Abstract
To evaluate birth outcomes in women with hypertensive disorders of pregnancy (HDP) and gestational diabetes mellitus (GDM), we used insurance data of Taiwan to evaluate 11 adverse neonatal outcomes of infants born to women with HDP (N = 7775) and with both HDP and GDM (HDP/GDM) (N = 1946), comparing to women with neither disorder (N = 19,442), matched by age. The impacts of preeclampsia/eclampsia were also evaluated. Results showed that Caesarean section delivery was near 1.7-fold greater in the HDP/GDM and HDP groups than in comparisons. The preterm delivery rates were more than threefold greater in HDP/GDM group and HDP group than in comparisons with adjusted odds ratios (aORs) of 4.84 (95% confidence interval (CI) 4.34–5.40) and 3.92 (95% CI 3.65–4.21), respectively, followed by jaundice (aORs 2.95 (95% CI 2.63–3.33) and 1.90 (95% CI 1.76–2.06)), and small gestation age (SGA) (aORs 6.57 (95% CI 5.56–7.75) and 5.81 (95% CI 5.15–6.55)). Incidence rates of birth trauma, patent ductus arteriosus, atrial septal defect, respiratory distress syndrome, and neonatal hypoglycemia were also higher in the HDP/GDM and HDP groups than in the comparison group. Most adverse outcomes increased further in women with preeclampsia or eclampsia. In conclusion, women with HDP are at elevated risks of adverse neonatal outcomes. Risks of most adverse outcomes increase further for women with both HDP and GDM. Preeclampsia or eclampsia may also contribute to these outcomes to higher risk levels. Every pregnant woman with these conditions deserves specialized prenatal care.
Similar content being viewed by others
Introduction
Hypertensive disorders of pregnancy (HDP) and gestational diabetes mellitus (GDM) are common disorders that may contribute to complications in pregnant women and newborns. The prevalence of HDP ranges from 5 to 10%1,2,3. Approximately 8.7–14% of pregnant women develop GDM4,5,6. Both disorders are important global public health concerns.
A WHO systemic analysis showed that hypertensive disorders accounted for 14.0% of maternal deaths in 2003–20097. Women with gestational hypertension (GHT) may progress to preeclampsia and eclampsia with proteinuria, edema, and tonic–clonic seizures after 20 weeks of gestation. These conditions can trigger acute liver rupture, chronic kidney disease, visual loss, and other maternal complications8,9,10,11,12. It can also pose a higher risk for adverse birth outcomes for the fetus13,14,15,16,17,18.
A multicenter study in the US found that neonates born to mothers with preeclampsia or GHT are 2.9-fold more likely to receive intensive care than those born to normotensive mothers19. Women with unmanaged GDM are also at an elevated risk of developing complications during pregnancy, delivery, and the postpartum period20,21,22,23,24. Poor glycemic control increases adverse infant outcomes as well25,26,27,28,29,30,31,32. Pregnant women may also experience both HDP and GDM33,34,35,36. Women with HDP or those with both HDP and GDM are at elevated risk for subsequent hypertension and DM after delivery33.
However, previous studies have rarely investigated the complications and adverse birth outcomes associated with co-existing GDM and HDP. Most studies have evaluated pregnant women with only one of these disorders. The presence of both disorders during pregnancy may pose a greater health impact on mothers and infants.
In this study, we used large insurance claims data to investigate risks of adverse obstetric and neonatal outcomes in pregnant women with HDP alone and with both HDP and GDM. We compared one obstetric and 11 adverse neonatal outcomes in these two groups of women, comparing to reference women without HDP and GDM. We further assessed whether preeclampsia or eclampsia during pregnancy contributed to adverse outcomes.
Results
Demographics characteristics of study groups
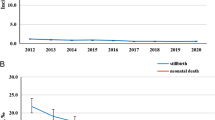
Age distributions were similar among the three study groups, with a mean age of approximately 33 years; 36.4% of women were 30–34 years old (Table 1). The comparison group had slightly less rural residents, but had higher white-collar employees. Baseline prevalence rates of comorbidities in the three study groups were all less than 0.5%. Figure 1 shows the increasing trends of annual incidence (per 100) in pregnant women with HDP and with both HDP/GDM. The annual incidence rates of HDP were higher than that of HDP/GDM and increased considerably from 2000 to 2012.
