Abstract
There is limited evidence regarding the possible role of dietary acid load (DAL) in the pathophysiology of migraine headaches. Therefore, we sought to examine DAL in relation to the clinical features of migraine including headache frequency, severity and duration, headache impact test-6 (HIT-6), and serum levels of nitric oxide (NO). In the present cross-sectional study, 262 patients (38 men and 224 women aged 20–50 years) were recruited through a simple random sampling method. Dietary intakes were obtained by using a validated 168-item semi-quantitative food frequency questionnaire (FFQ). DAL was then calculated by two different methods; potential renal acid load (PRAL) and net endogenous acid production (NEAP). In total, 262 patients with a mean (SE) age of 36.1 (0.53) and a BMI of 25.55 (0.21) were included in the current study. After controlling for potential confounders, a higher DAL was positively associated with headache frequency in those with the highest DAL score compared to the lowest (PRAL; β = 2.33; 95% CI 0.78, 3.88; NEAP; β = 1.74; 95% CI 0.13, 3.34). Increasing NEAP from 28.96 to 35.89 resulted in a 3.43 and 2.74 increment in HIT-6 scores in the crude (95% CI 1.35, 5.52) and fully-adjusted models (95% CI 0.40, 5.07), respectively. Moreover, a higher dietary PRAL was significantly associated with migraine-related disability, as shown by HIT-6, in subjects of the third tertile compared to those in the first tertile after controlling for confounders (β = 2.42; 95% CI 0.13, 4.70). In conclusion, our study highlighted the importance of the acid–base properties of a diet in the pathophysiology of migraine headaches. However, further well-designed studies are needed to confirm our findings.
Similar content being viewed by others
Introduction
Migraine is one of the most common neurological disorders worldwide that can cause substantial disability1,2. Globally, 18% and 6% of women and men, respectively are affected by migraine3. Recurrent episodes of headache and its concomitant symptoms (e.g., photophobia, phonophobia, nausea, and vomiting) which exist for 4–72 h are characterized as a migraine headache4. In addition to the substantial economic burden on societies that are imposed by migraine5, this condition has been linked to several health problems such as impaired cognition chronic heart disease, stroke, obesity, depression, and anxiety6,7.
Appropriate acid–base balance is a key factor for the normal physiological function of the body8. An imbalance in acid–base homeostasis can be linked with various diseases, such as diabetes, cardiovascular disease, Alzheimer’s disease, and mood disorders8. Chronic metabolic acidosis could also invoke hypertension, which is a potential precursor of migraine headaches9,10. Furthermore, a positive relation between acidosis and nitric oxide (NO) synthesis has been found11, NO has been suggested as a possible mechanism by which migraine attacks might be aggravated12.
Maintaining acid–base equilibrium by consuming beneficial foods has gained interest in recent years13. This could prevent metabolic acidosis which deleteriously affects human health13. Diets characterized by high intakes of meat, dairy products, and grains, as well as low intake of fruit and vegetables can lead to metabolic acidosis14. Dietary acid load (DAL) has been established as a means of detecting the balance between acidic foods (e.g. animal sources of protein) and alkaline foods (e.g. vegetables and fruit) and to provide the acid–base properties of the diet14.
The association between specific food groups and migraine has been investigated previously15,16. However, studies on the association between DAL and migraine have not been widely performed. A cross-sectional study found a higher DAL to be deleteriously associated with migraine headache characteristics among women17. Since previous studies focused mostly on specific foods and found an inverse association between alkaline foods and migraine headache15, there may be also a link between DAL and migraine. The association between DAL and migraine headache was previously investigated in women, and thus such association remains unsolved among men. Therefore, this study was carried out to investigate the association between DAL and clinical outcomes of migraine headaches including severity, frequency, and duration in a sample of Iranian adults.
Materials and methods
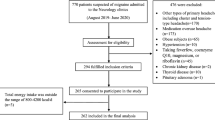
Participants
The current cross-sectional study was performed among Iranian adults between August 2019 and June 2020. Using a simple random sampling method, a total sample of 262 patients aged from 20 to 50 years was recruited from neurology clinics affiliated with Isfahan University of Medical Sciences. Patients were eligible for the present study if they: (1) had a body mass index (BMI) between 18.5 and 30 kg/m2 and (2) were diagnosed with migraine by an expert neurologist based on the International Classification of Headache Disorders (ICHD–3) criteria18. Those who had a history of diabetes, cardiovascular disease, hypertension, cancer, hepatic, thyroid, or renal disease, and other neurological disorders, as well as those who had used dietary and herbal supplements (i.e. magnesium, coenzyme Q10, riboflavin, or feverfew) were excluded. Also, individuals who reported daily energy intakes outside the range of 800–4200 kcal/day (3347–17,573 kJ/day) were excluded from the current analysis19. This study was approved by the Isfahan University of Medical Sciences Research Ethics Committee (IR.MUI.RESEARCH.REC.1398.352). All participants provided written informed consent forms. All study protocols were conducted according to the ethical guidelines of the 1975 Declaration of Helsinki.
