Abstract
The identification of acquired resistance mutations has been essential in non-small-cell lung cancer (NSCLC) patients with epidermal growth factor receptor (EGFR) active mutations. Rebiopsy plays a pivotal role in selecting the optimal treatment for patients who develop resistance to initial EGFR-tyrosine kinase inhibitors (EGFR-TKIs). This multicenter, observational study was conducted to investigate the details of rebiopsy in Japanese clinical practice. The primary endpoints were the implementation rate of rebiopsy and the concordance rate for T790M mutation detection between histological and cytological specimens using the cobas EGFR Mutation Test, version 2. One hundred ninety-four patients with EGFR-mutant NSCLC were enrolled, and 120 patients developed acquired resistance to EGFR-TKIs. The median age was 68 years (range 20–87), and 52.5% of the patients were women. Rebiopsy was performed in 109 patients, and the implementation rate of rebiopsy was 90.8%. The success rates of rebiopsy in the total, histology, cytology and liquid biopsy populations were 67.9%, 81.3%, 66.7% and 43.8%, respectively. The positive percent agreement and the negative percent agreement in the detection of the T790M mutation between the histological and cytological specimens were both 90.9%. Obtaining histological or cytological tissue samples at rebiopsy may contribute to improving the detection rate of the T790M mutation (trial registration number: UMIN000026019).
Similar content being viewed by others
Introduction
Molecular targeted therapies and immunotherapy using immune checkpoint inhibitors have emerged as essential modalities in various cancer treatments. Epidermal growth factor receptor (EGFR) mutations were strongly correlated with the clinical benefit of EGFR-tyrosine kinase inhibitors (EGFR-TKIs) and the first druggable driver mutation in non-small-cell lung cancer (NSCLC) 1,2. It has been reported that first- or second-generation EGFR-TKIs showed significant clinical benefits compared with standard chemotherapy in patients with EGFR active mutations 3,4,5,6,7,8. After the discovery of EGFR active mutations, various druggable driver mutations and TKIs were identified in lung adenocarcinoma, such as EML4-ALK, ROS1, and BRAF mutations. TKIs for these kinds of druggable driver mutations are highly recommended in the current treatment guidelines for NSCLC 9,10,11. In current clinical practice, the detection of druggable somatic gene alterations has been essential to select adequate treatments in the treatment of NSCLC 12.
Although NSCLC patients with EGFR active mutations respond to EGFR-TKIs, most of them will have disease progression with acquired resistance after a median of 12 months. The mechanisms of acquired resistance have been identified. The most prevalent resistance mutation was the Thr790Met (T790M) point mutation at exon 20, which was revealed in approximately half of the first- or second-generation EGFR-TKI-resistant patients. Osimertinib is a third-generation, irreversible EGFR-TKI that selectively inhibits not only EGFR active mutations but also T790M. The AURA 3 trial was a phase 3 trial to elucidate the efficacy of osimertinib compared with platinum doublet chemotherapy in patients with T790M-positive advanced NSCLC who had disease progression after first-line EGFR-TKI 13. This trial demonstrated that osimertinib has a significantly greater clinical effect than chemotherapy for T790M-positive NSCLC patients. Based on this result, osimertinib was approved for patients who were identified as having the T790M mutation. Osimertinib therapy as a first-line treatment showed a significant survival benefit in patients with NSCLC harboring 19 deletions and L858R compared with first-generation EGFR-TKIs, including gefitinib and erlotinib 14. In current clinical practice, most NSCLC patients with common EGFR mutations receive osimertinib as first-line therapy; however, some EGFR-mutated NSCLC patients are treated with first- or second-generation EGFR-TKIs with/without anti-vascular endothelial growth factor therapy, and these patients still need to receive T790M testing after a failure of first- or second-generation EGFR-TKIs.
In analyses for the T790M mutation, histological specimens from the relapsing sites need to be obtained using “rebiopsy”. However, there are some issues in performing rebiopsy, such as difficulty accessing the relapsing site and patient rejection because of invasive procedures15. Currently, the liquid biopsy method to identify the T790M mutation has been available to resolve these issues. However, the detection sensitivity of the T790M mutation using liquid biopsy is relatively low, and it is difficult to apply liquid biopsy methods to all resistant patients. In addition, there are limited data on the appropriateness of cytological specimens to test the T790M mutation using the cobas EGFR Mutation Test, version 2 if a suitable tissue specimen was not obtained. Therefore, we conducted this multicenter, prospective observational study to investigate the details of rebiopsy, including the implementation or success rate of rebiopsy and the concordance rate for T790M mutation detection between histological and cytological specimens in EGFR-TKI-resistant NSCLC patients.