Obstetric and neonatal adverse outcomes
Table 2 shows that HDP/GDM and HDP groups were approximately 1.7-fold more likely than the comparisons to deliver infants using Cesarean section (C-section) (66.0% and 66.7% versus 37.9%, respectively). Rates of adverse neonatal outcomes were all higher in the HDP group than in the comparison group, and increased further in the HDP/GDM group except respiratory distress syndrome (RDS). The adjusted odds ratios (aORs) of preterm delivery were 3.92 (95% CI 3.64–4.21) and 4.84 (95% CI 4.34–5.40), respectively, for women with HDP and with HDP/GDM relative to comparisons. The rates of neonatal hypoglycemia were more than fivefold greater in the HDP group and HDP/GDM group than in the comparisons with aORs of 5.20 (95% CI 3.91–6.92) and 8.68 (95% CI 6.13–12.3), respectively. The rate of large gestation age (LGA) was much greater in the HDP/GDM group than in both the comparisons and the HDP group, with aORs of 31.7 (95% CI 16.5–60.9) relative to the comparisons and 19.4 (95% CI 9.01–41.9) compared to the HDP group.
Outcomes associated with preeclampsia and eclampsia
Table 3 shows that the C-section delivery rate increased steadily with hypertension status to the highest of 80.5% in women with eclampsia. The preterm delivery rate was much greater in women with preeclampsia or eclampsia than in women with only GHT and comparisons (30.6% or 29.0% versus 19.8% and 8.30%, respectively). Eclampsia or preeclampsia also led to higher risks of preterm delivery, small gestation age (SGA), patent ductus arteriosus (PDA), patent foramen oval PFO (ASD), RDS and neonatal hypoglycemia. Large differences existed for SGA rates with aORs of 10.8 (95% CI 7.42–15.8), 7.36 (95% CI 6.46–8.38) and 3.59 (95% CI 3.04–4.24) associated with eclampsia, preeclampsia and GHT, respectively.
Table 3 also shows that all rates of neonatal adverse outcomes were greater in the HDP/GDM group than in the HDP group. Most these adverse outcomes in HDP/GDM women with eclampsia or preeclampsia also increased further, to levels greater than those in HDP women with eclampsia or preeclampsia. The risk of delivering a LGA baby was particularly higher in HDP/GDM women (aOR = 21.9, 95% CI 10.1–47.6) and in those with preeclampsia (aOR = 44.5, 95% CI 22.0–89.9).
Discussion
It is well known that pregnant women with HDP or GDM are at elevated risks of subsequent adverse maternal and neonatal health conditions. Our study showed that HDP is associated with increased C-section delivery with higher preterm delivery and 9 adverse neonatal outcomes than comparisons without HDP. The incidence of HDP in our study was 2.41% (65,021/2,694,351). The recent Canadian statistics showed that hypertension affected approximately 7.0% of pregnant women3. Another recent study analyzed the national data of China and found a HDP rate of 3.89% (n = 270,982) among 6,970,032 pregnancies13. Our study revealed that 4.555% of women had a concomitant diagnosis of GDM and HDP. The presence of both HDP and GDM during pregnancy posed greater risks of adverse neonatal outcomes than the presence of HDP alone. The risks of most adverse outcomes increased to more higher levels in women with preeclampsia or eclampsia developed in the HDP group and HDP/GDM group.
Comparing neonatal outcomes between HDP and HDP/GDM groups
The effect of HDP in pregnant women varies among populations. A recent cross-sectional study based on 3,659,553 women with a live birth delivery among the US states found HDP affecting 4.3% to 9.3% pregnancies37. The risk of developing HDP in our study population might not higher than other population1,2,3,37. Our study found the preterm delivery in women with HDP was more than threefold higher than comparisons. An earlier US study showed that the adjusted relative risk of preterm delivery in women with HDP was 1.87 compared to references38. In our study, the highest incidence among other adverse neonatal outcomes in HDP women was jaundice, followed by SGA and RDS, with few cases of LGA. However, the estimated relative risk was the highest for RDS with an aOR of 6.18. The risk is higher than the finding in a US nest case–control study within the Calcium for Preeclampsia Prevention trial, with an aOR of 2.18 for RDS associated with HDP39. For premature infants, the RDS is a common cause of respiratory failure. This is due to insufficient production of pulmonary surfactant and the immature structure of the lung40. Previous studies found the impact of preeclampsia on RDS conflicting41,42,43,44,45. However, we are unable to conclude the impact of HTN on RDS because there is no data on antenatal corticosteroid use.