Dietary intake assessment
We applied an interviewer-administered 168-item food frequency questionnaire (FFQ) to gather individuals’ usual dietary intakes during the previous year. Its validity and reliability have been reported previously20. Foods with their standard serving sizes were listed in this FFQ with a daily, weekly, or monthly frequency basis option. A trained dietitian asked the participants about the consumption frequency for each food item over the preceding year. Considering the reported portion size and frequency for each food, all food items were calculated on a daily basis and then were converted to grams per day using household measures21. Energy and the other nutrients’ content for each item were then computed using Nutritionist 4 software (First Databank, Hearst Corp., San Bruno, CA, USA), which had been modified for Iranian foods.
Calculating DAL
Potential renal acid load (PRAL) and net endogenous acid production (NEAP) are two different validated22,23 methods that were used to calculate DAL. They were computed using the algorithms below:
-
PRAL (mEq/day) = (protein intake [g/day] × 0.49) + (phosphorus intake [mg/day] × 0.037) − (potassium intake [mg/day] × 0.021) − (calcium intake [mg/day] × 0.013) − (magnesium intake [mg/day] × 0.026).
-
NEAP (mEq/day) = (54.5 × protein intake [g/day] ÷ potassium intake [mEq/day]) − 10.2.
Higher values show that the diet could potentially shift the acid–base equilibrium into acidosis.
Assessment of migraine clinical outcomes
The possible impact of migraine on participants’ quality of life was examined by a 6-item validated questionnaire, headache impact test (HIT-6)24. This questionnaire contains a five-level option for each question: never (6 scores), rarely (8 scores), sometimes (10 scores), very often (11 scores), and always (13 scores). The overall score ranges were from 36 to 78. The effect of headache on the individuals’ quality of life was categorized to be none (36–49), moderate (50–55), substantial (56–59), and severe (≥ 60).
Participants were asked to fill out a 30-day headache diary which was accompanied by written and verbal instructions throughout the upcoming month. In this diary, clinical features of migraine headache including time of attack onset, duration, and severity had to be reported. The visual analog scale (VAS) questionnaire was applied to assess the severity of headaches25. Each participant received a score ranging from 0 to 10, in which “0” meant no pain and “10” the worst imaginable pain. The number of attacks per month (frequency) and mean duration of headache attacks per month (duration) were also examined.
Assessment of serum NO
Following 8–12 h of fasting, 5 mL of venous blood was taken from participants in the Baradaran laboratory, affiliated with Isfahan University of Medical Sciences. The blood samples were centrifuged at 3500 rpm and serum was separated and kept at − 80 °C for later analysis. Serum NO was measured using available commercial kits (Kiazist Life Sciences, Iran) using the Griess method.
Assessment of other variables
Data on demographic characteristics including gender, age, smoking, marital status, number of family members, and medications were gathered through a face-to-face interview. We used an Iranian validated version of the International Physical Activity Questionnaire (IPAQ)26 for 7 days to examine individuals’ physical activity status. To measure blood pressure, a mercury sphygmomanometer (Riester, Germany) was applied. Weight was measured using a digital scale (Omron BF511, Omron Corp., Kyoto, Japan) in light clothes to the nearest 100 g. Height was measured to the nearest 1 mm by a wall tape meter in a standing position without shoes. The BMI was then calculated using weight (kg) divided by height squared (m2).
Statistical analysis
After constructing PRAL and NEAP, participants were classified based on tertiles of both PRAL and NEAP. Continuous and categorical variables were expressed as mean ± standard error (SE) and number (percent), respectively. To compare differences in qualitative and quantitative variables across tertiles of PRAL and NEAP, the Chi-square test and analysis of variance (ANOVA) were applied, respectively. Multiple linear regression analysis was used to evaluate the association between DAL (PRAL and NEAP) and headache frequency, duration, severity, HIT-6, and serum NO levels in crude and adjusted models. The first model was adjusted for age (continuous), sex, and energy intake (continuous). The second model was further controlled for smoking status (current smoker/non-current smoker), marital status (single/married), migraine characteristic (with aura/without aura), family history (yes/no), physical activity (continuous), and mean arterial pressure (continuous). A third model included those variables in Model 2 plus BMI. All beta (β) estimates were obtained by considering the first tertile of PRAL and NEAP as the reference. The tertiles of PRAL and NEAP were considered as ordinal variables in the linear regression models to estimate the trend of β across these tertiles. All the analyses were performed by applying SPSS version 26 (IBM Corp, Armonk, NY, USA). P-values < 0.05 were considered significant.