Results
Characteristics of patients with acquired resistance
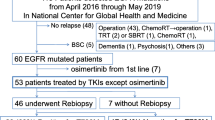
A total of 194 patients were enrolled from February 2017 to January 2019. Among these, 120 patients were diagnosed with acquired resistance to ongoing EGFR-TKI therapy and were considered for undergoing rebiopsy (Fig. 1). The characteristics of patients who received rebiopsy are shown in Table 1. The types of acquired resistance were as follows: 104 patients (86.7%) had RECIST-PD, 60 (50%) had clinical PD, and 8 (6.7%) had SD with enlarged tumors. The median age was 68 years (range, 20–87), and 52.5% of the patients were women. Adenocarcinoma (99.2%) was the most common histology. Sixty-six patients (55%) had exon 19 deletions, 45 (37.5%) had L858R point mutations, and 10 (8.4%) had uncommon mutations, including G719X, L861Q and compound mutations. Forty-seven patients (39.2%) had been treated with erlotinib, 36 patients (30%) received gefitinib, and 37 patients (30.8%) had been treated with afatinib at disease progression. The median time from the start of EGFR-TKIs to rebiopsy was 14 months (range, 1.9 − 90 months).
Results of rebiopsy
In 120 patients with acquired resistance to EGFR-TKIs, rebiopsy was performed on 109 patients, with an implementation rate of 90.8%, while 11 patients (9.2%) did not receive rebiopsy (Fig. 1). Reasons for not performing rebiopsy were as follows: difficulty accessing relapse sites (n = 5), patient refusal (n = 2), transfer to a different hospital (n = 3) and previously performed rebiopsy (n = 1).
Tissue histological specimens were obtained from 59 out of 109 patients (54.1%), including 27 out of 59 who received (45.8%) transbronchial biopsy using endobronchial ultrasonography with a guide-sheath (EBUS-GS); 8 (13.6%) with ultrasound-guided core needle liver biopsy; 6 (10.2%) with transbronchial biopsy without EBUS-GS; 5 (8.5%) with endobronchial ultrasonography-guided transbronchial needle aspiration (EBUS-TBNA); 5 (8.5%) with video-assisted thoracic surgery (VATS); 4 (6.8%) with superficial lymph node biopsy; 3 (5.1%) with bone biopsy using computed tomography (CT)-guided percutaneous core needle biopsy (PCNB); and 1 (1.8%) with lung biopsy using CT-guided PCNB. A summary of the rebiopsy results is shown in Table 2. In 59 patients, tissue histological specimens were diagnosed as follows: adenocarcinoma (n = 53, 90%) and transformation to other histology (n = 3, 5.1%). Two were small cell lung carcinomas, and 1 was a sarcomatoid cancer. No malignant tissue was collected by bone biopsy, EBUS-GS, or VATS in 3 patients. No PCR results were available from 8 patients. The success rate of rebiopsy using histological procedures was 81.3% (48/59). The T790M mutation was identified in 32 (54.2%) out of 53 patients with adenocarcinoma.
Only cytological specimens were available in 18 out of 109 patients (16.5%), including 13 (72.2%) thoracentesis; 3 (18.8%) lumbar puncture; 1 (5.6%) bronchoscopy brushing; and 1 (5.6%) superficial lymph node biopsy. In cytological specimens obtained from these 18 patients, malignant cells were revealed in 15 cytological specimens (83.3%). From cytological specimens, the T790M mutation was identified in only 1 patient (5.6%). No malignant cells were collected by thoracentesis or lumbar puncture in 3 patients. No PCR results were available from 6 patients. The success rate of rebiopsy using cytological procedures was 66.7% (12/18).
