Abstract
Fibular free flap (FFF) is frequently used for reconstruction requiring vascularized bone. Thus, understanding its vasculature variation is crucial. This study investigates the popliteal artery branching variations in Thai cadavers and compares them with previous studies. One hundred and sixty-two legs from 81 formalin-embalmed cadavers were dissected. The popliteal artery branching patterns were classified. The previous data retrieved from cadaveric and angiographic studies were also collected and compared with the current study. The most common pattern is type I-A (90.7%). For the variants, type III-A was the majority among variants (6.2%). Type IV-A, hypoplastic peroneal artery, was found in one limb. A symmetrical branching pattern was found in 74 cadavers. Compared with cadaveric studies, type III-B and III-C are significantly common in angiographic studies (p = 0.015 and p = 0.009, respectively). Type I-A is most common according to previous studies. Apart from this, the prevalence of type III-A variant was higher than in previous studies. Furthermore, type III-B and III-C are more frequent in angiographic studies which might be from atherosclerosis. Thus, if the pre-operative CTA policy is not mandatory, the patients at risk for atherosclerosis and population with high variants prevalence should undergo pre-operative CTA with cost-effectiveness consideration.
Similar content being viewed by others
Introduction
The fibular free flap (FFF) was introduced in 1975 by Taylor and colleagues1,2. This flap was frequently used for reconstructions, especially in defects which require vascularized bone3. The fibula is mainly supplied by the peroneal artery (PR) which has a parallel course along the fibula. PR provides the nutrient branch and several periosteal branches2. This vascular anatomy allows multiple osteotomy sites in this bone, which is necessary for reconstructive surgery such as mandibular reconstruction4,5.
Popliteal artery (PA) and its collaterals, including peroneal artery (PR), anterior tibial artery (AT), and posterior tibial artery (PT), are the main blood supply of the lower leg5. The AT arises from PA followed by the tibioperoneal trunk that later divides into PT and PR6. In 1989, Kim et al.6 proposed a classification modified from Lippert et al. Abou-Foul et al.5 proposed additional variants from Kim et al.’s classification. The later classification of Kim et al. together with Abou-Foul et al. are widely used in literature and studies in PA and its collaterals.
Regarding the variation of popliteal artery branching pattern, it has been proposed that embryogenic regression of sciatic artery, a primitive artery of the lower limb bud, and formation of the femoral artery are the antecedent determinants of PA branching variants7.
Usually, PR terminates above the ankle joint and contributes less to pedal circulation than AT and PT8. However, congenital abnormalities of AT and PT make PR become the dominant blood supply of pedal perfusion6. Type III variants, according to Kim et al. and Abou-Foul et al. studies, they categorized as having hypoplastic-aplastic of AT, PT, and type IV, hypoplastic-aplastic PR which precludes harvesting of vascularized FFF3,9,10. Harvesting of FFF together with PR in these vascular variants may result in foot ischemia of the donor’s leg or unusable fibular flap, respectively11.
Accumulating knowledge regarding PA branching patterns may facilitate surgeons in harvesting vascularized FFF and prevent severe donor site morbidities. To our best knowledge, there are several reports on the differences in prevalence of the popliteal artery variation. These differences do not solely result from ethnicity factor. Furthermore, the reports on PA branching pattern variation in the Asian population are limited11,12,13. In general, the Computed Tomography Angiography (CTA) is a mandatory policy for pre-operative planning of harvesting FFF in several centers. However, in some situations, such as excessive contrast media-level from pre-operative tumor imaging, limited contrast media amount in renal insufficiency patient which requires a separate session of CTA. Therefore, the pre-operative CTA might not be applicable. The cost-effectiveness of pre-operative leg CTA should also be considered8,14.
Hence, this study aims to investigate the congenital variation of PA branching by means of cadaveric dissection and compare the prevalence differences between angiographic and cadaveric studies in order to find out the cause of the difference. This will serve as a guidance for the currently controversial decision in pre-operative leg CTA and as baseline information for surgical procedure application.