Ethics approval and consent to participate
The research ethics committee of Isfahan University of Medical Sciences approved the protocol of the current study on 26 August 2019 (IR.MUI.RESEARCH.REC.1398.352).
Results
In total, 262 patients with a mean (SE) age of 36.1 (0.53) and a BMI of 25.55 (0.21) were included in the current study. Characteristics of study participants across the tertiles of dietary PRAL and NEAP are indicated in Table 1. Subjects in the last tertile of PRAL were less likely to be female (P = 0.018) and had lower age (P = 0.012) as well as higher headache frequency (P < 0.001), compared to the first tertile. Furthermore, individuals in the top versus bottom tertiles of NEAP had a lower age (P = 0.022) and earlier diagnosis of migraine (P = 0.027) as well as a higher headache frequency (P = 0.001) and HIT-6 score (P = 0.03). There was no significant difference in the case of other variables provided in Table 1 (all P-values > 0.05).
Dietary intakes of selected nutrients and food groups across tertiles of PRAL and NEAP are presented in Table 2. Compared to the lowest tertile, participants in the highest tertile of both PRAL and NEAP had significantly higher intakes of protein, fat, and meat as well as lower intakes of carbohydrate, potassium, magnesium, fruit, and vegetables. Furthermore, participants in the top tertile of PRAL had a significantly higher energy intake compared to the bottom tertile. In contrast; considering the highest versus lowest tertile of NEAP, subjects consumed less energy.
The β estimates and 95% CIs for headache frequency, duration, severity, HIT-6, and serum NO are shown in Table 3. In the crude model, subjects in the third tertile of PRAL had a higher headache frequency (β = 4.21; 95% CI 2.20, 6.23), compared to the first tertile. A similar result was found for the association between NEAP and headache frequency (β = 3.67; 95% CI 1.65, 5.70). After adjustment for age, sex and energy intake, the associations were attenuated for PRAL (β = 3.35; 95% CI 1.25, 5.45) and NEAP (β = 2.41; 95% CI 0.20, 4.62). The results were further attenuated for both PRAL (β = 2.31; 95% CI 0.75, 3.86) and NEAP (β = 1.71; 95% CI 0.11, 3.32) after additional adjustment for marital status, smoking status, migraine type, migraine characteristics, family history, mean arterial pressure, and physical activity. After controlling for BMI, a higher DAL was positively associated with headache frequency in those with the highest DAL score compared to the lowest (PRAL; β = 2.33; 95% CI 0.78, 3.88; NEAP; β = 1.74; 95% CI 0.13, 3.34). A higher dietary PRAL was significantly associated with migraine-related disability, as shown by HIT-6, in subjects of the third tertile compared to those in the first tertile, either in the crude model (β = 2.28; 95% CI 0.17, 4.39) or after controlling for age, sex and energy intake (β = 2.42; 95% CI 0.13, 4.70). Further adjustment for marital status, smoking status, migraine type, migraine characteristic, family history, mean arterial pressure and physical activity attenuated the findings (β = 2.11; 95% CI − 0.18, 4.41). Also, in the fully adjusted model, the association between PRAL and HIT-6 was not statistically significant (β = 2.04; 95% CI − 0.24, 4.33). Conversely, increasing NEAP from 28.96 to 35.89 resulted in a 3.43 and 2.74 increment in HIT-6 scores in the crude (95% CI 1.35, 5.52) and fully-adjusted models (95% CI 0.40, 5.07), respectively. In addition, both PRAL and NEAP were not found to be significantly associated with headache duration, headache severity, and serum NO either before or after adjustment for potential confounders.
Discussion
The present study is among the first to address the potential roles of DAL in migraine headaches using a sample of Iranian individuals diagnosed with migraine. We found that dietary PRAL and NEAP are independent predictors of headache frequency. Moreover, there was a significant association between NEAP and PRAL and migraine-related disability; however, this link was dependent on potential confounders for PRAL. Our findings highlighted the importance of acid–base properties of a diet in the pathophysiology of migraine headaches and contribute to the current literature to provide new information regarding the role of diet in migraine headaches in a sample of migraine patients seeking care from specialty clinics.
