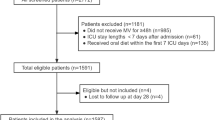
This observational cohort study was conducted to determine whether nutritional intake or other indicators are associated with successful extubation (Fig. 1). Participants had transferred to RCC and were studied from the time of ventilator-free protocol through the end of the weaning program at CSMUH from October 2017 to July 2019. Subjects were critically ill patients who were stable with prolonged MV-dependence (more than 21 days). The ventilator weaning protocol of CSMUH involves daily screening, followed by weaning parameter evaluation and process. Finally, T piece or continuous positive airway pressure (CPAP) is applied to achieve extubation (Supplemental Fig. 1). We recorded variables related to the use of BI during ventilator weaning. Patients in both groups received enteral nutrition (EN) support within 24 h, following assessment by a dietician. EN involved intermittent bag feeding with 5 meals per day. The total daily energy expenditure was estimated by a dietitian using the Harris-Benedict equation and adjusted for stress/active factors. Protein requirement was calculated as 0.9–1.5 g/kg based on patient condition and underlying diseases. Enteral feeding was suspended only if there were absolute contraindications, such as intestinal obstruction or hemodynamic instability25. Subjects were divided into successful extubation and failed weaning groups according to their actual status during the post-weaning period. Their basic information, nutritional intakes, laboratory data, and clinical outcomes were compared before admission to RCC and after transfer from RCC. Successful weaning was defined as removal of endotracheal tube and use of T-piece ventilation or CPAP26. Informed consent was waived by CSMUH for research projects in 2020 (CSH-2020-A-014) conducted according to the guidelines of the Declaration of Helsinki, with minimal risk to participants and approval from the Institutional Review Board (IRB) of CSMUH (IRB No. CS2-19144).
Primary and secondary outcomes
We collected data on patient characteristics, nutritional intakes, and outcomes via BI system. Personal basic data, laboratory values during the experimental period, and nutritional data including types and amounts of nutrition prescribed and delivered (both calories and protein) were recorded during RCC stay. The primary outcomes of this study were the nutrition received during the optimal ventilator weaning program. Secondary outcomes included in-hospital mortality, medical costs, acute physiology and chronic health evaluation II (APACHE II) score, overall hospital LOS, and RCC LOS. We determined several predictors of successful extubation and survival.
Statistical analysis
Normally distributed continuous variables are presented as means ± standard deviation (SD), while categorical variables are presented as numbers and proportions. National Health Insurance (NHI) premium and laboratory data are skewed and described using medians and interquartile ranges (IQRs). For hospital cost and biochemical data in non-normal distribution, we performed Mann–Whitney U test to compare differences between the groups. Two-sided p values of < 0.05 were considered significant. The Pearson chi-square test was used for categorical variables and the independent t test for continuous variables. The p values are from paired t test of continuous variables for within-group comparisons. Propensity score matching27,28,29,30,31,32,33,34 was based on gender, age, height, disease categories, initial weight, initial BMI, initial energy delivery, and initial protein intake. The propensity score was a probability that was estimated based on logistic regression. The binary variable was successful extubation and failed weaning. Every subject would create a propensity score between zero to one. Successful extubation group was matched to failed weaning group via 8-digit decimal point match of the propensity score. In the case of no match, 7-digit decimal point match was attempted by using nearest neighbor matching. The algorithm was allowed to proceed until no further matches could be made35. Survival was compared using log-rank tests and presented as Kaplan–Meier curves. We used post-hoc analysis to estimate the statistical power. Effect size was 0.26, alpha error was 0.05, group number was 140, and post-hoc power was 0.63. All analyses were performed using PASW Statistics 18, version 18.0.0 (formerly SPSS Statistics).