We found that children born to women with HDP/GDM had greater incidence adverse neonatal outcomes than children born to women with HDP, except RDS. Pregnant women with GDM are known at a higher risk of having newborns of LGA. A Swedish cohort study found an OR of 3.43 (95% CI 3.21–3.67) for LGA associated with GDM based on the birth registry data of 1,260,297 women27. This study did not evaluate LGA and SGA for women with both HDP and GDM. We note in our study that there were more neonatal SGA than LGA (12.5% versus 1.90%) born to women with HDP/GDM. However, the aOR of LGA was much greater than that of SGA (31.7 versus 6.57) relative to the comparison group. The corresponding aORs reduced to 21.9 and 5.22 for infants born to women with GHT/GDM. It seems hypertension may interact with diabetes exerting increased risk of adverse neonatal outcomes in pregnant women.
Preeclampsia or eclampsia impact
Our data also showed that most other investigated adverse neonatal outcomes increased further, in addition to the risk of preterm delivery and low birth weight, in women with preeclampsia or eclampsia; the impacts were even greater in the HDP/GDP group than in the HDP group.
Our data show that large portions of women in both the HDP group and HDP/GDM group developed preeclampsia (56.8% versus 43.7%, or 4415/7775 versus 851/1946), but 2.44% (n = 190) and 0.92% (n = 18) developed eclampsia, respectively. Infants born to pregnant women in the HDP group with preeclampsia or eclampsia developed had the highest SGA rates, with very low rate of LGA. Whereas infants born to the HDP/GDM group with preeclampsia were at the highest risk of LGA. The OR of giving birth to a LGA baby increased further to 44.5 in women with preeclampsia in the HDP/GDM group. This is an exceptional finding has not been reported previously22,42,44,45. A recent study evaluating 30,139 pregnancies in Ontario, Canada, also associated pre-pregnancy diabetes with increased risk of LGA with an adjusted relative risk of 28.9 in preterm births46. However, the absolute rate of LGA was smaller in our study than in the Ontario study (2.7% versus 6.4%).
Congenital malformations are associated with preterm delivery
Studies have associated GDM and hypertensive disorders with congenital defects, including congenital heart defects47,48,49,50, particularly in women with preterm preeclampsia51,52,53. A meta-analysis based on 15 cohort studies found a relative risk of 1.16 (1.07–1.25) for major congenital malformations in the offspring of women with GDM47. A Chinese study found that gestational diabetes is one of risk factors associated with the development of congenital heart disease based on the data of 90,796 infants48. A Demark study with 1,972,857 singleton pregnancies found a greater risk of offspring congenital heart defects in women with early preterm preeclampsia than in women with late preterm preeclampsia (OR 7.00 versus 2.82)52. Our study found elevated risks of PDA and PFO in both HDP group and HDP/GDM group, and increased further in women with Preeclampsia/GDM. However, we are unable to assess whether these neonatal abnormalities diagnosed were congenital defects without further follow up evaluation for these children. PFO and ASD are likely linked to prematurity. But, we found that VSD was the only adverse birth outcome of congenital defect presented in the 3 study groups ranging from 0.20 to 0.36%, which were not different between the groups.
Our study also found a high risk of neonatal hypoglycemia with an aOR of 10.5, in women with preeclampsia/GDM relative to comparisons. The development of neonatal hypoglycemia might be influenced by the early gestational age at delivery. Managing GDM by tight glycemic control during pregnancy is essential to effectively reduce the abnormalities. A secondary analysis from the North American Hyperglycemia and Adverse Pregnancy Outcome Study also found that women with GDM were at a 2.11-fold higher risk of neonatal hypoglycemia than those without GDM54. The development of neonatal hypoglycemia might be influenced by the early gestational age at delivery. Managing GDM by tight glycemic control during pregnancy is essential to effectively reduce the abnormalities.
