Abstract
Medical costs have recently increased in South Korea due to the rising rate of asthma. Primary clinics serve an important role in asthma management, as they are the first stop for patients presenting with symptoms. The Health Insurance Review and Assessment Service (HIRA) in South Korea has assessed asthma-management quality since 2013, but studies are lacking on whether these assessments have been performed properly and contribute toward reducing asthma exacerbations. Therefore, we investigated whether the HIRA’s quality assessments have decreased asthma exacerbations using national health insurance claims data from 2013 to 2017 of 83,375 primary-clinic and 15,931 tertiary-hospital patients with asthma. These patients were classified into four groups based on disease severity according to the monthly prescribed amount of asthma medication using K-means clustering. The associations between HIRA assessments and asthma exacerbation were analyzed using a generalized estimating equation. Our results showed that exacerbation odds gradually decreased as the HIRA assessments progressed, especially in the mild-severity group, and that exacerbation risk among patients with asthma decreased in the order of assessment grades: “Unsatisfactory,” “Satisfactory,” and “Tertiary.” Therefore, we may conclude that asthma exacerbations may decrease with high quality asthma management; appropriate quality assessment could be helpful in reducing asthma exacerbations.
Similar content being viewed by others
Introduction
The global prevalence of asthma has increased by more than 12% since the 1990s, with a much higher prevalence in developed countries and a marked rise in developing countries1,2,3. Especially in regions with a high sociodemographic index quintile, the percentage change in disability-adjusted life years increased by 12.7% during the same period1,4,5. Due to economic development in South Korea, the prevalence of asthma has steadily increased by approximately 2.3 times from 1998 to 2013, even after adjusting for age and sex6. The socioeconomic burden of asthma, including direct and indirect annual costs, has also increased by approximately USD 15,000 per patient7,8,9. The cost incurred by hospitalization owing to asthma exacerbation can be avoided with high-quality primary care10. Therefore, appropriate asthma care practices by primary care providers is important to reduce cases of asthma exacerbation11,12,13. Quality assessments of asthma management have been performed in South Korea since 2013 to improve the quality of asthma management provided by medical institutions. In South Korea, the Health Insurance Review and Assessment Service (HIRA) manages health insurance and medical claims data for 96.6% of the population and facilitates nationwide quality assessments14.
The assessment outcome for an institution, as classified by the HIRA, is assigned a “satisfactory” or “unsatisfactory” grade. A total of 11.89% (1066 out of 8967 primary clinics), 14.41% (1278 out of 8866), and 16.19% (1.419 out of 8762) primary clinics were assigned satisfactory grades in the 1st (July 2013–June 2014), 2nd (July 2014–June 2015), and 3rd (July 2015–June 2016) assessment periods, respectively15. The outcomes were officially announced each year only for primary clinics, as asthma is an ambulatory care sensitive condition10. Primary clinics referred to community hospital with few specialties or just general practice, while tertiary hospitals have highly specialized staff and technical equipment with 300–1500 beds16. Asthma management in tertiary hospitals was assumed to be the best among medical institutions, as they had sufficient personnel, facilities, and equipment as prescribed by the ordinance of the Ministry of Health and Welfare. To date, studies on the HIRA assessments have only examined simple descriptive statistics, for example, comparisons of the types of prescribed medications for each stage dependent on the medical institution or comparisons of the pulmonary function test (PFT) ratios17,18. In this study, intervention implementation in quality assessment could be tested while collecting evidence of clinical effectiveness that improved asthma management; such a study would be considered a type 3 hybrid design, i.e. a national-scale implementation study without effectiveness studies performed in advance19. The satisfactory clinics are assumed to have better prognostics than the unsatisfactory group. As the severe patients might be allocated in satisfactory clinics, there could be more asthma exacerbations in satisfactory clinics. So the quality assessment considered the performance rate of each asthma care indicator rather than exacerbation rate in the classification of satisfactory clinics and it was evaluated whether satisfactory asthma management decreases asthma exacerbation regardless of severity. Therefore, as part of the Joint Project on Quality Assessment Research by HIRA, we aimed to investigate whether asthma management quality assessments by the HIRA effectively classify the institutions and ultimately help encourage proper management to decrease asthma exacerbations.
Methods
Study subjects
In this retrospective cohort study, we used the HIRA database to identify whether asthma assessment significantly affected asthma exacerbation. Patients 15 years of age or older diagnosed with asthma (J45 and J46) as a primary or secondary code at least once between July 1, 2013 and June 30, 2017 in the HIRA claims data were eligible for enrolment. Data collection lasted from the first to fourth assessment periods, including data of 4,209,588 patients from the first period (July 2013–June 2014), 4,204,360 from the second (July 2014–June 2015), 4,151,057 from the third (July 2015–June 2016), and 5,288,586 from the fourth (July 2016–June 2017). Therefore, patient data could be repeated in each period. Assessment was performed from the first to the third premeasurement periods, and we evaluated the association between the assessment results and asthma exacerbations 1 year later during the measurement period.