Results
As shown in Fig. 1, a total of 326 ventilator-dependent patients were admitted to RCC and assessed for eligibility during the study period. Four patients were excluded, 2 due to missing EN data, 1 due to family’s refusal of treatment by a specialist physician, and 1 due to refractory transfer to ICU within the same hospitalization. Finally, 322 patients were enrolled in this study. Each group consisted of 161 patients. By matching the propensity score, a better balance in the heterogeneity between groups was achieved35. Finally, each group consisted of at least 140 patients. The parameters mentioned above were analyzed before and after the weaning process. Baseline characteristics of patients are shown in Table 1. There were no baseline differences in age, height, gender, BMI, or nutritional provision (both daily caloric and total protein intakes). Moreover, most of the laboratory data did not differ at baseline. Notable exceptions were significantly higher hemoglobin and phosphorus and lower blood urea nitrogen (BUN) and C-reactive protein (CRP).
Identifying at risk populations
The underlying diseases of ventilated patients were identified. There were significant differences in the successful extubation group versus the failed weaning group in terms of subspecialty (p = 0.031). Successful extubation group was mostly made up of surgical patients (50.7%) while failed weaning group was mostly made up of non-surgical patients (56.4%). Furthermore, a higher proportion of patients in the successful extubation group had neurological problems (45.7% vs 35.7%). There was a higher percentage of cancer patients in the failed weaning group (14.3% vs 3.6%), even though there were no baseline differences in cancer type36,37,38, nutritional status, or nutritional provision (data not shown).
Primary outcome analysis
Initially, nutrition intervention was the same for successful extubation and failed weaning groups (Table 1, 23.8 ± 7.8 vs 24.5 ± 7.9 kcal/kg/day, p = 0.092 and 0.97 ± 0.36 vs 1.01 ± 0.37 g/kg/day, p = 0.096). However, during ventilator weaning, the successful extubation group received more calories and protein (Table 2, 23.8 ± 7.8 vs 27.8 ± 9.1 kcal/kg/day, p < 0.001 and 0.97 ± 0.36 vs 1.14 ± 0.42 g/kg/day, p < 0.001). There were no significant differences in caloric intake during weaning (Table 2, 24.5 ± 7.9 vs 25.6 ± 7.5 kcal/kg/day, p = 0.051 and 1.01 ± 0.37 vs 1.03 ± 0.36 g/kg/day, p = 0.348) or post-weaning (Table 3, 27.8 ± 9.1 vs 25.6 ± 7.5 kcal/kg/day, p = 0.199). After matching the propensity score, initial body weight of the successful extubation group did not significantly differ from that of the failed weaning group (Table 1, 63.2 ± 14.7 vs 60.0 ± 12.2 kg, p = 0.26). During the ventilator weaning process, the successful extubation group lost a significant amount of body weight. No body weight change was observed in the failed weaning group (Table 2, 63.2 ± 14.7 vs 59.5 ± 14.5 kg, p < 0.001 and 60.6 ± 12.2 vs 60.2 ± 11.6 kg, p = 0.284). In the post-weaning phase, there were no significant differences between the groups (Table 3, 59.9 ± 14.5 vs 60.2 ± 11.6 kg, p = 0.665).
Only the successful extubation group demonstrated significantly reduced APACHE II scores during the weaning process (Table 2, from 18.3 ± 3.6 to 10.1 ± 6.8, p < 0.001), with no change in disease severity in the failed weaning group (Table 2, from 19.9 ± 4.6 to 20.6 ± 7.8, p = 0.436). Similar findings for serum albumin and CRP were observed (Table 2). Serum phosphorus levels significantly differed at baseline. However, there were no differences in serum phosphorus levels within groups (p = 0.078 and 0.309) or between groups (p = 0.954) at the end of the study period. There were significant differences in BUN at baseline and at the end of the study period (p = 0.011 and 0.027), but not during the weaning period (p = 0.369 and 0.747).