Strengths and limitations
To the best of our knowledge, this is the first Asian study to evaluate multiple birth outcomes in pregnant women with HDP and HDP/GDM and in those who developed preeclampsia or eclampsia. Although this study was strengthened by the use of the large insurance claims database, there were several limitations. First, information on body mass index, lifestyle of drinking, smoking and diet, and family health history was unavailable to adjust for these potential confounders in data analyses. However, the impact from some of these factors might be minor because pregnant women are more likely to avoid unhealthy behaviors. Smoking and drinking are rare habits in women in Taiwan and obesity is not prevalent as well. The study results might not be generalizable to non-Chinese populations and populations with higher rates of obesity. Second, the HDP and HDP/GDM cohorts utilized more medical interventions, which might increase the diagnosis of adverse outcomes in these groups. Third, information on the severity of disorders during pregnancy was unavailable for analyses. Misclassification would tend to increase the observed magnitude associated with severe conditions. However, it is unlikely that we have misclassified women with preeclampsia or eclampsia, as these conditions made a strong impact that had not been previously reported. Fourth, we established groups of women with HDP and women with both HDP and GDM, without a group of GDM. Therefore, the impact associated with GDM alone or with the severity of GDM could not be evaluated in this study, but we were able to subdivide hypertensive disorders of pregnancy into pregnancy-induced hypertension and preeclampsia or eclampsia. Fifth, a high incidence of preterm delivery was observed in this study. However, we were unable to identify the spontaneous preterm delivery to further evaluate the attribution to the neonatal outcomes.
Conclusions
This study showed a steady increase in risks of adverse neonatal outcomes for pregnant women with HDP, HDP/GDM and those with preeclampsia or eclampsia. Because of the progressive nature of HDP and GDM, early delivery is usually recommended to minimize the maternal morbidity and mortality, especially for the more severe presentations of HDP or GDM, such as preeclampsia and eclampsia.
Our findings underscore the need for prenatal care with careful attention to pregnant women with HDP, particularly to women with both HDP and GDM. Obstetricians may need to screen for fetal abnormalities in pregnant women with these disorders, particularly in those with preeclampsia or eclampsia. It is important to detect and treat HDP and GDM early to reduce obstetrical complications and adverse neonatal outcomes, tight glycemic control and hypertension control are prudent. Future studies need to evaluate the risks and benefits of labor and Cesarean delivery for women with HDP and/or GDM.
Methods
Data sources
The Department of Health Insurance in Taiwan is a government-managed system established in 1995 through integration of 11 public insurance programs to create a universal insurance system, which is compulsory for all residents. Approximately 99% of the 23 million Taiwanese people have been covered in the program since 1997. The National Health Research Institutes (NHRI) of Taiwan established several data files of reimbursement claims available for research at the inception of 1997. For this study, we aimed to investigate the neonatal outcomes for women with a singleton pregnancy at their first birth. To minimize the inclusion of multiple pregnancies and multiple births, we used the whole population claims data for the period of 2000–2012.
To ensure the privacy of the participants, all the data were linked with surrogate identifications processed by NHRI before releasing to researchers. Information on patient demographic status and health care received were available. Diseases and other health care events were coded using the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM). The use of insurance claim data was approved by the Research Ethics Committee of China Medical University and Hospital, Taichung, Taiwan (CMUH104-REC2-115). We adhered to the principles in the Declaration of Helsinki in this study. Informed consent of patients was not required due to the retrospective design of the study and the use of scrambled data.
Study population
From the claims data of the whole female insured population (N = 14,678,205), we identified 2,694,351 women with pregnancy diagnosed from 2000 to 2012 in Taiwan (Fig. 2). Of these women 65,021 women had HDP (ICD-9-CM 642). The date of HDP diagnosis was defined as the index date. We exclude those with HDP diagnosed before the year of 2000; those with a history of diabetes, GDM and hypertension history (ICD-9-CM 250, 648.0, 648.8 and 401–405 respectively); and those younger than 14 or older than 45 years; and those with multiple birth history (ICD-9-CM 651, 652.6 and 761.5) or at this admission. Women with multifetal gestations were also excluded. Of the remaining 42,767 women with HDP were eligible for this study. Among them, 1946 women who had also developed GDM during pregnancy were identified as the HDP/GDM cohort. Among women with only HDP, we selected a cohort with a size fourfold (N = 7775) of the HDP/GDM cohort, frequency matched by age and the diagnosis year of HDP. From 2,629,330 pregnant women without HDP, we randomly selected a comparison cohort, with a size twofold of the combined size of HDP cohort and HDP/GDM cohort, frequency matched by age and pregnant year. The exclusion criteria used for selecting the HDP/GDM and HDP cohorts were applied for establishing the comparison cohort, with a sample size of 19,442 women.