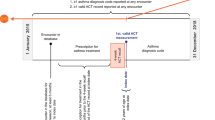
In total, 83,375 patients with asthma (32,472, 32,203, and 29,579 patients from the first, second, and third periods, respectively) were selected according to our inclusion and exclusion criteria: (1) more than two outpatient clinic visits while using asthma medication or at least one hospitalization while using oral/intravenous corticosteroids and an outpatient clinic visit while using asthma medication (the list of asthma medications was obtained according to the 2017 Global Initiative for Asthma [GINA] guidelines (Supplementary Table S1)20), (2) diagnosed at a primary clinic, (3) had not lost health insurance qualification, and (4) had visited only one primary clinic in any given period. The fourth criterion was adopted because treatment from multiple clinics might overlap, making it difficult to determine the association between HIRA grade and asthma exacerbation. Similarly, 15,931 patients with asthma (6019, 6418, and 7257 patients from the first, second, and third periods, respectively) diagnosed at only one tertiary hospital for each period were selected who also met the first and third criteria (Fig. 1a). There may have been patient overlap; for example, a patient may have visited a primary clinic one year and a tertiary hospital in another year.
(a) Selection process of the study cohort. The study population was categorized as 83,375 primary clinic patients and 15,931 tertiary hospital patients, after all of the following exclusion criteria. (b) Retrospective study design. Assessment outcome and other explanatory variables were collected during the premeasurement period (A), and the exacerbation as outcome of assessment was collected the following measurement period (B) for three assessment periods, repeatedly.
Study design
Assessment grades and asthma severity information from the first to fourth periods were collected during the premeasurement period (A), and asthma exacerbation outcomes were measured during the measurement period (B) of the next year. This was repeated for each period (Fig. 1b); we evaluated whether a hospital with a satisfactory grade in the premeasurement period (A) had less asthma exacerbation cases in the next year’s measurement period (B).
Outcome and covariate variables
Asthma exacerbation
Asthma exacerbation during the measurement period was the primary outcome variable, defined as systemic corticosteroid bursts for asthma treatment based on previous studies21 (i.e. more than 80 mg of hydrocortisone or any other corticosteroid of any potency or short-acting beta2 agonists [SABA] nebulizer treatment under J45 and J46 as shown in Supplementary Table S1, obtained from the GINA guidelines). Emergency department visits or hospitalizations for asthma that did not occur in primary clinics were excluded from the definition of asthma exacerbation because HIRA assessment results were only published for primary clinics.
Asthma assessment grades
Institutions were classified into three groups: unsatisfactory primary clinics, satisfactory primary clinics, and tertiary hospitals; the quality of asthma management ascended in this order. The assessment outcomes of primary clinics were assigned “satisfactory” or “unsatisfactory” grades and defined according to the following steps. From July to June of every year, patients older than 15 years with asthma (J45 and J46 according to 10th International Statistical Classification of Diseases and Related Health Problems [ICD-10]) were surveyed. The quality assessment was based on seven items: (1) percentage of patients who received the pulmonary function test (PFT) at least once during the assessment period, (2) percentage of ongoing visits (at least three), (3) percentage of patients prescribed inhaled corticosteroids (ICSs), (4) percentage of patients requiring prescribed medicines such as leukotriene receptor antagonists (LTRAs) or ICSs, (5) percentage of patients prescribed long-acting beta2 agonists (LABAs) not using ICSs, (6) percentage of patients prescribed SABAs not using ICSs, (7) percentage of patients prescribed oral corticosteroids snot using ICSs. For the first four items, which were mandatory, a higher score was satisfactory; for the remaining items, a higher score was unsatisfactory. Institutions were assigned a satisfactory grade when they scored higher than the median on each of the mandatory items. However, institutions with scores at the lowest 10% on the remaining three items were excluded. The list of institutions with satisfactory grades is disclosed only in the case of primary clinics, as asthma is a chronic disease for which it is important to prevent acute deterioration and hospitalization through continuous management at a nearby primary medical institution. Although the assessment results of tertiary hospitals were not disclosed, tertiary hospitals are assumed to provide better medical care than primary clinic.