Secondary outcomes and clinical benefits
The survival rate of the successful extubation group was significantly higher than that of the failed weaning group (Fig. 2, p = 0.016). As shown in Table 3, the successful extubation group had a mortality rate of 12.1% and the failed weaning group had a mortality rate of 25.7%. Furthermore, RCC LOS (Table 3, 19.9 ± 10.0 vs 28.5 ± 14.5 days, p < 0.001) and hospital LOS (Table 3, 48.3 ± 19.5 vs 56.3 ± 26.9 days, p = 0.001) were reduced. In the successful extubation group, medical costs were reduced by $5,475 per person on average when compared with the failed weaning group (Table 3, p < 0.001).
Discussion
In this study we found that more near the target caloric intake, and protein delivery above 1.2 g/kg/day can improve nutrition for successful ventilator weaning. Optimizing nutrition for critically ill patients can improve their clinical outcomes39,40,41. ASPEN and SCCM guidelines include weight-based equations of 25–30 kcal/kg/day and recommended protein intakes of at least 1.2 g/kg/d13. This is consistent with our experimental results, which showed that reducing caloric and protein deficits is associated with successful ventilator weaning and significantly lower mortality (Fig. 2). In the FEED Trial, targeted energy and protein delivery were associated with attenuation of muscle loss and malnutrition at ICU discharge42. Higher caloric and protein deficits in the surgical intensive care unit are associated with lower discharge rates43. There is a significant and positive association between nutritional adequacy and 6-month survival in patients with higher Nutrition Risk in Critically ill (NUTRIC) score44.
According to the literature, patients with COPD or postoperative neuromuscular disease are at high risk of developing ventilator dependence45. A weaning protocol that combines respiratory parameters with neurologic measures leads to superior outcomes46. We identified the population with a high weaning success rate, i.e., neurosurgical patients with the capacity to undergo aggressive extubation therapy. However, poor outcomes and extubation failure have been demonstrated in medical patients who are elderly and have underlying chronic cardiac47,48,49,–50 or respiratory disease9, which is consistent with our results. Similarly, a previous study did not show an improvement in the rates of successful ventilator weaning among cancer patients after the implementation of a resource-intensive weaning program51. It has also been demonstrated that APACHE II score is useful for predicting the outcome of weaning in ventilator patients52, consistent with our findings.
Intensive care unit-acquired weakness (ICU-AW) is a common complication with a clinically relevant impact on short- and long-term outcomes53. Initial body weight is a potential factor. Being mildly overweight is associated with successful weaning. Previous research has demonstrated that macronutrient deficit in the surgical intensive care unit is associated with worse in-hospital outcomes and lower rates of home discharge43, which is in line with the results of this study. Also consistent with our findings, correcting the serum phosphorus level has no effect on clinical outcome54 while increasing the hemoglobin level is positively associated with preferable weaning outcomes55. In this study, the hemoglobin level56 of the successful extubation group was higher than 10 g/dL57. Hyperinflammation induces elevated CRP level-related failure of weaning58. As shown on subgroup analysis in this study, this condition was more significant in the surgical patients than in the medical patients (Supplementary Table 1). Further studies are needed to clarify these results.
Of clinical relevance is that enteral feeding intolerance in mechanically ventilated critically ill patients is associated with malnutrition, fewer ventilator-free days (VFDs), longer LOS, and increased mortality40. From clinical outcomes (successful or failed weaning), we identified and assessed the influence of nutritional intervention. Recent guidelines have recommended the use of standardized protocols to reduce weaning duration and ICU LOS59. This study was based on our weaning practice. Higher caloric intake compared to lower caloric intake modifies the outcome and more protein delivery is recommended for nutritional support during ventilator weaning. We suggest 25–30 kcal/kg/day with > 1.2 g/kg protein for a better outcome.
In recent decades, there has been a growing body of research on artificial intelligence (AI) for precise diagnostics60. Various technical applications have been intensively researched to improve the accuracy of AI-facilitated diagnoses61. Moreover, through BI, deep learning has led to the development of predictive models based on large datasets62. The application of BI system to real-time monitoring of nutritional support provides more sophisticated information for developing ventilator weaning strategies. In addition, interactive visualization capabilities improve overall respiratory therapies and enhance efficiency.