Migraine is considered the first cause of disability in adults under 50, and its growing prevalence can impose a detrimental effect on public health27. Migraine can also lead to other chronic diseases and mortality28,29, and needs special attention. We found a positive association between the acidity of the diet and some migraine headache features. Therefore, it is clinically important to recommend migraine patients to consume alkaline foods such as vegetables, fruits, nuts, and legumes as well as limiting acidifying foods including meats and meat products. This approach could be done in the context of plant-based diets such as the Mediterranean diet30 or the dietary approaches to stop hypertension (DASH) diet31.
We found that the association between PRAL and HIT-6 was not independent of marital status, smoking status, migraine type, migraine characteristics, family history, mean arterial pressure, physical activity, and BMI, indicating that the potential effect of PRAL is related to various lifestyle and clinical aspects of migraine patients and that it is not specific to PRAL alone. Previously, a direct association between obesity and migraine characteristics was shown32,33,34. An inverse association between adiposity and health-related quality of life was also investigated35. Relations between migraine headache and smoking36,37, physical activity38, family history of migraine39, and blood pressure40 was found in the prior studies. Also, lower quality of life could be associated with smoking habits41, less physical activity42,43,44, and having hypertension45. On the other hand, PRAL has been shown to be related to hypertension46 and obesity47. Studies have suggested that individuals with higher physical activity levels have a higher consumption of fruit and vegetables, which have a less acidifying effect48,49. Given the potential mediating effect of the above-mentioned confounders, the insignificant association between PRAL and HIT-6 in the adjusted models might be explained.
In the current study, PRAL and NEAP were independently used to calculate DAL. We found that individuals in the highest tertile of PRAL and NEAP have higher intakes of protein and lower intakes of potassium and magnesium. We also showed that patients in the highest tertile of PRAL and NEAP have higher intakes of meat and lower intakes of fruit and vegetables. Higher intakes of protein and phosphorus contribute to higher scores of PRAL and NEAP, indicating potential acidity of the diet50, whereas higher intakes of potassium, magnesium, and calcium result in lower scores of PRAL and NEAP50. It is worth mentioning that the quality of protein is also an important factor. Animal proteins have higher contents of phosphorus that increase PRAL and, therefore, have an acidifying effect on the diet13. Furthermore, hydrochloric acid is generated in the metabolism of arginine, lysine, and histidine, which are highly prevalent in animal proteins14. Studies have suggested that milk and dairy products, as animal sources of protein, are rich in calcium that compensates for their high phosphorous content13. In contrast to animal proteins, phosphorous found mostly in the form of phytate in vegetable proteins has less bioavailability13. Also, vegetable proteins are high in glutamate which requires hydrogen ions for their metabolism, and thus, vegetable proteins have a neutral effect on the acid load51. In addition, fruit and vegetables are generally rich in potassium and magnesium that resulting in a higher alkalinizing capacity of the diet13. Given the above-mentioned points, animal-based foods such as meat and meat products are responsible for the potential acidity of the diet, and fruit and vegetables act as protective determinants for metabolic acidosis. Therefore, a diet high in fruit and vegetables, with reduced meat intake, could be recommended to maintain the acid–base equilibrium in the body.
In the previous studies, specific foods have been investigated mostly in relation to migraine headaches. A case–control study found that those who have migraine headaches have higher intakes of red and white meat, whereas they consume lower amounts of fruit and vegetables compared to healthy controls52. Furthermore, another case–control study found fruit and vegetables to be inversely associated with the odds of migraine among children15. Conversely, a cross-sectional study on 11,910 Canadian adults did not observe a significant relationship between fruit and vegetables intake and risk of migraine53. Another cross-sectional study revealed that a dietary pattern high in meat and meat products, known as the Western dietary pattern, is inversely related to the odds of migraine54. However, no significant association was depicted between the dietary pattern rich in fruit and vegetables and migraine risk54. Nevertheless, we must keep in mind that humans consume a combination of different nutrients and foods; therefore, it is more important to take the whole diet into account when examining the acidifying or alkalinizing effects of foods concerning diseases.
DAL has not been widely investigated in relation to migraine headaches. In opposition to our findings, a cross-sectional study found that women in the top tertile of PRAL and NEAP were more likely to experience severe headaches compared to the bottom tertile17. It was also found that PRAL and NEAP scores were directly correlated to the duration of headaches17. A case–control study revealed that adults in the highest tertile of PRAL and NEAP have a seven and fourfold increase in the odds of having migraines55. These discrepancies might be explained by different study designs, sample sizes, and methods for assessing dietary intake and the outcome. Also, considering different confounders in the studies might result in inconsistent results.