After the approval of plasma liquid biopsy using the cobas EGFR Mutation Test, version 2 for T790M detection in July 2017, 32 patients received liquid biopsy. In these 32 patients, the T790M mutation was identified in 8 patients (25%) and not identified in 6 patients (18.8%). Information on EGFR mutations, including T790M, 19 deletions, L858R, and uncommon mutations, was not obtained from liquid biopsy due to poor PCR products in 18 patients (56.2%). Thus, the success rate of liquid biopsy was 43.8% (14/32).
In total, the T790M mutation was identified in 41 patients (37.6%) out of 109 patients who received initial rebiopsy. The total success rate of rebiopsy was 67.9% (74/109). Additional rebiopsy after negative initial rebiopsy results was performed in 7 patients. Among the 7 patients who underwent a second rebiopsy, the T790M mutation was revealed in 2 patients (28.6%) by the cytology procedures. Finally, the T790M mutation was identified in 43 patients (43/109, 39.4%) in this observational cohort, including first and second rebiopsies. Problematic complications regarding rebiopsy were not reported.
The concordance rate for T790M mutation detection between histological and cytological specimens
Both the histological and cytological specimens were obtained at the same time for the T790M mutation testing in 22 patients (Table 3). Each group had one patient who had a discrepancy for the T790M mutation result. Both the positive percent agreement and the negative percent agreement were 90.1% (10/11 for both), and the concordance rate for T790M mutation detection between histological and cytological specimens was 90.1% (20/22).
Discussion
The importance of rebiopsy has increased in patients with EGFR mutations since the report of the AURA3 study results, which demonstrated the efficacy of osimertinib for patients with T790M-positive NSCLC. It is suggested that the implementation rate of rebiopsy may be associated with the prognosis of EGFR-TKI-refractory NSCLC patients 16. In the current observational study, the implementation rate of rebiopsy was 93.4% (109 out of 120 patients with acquired resistance), with a T790M-positive rate of 39.4% (43 out of 109 patients receiving rebiopsy). To our knowledge, the implementation rate of rebiopsy was the highest compared with previous retrospective or observational studies investigating T790M detection in EGFR-mutated NSCLC patients after EGFR-TKIs. The implementation rate of rebiopsy has been reported to range from 55.1 − 63% in retrospective studies and 86.9% in the Japanese observational study named the REMEDY 15,17,18. The use of liquid biopsy might obviously affect the high implementation rate of rebiopsy. Liquid biopsy has significant advantages of feasibility, such as noninvasiveness and accessibility, for detecting the T790M mutation 19. Indeed, the most common procedure of rebiopsy in the REMEDY study was liquid biopsy using plasma, accounting for 58.1% 17. In the current study, 28.9% of patients received liquid biopsy as a rebiopsy procedure. However, liquid biopsy for EGFR-TKI-resistant patients has some limitations. The first problem is the transformation to other histopathological features, such as small cell lung carcinoma (SCLC) transformation, which cannot be detected by liquid biopsy 20. There were four transformation cases (3 small cell lung carcinoma and one sarcomatoid cancer) in this study. The efficacy of osimertinib may be limited for the concomitant case of the T790M mutation and SCLC transformation 21. The second problem of liquid biopsy using plasma is the lower detection rate of the T790M mutation. A previous study demonstrated that one-third of patients who underwent liquid biopsy had the T790M mutation according to the cobas EGFR Mutation Test 22. In this study, the success rate of liquid biopsy was 43.8%, and the detection rate of the T790M mutation was 25%. These results indicated that liquid biopsy could be a useful option for patients for whom tissue samples were not available.
The success of rebiopsy is important to determine the subsequent treatments for EGFR-TKI-refractory patients. In this study, the success rate of the histological procedure (81.3%) was higher than that of the cytological procedure (66.7%) or liquid biopsy (43.8%). The main reason for the selection of liquid biopsy as a rebiopsy procedure was the inaccessibility to relapse lesions, such as bone metastases, central nerve metastases or small lung metastases (data not shown). A skilled expert and adequate devices are needed to perform the invasive procedures accessing such relapse lesions, which may depend on the status of participating institutions. The rebiopsy sites and methods in histology-based procedures may affect the positive rate of the T790M mutation. In this study, the positive rates of the T790M mutation by rebiopsy sites, lung, lymph node, liver and bone, were 47.4% (18/38), 100% (10/10), 50% (5/10) and 66.7% (2/3), respectively. The positive rates of the T790M mutation by BF, open biopsy and needle biopsy were 47.4% (18/38), 77.8% (7/9) and 58.3% (7/12), respectively. It is important to cooperate with each institution in local communities to improve the success rate of rebiopsy.