As this was a retrospective observational study, there were some limitations. First of all, some baseline laboratory values differed between groups, including albumin, hemoglobin, phosphorus, BUN, and CRP. A downside of this study is that we did not collect data on the tracheostomy rate. However, the tracheostomy rate tends to be low in Taiwan due mainly to cultural factors, even though the “shared decision-making”63 protocol has been implemented. Second, we focused only on the ventilator weaning period during RCC stay, for which comprehensive data from admission, ICU, to post-acute care may augment our findings. Furthermore, as data on comorbidities were not collected, we were unable to explore their effects on the weaning process. Moreover, the number of cases was relatively small and the cases were localized. In future studies, data from multiple medical centers64,65 should be linked to validate the findings. That said, findings of this study revealed that the use of AI can greatly contribute to clinical medicine.
Conclusions
Delivery of proteins and calories around the target calories intake allowed for preferable weaning outcomes in patients undergoing prolonged mechnical ventilation.
Data availability
The data sets generated and analyzed during the current study are available from the corresponding author upon reasonable request.
References
Thille, A. W., Richard, J. C. & Brochard, L. The decision to extubate in the intensive care unit. Am. J. Respir. Crit. Care Med. 187, 1294–1302. https://doi.org/10.1164/rccm.201208-1523CI (2013).
Asehnoune, K. et al. Extubation success prediction in a multicentric cohort of patients with severe brain injury. Anesthesiology 127, 338–346. https://doi.org/10.1097/aln.0000000000001725 (2017).
Alía, I. & Esteban, A. Weaning from mechanical ventilation. Crit. Care 4, 72–80. https://doi.org/10.1186/cc660 (2000).
MacIntyre, N. R. et al. Evidence-based guidelines for weaning and discontinuing ventilatory support: A collective task force facilitated by the American College of Chest Physicians; the American Association for Respiratory Care; and the American College of Critical Care Medicine. Chest 120, 375s–395s. https://doi.org/10.1378/chest.120.6_suppl.375s (2001).
Bellani, G. et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA 315, 788–800. https://doi.org/10.1001/jama.2016.0291 (2016).
Laffey, J. G. et al. Potentially modifiable factors contributing to outcome from acute respiratory distress syndrome: The LUNG SAFE study. Intensive Care Med. 42, 1865–1876. https://doi.org/10.1007/s00134-016-4571-5 (2016).
Dumas, G. et al. Survival in immunocompromised patients ultimately requiring invasive mechanical ventilation: A pooled individual patient data analysis. Am. J. Respir. Crit. Care Med. 204, 187–196. https://doi.org/10.1164/rccm.202009-3575OC (2021).
Béduneau, G. et al. Epidemiology of weaning outcome according to a new definition. The WIND study. Am. J. Respir. Crit. Care Med. 195, 772–783. https://doi.org/10.1164/rccm.201602-0320OC (2017).
Thille, A. W., Harrois, A., Schortgen, F., Brun-Buisson, C. & Brochard, L. Outcomes of extubation failure in medical intensive care unit patients. Crit. Care Med. 39, 2612–2618. https://doi.org/10.1097/CCM.0b013e3182282a5a (2011).
Cortegiani, A. et al. Immunocompromised patients with acute respiratory distress syndrome: Secondary analysis of the LUNG SAFE database. Crit. Care 22, 157. https://doi.org/10.1186/s13054-018-2079-9 (2018).
Laffey, J. G. et al. Geo-economic variations in epidemiology, patterns of care, and outcomes in patients with acute respiratory distress syndrome: Insights from the LUNG SAFE prospective cohort study. Lancet Respir. Med. 5, 627–638. https://doi.org/10.1016/s2213-2600(17)30213-8 (2017).
Boyle, A. J. et al. Identifying associations between diabetes and acute respiratory distress syndrome in patients with acute hypoxemic respiratory failure: An analysis of the LUNG SAFE database. Crit. Care 22, 268. https://doi.org/10.1186/s13054-018-2158-y (2018).
