Abstract
To compare the visual performance of a monofocal intraocular lens (IOL) (ZCB00) and a multifocal IOL (ZMB00) of the same material and basic design, we evaluated postoperative parameters at 10 weeks after the last surgery in cataract patients who underwent bilateral ZCB00 or ZMB00 implantation from December 13, 2010, to July 29, 2019, with the right and left lenses implanted within 3 months of each other. The study enrolled 2,230 eyes of 1,115 patients. The monofocal group comprised 904 eyes of 452 patients (72.3 ± 6.8 years; females/males, 268/184), and the multifocal group comprised 1,326 eyes of 663 patients (67.0 ± 7.8 years; females/males, 518/145). Contrast sensitivity (4.0/2.5/1.6/1.0/0.7 degrees), contrast sensitivity with glare (1.6/1.0/0.7 degrees), and the VFQ-25 score for driving at night were significantly better in the monofocal group (p < 0.00068, Wald test). Uncorrected intermediate/near visual acuity and near spectacle independence were significantly better in the multifocal group (p < 0.00068, Wald test). The two IOL groups had different characteristics in terms of contrast sensitivity, night-time driving, uncorrected intermediate/near visual acuity and near spectacle independence.
Similar content being viewed by others
Introduction
There is a long-standing debate about whether monofocal or multifocal lenses should be implanted during cataract surgery.
Multifocal lenses have been shown to provide good distance and near functional vision without the use of corrective lenses1,2,3,4,5,6,7,8 and have been improved in many ways. However, many studies have reported that multifocal lenses compromise contrast sensitivity and night-time driving with unwanted subjective phenomena, such as halos, glare and starbursts9,10,11,12,13, which could affect the patient’s visual performance and satisfaction. Those reports have inhibited many Japanese from choosing multifocal lenses, and a national survey in 2019 reported that the rate of multifocal IOL use for cataract surgery in Japan was only 3.9%14.
However, to achieve the ultimate goals of cataract surgery, i.e., fast and complete visual rehabilitation and optimal satisfaction regarding vision-related issues, multifocal lenses have continually evolved over the years and achieved better outcomes15, and the range of choices is much larger now than in the past.
The Tecnis monofocal IOL (ZCB00) and the Tecnis multifocal IOL (ZMB00) are representative IOLs that have been used in Japan for more than a decade because of the high quality of the materials, as shown in previous reports; these lenses have an aspherical, modified prolate anterior surface that is designed to minimize spherical aberrations and improve contrast sensitivity under mesopic conditions after cataract surgery16,17,18. Except for additional bifocal diffraction gratings in the multifocal IOLs with + 4.0 dioptres, they have the same design as clear acrylic 6.0-mm optics.
In our previous study, we retrospectively compared the visual performance of two small groups of patients who received monofocal IOLs (ZCB00) (170 eyes of 85 patients) or multifocal IOLs (ZMB00) (92 eyes of 46 patients) in cataract surgery at the cataract unit of the Department of Ophthalmology of Tsukazaki Hospital between April 2009 and January 201219. In the current study, we obtained larger numbers of patients who received these lens types (ZCB00 monofocal IOLs, 904 eyes of 452 patients; ZMB00 multifocal IOLs, 1,326 eyes of 663 patients) from December 13, 2010, to July 29, 2019.
In this study, we retrospectively compared the visual performance of the Tecnis monofocal IOL (ZCB00) and the Tecnis multifocal IOL (ZMB00) based on the accumulated data of a decade of practice at a single eye institute.
Results
Patient characteristics
The patient demographics and pre/postoperative visual parameters are shown in Supplementary Table S1. The study enrolled 2,230 eyes of 1,115 patients. The monofocal group comprised 904 eyes of 452 patients (72.3 ± 6.8 years; females/males, 268 [59.3%]/184 [40.7%]), and the multifocal group comprised 1,326 eyes of 663 patients (67.0 ± 7.8 years; females/males, 518 [78.1%]/145 [21.9%]).