Birth outcomes and associated factors
For each patient, we examined normal delivery (650) and Cesarean section (ICD-9 code operation 74), and 11 adverse neonatal outcomes from the birth records, including preterm delivery (ICD-9 code: 644 and 765.1), low birthweight (small for gestational age (SGA) (ICD-9 code: 765), large baby (large for gestational age (LGA)) (ICD-9 code: 766), birth trauma (ICD-9 code: 767), stillbirth (ICD-9 code: 768.0, 768.1), patent ductus arteriosus (PDA, ICD-9 code: 747.0), patent foramen ovale/atrial septal defect (PFO [ASD], ICD-9 code: 745.5), ventricular septal defect (VSD, ICD-9 code: 745.4), jaundice (ICD-9 code: 774), respiratory distress syndrome (RDS, ICD-9 code: 769), and neonatal hypoglycemia (ICD-9 code: 775.6). The demographic data file provided information on age (16–29, 30–34, 35–39, and 40–45 years), urbanization level, and occupation (white-collar, blue-collar, and others). We categorized all residential areas into five urbanization levels from the highest urbanized level as 1 to the lowest level as 5. We also searched for comorbidities that were potentially linked to obstetric birth outcomes including stroke (ICD-9-CM 430–438), heart failure (ICD-9-CM 428), ischemic heart disease (ICD-9-CM 410–414), renal disease (ICD-9-CM 580–589), placental abruption (ICD-9-CM 641.2), and obesity (ICD-9-CM 278, 783.1). All baseline comorbidities were defined before the index date.
Statistical analyses
We used SAS software version 9.4 (SAS Institute Inc., Cary, NC) to perform the data analysis for this study, with a p-value of < 0.05 considered statistically significant. The Chi-square test and Fisher's exact test were used to examine differences of categorical variables between HDP, HDP/GDM and comparison groups, including age, urbanization level and occupation, and comorbidities. Analysis of variance (ANOVA) was used to examine differences of mean ages among the three groups. Multivariable logistic regression was used to estimate the adjusted odds ratio (aOR) with 95% confidence interval (CI) of each birth outcome measured for the HDP group and the HDP/GDM group, relative to the comparison group. The aOR was estimated after controlling for age, urbanization level and occupation, and significant comorbidities at the baseline. The aOR of each birth outcome was also measured for women with HDP/GDM compared to women with HDP. We further calculated the aOR of each birth event associated with GHT, preeclampsia and eclampsia (ICD-9-CM 642.4–642.6) in the HDP group, and associated with GHT/GDM, preeclampsia and eclampsia in the HDP/GDM group, controlling for age, urbanization level, occupation, and comorbidity.
Data availability
The data that support the findings of this study were obtained from National Health Insurance Research database (NHIRD) of the Ministry of Health and Welfare, established by the National Health Research Institutes of Taiwan. The Ministry of Health and Welfare approved our use of the data. Any researcher interested in accessing this dataset can submit an application to the Ministry of Health and Welfare requesting access. We are not eligible to duplicate and disseminate the database. For further access to the database, please contact the Ministry of Health and Welfare (Email: stcarolwu@mohw.gov.tw) for further assistance. Taiwan Ministry of Health and Welfare Address: 488 Zhongxiao E. Rd. Sec. 6, Nangang Dist., Taipei 115, Taiwan (R.O.C.). Phone: + 886-2-8590-6848).
References
Kharakwal, S., Bala, S. & Yadav, U. K. Prevalence of hypertensive disorders of pregnancy in Bundelkhand region. Glob. J. Res. Anal. 6, 46–47 (2017).
Berhe, A. K., Kassa, G. M., Fekadu, G. A. & Muche, A. A. Prevalence of hypertensive disorders of pregnancy in Ethiopia: A systemic review and meta-analysis. BMC Pregnancy Childb. 18, 34 (2018).
Butalia, S. et al. Hypertension Canada’s 2018 Guidelines for the Management of Hypertension in Pregnancy. Can. J. Cardiol. 34, 526–531 (2018).