Results
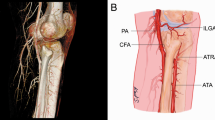
One hundred and sixty-two lower extremities were harvested from 81 cadavers. The average age at death is 79.3 years, ranging between 23 and 100 years (Table 1). According to the type of popliteal artery branching, we found that type I-A, the common pattern, was the most common type in this study (90.7%). The variant patterns were found in 15 of 162 limbs (9.3%). Among these variants, the most common variant in this study was type III-A, hypoplasia or aplasia of PT (6.2%), followed by type I-B (trifurcation of AT, PR, and PT), type II-B (a high division of PA), and IV-A (hypoplasia of PR) with the percentage of 1.2%, 1.2%, and 0.6% respectively (Table 2). Other branching patterns, which were not mentioned above, were not found in this study (Fig. 1). We have noticed that type III-A (absent or hypoplastic PT) limbs have a pedal arterial network originating from AT and distal PR, replacing the absence of PT.
An illustration of popliteal artery (PA) and its branches following classification by Kim et al. and Abou-Foul et al. The popliteal artery branching patterns are classified into 4 major types (I–IV) and divided into 12 subtypes. To note, Type I-A, I-B, II-B, III-A, and IV-A are found in this study (indicated by highlighted in blue rectangles). Type I-A: The common pattern of the popliteal artery and its branches. Type I-B: Trifurcation, AT, PT, and PR arise from the same point, Type I-C: The PT is the first branch, then AT and PR arise from common trunk. Type II-A: The AT arises above the knee joint. Type II-B the PT arises above the knee joint. Type II-C the PR arises above the knee joint. Type III-A: Hypoplastic or aplastic of PT and distal PT replaced by PR. Type III-B hypoplastic or aplastic of AT and dorsalis pedis artery is replaced by PR. Type III-C: hypoplastic or aplastic of both AT and PT results in dominant PR, also called “Peronea arteria magna (PAM)”, which distal PT and dorsalis pedis artery are replaced by PR. Type IV-A: Hypoplastic of PR. Type IV-B: Aplastic of PR. Type III-A and III-B have surgical significance due to the fact that the distal limb will be only supplied by remaining AT or PT, respectively, after FFF harvesting. Type III-C, the dominance of PR without AT and PT supply distal limb, which is contraindicated for FFF harvesting due to the unusable flap. PA popliteal artery, AT anterior tibial artery, PT posterior tibial artery, and PR peroneal artery.
When comparing both legs, 74 cadavers had symmetrical arterial branching pattern. Seventy cadavers in the symmetrical pattern group had the type I-A pattern, and the remaining had the symmetrical variant pattern in both legs. Asymmetrical branching pattern was found in 7 cadavers composed of a common pattern in one leg and variant type in another leg (Table 2).
Discussion
The popliteal artery branching patterns were classified by the classification of Kim et al. and Abou-Foul et al. into 12 subtypes. Type I-A is common in this study (90.7%). The major variant type in this study is type III-A, which is hypoplasia or aplasia of PT. This variant is found in 10 out of 162 limbs (6.2%). Type III-A pattern is also the most common variant pattern in South Korea, 5.1%13 and 4.8%12; Turkey, 3.5%15 and 5.6%16 and USA 3.8%6 (Table 3).
The prevalence of type III-A in this study is higher than that found in the previous studies (Table 3). Thus, it suggests that the Thai population might have a higher prevalence of type III-A. As AT will be the only major blood supply for pedal circulation after FFF harvesting in type III-A pattern, donor site morbidity might occurs10. Hence, FFF harvest together with PR in type III-C variant, the dominant peroneal artery, and type IV, hypoplasia-aplasia of PR, may lead to distal limb ischemia of the donor’s leg or unusable fibular flap, respectively11.