Asthma severity
The asthma severity is known as an important confounder of asthma exacerbation and its adjustment is crucial to obtain the unbiased estimates of asthma management effect22,23,24. However, it is difficult to classify asthma severity by diagnosis code, so patients were classified in consideration of their 12-month medication and prescription by using K-means clustering. Each resulting cluster was used as an indicator of asthma severity: From the mildest severity I to the most intense severity IV. First, a rank was assigned according to each principal component code of the GINA guidelines for the drug prescribed throughout the indicated medication period starting on the date of prescription (Supplementary Table S1): Rank 1, low-dose ICS, LTRA, xanthine, or LABA; Rank 2, high-dose ICS, low-dose ICS/LABA; Rank 3, high-dose ICS/LABA; and Rank 4, long-acting muscarinic antagonist inhaler and low-dose oral prednisolone for long-term use20. Then, the daily rank-sum was calculated by adding the ranks of all drugs assigned to each day, and the average monthly ranks were determined. Finally, we observed the time-varying pattern of the average monthly rank for each 12-month period. We conducted k-means clustering to distinguish the varying pattern of medication and the degree of severity was classified into four severity clusters for each pattern25. The clustering analysis here is described in detail in the Statistical Analyses section. The medications prescribed for asthma exacerbations were not considered in the above severity calculations.
Total medication rank
By summing the 365 daily medication ranks, we calculated the yearly total medication rank and consider it as a covariate to control the potential residual effects within the cluster, even after considering the clustered annual asthma severity.
Medication possession ratio (MPR)
The MPR reflects the adherence to medication, which tends to reduce the risk of asthma exacerbations23,26,27,28,29. In administrative claims data, it can be calculated as follows30,31,32,33,34,35,36,37,38.
The follow-up period denotes the period from the first to the last prescription of asthma medication within the premeasurement period. Observations with an MPR < 20% were categorized as 1 (low adherence 20%–80% as 2, and > 80% as 3 (high adherence. Level 0 indicated the patient had not been prescribed any asthma medication except for alleviating exacerbations during the period.
Comorbidity
Comorbidities were adjusted for in the premeasurement period (A) (Fig. 1b) because they may affect asthma exacerbation39. Comorbidity variables were defined by whether at least one of the following ICD-10 codes had ever been diagnosed: atopic dermatitis (L20), gastroesophageal reflux disease (K21), chronic rhinitis (J31), allergic rhinitis (J30), chronic sinusitis (J32), depression (F32, F33), anxiety (F40, F41), or obesity (E66)26.
Statistical analyses
Asthma severity was calculated with the average monthly rank based on prescribed drugs for each 12-month period, and the corresponding annual value of severity was obtained. K-means clustering was performed by reflecting these monthly mean values to each dimension. The k-means algorithm was executed using the Euclidean distance, and k was determined to be 4 (the model had the largest overall R-square when k = 4). Chi-square tests were used to examine significant relationships between exacerbations and covariates and P values less than 0.05 were considered statistically significant.
Model for asthma exacerbation
Associations between risk factors and asthma exacerbations were analyzed with the generalized estimating equation (GEE). PROC GENMOD (SAS version 6.1) and Rex (Version 3.1.3.1) were used to conduct the analysis and generate figures40. The logit link function was used because the outcome was binary. There were patients prescribed asthma medications in multiple assessment periods; hence, they may have been repeatedly observed and measured. In such cases, repeated patient measures had a first-order autoregressive (AR[1]) correlation structure according to the period of assessment. We used the AR[1] correlation structure between consecutive measurements on each patient where correlation between two different time points is inversely related with their intervals41 and we also found that the results for different correlation structure were similar. Meanwhile, all study subjects had at most one observation per period. With Yij as 1 if there was exacerbation in the i-th observation of patient j and otherwise 0; we can define \(p_{ij} = P\left( {Y_{ij} = 1|X} \right) = E\left( {Y_{ij} } \right)\) with designed matrix X. The model for all patients is as follows.
However, the severity group I occupied a very large portion of clusters and they usually visit unsatisfactory clinics more but have less exacerbation than other groups. This can lead to biased estimates of asthma management effects. Hence, we also performed subgroup analyses according to severity for unbiased evaluation of asthma assessment. The final model was selected by comparing the goodness of fit (QICu):
Ethics statement
The institutional review board of Seoul National University approved this study (IRB No. E1805/003-010). As the data was anonymized, the requirement for written informed consent was waived. All methods were performed in accordance with the relevant guidelines and regulation.
Results
Characteristics of all patients
The distribution of each explanatory variable for exacerbations in the following year is shown in Table 1. The number of patients presented in Fig. 1a and the total number of patients presented in Table 1 are inconsistent, as the same patients were repeatedly counted over the periods. There was no significant difference in asthma exacerbation according to assessment period. Male patients had more asthma exacerbations, and age appeared to be positively associated with asthma exacerbations. The proportion of patients with level 0 MPR among those with asthma exacerbations (5.9%) was almost three times that of those without asthma exacerbations (2.1%). Patients with exacerbations had a slightly but significantly lower rate of comorbidities (65.0%) compared to those without exacerbations (67.6%).