The concordance of tissue or plasma samples was well investigated in a previous report 23. However, the data regarding the concordance of histological and cytological samples have been insufficient. Transbronchial procedures are common methods used to perform rebiopsy because of the availability and feasibility of bronchoscopy. The percentage of patients who received rebiopsy by transbronchial procedures without liquid biopsy was 50.6% (39/77), including EBUS-GS, transbronchial biopsy, EBUS-TBNA and BF brushing in this study (Fig. 1). The percentages of rebiopsy procedure transbronchial procedures in prospective cohort trials were 52.4% (43/82) and 63.9% (69/108) 17,24. However, it is difficult to obtain sufficient tissue samples for histology-based testing by transbronchial procedures from all patients. We investigated the accuracy of cytology-based T790M detection compared with histology-based testing using tissues obtained at the same time. As a result, the positive percent agreement and the negative percent agreement were both 90.1% (Table 3). DNA degradation by formalin in histology-based procedures and a small percentage of malignant cells in cytology-based procedures might result in these discordant mutation results. These results indicate that cytological specimens obtained by transbronchial procedures could be useful for detecting the T790M mutation.
This study has several limitations. First, when this study was conducted, liquid biopsy was not approved for use in clinical practice in Japan. The main limitation of this study was that the implementation rate of rebiopsy could not be evaluated according to the original statistical hypothesis because of the approval status of liquid biopsy in Japan. Indeed, 5 patients did not receive rebiopsy because of difficulty accessing relapse sites and the unavailability of liquid biopsy. Second, in this study, liquid biopsy was performed using the cobas EGFR Mutation Test, version 2, which can detect only EGFR mutations in exons 18–21. This restriction by PCR-based methods could affect the lower success rate of liquid biopsy. In current clinical practice, next-generation sequencing (NGS) panels, such as FoundationOne Liquid CDx and Guardant360 CDx, cover more mutations with higher sensitivity than the cobas EGFR Mutation Test, version 2. It is expected that a higher success rate of liquid biopsy can be achieved using the NGS panel. Future studies are warranted to compare the success rate of liquid biopsy by the NGS oncology panel with histology- and cytology-based procedures. In addition, the NGS panel could detect other mutations that cause acquired resistance to EGFR-TKIs. NGS-based testing will become the mainstream rebiopsy method to address this situation in the future. Third, information on treatment after rebiopsy was not collected in the present study. We did not include treatment after rebiopsy as an endpoint; therefore, this information is missing.
Revealing the resistance mechanisms and developing a strategy for overcoming resistance to EGFR-TKIs remain the main focuses of the investigation of EGFR mutation-positive patients. After the report of the FLAURA study, the importance of T790M detection has decreased because most physicians tend to choose osimertinib for chemo-naive EGFR mutation-positive NSCLC patients. However, new resistance mechanisms have been identified from the analysis using liquid biopsy after treatment with osimertinib in the FLAURA trial 25. The most frequent resistance mechanisms were MET amplification (15%) and secondary EGFR mutations (10%), including C797X and uncommon mutations. These resistance mechanisms will become new targets to overcome osimertinib resistance, and a number of clinical trials are ongoing in this area. Clinical investigations concerning rebiopsy procedures and mutation detection methods should be continued for future driver-based medicine. The current study demonstrated that rebiopsy was feasible and could provide useful data to select subsequent treatments even in clinical practice.