As the AT arises as a branch of the PA while PT is formed by an anastomosis between PA and early distal femoral artery during embryogenesis7, it is hypothesized that the high prevalence of type III-A among studies might occur from abnormal formation of the arterial system during embryogenesis which results in higher prevalence of III-A than III-B in most studies (Table 3). Other variants found in this study are type I-B, II-B, and IV-A with the percentage of 1.2%, 1.2%, and 0.6%, respectively. Other patterns, which were not mentioned above, were not found in this study.
It was found that only 70 out of 81 cadavers have symmetrical common PA branching patterns compared to both legs due to the high number of this typical symmetrical pattern. FFF harvesting can be performed on at least one leg in most cases. However, the other 7, out of 81 cadavers, have asymmetrical patterns, common pattern in one leg and a variant in the other (Table 2). Therefore, if we found the variant pattern in one leg intraoperatively, the likelihood of the common pattern in the contralateral leg was 63.6%.
Typically, the distal AT and PT pulse are palpable at just above the foot's dorsum and medial malleolus, respectively10. Type III-A variant, hypoplasia or aplasia of the PT, leading to the replacement of distal PT by the PR 6. Our findings were also similar to prior study6. In this case, the pulse behind the medial malleolus might be palpable. For this reason, palpation of a distal pulse was unreliable for indicating the presence of PT.
With regard to other reports, the frequent variant was type III, as reported in South Korea, Turkey, and the USA. This suggested that the risk of serious complications after harvesting of FFF was similar among these countries (Table 3). In addition, type IV-A, hypoplastic PR, was found at a rate of 0.6% in our study and 0.1% in Turkey15.
Comparison between angiographic studies and cadaveric studies is shown in (Table 3). Type III-B and III-C patterns are mainly found in angiographic studies. The prevalence of these variants is different with statistically significant between angiographic study and cadaveric study (independent t-test at α = 0.05; p = 0.015 for type III-B and p = 0.009 for type III-C) (Table 4). We propose that atherosclerotic change of vessels might interfere with angiographic study’s interpretation, whereas cadaveric study dissects vessels from extraluminal. From this point and the fact that the peroneal artery is less involved by atherosclerotic change5, the prevalence of variant type III-B and III-C in the angiographic study might be acquired atherosclerosis of AT and PT. Hence, the decision-making for fibula free flap reconstruction in terms of the prevalence of popliteal artery branching variants should be considered by atherosclerosis risk. From the fact that the young patients who generally have less atherosclerosis risk might have benefited from cadaveric-based prevalence since the cadaveric studies investigate vessels from extraluminal which represent the congenital branching patterns of individuals. On the contrary, the old patients who mostly have atherosclerosis should be considered by the angiographic study because the acquired variants might play a role.
For the surgical planning of FFF harvesting, pre-operative leg CTA is mandatory in some centers. If mandatory leg CTA policy is not applicable, which might be from the cost-effectiveness8,14 in low prevalence of variants or limited amount of contrast media from patient’s underlying disease, the patient should be assessed by the atherosclerosis risk. For the patient who is at risk for atherosclerosis, he/ she should undergo pre-operative CTA due to the increased chance of acquired variants from atherosclerosis. However, the patient with low atherosclerosis risk and low prevalence of variants in the population can go on surgery with careful intraoperative evaluation. The prevalence of variants should be referred from cadaveric studies since the prevalence is similar to the congenital prevalence (Fig. 2).
A schematic overview of pre-operative leg CTA in fibular free flap harvesting. If mandatory leg CTA policy is not applicable, which might be from the low prevalence of variants, limited contrast media amount from renal impairment, the leg CTA should be done following an atherosclerosis risk assessment. *The decision-making at this point should be based upon cost-effectiveness8,14 of leg CTA and prevalence in each population. To elaborate, in the low-risk for atherosclerosis group, the prevalence of variants should be referred from cadaveric studies since the prevalence is similar to the congenital prevalence. By contrast, patients at risk for atherosclerosis have a higher rate of acquired variants. FFF fibular free flap, CTA computed tomography angiography.
However, further study of each branching type prevalence, which is categorized by age group, might help study the effects of atherosclerosis in PA and its collaterals. Then we might find a cutting point that can designate the benefit of using angiographic studies.