McClave, S. A. et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N). J. Parenteral Enteral Nutr. 40, 159–211. https://doi.org/10.1177/0148607115621863 (2016).
Singer, P. et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin. Nutr. 38, 48–79. https://doi.org/10.1016/j.clnu.2018.08.037 (2019).
Nicolo, M., Heyland, D. K., Chittams, J., Sammarco, T. & Compher, C. Clinical outcomes related to protein delivery in a critically ill population: A multicenter, multinational observation study. J. Parenteral Enteral Nutr. 40, 45–51. https://doi.org/10.1177/0148607115583675 (2016).
Ma, K. S., et al. Safety and Seroconversion of Immunotherapies against SARS-CoV-2 Infection: A Systematic Review and Meta-Analysis of Clinical Trials. Pathogens. 10(12), 1537. https://doi.org/10.3390/pathogens10121537 (2021).
Kuo, C. F., et al. Discordance of vancomycin minimum inhibitory concentration for methicillin-resistant Staphylococcus aureus at 2 μg/mL between Vitek II, E-test, and Broth Microdilution. PeerJ. 8, e8963. https://doi.org/10.7717/peerj.8963 (2020).
Chiang, C. H., et al. Prevalence of Nontuberculous Mycobacterium Infections versus Tuberculosis among Autopsied HIV Patients in Sub-Saharan Africa: A Systematic Review and Meta-Analysis. Am. J. Trop. Med. Hyg. 104(2), 628–633. https://doi.org/10.4269/ajtmh.20-0973 (2020).
Juang, S. E., et al. Human Papillomavirus Infection and the Risk of Erectile Dysfunction: A Nationwide Population-Based Matched Cohort Study. J .Pers. Med. 12(5), 699. https://doi.org/10.3390/jpm12050699 (2022).
Ma, K.S., Chiang, C. H., Chen, Y. W., Wang, L. T. Correspondence to 'Bacterial citrullinated epitopes generated by Porphyromonas gingivalis infection-a missing link for ACPA production'. Ann. Rheum. Dis. https://doi.org/10.1136/annrheumdis-2020-219255 (2021).
Wu, M. C., Ma, K. S., Chen, H. H., Huang, J. Y, Wei, J. C. Relationship between Helicobacter pylori infection and psoriasis: a nationwide population-based longitudinal cohort study. Medicine (Baltimore). 99(24), e20632. https://doi.org/10.1097/MD.0000000000020632 (2020).
Arabi, Y. M. et al. Near-target caloric intake in critically ill medical-surgical patients is associated with adverse outcomes. J. Parenteral Enteral Nutr. 34, 280–288. https://doi.org/10.1177/0148607109353439 (2010).
Rubinson, L., Diette, G. B., Song, X., Brower, R. G. & Krishnan, J. A. Low caloric intake is associated with nosocomial bloodstream infections in patients in the medical intensive care unit. Crit. Care Med. 32, 350–357. https://doi.org/10.1097/01.Ccm.0000089641.06306.68 (2004).
Huang, Y. C., Yen, C. E., Cheng, C. H., Jih, K. S. & Kan, M. N. Nutritional status of mechanically ventilated critically ill patients: Comparison of different types of nutritional support. Clin. Nutr. 19, 101–107. https://doi.org/10.1054/clnu.1999.0077 (2000).
Tadlock, M. D. et al. Nutritional support using enteral and parenteral methods. Mil. Med. 183, 153–160. https://doi.org/10.1093/milmed/usy074%JMilitaryMedicine (2018).
Boles, J.-M. et al. Weaning from mechanical ventilation. Eur. Respir. J. 29, 1033–1056. https://doi.org/10.1183/09031936.00010206 (2007).
Ma, K. S., et al. Dementia and the Risk of Periodontitis: A Population-Based Cohort Study. J. Dent. Res. 101(3), 270–277. https://doi.org/10.1177/00220345211037220 (2022).