Nguyen, C. L., Pham, N. M., Binns, C. W., Duong, D. V. & Lee, A. H. Prevalence of gestational diabetes mellitus in Eastern and Southeastern Asia: A systematic review and meta-analysis. J. Diabetes Res. 2018, 6536974 (2018).
DeSisto, C. L., Kim, S. Y. & Sharma, A. J. Prevalence estimates of gestational diabetes mellitus in the United States, pregnancy risk assessment monitoring system (PRAMS), 2007–2010. Prev. Chronic Dis. 11, 1304415 (2014).
Eades, C. E., Cameron, D. M. & Evans, J. M. Prevalence of gestational diabetes mellitus in Europe: A meta-analysis. Diabetes Res. Clin. Pract. 129, 173–181 (2017).
Say, L. et al. Global causes of maternal death: A WHO systematic analysis. Lancet Glob. Health. 2, e323–e333 (2014).
American College of Obstetricians and Gynecologists & Task Force on Hypertension in Pregnancy. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet. Gynecol. 122, 1122–1131 (2013).
Rotem, R. et al. Association between hypertensive disorders of pregnancy and third stage of labor placental complications. Pregnancy Hypertens. 13, 166–170 (2018).
Hayase, M., Shimada, M. & Seki, H. Sleep quality and stress in women with pregnancy-induced hypertension and gestational diabetes mellitus. Women Birth. 27, 190–195 (2014).
Tanz, L. J. et al. Cardiovascular biomarkers in the years following pregnancies complicated by hypertensive disorders or delivered preterm. Pregnancy Hypertens. 13, 14–21 (2018).
Wallace, K. et al. Acute kidney injury in pregnancy and HELLP syndrome. FASEB J. 32, lb347 (2018).
Xiong, T. et al. Hypertensive disorders in pregnancy and stillbirth rates: A facility-based study in China. Bull World Health Organ. 96, 531–539 (2018).
Gemmell, L. et al. Hypertensive disorders of pregnancy and outcomes of preterm infants of 24 to 28 weeks’ gestation. J. Perinatol. 36, 1067–1072 (2016).
Lu, C. Q. et al. Pregnancy induced hypertension and outcomes in early and moderate preterm infants. Pregnancy Hypertens. 14, 68–71 (2018).
Villar, J. et al. Preeclampsia, gestational hypertension and intrauterine growth restriction, related or independent conditions?. Am. J. Obstet. Gynecol. 194, 921–931 (2006).
Maher, G. M. et al. Association of hypertensive disorders of pregnancy with risk of neurodevelopmental disorders in offspring a systematic review and meta-analysis. JAMA Psychiatr. 75, 809–819 (2018).
Curran, E. A. et al. Exposure to hypertensive disorders of pregnancy increases the risk of autism spectrum disorder in affected offspring. Mol. Neurobiol. 55, 5557–5564 (2018).
Habli, M., Levine, R. J., Qian, C. & Sibai, B. Neonatal outcomes in pregnancies with preeclampsia or gestational hypertension and in normotensive pregnancies that delivered at 35, 36, or 37 weeks of gestation. Am. J. Obstet. Gynecol. 197, 406.e1–e7 (2007).
Yogev, Y., Xenakis, E. M. & Langer, O. The association between preeclampsia and the severity of gestational diabetes: The impact of glycemic control. Am. J. Obstet. Gynecol. 191, 1655–1660 (2004).
Xiong, X., Saunders, L. D., Wang, F. L. & Demianczuk, N. N. Gestational diabetes mellitus: Prevalence, risk factors, maternal and infant outcomes. Int. J. Gynecol. Obstet. 75, 221–228 (2001).
Jovanovic, L. & Pettitt, D. J. Gestational diabetes mellitus. JAMA 286, 2516–2518 (2004).
Li, L. J. et al. Retinal vasculature and 5-year metabolic syndrome among women with gestational diabetes mellitus. Metabolism 83, 216–224 (2018).
Mak, J. K. L. et al. Gestational diabetes and postnatal depressive symptoms: A prospective cohort study in Western China. Women Birth. 32, e427–e431 (2019).