Limitations of the study
There are some limitations to this study. First, this is an observational study using cadaveric dissection. The pre-mortem angiographic study of type III in patients could not be found in the first place. Thus, this was in contrast to what was found as type I in cadaveric dissection. It focused on demonstrating a case of acquired type III due to atherosclerosis change. Second, the number of cadavers in this study was relatively low compared to the number of cases in the angiographic study. Finally, this study highlighted popliteal artery branching patterns and arterial supply of fibula. Further study on the venous system of these areas should be considered.
Materials and methods
This study was designed to meet criteria established in Helsinki declaration guidelines for research involving human subjects. Informed consent for donation to educational purposes and scientific research had been signed before death by the donors or after death by relatives, according to the local guidelines. This study was approved by the Institutional Review Board (IRB) of Faculty of Medicine Siriraj Hospital, Mahidol University (477/2564). The cadaver anonymity has been preserved. All methods were performed in accordance with the relevant guidelines and regulations described in the proposal submitted to the Ethical Committee.
The arteries of 168 lower limbs from 84 cadavers were dissected after a medical student’s routine cadaveric study, which has not been dissected in the interested area 162 lower limbs from 81 cadavers were recruited after exclusion criteria were applied. The cadavers in this study were embalmed immediately after death by injecting the solution containing formalin, glycerin, 95% ethanol, phenol, and water via the right femoral artery then immersed in the embalming solution consist of glycerin, carbolic acid, and water for 6 months.
Regarding the dissection methods, 162 lower limbs were separated from the trunk. Dissection of arteries and their collaterals was operationalized under Siriraj hospital’s laboratory manual. Veins in study area were sacrificed. The pattern of arterial branching and their relation to popliteus muscle was recorded.
Demographic data of cadavers and types of popliteal artery branching pattern according to classification by Kim et al.6 and Abou-Foul et al.5 were presented with descriptive statistics, including mean, range, and percentage. The differences in angiographic and cadaveric study variants were done using the Chi-square test and p-value under IBM SPSS Statistics for Windows, version 26.0 (IBM Corp., Armonk, NY, USA). A p-value lower than 0.05 was statistically significant.
Conclusion
In order to harvest FFF safely, it is crucial to understand the arterial supply and anatomical variation of popliteal artery. Although type I-A is the most common pattern according to previous studies, it should be aware that there is a discrepancy in the prevalence of type III-B and III-C, which are mainly found in angiographic studies compared to cadaveric studies with statistically significant (p = 0.015 for type III-B and p = 0.009 for type III-C). Atherosclerosis might be the underlying of these differences.
The decision-making for pre-operative CTA for fibula free flap reconstruction in terms of the prevalence of popliteal artery branching variants should be considered by atherosclerosis risk. If pre-operative CTA policy is not mandatory, the authors suggest a selective CTA policy in patients at risk for atherosclerosis or high prevalence of variants in the population to select the suitable donor limb.
References
Taylor, G. I., Miller, G. D. & Ham, F. J. The free vascularized bone graft. A clinical extension of microvascular techniques. Plast. Reconstruct. Surg. 55, 533–544 (1975).
Taylor, G. I., Wilson, K. R., Rees, M. D., Corlett, R. J. & Cole, W. G. The anterior tibial vessels and their role in epiphyseal and diaphyseal transfer of the fibula: Experimental study and clinical applications. Br. J. Plast. Surg. 41, 451–469. https://doi.org/10.1016/0007-1226(88)90001-x (1988).
Young, D. M., Trabulsy, P. P. & Anthony, J. P. The need for preoperative leg angiography in fibula free flaps. J. Reconstr. Microsurg. 10, 283–287. https://doi.org/10.1055/s-2007-1006596 (1994).
Hidalgo, D. A. Fibula free flap: A new method of mandible reconstruction. Plast. Reconstr. Surg. 84, 71–79 (1989).