Clustering severity of asthma
As a result of the clustering analysis, the patients with asthma were classified into four groups according to their overall severity. Severity group I (n = 83,175) showed the lowest severity, with a stable pattern, and included most patients (Fig. 2). The 83,175 patients in severity group I comprised 35.1% of the patients from the first assessment period, 34.1% from the second, and 30.8% from the third. Severity group II (n = 11,116) showed a rapidly increasing pattern in winter, peaking in January and gradually decreasing as the weather improved. However, it still showed the second lowest overall severity among the four groups. Severity group III (n = 16,692) showed moderate and stable severity throughout the year. Severity group IV comprised only 2965 patients, but they had high severity throughout the year. They also showed a severity peak in January and relatively low severity during the summer season. Notably, the number of patients included in severity group IV increased over the periods, as opposed to the distribution in severity group I (Table 2). The distribution of exacerbations in the following year according to severity clustering showed that the exacerbation rate gradually increased as severity increased (Table 3, Supplementary Fig. S1).
In addition, the distribution of assessment grades according to asthma severity, presented in Fig. 3, showed that severity group I accounted for the largest portion of patients. As a result, the overall analysis result can be determined according to the result of severity group I. Also, the higher the severity, the higher the rate of visits to a hospital with better grade. This selection bias can lead to more exacerbations in better hospitals. Therefore, subgroup analyses were conducted to correct for this bias.
GEE model selection and effect of assessment
The results of the GEE analyses of risk factors associated with asthma exacerbation are shown in Tables 4 and 5, wherein estimated values of the odds ratios (ORs) and P values are described. The statistics for the periods and grades were presented according to severity subgroup in the subgroup analyses. Total QICu can be calculated by summing the QICus at each severity level. In the whole-group model, a higher OR was observed in the satisfactory-grade clinics than in those with unsatisfactory grades (Table 4). The OR of the grade was different from before considering severity as a covariate (results are not attached). The estimates of covariates other than asthma management can be biased unless their confounders were considered properly. However, the direct effect of assessment period showed the OR decreased over time significantly, with P values lower than 0.0001 over time. The OR of exacerbation significantly increased with the severity of asthma, except for the highest severity. Further, men showed a higher degree of asthma exacerbation than women, but the difference was not significant (P = 0.09). Patients younger than 45 years had a significantly lower degree of exacerbation than patients older than 65 years (P < 0.0001). Regarding MPR, exacerbations were more frequent in the group with adherence of 80% or lower than in the group with adherence of > 80% (all P < 0.0001). In particular, the group with 0 MPR, with conditions entirely unmanaged by asthma medication, had a large OR of exacerbation as a result of the lack of proper management. Patients without comorbidities were found to have a lower OR of exacerbation than those with comorbidities (P = 0.04) (Supplementary Table S2).
In the final model, controlling for the bias due to large cluster I, the QICu value (109,430) signified a better model with a lower value than that of the whole-group model (Table 5). The cluster-wise analysis of the entire dataset showed statistically significant outcomes of the grade variable with ORs larger than 1 in severity clusters I, II, and III. The OR of clinics with unsatisfactory grades was larger than that of clinics with satisfactory grades in the case of clusters II and III, suggesting that poor asthma management was positively associated with asthma exacerbations. In cluster IV, the ORs were larger than 1 but statistically insignificant. In addition, the OR of exacerbation in terms of period significantly decreased over time in cluster I, which also suggests exacerbation was reduced in the mildest severity group, as the assessment was repeated every year.
Discussion
Our large cohort study showed that institution assessment grade, severity, sex, age, MPR, comorbidities, and assessment itself may be important factors related to asthma exacerbations. Moreover, the magnitude of the effect of grade on asthma exacerbation varied in the subgroup analysis according to severity. We compared primary outcomes of asthma patients between satisfactory primary clinics and tertiary hospitals to accurately determine the effect of severity on the exacerbation, with the trend of severe patients being concentrated in satisfactory clinics more than in unsatisfactory clinics.
All patients could be clustered into four severity groups. In severity groups I-IV, 6185 (7.4%), 5357 (48.2%), 5963 (35.7%), and 2189 (73.8%) patients visited tertiary institutions, respectively (Table 3, Table S4). As shown in Fig. 2, severity groups II and IV showed a common peak in January, with severity group IV decreasing in February and peaking again in March. Therefore, seasonality was observed in our data, suggesting that seasonality or air pollution, risk factors for asthma exacerbation, may affect the severity of asthma42,43. Based on the results of a long-term monthly time-series analysis from 2000 to 2014, fine dust concentration (PM10) is highest in March in South Korea44. Therefore, the second peak in March for the highest asthma severity group could be explained by the effect of air pollution. Meanwhile, we included years as a covariate to adjust the national trends and the number of patients with asthma exacerbation tends to slightly decrease.