Methods
Study design
The present study was a multicenter, prospective, observational study in patients with EGFR mutation-positive advanced NSCLC who experienced disease progression during treatment with EGFR-TKIs. Patients with advanced NSCLC meeting all inclusion criteria and not meeting exclusion criteria were consecutively enrolled from medical institutions participating in the Niigata Lung Cancer Treatment Group (NLCTG) to collect information on rebiopsy data. This study was conducted according to the principles of the Declaration of Helsinki. The institutional review board of each participating institution (Niigata Cancer Center Hospital, Niigata University Graduate School of Medical and Dental Sciences, Nagaoka Red Cross Hospital, Nagaoka Chuo General Hospital, Niigata Prefectural Central Hospital, Niigata City General Hospital, Saiseikai Niigata Hospital, Shibata Hospital—Niigata Prefectural Hospital, Nishi Niigata Chuo Hospital, Sado General Hospital, Tsuruoka Municipal Shonai Hospital, Shinrakuen Hospital, Niigata Medical Center) approved the protocol. This study is registered in February 2017 on the clinical trials site of the University Hospital Medical Information Network Clinical Trials Registry (registration number: UMIN000026019). Information on patient demographics was collected retrospectively from the medical records at study enrollment. Additional data regarding rebiopsy were collected when the following situations were met: sustained response to EGFR-TKI (compete response, pertain response, or stable disease more than 6 weeks) and acquired resistance to ongoing EGFR-TKI. The definition of acquired resistance in this study was as follows: progressive disease according to Response Evaluation Criteria in Solid Tumors (RECIST) criteria (RECIST-PD), clinically progressive disease assessed by physicians (clinical PD), and stable disease according to RECIST criteria but increasing tumor volume compared with baseline (SD with enlarged tumor). The collected data were as follows: patient status at the point of rebiopsy, information on rebiopsy sites (relapse site, size, number, and so on) and the rebiopsy procedure, the results of rebiopsy (cytology, histology, and the T790M status), complications regarding rebiopsy, subsequent treatments, and prognosis. If patients did not undergo rebiopsy at the point when acquired resistance developed, the reasons for not undergoing rebiopsy, including patient refusal, were collected. The existence of malignant cells was determined by pathologists at each participating institution. All data were collected using electronic data capture.
Patients
The inclusion criteria were as follows: a histologically or cytologically confirmed advanced NSCLC with EGFR active mutations; stage III/IV not amenable to definitive radiation therapy or postoperative recurrence at the start of EGFR-TKI therapy; ongoing EGFR-TKI therapy (gefitinib, erlotinib or afatinib); no prior T790M mutation detection; written informed consent for study participation from the patient. Patients treated with third-generation EGFR-TKIs were excluded. Prior cytotoxic chemotherapies were allowed. Written informed consent was obtained from all study participants.
Study endpoints
The primary endpoint was the implementation rate of rebiopsy, defined as the number of patients who underwent rebiopsy from any site/total number of patients with acquired resistance to EGFR-TKIs. After approval of liquid biopsy testing for the T790M mutation in July 2017, liquid biopsy, which was performed using the cobas EGFR Mutation Test, version 2, was also counted as rebiopsy. The coprimary endpoint was the concordance rate for T790M mutation detection between histological and cytological specimens using the cobas EGFR Mutation Test, version 2. The concordance rate for T790M mutation detection between histological and cytological specimens was defined as the percentage of patients with T790M positivity according to cytological specimens among patients with T790M positivity according to histological specimens. Cell block analysis was included in cytological specimens. Secondary endpoints were as follows: the success rate of rebiopsy according to procedure, the T790M mutation-positive rate according to biopsy site or procedure, safety of rebiopsy procedures, reasons for patients not undergoing rebiopsy, and implementation rate of rebiopsy according to institution and available rebiopsy procedures. For histology- and cytology-based procedures, the success rate of rebiopsy was defined as the percentage of patients in whom malignant cells and the results of gene mutation analysis were available among the patients who underwent rebiopsy. For liquid biopsy, the success rate of rebiopsy was defined as the percentage of patients in whom EGFR mutations were detected among the patients who underwent liquid biopsy.
Statistical analyses
In a retrospective study regarding rebiopsy, the implementation rate of rebiopsy was reported to be 62.5%, and the percentage of patients who could be examined for EGFR gene mutations using histological specimens was reported to be 28% 16. We estimated the lower limit to be able to examine the T790M mutation in both histological and cytological specimens to be 30%. If we assumed a threshold rate of 0.5 and an expected rate of 0.8, 83 patients were needed to evaluate the positive percent agreement of T790M mutation detection between histological and cytological specimens with 80% power and an alpha level of 0.05 (2-sided). Even if a dropout rate of approximately 5% was considered, it was estimated that 100 patients was the target number of patients who had acquired resistance. This sample size would have a half-width of the exact 95% confidence interval of ± 10% or less for the implementation rate of rebiopsy. SAS version 9.4 (SAS Inc., Cary, NC, USA) was used for the sample size evaluation.