Abou-Foul, A. K. & Borumandi, F. Anatomical variants of lower limb vasculature and implications for free fibula flap: Systematic review and critical analysis. Microsurgery 36, 165–172. https://doi.org/10.1002/micr.30016 (2015).
Kim, D., Orron, D. E. & Skillman, J. J. Surgical significance of popliteal arterial variants: A unified angiographic classification. Ann. Surg. 210, 776–781. https://doi.org/10.1097/00000658-198912000-00014 (1989).
Mauro, M. A., Jaques, P. F. & Moore, M. The popliteal artery and its branches: Embryologic basis of normal and variant anatomy. AJR Am. J. Roentgenol. 150, 435–437. https://doi.org/10.2214/ajr.150.2.435 (1988).
Blackwell, K. E. Donor site evaluation for fibula free flap transfer. Am. J. Otolaryngol. 19, 89–95. https://doi.org/10.1016/s0196-0709(98)90101-6 (1998).
Chow, L. C., Napoli, A., Klein, M. B., Chang, J. & Rubin, G. D. Vascular mapping of the leg with multi-detector row CT angiography prior to free-flap transplantation. Radiology 237, 353–360. https://doi.org/10.1148/radiol.2371040675 (2005).
Hölzle, F. et al. Evaluation of the vessels of the lower leg before microsurgical fibular transfer. Part I: Anatomical variations in the arteries of the lower leg. Br. J. Oral Maxillofac. Surg. 49, 270–274. https://doi.org/10.1016/j.bjoms.2010.05.002 (2011).
Lutz, B. S., Wei, F.-C., Ng, S.-H., Chen, I.-H. & Chen, S. H. T. Routine donor leg angiography before vascularized free fibula transplantation is not necessary: A prospective study in 120 clinical cases. Plast. Reconstr. Surg. 103, 121–127. https://doi.org/10.1097/00006534-199901000-00019 (1999).
Choi, S. W., Kim, H. J., Koh, K. S., Chung, I. H. & Cha, I. H. Topographical anatomy of the fibula and peroneal artery in Koreans. Int. J. Oral Maxillofac. Surg. 30, 329–332. https://doi.org/10.1054/ijom.2001.0055 (2001).
Kil, S.-W. & Jung, G.-S. Anatomical variations of the popliteal artery and its tibial branches: Analysis in 1242 extremities. Cardiovasc. Intervent. Radiol. 32, 223–240. https://doi.org/10.1007/s00270-008-9460-z (2009).
Rosson, G. D. & Singh, N. K. Devascularizing complications of free fibula harvest: Peronea arteria magna. J. Reconstr. Microsurg. 21, 533–538. https://doi.org/10.1055/s-2005-922432 (2005).
Demirtaş, H. et al. Anatomic variations of popliteal artery: Evaluation with 128-section CT-angiography in 1261 lower limbs. Diagn. Interv. Imaging 97, 635–642. https://doi.org/10.1016/j.diii.2016.02.014 (2016).
Celtikci, P., Ergun, O., Durmaz, H. A., Conkbayir, I. & Hekimoglu, B. Evaluation of popliteal artery branching patterns and a new subclassification of the “usual” branching pattern. Surg. Radiol. Anat. 39, 1005–1015. https://doi.org/10.1007/s00276-017-1834-y (2017).
Manaster, B. J., Coleman, D. A. & Bell, D. A. Magnetic resonance imaging of vascular anatomy before vascularized fibular grafting. J. Bone Jt. Surg. Am. 72, 409–414 (1990).
Seres, L., Csaszar, J., Voros, E. & Borbely, L. Donor site angiography before mandibular reconstruction with fibula free flap. J. Craniofac. Surg. 12, 608–613. https://doi.org/10.1097/00001665-200111000-00021 (2001).
Day, C. P. & Orme, R. Opliteal artery branching patterns—An angiographic study. Clin. Radiol. 61, 696–699. https://doi.org/10.1016/j.crad.2006.03.014 (2006).