The asthma exacerbation rate decreased as the HIRA assessment progressed in this study, although this was only observed in severity group I in the final subgroup model. As each primary clinics’ grade is disclosed in public, asthma patients can select and visit the satisfactory clinic nearby and this may have made hospitals strive to provide higher health care and receive satisfactory grades. Actually, the percentage of clinics that were all in the top 50% of the previous 4 items and not in the bottom 10% of the last 3 items and met the satisfactory grade increased from 11.89% to 16.79% as assessment period passed15. However, financial rewards and penalties based on assessment results as applied to the results of the quality assessment of other diseases (high blood pressure, diabetes, hemodialysis) are not yet utilized for patients with asthma. The HIRA assessment itself might be more helpful in improving the quality of asthma management to prevent asthma exacerbation and alleviate asthma severity if administrators applied a similar incentive system for patients with asthma.
According to HIRA reports, each of the seven indicators had its own basis for selection and improved as the assessment experience increased. Adhering to these guidelines is known to reduce the risk of asthma exacerbation, and hospitals that comply with the 7 items are expected to better prevent exacerbations26,45,46. Due to the imbalance of asthma severity between grades, the quality assessment program did the best to encourage improving performance rate, did not consider the exacerbation rate in the classification of satisfactory clinics. HIRA does not disclose the individual performance rates each medical institution had for each item, but it presents three-year statistics as the HIRA report15. It also provides rationale for selection as the evaluation criteria for each item as follows. (1) The total percentage of patients who received the PFT at least once during the assessment period was included because, when asthma is diagnosed, the most useful indicator of future risk is pulmonary function, which requires periodic tests of lung function not only at the time of diagnosis, but also 3–6 months after treatment and during follow-up. The PFT rate of the third period of assessment increased 4.87% compared to that of the first period. Tertiary hospitals showed 85.44%, while primary clinics showed 20.09%15,45. (2) The percentage of ongoing visits (at least three) was considered as an indicator of a favorable hospital; regular visits from patients allow for regular monitoring of their asthma46. (3) and (4) The percentage of patients requiring prescribed medicines such as LTRAs or ICSs was included, because inhaled steroids are the most effective prophylactic drug for maintaining asthma control and should be used if possible for all patients with asthma. The use of anti-leukotriene alone is less effective than low-dose inhaled steroids. However, in some cases, it can be used as initial maintenance treatment. The proportion of patients prescribed ICS or LTRA in the third period was 63.65%, increased 4.50% from the first period47,48. (5), (6) and (7) The percentage of patients prescribed LABAs/SABAs or oral corticosteroids not using ICSs should be low to get a satisfactory grade. This is because beta2 agonists or oral corticosteroids need be used with inhaled steroids, used in urgent situations such as acute exacerbations, or used with various restrictions and caution of abuse49,50. These last three items showed decreasing trends over the periods according to HIRA report15,18.
For severity groups II and III, the patients managed in primary clinics had more exacerbations than had those managed in tertiary hospitals; the patients managed in unsatisfactory-grade primary clinic had the most exacerbations. In contrast, severity groups I and IV required in-depth analyses. Severity group I was composed of patients with mild asthma, ranking close to 0 throughout the year. As such, they did not require medicated most of the time, but experienced exacerbation sometimes. This made it hard to classify severity among patients with mild asthma and control the residual effects of each patient’s severity in the model. Although the OR of the satisfactory group was larger than that of the unsatisfactory group, their confidence intervals overlapped. We can conclude there was no significant difference between satisfactory and unsatisfactory clinics among severity group I in terms of asthma exacerbation. For severity group IV, it was also difficult to judge whether (1) the characteristics of the patients differed, (2) the results were not significant because the sample was too small, or (3) the current classification criteria were insufficient for severity group IV. There were only 776 patients in severity group IV who visited primary clinics, and 435 of those had exacerbations (Supplementary Table S4).
Our study had several strengths. There were previously only reviews of reports published by the HIRA regarding qualitative assessments18,51,52, but we actively evaluated the effectiveness of the asthma management and the policy through quantitative analysis using raw data from health insurance claims. Also, this quantitative statistical analysis applied a clustering algorithm to analyze the asthma severity pattern in large cohort data. Asthma severity, one of the important confounding variable of asthma exacerbation, was calculated by rank according to the GINA guideline, and patients with asthma were grouped according to the rank-sum values, unlike in previous studies that only utilized clinical findings and hospital data with small numbers of patients14,24,53. The individual effect was also considered in the statistical model with a correlation structure. As such, the characteristics of each patient could be more accurately considered using the 3-year data with repetition.