Boriboonhirunsarn, D. & Waiyanikorn, R. Emergency cesarean section rate between women with gestational diabetes and normal pregnant women. Taiwan J. Obstet. Gynecol. 55, 64–67 (2016).
Zeki, R. et al. Neonatal outcomes of live-born term singletons in vertex presentation born to mothers with diabetes during pregnancy by mode of birth: A New South Wales population-based retrospective cohort study. BMJ Paediatr. Open. 2, e000224 (2018).
Fadl, H. E., Ostlund, I. K., Magnuson, A. F. & Hanson, U. S. Maternal and neonatal outcomes and time trends of gestational diabetes mellitus in Sweden from 1991 to 2003. Diabet. Med. 27, 436–441 (2010).
Santamaria, A. et al. Clinical and metabolic outcomes in pregnant women at risk for gestational diabetes mellitus supplemented with myo-inositol: A secondary analysis from 3RCTs. Am. J. Obstet. Gynecol. 219, e330.e1–e6 (2018).
Pintaudi, B. et al. The risk stratification of adverse neonatal outcome in women with gestational diabetes (STRONG) study. Acta Diabetol. 55, 1261–1273 (2018).
Feghali, M. N. et al. Pregnancy outcomes in women with an early diagnosis of gestational diabetes mellitus. Diabetes Res. Clin. Pract. 138, 177–186 (2018).
Feig, D. S. et al. Trends in Incidence of diabetes in pregnancy and serious perinatal outcomes: A large population-based study in Ontario, Canada, 1996–2010. Diabetes Care 37, 1590–1596 (2014).
Bartsch, E., Medcalf, K. E., Park, A. L. & Ray, J. G. High Risk of Pre-eclampsia Identification, Group. Clinical risk factors for pre-eclampsia determined in early pregnancy: Systematic review and meta-analysis of large cohort studies. BMJ 353, i1753 (2016).
Hwu, L. J. et al. Risk of subsequent hypertension and diabetes in women with hypertension during pregnancy and gestational diabetes. Mayo Clin. Proc. 91, 1158–1165 (2016).
Bryson, C. L., Loannou, G. N., Rulyak, S. J. & Critchlow, C. Association between gestational diabetes and pregnancy-induced hypertension. Am. J. Epidemiol. 158, 1148–1153 (2003).
Dos Santos Da Silva, L. L. G. et al. Hypertensive disorders of pregnancy in women with gestational diabetes mellitus from Rio de Janeiro, Brazil. Pregnancy Hypertens. 10, 196–201 (2017).
Black, M. H. et al. Prehypertension prior to or during early pregnancy is associated with increased risk for hypertensive disorders in pregnancy and gestational diabetes. J. Hypertens. 33, 1860–1867 (2015).
Butwick, A. J., Druzin, M. L., Shaw, G. M. & Guo, N. Evaluation of US state-level variation in hypertensive disorders of pregnancy. JAMA Netw Open. 3(10), e2018741 (2020).
Cripe, S. M., Frederick, I. O., Qiu, C. F. & Williams, M. A. Risk of preterm delivery and hypertensive disorders of pregnancy in relation to maternal co-morbid mood and migraine disorders during pregnancy. Paediatr. Perinatal Epidemiol. 25, 116–123 (2011).
Wang, A. et al. Circulating anti-angiogenic factors during hypertensive pregnancy and increased risk of respiratory distress syndrome in preterm neonates. J. Matern. Fetal Neonatal Med. 25(8), 1447–1452 (2012).
Rubarth, L. B. & Quinn, J. Respiratory development and respiratory distress syndrome. Neonatal Netw. 34(4), 231–238 (2015).
Yoon, J. J., Kohl, S. & Harper, R. G. The relationship between maternal hypertensive disease of pregnancy and the incidence of idiopathic respiratory distress syndrome. Pediatrics 65, 735–739 (1980).
Shah, D. M., Shenai, J. P. & Vaughn, W. K. Neonatal outcome of premature infants of mothers with preeclampsia. J. Perinatol. 15, 264–267 (1995).
Langenveld, J. et al. Neonatal outcome of pregnancies complicated by hypertensive disorders between 34 and 37 weeks of gestation: A 7 year retrospective analysis of a national registry. Am. J. Obstet. Gynecol. 205(540), e541–e547. https://doi.org/10.1016/j.ajog.2011.07.003 (2011).