An essential concern in epidemiologic studies, especially in cross-sectional studies, is the possible existence of reverse causation. The reverse causation hypothesis is that the relation might be in the reverse direction, for which the study is conducted56. It is worth noting that migraine patients might change their dietary habits, and thus, a bidirectional association might exist between DAL and migraine headaches. Given the lack of studies examining such associations, further prospective cohort studies on large populations are essential to elucidate the causal relationship between DAL and migraine headaches.
The association between DAL and migraine headaches could be explained through several mechanisms. Acidosis has been suggested to augment NO and inflammatory marker production11,57,58. Consequently, migraine headaches can be initiated by the action of the NO-cyclic guanosine monophosphate (cGMP) pathway12. Also, NO and TNF-α can prolong the pain by stimulating calcitonin gene-related peptide release, a potential factor triggering migraine headaches, in trigeminal ganglion neurons12. However, we did not find a significant association between NO concentrations and DAL. Despite the high nitrate content of vegetables, almost 65% of the dietary nitrate (the precursor for NO) could be excreted in the urine, and the remaining 35% might not be converted completely to NO59. Therefore, the dietary proportion for NO production is not as much as that of endogenous l-arginine. Another mechanism might be increased levels of cortisol in response to the high acidity of the diet60. Cortisol might negatively affect migraine headache recovery61. Studies have also suggested that elevated levels of cortisol could be linked to high BMI and blood pressure that have adverse effects on the pathogenesis of migraines62,63. Another possible mechanism is the imbalance of gut microbiota, possibly because of lower consumption of fruit and vegetables, in persons with higher DAL. Prior evidence has suggested that gut microbiota are related to migraines64. Furthermore, patients with higher DAL were found to have lower magnesium intake, in our study. It has been shown that in those experiencing migraine attacks, brain magnesium levels declined65. This is mainly due to the role of magnesium in the human buffering system that acts to balance the acid–base equilibrium under acidic conditions66.
There are some strengths and limitations that need to be addressed. First, this is the first investigation that has examined the association between two different measures of DAL and migraine headache frequency, duration, severity, and NO concentrations. Second, dietary intake and the outcomes of interest were assessed through the application of validated questionnaires and laboratory tests. Finally, several possible confounders were taken into account in our analysis. Notwithstanding these strengths, we should acknowledge some limitations in the interpretation of our findings. First, as we have previously mentioned, migraine patients might change their food intake preferences, and thus, the causal relationship cannot be inferred due to the cross-sectional design of the study. Second, despite using validated questionnaires, patients’ responses were subjective, based on their memory, which could lead to inevitable measurement errors. Third, there might still be some residual confounders that we did not consider in our analysis. Finally, although both male and female patients were included in our investigation, we were not able to do a sex-stratified analysis because of the small male sample size. This study was performed on Iranian patients suffering from migraine, therefore, extrapolation of our results to other populations should be made with caution.
Conclusion
In conclusion, we found PRAL and NEAP to be significantly related to migraine headache frequency. We also observed a significant association between NEAP and HIT-6 scores. However, we did not detect such associations in the case of migraine headache duration and severity, as well as NO concentrations. Further well-designed studies on different populations are needed to confirm our findings.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Steiner, T. J., Stovner, L. J., Jensen, R., Uluduz, D. & Katsarava, Z. Migraine remains second among the world’s causes of disability, and first among young women: Findings from GBD2019. J. Headache Pain 21, 137. https://doi.org/10.1186/s10194-020-01208-0 (2020).
Di Lorenzo, C. et al. Cortical functional correlates of responsiveness to short-lasting preventive intervention with ketogenic diet in migraine: A multimodal evoked potentials study. J. Headache Pain 17, 1–10 (2016).
Pietrobon, D. & Moskowitz, M. A. Pathophysiology of migraine. Annu. Rev. Physiol. 75, 365–391 (2013).
Beh, S. C., Masrour, S., Smith, S. V. & Friedman, D. I. The spectrum of vestibular migraine: Clinical features, triggers, and examination findings. Headache J. Head Face Pain 59, 727–740 (2019).
Weatherall, M. W. The diagnosis and treatment of chronic migraine. Ther. Adv. Chronic Dis. 6, 115–123. https://doi.org/10.1177/2040622315579627 (2015).
Buse, D., Manack, A., Serrano, D., Turkel, C. & Lipton, R. Sociodemographic and comorbidity profiles of chronic migraine and episodic migraine sufferers. J. Neurol. Neurosurg. Psychiatry 81, 428–432 (2010).