However, our study also had several limitations. There is a possibility of incomplete coding accuracy and recording, as the measurement of asthma medication and diagnosis of exacerbation was based on claims data. A previous study on the validity of health claims data in Korea using ICD-10 codes showed primary and secondary codes on 9278 claims had accordance rates of only 82.0% and 56.4%, respectively54. Secondly, because this was an observational study, all of the confounding factors could not be included in the model, leading to residual confounding. Many variables affecting the results, including smoking status, medical records, and socioeconomic status, were not fully available in the HIRA database. Despite the seasonality of asthma severity due to air pollution in our data (Fig. 2), patient residence was not included in the HIRA database due to privacy issues. Thus, the air pollution factor was not included in the model. Finally, asthma exacerbation was defined on the basis of prescription medications, but emergency room visits or hospitalizations due to asthma should be included21,26,28. However, admission and emergency room visits could be excluded from the definition, as the major concern of this study was the quality assessment grades of primary clinics.
In conclusion, asthma exacerbation is affected by the quality of asthma management and its assessment, and our findings suggest that proper asthma management can reduce asthma exacerbations, regardless of asthma severity (Table 5). Thus, evidence has been provided for the clinical effectiveness of and justification for quality assessment based on national-scale policy implementation19. However, as the effectiveness of asthma management could not be analyzed properly for patients with the lowest severity, new criteria should be established in further study to clearly subdivide asthma severity11,12,13.
Data availability
The data that support the findings of this study are available from the HIRA. Restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available due to personal information protection. Data are available at https://opendata.hira.or.kr/ with the permission of the HIRA.
References
Soriano, J. B. et al. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet Respir. Med. 5, 691–706. https://doi.org/10.1016/s2213-2600(17)30293-x (2017).
World Health Organization. WHO factsheet 206: bronchial asthma (2014).
Nunes, C., Pereira, A. M. & Morais-Almeida, M. Asthma costs and social impact. Asthma Res. Pract. 3, 1. https://doi.org/10.1186/s40733-016-0029-3 (2017).
Murray, C. J. & Acharya, A. K. Understanding DALYs (disability-adjusted life years). J. Health Econ. 16, 703–730 (1997).
The Lancet. GBD 2015: From big data to meaningful change. The Lancet https://doi.org/10.1016/s0140-6736(16)31790-1 (2016).
Park, S. Y. et al. High prevalence of asthma in elderly women: Findings from a Korean National Health Database and adult asthma cohort. Allergy Asthma Immunol. Res. 10, 387–396. https://doi.org/10.4168/aair.2018.10.4.387 (2018).
Yoo, K.-H. et al. Burden of respiratory disease in Korea: An observational study on allergic rhinitis, asthma, COPD, and rhinosinusitis. Allergy Asthma Immunol. Res. 8, 527–534 (2016).
Kim, S. Y. et al. Increased prevalence of self-reported asthma among Korean adults: An analysis of KNHANES I and IV data. Lung 191, 281–288. https://doi.org/10.1007/s00408-013-9453-9 (2013).
Uphoff, E. P., Cabieses, B., Wright, J. & Pickett, K. E. International prevalence rates of asthma and allergy are associated with income inequality. J. Allergy Clin. Immunol. 136, 189e182-190e182. https://doi.org/10.1016/j.jaci.2015.01.037 (2015).
Bodenheimer, T., Wagner, E. H. & Grumbach, K. Improving Primary Care for Patients With Chronic Illness. JAMA 288, 1775–1779. https://doi.org/10.1001/jama.288.14.1775 (2002).
Eccles, M. et al. Effect of computerised evidence based guidelines on management of asthma and angina in adults in primary care: Cluster randomised controlled trial. BMJ 325, 941. https://doi.org/10.1136/bmj.325.7370.941 (2002).
Picken, H. A., Greenfield, S., Teres, D., Hirway, P. S. & Landis, J. N. Effect of local standards on the implementation of national guidelines for asthma: Primary care agreement with national asthma guidelines. J. Gen. Intern. Med. 13, 659–663. https://doi.org/10.1046/j.1525-1497.1998.00200.x (1998).
Cloutier, M. M., Hall, C. B., Wakefield, D. B. & Bailit, H. Use of asthma guidelines by primary care providers to reduce hospitalizations and emergency department visits in poor, minority, urban children. J. Pediatr. 146, 591–597. https://doi.org/10.1016/j.jpeds.2004.12.017 (2005).
Kim, S. H. et al. The effect of asthma clinical guideline for adults on inhaled corticosteroids PrescriptionTrend: A quasi-experimental study. J. Korean Med. Sci. 30, 1048–1054. https://doi.org/10.3346/jkms.2015.30.8.1048 (2015).
Kim, S. R., Lee, Y. C., Sung, M. J. & Bae, H. W. Current epidemiological data on asthma management in South Korea from qualitative assessment of asthma management by Health Insurance Review and Assessment Service (HIRA). Tuberc. Respir. Dis. 80, 221–225. https://doi.org/10.4046/trd.2017.80.3.221 (2017).