References
Lynch, T. J. et al. Activating mutations in the epidermal growth factor receptor underlying responsiveness of non-small-cell lung cancer to gefitinib. N. Engl. J. Med. 350, 2129–2139. https://doi.org/10.1056/NEJMoa040938 (2004).
Paez, J. G. et al. EGFR mutations in lung cancer: Correlation with clinical response to gefitinib therapy. Science 304, 1497–1500. https://doi.org/10.1126/science.1099314 (2004).
Maemondo, M. et al. Gefitinib or chemotherapy for non-small-cell lung cancer with mutated EGFR. N. Engl. J. Med. 362, 2380–2388. https://doi.org/10.1056/NEJMoa0909530 (2010).
Mitsudomi, T. & Yatabe, Y. Mutations of the epidermal growth factor receptor gene and related genes as determinants of epidermal growth factor receptor tyrosine kinase inhibitors sensitivity in lung cancer. Cancer Sci. 98, 1817–1824. https://doi.org/10.1111/j.1349-7006.2007.00607.x (2007).
Rosell, R. et al. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): A multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 13, 239–246. https://doi.org/10.1016/s1470-2045(11)70393-x (2012).
Zhou, C. et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): A multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 12, 735–742. https://doi.org/10.1016/s1470-2045(11)70184-x (2011).
Sequist, L. V. et al. Phase III study of afatinib or cisplatin plus pemetrexed in patients with metastatic lung adenocarcinoma with EGFR mutations. J. Clin. Oncol. 31, 3327–3334. https://doi.org/10.1200/jco.2012.44.2806 (2013).
Wu, Y. L. et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): An open-label, randomised phase 3 trial. Lancet Oncol. 15, 213–222. https://doi.org/10.1016/s1470-2045(13)70604-1 (2014).
Hanna, N. et al. Systemic Therapy for Stage IV non-small-cell lung cancer: American society of clinical oncology clinical practice guideline update. J. Clin. Oncol. 35, 3484–3515. https://doi.org/10.1200/jco.2017.74.6065 (2017).
Planchard, D. et al. Metastatic non-small cell lung cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 29, iv192–iv237. https://doi.org/10.1093/annonc/mdy275 (2018).
Akamatsu, H. et al. The Japanese Lung Cancer Society Guideline for non-small cell lung cancer, stage IV. Int. J. Clin. Oncol. 24, 731–770. https://doi.org/10.1007/s10147-019-01431-z (2019).
Kalemkerian, G. P. et al. Molecular testing guideline for the selection of patients with lung cancer for treatment with targeted tyrosine kinase inhibitors: American society of clinical oncology endorsement of the college of American pathologists/international association for the study of lung cancer/association for molecular pathology clinical practice guideline update. J. Clin. Oncol. 36, 911–919. https://doi.org/10.1200/jco.2017.76.7293 (2018).
Mok, T. S. et al. Osimertinib or platinum-pemetrexed in EGFR T790M-positive lung cancer. N. Engl. J. Med. 376, 629–640. https://doi.org/10.1056/NEJMoa1612674 (2017).
Soria, J. C. et al. Osimertinib in untreated EGFR-mutated advanced non-small-cell lung cancer. N. Engl. J. Med. 378, 113–125. https://doi.org/10.1056/NEJMoa1713137 (2018).
Kawamura, T. et al. Clinical factors predicting detection of T790M mutation in rebiopsy for EGFR-mutant non-small-cell lung cancer. Clin. Lung. Cancer 19, e247–e252. https://doi.org/10.1016/j.cllc.2017.07.002 (2018).
Imakita, T. et al. Impact on prognosis of rebiopsy in advanced non-small cell lung cancer patients after epidermal growth factor receptor-tyrosine kinase inhibitor treatment: A systematic review. BMC Cancer 19, 105. https://doi.org/10.1186/s12885-019-5309-x (2019).
Seto, T. et al. Real-World EGFR T790M testing in advanced non-small-cell lung cancer: A prospective observational study in Japan. Oncol. Ther. 6, 203–215 (2018).
Tseng, J. S. et al. The emergence of T790M mutation in EGFR-mutant lung adenocarcinoma patients having a history of acquired resistance to EGFR-TKI: Focus on rebiopsy timing and long-term existence of T790M. Oncotarget 7, 48059–48069. https://doi.org/10.18632/oncotarget.10351 (2016).