Goadsby, P. J. et al. 21st century headache: Mapping new territory. J. Headache Pain 22, 1–4 (2021).
Quade, B. N., Parker, M. D. & Occhipinti, R. The therapeutic importance of acid-base balance. Biochem. Pharmacol. 183, 114278–114278. https://doi.org/10.1016/j.bcp.2020.114278 (2021).
Aryal, D., Roy, T., Chamcheu, J. C. & Jackson, K. E. Chronic metabolic acidosis elicits hypertension via upregulation of intrarenal angiotensin ii and induction of oxidative stress. Antioxidants 10, 2 (2021).
De Simone, R. & Ranieri, A. The role of intracranial hypertension in the chronification of migraine. Neurol. Sci. 36, 23–28 (2015).
Capellini, V. K., Restini, C. B., Bendhack, L. M., Evora, P. R. & Celotto, A. C. The effect of extracellular pH changes on intracellular pH and nitric oxide concentration in endothelial and smooth muscle cells from rat aorta. PLoS ONE 8, e62887 (2013).
Malhotra, R. Understanding migraine: Potential role of neurogenic inflammation. Ann. Indian Acad. Neurol. 19, 175–182. https://doi.org/10.4103/0972-2327.182302 (2016).
Osuna-Padilla, I., Leal-Escobar, G., Garza-García, C. & Rodríguez-Castellanos, F. Dietary acid load: Mechanisms and evidence of its health repercussions. Nefrología (English Edition) 39, 343–354 (2019).
Adeva, M. M. & Souto, G. Diet-induced metabolic acidosis. Clin. Nutr. 30, 416–421 (2011).
Ariyanfar, S. et al. Fruit and vegetable intake and odds of pediatric migraine. Nutr. Food Sci. 50, 829 (2019).
Razeghi Jahromi, S., Ghorbani, Z., Martelletti, P., Lampl, C. & Togha, M. Association of diet and headache. J. Headache Pain 20, 1–11 (2019).
Askarpour, M., Sheikhi, A., Khorsha, F., Togha, M. & Mirzaei, K. Associations between dietary acid load and migraine headache severity and duration among women: A cross-sectional study. J. Iran. Med. Council 4, 93–103 (2021).
Olesen, J. Headache Classification Committee of the International Headache Society (IHS) the international classification of headache disorders, asbtracts. Cephalalgia 38, 1–211 (2018).
Willett, W. Issues in analysis and presentation of dietary data. In Nutritional Epidemiology (ed. Willett, W. C.) 321–346 (Oxford University Press, 1998).
Esfahani, F. H., Asghari, G., Mirmiran, P. & Azizi, F. Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the Tehran lipid and glucose Study. J. Epidemiol. 20, 150–158 (2010).
Ghaffarpour, M., Houshiar-Rad, A. & Kianfar, H. The manual for household measures, cooking yields factors and edible portion of foods. Tehran Nashre Olume Keshavarzy 7, 42–58 (1999).
Remer, T., Dimitriou, T. & Manz, F. Dietary potential renal acid load and renal net acid excretion in healthy, free-living children and adolescents. Am. J. Clin. Nutr. 77, 1255–1260 (2003).
Frassetto, L. A., Todd, K. M., Morris, R. C. Jr. & Sebastian, A. Estimation of net endogenous noncarbonic acid production in humans from diet potassium and protein contents. Am. J. Clin. Nutr. 68, 576–583 (1998).
Zandifar, A. et al. Reliability and validity of the Persian HIT-6 questionnaire in migraine and tension-type headache. Pain Pract. 14, 625–631 (2014).
Hajihashemi, P., Askari, G., Khorvash, F., Reza Maracy, M. & Nourian, M. The effects of concurrent Coenzyme Q10, L-carnitine supplementation in migraine prophylaxis: A randomized, placebo-controlled, double-blind trial. Cephalalgia 39, 648–654 (2019).
Moghaddam, M. B. et al. The Iranian version of international physical activity questionnaire (IPAQ) in Iran: Content and construct validity, factor structure, internal consistency and stability. World Appl. Sci. J. 18, 1073–1080 (2012).
Steiner, T. J., Stovner, L. J., Vos, T., Jensen, R. & Katsarava, Z. Migraine is first cause of disability in under 50s: Will health politicians now take notice? J. Headache Pain 19, 1–4 (2018).
Mahmoud, A. N. et al. Migraine and the risk of cardiovascular and cerebrovascular events: A meta-analysis of 16 cohort studies including 1,152,407 subjects. BMJ Open 8, e020498 (2018).