Wu, M. C., Ma, K. S., Wang, Y. H., & Wei, J. C. Impact of tonsillectomy on irritable bowel syndrome: A nationwide population-based cohort study. PLoS One. 15(9), e0238242. https://doi.org/10.1371/journal.pone.0238242 (2020).
Ma, K. S., et al. Patients with juvenile idiopathic arthritis are at increased risk for obstructive sleep apnoea: a population-based cohort study. Eur. J. Orthod. 44(2), 226–231 (2022).
Ma, K. S., et al. Fibromyalgia and periodontitis: Bidirectional associations in population-based 15-year retrospective cohorts. J. Periodontol. 93(6), 877–887. https://doi.org/10.1002/JPER.21-0256 (2022).
Ma, K. S., Thota, E., Huang, J. Y., Wei, J. C., & Resnick, C. M. Increased risk of temporomandibular joint disorders and craniofacial deformities in patients with juvenile idiopathic arthritis: a population-based cohort study. Int. J. Oral. Maxillofac. Surg. https://doi.org/10.1016/j.ijom.2022.04.007 (2022).
Ma, K. S., Thota, E., Huang, J. Y., Huang, Y. F., Wei, J. C. Onset of oral lichen planus following dental treatments: A nested casecontrol study. Oral. Dis. https://doi.org/10.1111/odi.14115 (2021).
Ma, K. S., et al. Tonsillectomy as a risk factor of periodontitis: A population-based cohort study. J. Periodontol. 93(5), 721–731. https://doi.org/10.1002/JPER.21-0215 (2022)
Ma, K. S., Lee, C. M., Chen, P. H., Yang, Y., Dong, Y. W., Wang, Y. H., Wei, J. C., Zheng, W. J. Risk of Autoimmune Diseases Following Optic Neuritis: A Nationwide Population-Based Cohort Study. Front. Med. (Lausanne). 9, 903608. https://doi.org/10.3389/fmed.2022.903608 (2022).
Austin, P. C. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav. Res. 46, 399–424. https://doi.org/10.1080/00273171.2011.568786 (2011).
Ma, K. S., et al. Ocular manifestations of anti-neoplastic immune checkpoint inhibitor-associated Stevens-Johnson syndrome/toxic epidermal necrolysis in cancer patients. Ocul. Surf. 22, 47–50. https://doi.org/10.1016/j.jtos.2021.06.010 (2021).
Kao, Y. S., et al. Topical Prevention of Radiation Dermatitis in Head and Neck Cancer Patients: A Network Meta-analysis. In Vivo. 36(3), 1453–1460. https://doi.org/10.21873/invivo.12851 (2022).
Huang, J. W., et al. Case Report: In Situ Vaccination by Autologous CD16+ Dendritic Cells and Anti-PD-L 1 Antibody Synergized With Radiotherapy To Boost T Cells-Mediated Antitumor Efficacy In A Psoriatic Patient With Cutaneous Squamous Cell Carcinoma. Front. Immunol. 12, 752563. https://doi.org/10.3389/fimmu.2021.752563 (2021).
Yamamoto, S. et al. Meeting calorie and protein needs in the critical care unit: A prospective observational pilot study. Nutr. Metab. Insights 13, 1178638820905992. https://doi.org/10.1177/1178638820905992 (2020).
Gungabissoon, U. et al. Prevalence, risk factors, clinical consequences, and treatment of enteral feed intolerance during critical illness. J. Parenteral Enteral Nutr. 39, 441–448. https://doi.org/10.1177/0148607114526450 (2015).
Ang, D. et al. Optimizing energy expenditure and oxygenation toward ventilator tolerance is associated with lower ventilator and intensive care unit days. J. Trauma Acute Care Surg. 87, 559–565. https://doi.org/10.1097/ta.0000000000002404 (2019).
Fetterplace, K. et al. Targeted full energy and protein delivery in critically ill patients: A pilot randomized controlled trial (FEED trial). J. Parenteral Enteral Nutr. 42, 1252–1262. https://doi.org/10.1002/jpen.1166 (2018).