Hensher, M., Price, M. & Adomakoh, S. Disease Control Priorities in Developing Countries. Referral Hospitals.
Cho, E. Y. et al. Comparison of clinical characteristics and management of asthma by types of health care in South Korea. J. Thorac. Dis. 10, 3269–3276. https://doi.org/10.21037/jtd.2018.05.95 (2018).
Choi, J. Y. et al. Current status of asthma care in South Korea: Nationwide the Health Insurance Review and Assessment Service database. J. Thorac. Dis. 9, 3208–3214. https://doi.org/10.21037/jtd.2017.08.109 (2017).
Bernet, A. C., Willens, D. E. & Bauer, M. S. Effectiveness-implementation hybrid designs: Implications for quality improvement science. Implement. Sci. 8, S2. https://doi.org/10.1186/1748-5908-8-S1-S2 (2013).
Global Initiative for Asthma. Global strategy for asthma management and prevention. https://ginasthma.org/2018-gina-report-global-strategy-for-asthma-management-and-prevention/.
Fuhlbrigge, A. et al. Asthma outcomes: Exacerbations. J. Allergy Clin. Immunol. 129, S34-48. https://doi.org/10.1016/j.jaci.2011.12.983 (2012).
Aldington, S. & Beasley, R. Asthma exacerbations. 5: Assessment and management of severe asthma in adults in hospital. Thorax 62, 447–458. https://doi.org/10.1136/thx.2005.045203 (2007).
Zeiger, R. S. et al. Utilization and costs of severe uncontrolled asthma in a managed-care setting. J. Allergy Clin. Immunol. Pract. 4, 120-129.e123. https://doi.org/10.1016/j.jaip.2015.08.003 (2016).
Kim, J.-H. Diagnosis of severe asthma: Definition and identification. Korean J. Med. 93, 153–158. https://doi.org/10.3904/kjm.2018.93.2.153 (2018).
Koo, S. M. et al. Effect of pregnancy on quantitative medication use and relation to exacerbations in asthma. Biomed. Res. Int. 2017, 8276190. https://doi.org/10.1155/2017/8276190 (2017).
Kang, H. R. et al. Risk factors of asthma exacerbation based on asthma severity: A nationwide population-based observational study in South Korea. BMJ Open 8, e020825. https://doi.org/10.1136/bmjopen-2017-020825 (2018).
Ivanova, J. I. et al. Impact of medication adherence to disease-modifying drugs on severe relapse, and direct and indirect costs among employees with multiple sclerosis in the US. J. Med. Econ. 15, 601–609. https://doi.org/10.3111/13696998.2012.667027 (2012).
Engelkes, M., Janssens, H. M., de Jongste, J. C., Sturkenboom, M. C. & Verhamme, K. M. Medication adherence and the risk of severe asthma exacerbations: A systematic review. Eur. Respir. J. 45, 396–407. https://doi.org/10.1183/09031936.00075614 (2015).
Lee, T. et al. Risk factors for asthma-related healthcare use: Longitudinal analysis using the NHI claims database in a Korean asthma cohort. PLoS ONE 9, e112844. https://doi.org/10.1371/journal.pone.0112844 (2014).
Steiner, J. F., Koepsell, T. D., Fihn, S. D. & Inui, T. S. A general method of compliance assessment using centralized pharmacy records. Description and validation. Med. Care 26, 814–823 (1988).
Steiner, J. F. & Prochazka, A. V. The assessment of refill compliance using pharmacy records: Methods, validity, and applications. J. Clin. Epidemiol. 50, 105–116 (1997).
Sclar, D. A. et al. Effect of health education in promoting prescription refill compliance among patients with hypertension. Clin. Ther. 13, 489–495 (1991).
Sikka, R., Xia, F. & Aubert, R. E. Estimating medication persistency using administrative claims data. Am. J. Manag. Care 11, 449–457 (2005).
Karve, S. et al. Prospective validation of eight different adherence measures for use with administrative claims data among patients with schizophrenia. Value Health 12, 989–995. https://doi.org/10.1111/j.1524-4733.2009.00543.x (2009).
Karve, S. et al. An empirical basis for standardizing adherence measures derived from administrative claims data among diabetic patients. Med. Care 46, 1125–1133. https://doi.org/10.1097/MLR.0b013e31817924d2 (2008).
Engelkes, M. Asthma: Epidemiology, treatment and exacerbations in real life (2016).
Mattke, S. et al. Effect of disease management on prescription drug treatment: What is the right quality measure?. Disease Manag. 10, 91–100. https://doi.org/10.1089/dis.2006.635 (2007).
Hess, L. M., Raebel, M. A., Conner, D. A. & Malone, D. C. Measurement of adherence in pharmacy administrative databases: A proposal for standard definitions and preferred measures. Ann. Pharmacother. 40, 1280–1288. https://doi.org/10.1345/aph.1H018 (2006).