Burch, R. C., Buse, D. C. & Lipton, R. B. Migraine: Epidemiology, burden, and comorbidity. Neurol. Clin. 37, 631–649 (2019).
Arab, A., Khorvash, F., Karimi, E., Hadi, A. & Askari, G. Associations between adherence to Mediterranean dietary pattern and frequency, duration, and severity of migraine headache: A cross-sectional study. Nutr. Neurosci. https://doi.org/10.1080/1028415X.2021.2009162 (2021).
Arab, A., Khorvash, F., Kazemi, M., Heidari, Z. & Askari, G. Effects of the dietary approaches to stop hypertension (DASH) diet on clinical, quality of life, and mental health outcomes in women with migraine: A randomised controlled trial. Br. J. Nutr. https://doi.org/10.1017/S000711452100444X (2021).
Verrotti, A. et al. Migraine and obesity: Metabolic parameters and response to a weight loss programme. Pediatr. Obes. 10, 220–225 (2015).
Bond, D. S., Roth, J., Nash, J. M. & Wing, R. R. Migraine and obesity: Epidemiology, possible mechanisms and the potential role of weight loss treatment. Obes. Rev. 12, e362–e371 (2011).
Vo, M. et al. Body mass index and adult weight gain among reproductive age women with migraine. Headache J. Head Face Pain 51, 559–569 (2011).
Kolotkin, R. L. & Andersen, J. R. A systematic review of reviews: Exploring the relationship between obesity, weight loss and health-related quality of life. Clin. Obes. 7, 273–289. https://doi.org/10.1111/cob.12203 (2017).
López-Mesonero, L. et al. Smoking as a precipitating factor for migraine: A survey in medical students. J. Headache Pain 10, 101–103 (2009).
Aras, Y. G., Güngen, B. D., Kotan, D. & Güngen, A. C. Effect of smoking on migraine attack frequency in patients with migraines. Acıbadem Üniv. Sağlık Bilimleri Dergisi 2, 75–78 (2016).
Amin, F. M. et al. The association between migraine and physical exercise. J. Headache Pain 19, 1–9 (2018).
Pelzer, N. et al. Linking migraine frequency with family history of migraine. Cephalalgia 39, 229–236 (2019).
Fagernaes, C. et al. Blood pressure as a risk factor for headache and migraine: A prospective population-based study. Eur. J. Neurol. 22, 156-e111 (2015).
Goldenberg, M., Danovitch, I. & IsHak, W. W. Quality of life and smoking. Am. J. Addict. 23, 540–562. https://doi.org/10.1111/j.1521-0391.2014.12148.x (2014).
Pucci, G. C., Rech, C. R., Fermino, R. C. & Reis, R. S. Association between physical activity and quality of life in adults. Rev. Saude Publica 46, 166–179. https://doi.org/10.1590/s0034-89102012000100021 (2012).
Vagetti, G. C. et al. Association between physical activity and quality of life in the elderly: A systematic review, 2000–2012. Rev. Bras. de Psiquiatr. (Sao Paulo) 36, 76–88. https://doi.org/10.1590/1516-4446-2012-0895 (2014).
Marker, A. M., Steele, R. G. & Noser, A. E. Physical activity and health-related quality of life in children and adolescents: A systematic review and meta-analysis. Health Psychol. 37, 893–903. https://doi.org/10.1037/hea0000653 (2018).
Riley, E., Chang, J., Park, C., Kim, S. & Song, I. Hypertension and health-related quality of life (HRQoL): Evidence from the US hispanic population. Clin. Drug Investig. 39, 899–908. https://doi.org/10.1007/s40261-019-00814-4 (2019).
Akter, S. et al. High dietary acid load is associated with increased prevalence of hypertension: The Furukawa nutrition and health study. Nutrition 31, 298–303 (2015).
Abbasalizad Farhangi, M., Nikniaz, L. & Nikniaz, Z. Higher dietary acid load potentially increases serum triglyceride and obesity prevalence in adults: An updated systematic review and meta-analysis. PLoS ONE 14, e0216547 (2019).
Woolcott, C. G., Dishman, R. K., Motl, R. W., Matthai, C. H. & Nigg, C. R. Physical activity and fruit and vegetable intake: Correlations between and within adults in a longitudinal multiethnic cohort. Am. J. Health Promot. 28, 71–79. https://doi.org/10.4278/ajhp.100917-QUAN-312 (2013).