Yeh, D. D. et al. Adequate nutrition may get you home: Effect of caloric/protein deficits on the discharge destination of critically ill surgical patients. J. Parenteral Enteral Nutr. 40, 37–44. https://doi.org/10.1177/0148607115585142 (2016).
Rahman, A. et al. Identifying critically-ill patients who will benefit most from nutritional therapy: Further validation of the “modified NUTRIC” nutritional risk assessment tool. Clin. Nutr. 35, 158–162. https://doi.org/10.1016/j.clnu.2015.01.015 (2016).
Sindhwani, G. & Rawat, J. Ventilator dependence: Role of nutrition and airway clearance therapy. Lung India 23, 39–41. https://doi.org/10.4103/0970-2113.44429 (2006).
Namen, A. M. et al. Predictors of successful extubation in neurosurgical patients. Am. J. Respir. Crit. Care Med. 163, 658–664. https://doi.org/10.1164/ajrccm.163.3.2003060 (2001).
Chiang, C. H., et al. Performance of the European Society of Cardiology 0/1-Hour, 0/2-Hour, and 0/3-Hour Algorithms for Rapid Triage of Acute Myocardial Infarction : An International Collaborative Meta-analysis. Ann. Intern. Med. 175(1), 101–113. https://doi.org/10.7326/M21-1499 (2022).
Ma, K. S., Hao, H., Huang, H. C., Tang, Y. H., Entropy-Facilitated Machine Learning for Blood Pressure Estimation Using Electrocardiogram and Photoplethysmogram in a Wearable Device. In Proceedings in 2021 14th International Congress on Image and Signal Processing, BioMedical Engineering and Informatics, 1–6. IEEE. https://doi.org/10.1109/CISP-BMEI53629.2021.9624370
Ma, K. S., Chiang, C., Velarde Lopez, A. A., Tsai, S. Identifying Mechanisms Underlying the Association Between Cardiovascular Diseases and Periodontitis Using in Silico Analysis of Canonical Pathways. American Heart J. 229, 172–173. https://doi.org/10.1016/j.ahj.2020.10.038 (2020).
Ma, K. S., Chiang, C., Velarde Lopez, A. A., Wang, L. Cohort Study of Periodontitis-associated Signaling Pathways In Myocardial Infarction Following Atherosclerotic Cardiovascular Diseases. Metabolism: Clinical and Experimental. 154478, 116. https://doi.org/10.1016/j.metabol.2020.154478 (2021).
Haviland, K. et al. Outcomes after long-term mechanical ventilation of cancer patients. BMC Palliat. Care 19, 42. https://doi.org/10.1186/s12904-020-00544-x (2020).
Schönhofer, B., Guo, J. J., Suchi, S., Köhler, D. & Lefering, R. The use of APACHE II prognostic system in difficult-to-wean patients after long-term mechanical ventilation. Eur. J. Anaesthesiol. 21, 558–565. https://doi.org/10.1017/s0265021504007100 (2004).
Piva, S., Fagoni, N. & Latronico, N. Intensive care unit-acquired weakness: Unanswered questions and targets for future research. F1000Research https://doi.org/10.12688/f1000research.17376.1 (2019).
Lemon, S. J., Zack, S. D. & Voils, S. A. No difference in mechanical ventilation-free hours in critically ill patients who received intravenous, oral, or enteral phosphate replacement. J. Crit. Care 39, 31–35. https://doi.org/10.1016/j.jcrc.2017.01.002 (2017).
El Hadidy, S., Saad, M., El Hossany, R., El Gohary, T. & El Ghobashy, M. Coinciding changes in B lines patterns, haemoglobin and hematocrit values can predict outcomes of weaning from mechanical ventilation. Open Access Macedonian J. Med. Sci. 7, 4010–4014. https://doi.org/10.3889/oamjms.2019.615 (2019).