Boulet, L. P. Influence of comorbid conditions on asthma. Eur. Respir. J. 33, 897–906. https://doi.org/10.1183/09031936.00121308 (2009).
RexSoft, Rex: Excel-based statistical analysis software. http://rexsoft.org/ (2018).
Ratcliffe, S. J. & Shults, J. Analysis of multi-level correlated data in the framework of generalized estimating equations via xtmultcorr procedures in Stata and qls functions in Matlab. Stat. Interface 2, 187–196. https://doi.org/10.4310/SII.2009.v2.n2.a8 (2009).
Forno, E. & Celedon, J. C. Predicting asthma exacerbations in children. Curr. Opin. Pulm. Med. 18, 63–69. https://doi.org/10.1097/MCP.0b013e32834db288 (2012).
Kim, H., Kim, H., Park, Y.-H. & Lee, J.-T. Assessment of temporal variation for the risk of particulate matters on asthma hospitalization. Environ. Res. 156, 542–550. https://doi.org/10.1016/j.envres.2017.04.012 (2017).
Yang, G.-H. et al. Analysis of the recent trend of national background PM10Concentrations over Korea, China, and Japan. J. Korean Soc. Atmos. Environ. 32, 360–371. https://doi.org/10.5572/kosae.2016.32.4.360 (2016).
Chan-Yeung, M., Chang, J. H., Manfreda, J., Ferguson, A. & Becker, A. Changes in peak flow, symptom score, and the use of medications during acute exacerbations of asthma. Am. J. Respir. Crit. Care Med. 154, 889–893. https://doi.org/10.1164/ajrccm.154.4.8887581 (1996).
Park, H. J. et al. Regular follow-up visits reduce the risk for asthma exacerbation requiring admission in Korean adults with asthma. Allergy Asthma Clin. Immunol. 14, 29. https://doi.org/10.1186/s13223-018-0250-0 (2018).
Price, D. et al. Leukotriene antagonists as first-line or add-on asthma-controller therapy. N. Engl. J. Med. 364, 1695–1707. https://doi.org/10.1056/NEJMoa1010846 (2011).
O’Byrne, P. et al. Asthma progression and mortality: The role of inhaled corticosteroids. Eur. Respir. J. 54, 1900491. https://doi.org/10.1183/13993003.00491-2019 (2019).
Nwaru, B. I. et al. Overuse of short-acting β2-agonists in asthma is associated with increased risk of exacerbation and mortality: A nationwide cohort study of the global SABINA programme. Eur. Respir. J. 55, 1901872. https://doi.org/10.1183/13993003.01872-2019 (2020).
Guo, J. J., Tsai, K., Kelton, C. M., Bian, B. & Wigle, P. R. Risk of serious asthma exacerbations associated with long-acting beta agonists among patients with asthma: A retrospective cohort study. Ann. Allergy Asthma Immunol. 106, 214–222. https://doi.org/10.1016/j.anai.2010.12.008 (2011).
Chung, S. M. & Lee, S. Y. Evaluation of appropriate management of chronic obstructive pulmonary disease in Korea: Based on Health Insurance Review and Assessment Service (HIRA) claims. Tuberc. Respir. Dis. 80, 241–246. https://doi.org/10.4046/trd.2017.80.3.241 (2017).
Yeo, C. D. et al. Indicators and Qualitative Assessment of Lung Cancer Management by Health Insurance Review and Assessment Service (HIRA) of Korea in 2015. Tuberc. Respir. Dis. 81, 19–28. https://doi.org/10.4046/trd.2017.0112 (2018).
Forno, E. et al. Risk factors and predictive clinical scores for asthma exacerbations in childhood. Chest 138, 1156–1165. https://doi.org/10.1378/chest.09-2426 (2010).
EC, P. & SI, J. Evaluation of accordance between health insurance claims disease code and EMR data (Korean) (2017).
Acknowledgements
We would like to thank Editage (www.editage.co.kr) for English language editing. This study was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF), funded by the Ministry of Education (NRF-2019R1F1A1061096).
Author information
Authors and Affiliations
Contributions
Conceptualization, N.E.K., H.J.Y., and S.W.; data curation, N.E.K.; formal analysis, N.E.K.; Resources, B.Y.K., A.G.H., and J.H.S.; supervision, H.J.Y. and S.W.; writing – original draft, N.E.K.; writing – review & editing, N.E.K., S.L., H.J.Y., and S.W.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kim, NE., Lee, S., Kim, B.Y. et al. The nationwide retrospective cohort study by Health Insurance Review and Assessment Service proves that asthma management decreases the exacerbation risk of asthma. Sci Rep 11, 1442 (2021). https://doi.org/10.1038/s41598-021-81022-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-81022-z
- Springer Nature Limited