Li, C., Jia, R., Liu, H., Zhang, B. & Wang, C. EGFR T790M detection and osimertinib treatment response evaluation by liquid biopsy in lung adenocarcinoma patients with acquired resistance to first generation EGFR tyrosine kinase inhibitors. Diagn. Pathol. 13, 49. https://doi.org/10.1186/s13000-018-0728-6 (2018).
Oser, M. G., Niederst, M. J., Sequist, L. V. & Engelman, J. A. Transformation from non-small-cell lung cancer to small-cell lung cancer: molecular drivers and cells of origin. Lancet Oncol. 16, e165-172. https://doi.org/10.1016/s1470-2045(14)71180-5 (2015).
Minari, R. et al. Primary resistance to osimertinib due to SCLC transformation: Issue of T790M determination on liquid re-biopsy. Lung Cancer 115, 21–27. https://doi.org/10.1016/j.lungcan.2017.11.011 (2018).
Thress, K. S. et al. EGFR mutation detection in ctDNA from NSCLC patient plasma: A cross-platform comparison of leading technologies to support the clinical development of AZD9291. Lung Cancer 90, 509–515. https://doi.org/10.1016/j.lungcan.2015.10.004 (2015).
Zhou, J. et al. Re-biopsy and liquid biopsy for patients with non-small cell lung cancer after EGFR-tyrosine kinase inhibitor failure. Thorac. Cancer 10, 957–965. https://doi.org/10.1111/1759-7714.13035 (2019).
Chouaid, C. et al. Feasibility and clinical impact of re-biopsy in advanced non small-cell lung cancer: A prospective multicenter study in a real-world setting (GFPC study 12–01). Lung Cancer 86, 170–173. https://doi.org/10.1016/j.lungcan.2014.08.016 (2014).
Ramalingam, S. S. et al. Mechanisms of acquired resistance to first-line osimertinib: Preliminary data from the phase III FLAURA study. Ann. Oncol. 29(Suppl 8), viii740. https://doi.org/10.1093/annonc/mdy424.063 (2018).
Acknowledgements
We thank the patients and their families and Hiroko Aita for their support and participation in this study. We also thank the data service division of Niigata University Medical and Dental Hospital Clinical and Translational Research Center for their professional support.
Funding
This study was funded by AstraZeneca Japan.
Author information
Authors and Affiliations
Contributions
K. K., S. M. and S. W. wrote the main manuscript text and K. K. prepared Fig. 1. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
Satoshi Watanabe received honoraria (lecture fee) from AstraZeneca, CHUGAI PHARMACEUTICAL, ONO PHARMACEUTICAL, Eli Lilly Japan, Bristol-Myers, Boehringer Ingelheim, MSD, TAIHO PHARMACEUTICAL, Pfizer, Novartis, and DAIICHI SANKYO. Satoshi Watanabe received research grants from AstraZeneca, Boehringer Ingelheim. Hiroshi Tanaka received honoraria (lecture fee) from AstraZeneca. Toshiaki Kikuchi received honoraria (lecture fee) from Boehringer Ingelheim, AstraZeneca, CHUGAI PHARMACEUTICAL. Toshiaki Kikuchi received a research fund from AstraZeneca. Toshiaki Kikuchi received research grants from SHIONOGI PHARMACEUTICAL, CHUGAI PHARMACEUTICAL, ONO PHARMACEUTICAL, Eli Lilly Japan. Other authors did not have any competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Koyama, K., Miura, S., Watanabe, S. et al. Observational study of rebiopsy in EGFR-TKI-resistant patients with EGFR mutation-positive advanced NSCLC. Sci Rep 12, 6367 (2022). https://doi.org/10.1038/s41598-022-10288-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-10288-8
- Springer Nature Limited
This article is cited by
-
Monitoring of T790M in plasma ctDNA of advanced EGFR-mutant NSCLC patients on first- or second-generation tyrosine kinase inhibitors
BMC Cancer (2023)
-
Liquid biopsy for detecting epidermal growth factor receptor mutation among patients with non-small cell lung cancer treated with afatinib: a multicenter prospective study
BMC Cancer (2022)