Friedman, S. A., Schif, E., Kao, L. & Sibai, B. M. Neonatal outcome after preterm delivery for preeclampsia. Am. J. Obstet. Gynecol. 172, 1785–1788 (1995) (discussion 1788–1792).
Jelin, A. C. et al. Early-onset preeclampsia and neonatal outcomes. J. Maternal Fetal neonatal Med. 23, 389–392. https://doi.org/10.3109/14767050903168416 (2010).
Berger, H. et al. Impact of diabetes, obesity and hypertension on preterm birth: Population-based study. PLoS ONE 15, e0228743 (2020).
Balsells, M., García-Patterson, A., Gich, I. & Corcoy, R. Major congenital malformations in women with gestational diabetes mellitus: A systematic review and meta-analysis. Diabetes Metab. Res. Rev. 28, 252–257 (2012).
Liu, X. et al. Prevalence of congenital heart disease and its related risk indicators among 90,796 Chinese infants aged less than 6 months in Tianji. Int. J. Epidemiol. 44, 884–893. https://doi.org/10.1093/ije/dyv107 (2015).
Leirgul, E. et al. Maternal diabetes, birth weight, and neonatal risk of congenital heart defects in Norway, 1994–2009. Obstet. Gynecol. 128, 1116–1125 (2016).
Garg, S. et al. Use of fetal echocardiography for characterization of fetal cardiac structure in women with normal pregnancies and gestational diabetes mellitus. J. Ultrasound Med. 33, 1365–1369 (2014).
Gao, Y. & Huang, G. Y. Advance in the etiology and the epidemiology of congenital heart disease. Chin. J. Evid. Based Pediatr. 3, 213–222 (2008).
Boyd, H. A. et al. Association between fetal congenital heart defects and maternal risk of hypertensive disorders of pregnancy in the same pregnancy and across pregnancies. Circulation 136, 39–48. https://doi.org/10.1161/CIRCULATIONAHA.116.024600 (2017).
Sliwa, K. & Mebazaa, A. Possible joint pathways of early pre-eclampsia and congenital heart defects via angiogenic imbalance and potential evidence for cardio-placental syndrome. Eur. Heart J. 35, 680–682. https://doi.org/10.1093/eurheartj/eht4 (2014).
Waters, T. P. et al. Maternal and neonatal morbidity for women who would be added to the diagnosis of GDM using IADPSG criteria: A secondary analysis of the hyperglycemia and adverse pregnancy outcome study. Diabet. Care. 39, 2204–2210 (2016).
Funding
This study is supported in part by Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW109-TDU-B-212-114004), MOST Clinical Trial Consortium for Stroke (MOST Clinical Trial Consortium for Stroke (MOST 109-2321-B-039-002), China Medical University Hospital (DMR-106-140), and Tseng-Lien Lin Foundation, Taichung, Taiwan.
Author information
Authors and Affiliations
Contributions
The study was conceptualized by Y.W.L., M.H.L., L.W.P. and J.W.F. C.H.M. and F.C.S. analyzed and curated the data. Y.L.T., F.C.S., Y.W.L., L.W.P. and J.W.F. were involved in validation. F.C.S. and Y.L.T. were involved with the resources and supervision. Y.W.L., M.H.L. and J.W.F. wrote the original draft. All authors were involved in the investigation and methodology of the study. All authors reviewed and edited the manuscript. F.C.S. and Y.L.T. finalized the revision.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lin, YW., Lin, MH., Pai, LW. et al. Population-based study on birth outcomes among women with hypertensive disorders of pregnancy and gestational diabetes mellitus. Sci Rep 11, 17391 (2021). https://doi.org/10.1038/s41598-021-96345-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-96345-0
- Springer Nature Limited
This article is cited by
-
Development and internal validation of a clinical score to predict neonatal hypoglycaemia in women with gestational diabetes
Endocrine (2024)
-
Interactions between long interpregnancy interval and advanced maternal age on neonatal outcomes
World Journal of Pediatrics (2023)
-
Characteristics and fetal outcomes of pregnant women with hypertensive disorders in China: a 9-year national hospital-based cohort study
BMC Pregnancy and Childbirth (2022)
-
Development and evaluation of a nomogram for adverse outcomes of preeclampsia in Chinese pregnant women
BMC Pregnancy and Childbirth (2022)