Chen-Roetling, J., Ma, S. K., Cao, Y., Shah, A., & Regan, R. F. Hemopexin increases the neurotoxicity of hemoglobin when haptoglobin is absent. J. Neurochem. 145(6), 464–473. https://doi.org/10.1111/jnc.14328 (2018).
Lai, Y. C., Ruan, S. Y., Huang, C. T., Kuo, P. H. & Yu, C. J. Hemoglobin levels and weaning outcome of mechanical ventilation in difficult-to-wean patients: A retrospective cohort study. PLoS ONE 8, e73743. https://doi.org/10.1371/journal.pone.0073743 (2013).
Herold, T. et al. Elevated levels of IL-6 and CRP predict the need for mechanical ventilation in COVID-19. J. Allergy Clin. Immunol. 146, 128-136.e124. https://doi.org/10.1016/j.jaci.2020.05.008 (2020).
Rose, L. Strategies for weaning from mechanical ventilation: A state of the art review. Intensive Crit. Care Nurs. 31, 189–195. https://doi.org/10.1016/j.iccn.2015.07.003 (2015).
Ma K. S., Liou, Y. J., Huang, P. H., Lin, P. S., Chen, Y. W.,Chang, R. F., Identifying Medically-compromised Patients with Periodontitis-Associated Cardiovascular Diseases Using Convolutional Neural Network-facilitated Multilabel Classification of Panoramic Radiographs. Proceedings of 2021 International Conference on Applied Artificial Intelligence, 1–4. IEEE. https://doi.org/10.1109/ICAPAI49758.2021.9462069.
Ma K. S., Deep neural networks for prediction and detection of ocular sequelae among survivors of Stevens-Johnson syndrome/toxic epidermal necrolysis. Proceedings in 2021 IEEE 17th International Conference on Intelligent Computer Communication and Processing, 463–467. IEEE. https://doi.org/10.1109/ICCP53602.2021.973363
Ma K. S., Screening programs incorporating big data analytics. In P. Keikhosrokiani (Ed.). Big Data Analytics for Healthcare: Datasets, Techniques, Life Cycles, Management, and Applications. 313–327. Academic Press: Elsevier. https://doi.org/10.1016/B978-0-323-91907-4.00023-6 (2022).
Ma, K. S., Chang, H. C., & Krupat, E. Teaching evidence-based medicine with electronic databases for preclinical education. Adv. Physiol. Educ. 45(4), 849–855. https://doi.org/10.1152/advan.00057.2021 (2021).
Ma, K. S. Integrating travel history via big data analytics under universal healthcare framework for disease control and prevention in the COVID-19 pandemic. J. Clin. Epidemiol. 130, 147–148. https://doi.org/10.1016/j.jclinepi.2020.08.016 (2021).
Ma, K. S., Tsai, S. Y. Big Data-driven personal protective equipment stockpiling framework under Universal Healthcare for Disease Control and Prevention in the COVID-19 Era. Int. J. Surg. 79, 290–291. https://doi.org/10.1016/j.ijsu.2020.05.091 (2020).
Acknowledgements
We would like to thank Yu-Xun Wang of Chung Shan Medical University Hospital for providing statistical assistance. This study was supported by a grant from Chung Shan Medical University Hospital for research projects in 2020 (CSH-2020-A-014).
Author information
Authors and Affiliations
Contributions
Y.R.L. and H.C.L. were responsible for the concept and design of the study. Z.Y.L. and K.S.M. contributed to the acquisition and interpretation of the data. C.H.L. established the BI system. S.C.L. and K.S.M. mainly wrote the manuscript. S.F.Y. critically revised the manuscript. All authors participated in the critical revision of the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lo, SC., Ma, K.SK., Li, YR. et al. Nutritional support for successful weaning in patients undergoing prolonged mechanical ventilation. Sci Rep 12, 12044 (2022). https://doi.org/10.1038/s41598-022-15917-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-15917-w
- Springer Nature Limited
This article is cited by
-
Patients with obstructive sleep apnea are at great risk of flavor disorders: a 15-year population-based cohort study
Clinical Oral Investigations (2022)