Lohan, D. G. et al. MR angiography of lower extremities at 3T: Presurgical planning of fibular free flap transfer for facial reconstruction. Am. J. Roentgenol. 190, 770–776. https://doi.org/10.2214/ajr.07.2753 (2008).
Sandhu, G. S. et al. Time-resolved and bolus-chase MR angiography of the leg: Branching pattern analysis and identification of septocutaneous perforators. AJR Am. J. Roentgenol. 195, 858–864. https://doi.org/10.2214/ajr.09.3766 (2010).
Mavili, E. et al. Popliteal artery branching patterns detected by digital subtraction angiography. Diagn. Interv. Radiol. 17, 80–83. https://doi.org/10.4261/1305-3825.DIR.3141-09.1 (2011).
Muhammad, A. & Muhammad, R. Variations in popliteal artery branching patterns. Int. J. Integr. Biol. 13, 4–18 (2012).
Akashi, M., Nomura, T., Sakakibara, S., Sakakibara, A. & Hashikawa, K. Preoperative MR angiography for free fibula osteocutaneous flap transfer. Microsurgery 33, 454–459. https://doi.org/10.1002/micr.22128 (2013).
Yanik, B., Bulbul, E. & Demirpolat, G. Variations of the popliteal artery branching with multidetector CT angiography. Surg. Radiol. Anat. 37, 223–230. https://doi.org/10.1007/s00276-014-1346-y (2015).
Calisir, C., Simsek, S. & Tepe, M. Variations in the popliteal artery branching in 342 patients studied with peripheral CT angiography using 64-MDCT. Jpn. J. Radiol. 33, 13–20. https://doi.org/10.1007/s11604-014-0373-2 (2015).
Oner, S. & Oner, Z. Popliteal artery branching variations: A study on multidetector CT angiography. Sci. Rep. 10, 8147. https://doi.org/10.1038/s41598-020-65045-6 (2020).
Piral, T., Germain, M. & Princ, G. Absence of the posterior tibial artery: Implications for free transplants of the fibula. Surg. Radiol. Anat. 18, 155–158. https://doi.org/10.1007/BF01795242 (1996).
Ozgur, Z., Ucerler, H. & Aktan Ikiz, Z. A. Branching patterns of the popliteal artery and its clinical importance. Surg. Radiol. Anat. 31, 357–362. https://doi.org/10.1007/s00276-008-0454-y (2009).
Lappas, D., Stavropoulos, N. A., Noussios, G., Sakellariou, V. & Skandalakis, P. Anatomic study of infrapopliteal vessels. Folia Morphol. (Warsz) 71, 164–167 (2012).
Olewnik, Ł et al. Variations in terminal branches of the popliteal artery: Cadaveric study. Surg. Radiol. Anat. 41, 1473–1482. https://doi.org/10.1007/s00276-019-02262-3 (2019).
Acknowledgements
The authors sincerely thank those who donated their bodies to science so that anatomical research could be performed. Results from such research can potentially increase humanity’s overall knowledge that can then improve patient health care. Therefore, these donors and their families deserve our highest gratitude. In addition, thanks go to Nachasa Khongchu from the Research Department, Faculty of Medicine Siriraj Hospital, Mahidol University for data analysis. Irin Chaikangwan, M.D. and Jiraya Prompattanapakdee, M.D. from Division of Plastic Surgery, Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University for data enrollment and technical issues.
Author information
Authors and Affiliations
Contributions
M.O.: Project development, cadaveric dissection, and data collection. P.J., and S.P.: Cadaveric dissection and data collection. N.K.: Data collection, data analysis, manuscript writing and editing. K.P.: Manuscript editing. N.Y.: Project initiation, project development, data analysis, manuscript writing and editing. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ongsiriporn, M., Jongpradubgiat, P., Pisittrakoonporn, S. et al. The congenital popliteal vasculature patterns in fibular free flap reconstruction by means of surgical anatomy in cadavers. Sci Rep 11, 19584 (2021). https://doi.org/10.1038/s41598-021-99203-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-99203-1
- Springer Nature Limited