Alakaam, A. A. H. & Lemacks, J. L. Fruit and vegetable consumption, fat intake, and physical activity participation in relation to socio-demographic factors among medically underserved adults. AIMS Public Health 2, 402 (2015).
Alam, I., Alam, I., Paracha, P. I. & Pawelec, G. Higher estimates of daily dietary net endogenous acid production (NEAP) in the elderly as compared to the young in a healthy, free-living elderly population of Pakistan. Clin. Interv. Aging 7, 565–573. https://doi.org/10.2147/cia.s37158 (2012).
Cupisti, A. et al. Non-traditional aspects of renal diets: Focus on fiber, alkali and vitamin K1 intake. Nutrients 9, 444 (2017).
Nazari, F. & Eghbali, M. Migraine and its relationship with dietary habits in women. Iran. J. Nurs. Midwifery Res. 17, S65-71 (2012).
Hammond, N. G. & Colman, I. The role of positive health behaviors in the relationship between early life stress and migraine. Headache J. Head Face Pain 60, 1111–1123 (2020).
Hajjarzadeh, S., Mahdavi, R., Shalilahmadi, D. & Nikniaz, Z. The association of dietary patterns with migraine attack frequency in migrainous women. Nutr. Neurosci. 23, 724–730 (2020).
Mousavi, M. et al. The association between dietary acid load and odds of migraine: A case-control survey. Neurol. Ther. 10, 335–348. https://doi.org/10.1007/s40120-021-00247-2 (2021).
Flegal, K. M., Graubard, B. I., Williamson, D. F. & Cooper, R. S. Reverse causation and illness-related weight loss in observational studies of body weight and mortality. Am. J. Epidemiol. 173, 1–9 (2011).
Celotto, A. et al. Acute but not chronic metabolic acidosis potentiates the acetylcholine-induced reduction in blood pressure: An endothelium-dependent effect. Braz. J. Med. Biol. Res. https://doi.org/10.1590/1414-431x20155007 (2015).
Wu, T. et al. Associations between dietary acid load and biomarkers of inflammation and hyperglycemia in breast cancer survivors. Nutrients 11, 1913 (2019).
Gilchrist, M., Winyard, P. G. & Benjamin, N. Dietary nitrate–good or bad? Nitric Oxide 22, 104–109 (2010).
Ostrowska, J., Janiszewska, J. & Szostak-Węgierek, D. Dietary acid load and cardiometabolic risk factors—A narrative review. Nutrients 12, 3419. https://doi.org/10.3390/nu12113419 (2020).
Woldeamanuel, Y. W., Sanjanwala, B. M. & Cowan, R. P. Endogenous glucocorticoids may serve as biomarkers for migraine chronification. Ther. Adv. Chronic Dis. 11, 2040622320939793 (2020).
Gardener, H. et al. Hypertension and migraine in the Northern Manhattan Study. Ethn. Dis. 26, 323 (2016).
Peterlin, B. L., Rosso, A. L., Rapoport, A. M. & Scher, A. I. Obesity and migraine: The effect of age, gender and adipose tissue distribution. Headache J. Head Face Pain 50, 52–62 (2010).
Arzani, M. et al. Gut-brain axis and migraine headache: A comprehensive review. J. Headache Pain 21, 1–12 (2020).
Maier, J. A., Pickering, G., Giacomoni, E., Cazzaniga, A. & Pellegrino, P. Headaches and magnesium: Mechanisms, bioavailability, therapeutic efficacy and potential advantage of magnesium pidolate. Nutrients 12, 2660. https://doi.org/10.3390/nu12092660 (2020).
Nijenhuis, T., Renkema, K. Y., Hoenderop, J. G. & Bindels, R. J. Acid-base status determines the renal expression of Ca2+ and Mg2+ transport proteins. J. Am. Soc. Nephrol. 17, 617–626 (2006).
Acknowledgements
The authors wish to thank all participants who kindly contributed to the study.
Funding
This study was funded by Isfahan University of Medical Sciences, Isfahan, Iran.
Author information
Authors and Affiliations
Contributions
Conception and Design: A.A., G.A., F.K. Acquisition of Data: A.A., K.L., F.K. Analysis and Interpretation of Data: A.A., H.M. Drafting the Manuscript: A.A., K.L. Revising Manuscript for Intellectual Content: A.A., G.A., F.K., H.M., K.L., A.F.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lotfi, K., Askari, G., Mohammad, H. et al. Association between dietary acid load and clinical features of migraine headaches among Iranian individuals. Sci Rep 12, 2460 (2022). https://doi.org/10.1038/s41598-022-06515-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-06515-x
- Springer Nature Limited