Comparison of postoperative parameters between Tecnis monofocal IOLs (ZCB00) and Tecnis multifocal IOLs (ZMB00)
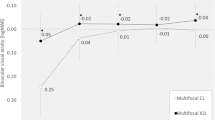
Multiple regression analysis was applied to all postoperative parameters of the monofocal and multifocal groups at 10 weeks after surgery on both eyes; the parameters were adjusted by multiple regression with the explanatory variables in Table 1, and the results of the analysis are shown in Supplementary Table S2. Contrast sensitivity (4.0/2.5/1.6/1.0/0.7 degrees), contrast sensitivity with glare (1.6/1.0/0.7 degrees), and the Visual Function Questionnaire (VFQ)-25 score for driving at night were significantly better in the monofocal group (p < 0.00068, Wald test), and corrected near visual acuity, contrast sensitivity (6.3 degrees), contrast sensitivity with glare (2.5 degrees), and the VFQ-25 scores for mental health/driving in general/driving during the day/driving in adverse conditions were likely better in the monofocal group (p < 0.05, Wald test) (Table 2, Figs. 1, 2). Uncorrected intermediate/near visual acuity and near spectacle independence were significantly better in the multifocal group (p < 0.00068, Wald test), and the VFQ-25 score for general health and distance spectacle independence were likely better in the multifocal group (p < 0.05, Wald test) (Table 2, Fig. 2).
Contrast sensitivity with or without glare in the monofocal and multifocal groups before and 10 weeks after surgery on both eyes. The solid line connects the median values for each group. Each parameter was adjusted by multiple linear regression with the explanatory variables in Table 1. The significance level was set to 0.0083 after Bonferroni’s correction.
Parameters that demonstrated a significant difference between the monofocal and multifocal groups at 10 weeks after surgery on both eyes. Each parameter was adjusted by multiple regression with the explanatory variables in Table 1.
Correlation among postoperative parameters of Tecnis monofocal IOLs (ZCB00) and Tecnis multifocal IOLs (ZMB00)
The correlation coefficients (A) and p values for the correlation analyses (B) between all possible combinations of postoperative parameters for the monofocal and multifocal groups were adjusted by multiple regression with the explanatory variables in Table 1 and are shown in Supplementary Table S3, Fig. 3, Supplementary Table S4, Fig. 4, respectively.
Heatmap of correlation coefficients between all possible combinations of variables, which were adjusted by multiple regression with the explanatory variables in Table 1, in the monofocal IOL group. The asterisk * in this figure indicates a significant correlation between two parameters at p < 0.00002 after Bonferroni’s correction. The illustration was performed using a commercially available software program (R, version 3.6.1; R Core Team, 2019, Vienna, Austria.)59 (https://cran.r-project.org/web/packages/pheatmap/pheatmap.pdf).
Heatmap of correlation coefficients between all possible combinations of variables, which were adjusted by multiple regression with the explanatory variables in Table 1, in the multifocal group. The asterisk * in this figure indicates a significant correlation between two parameters at p < 0.00002 after Bonferroni’s correction. The illustration was performed using a commercially available software program (R, version 3.6.1; R Core Team, 2019, Vienna, Austria)59 (https://cran.r-project.org/web/packages/pheatmap/pheatmap.pdf).
Discussion
We previously reported the results of a retrospective study in which we compared the visual performance of two small groups of patients who received monofocal IOLs (ZCB00) (170 eyes of 85 patients) or multifocal IOLs (ZMB00) (92 eyes of 46 patients)19. In that study, we showed that patients in the multifocal IOL group demonstrated better uncorrected near visual acuity and lower spectacle dependence (intermediate/near), and those in the monofocal IOL group had better CIVA/CNVA and higher VFQ-25 scores for night-time driving. In the current study, we obtained a larger number of samples based on data accumulated over a decade of practice at a single eye institute. The superior uncorrected intermediate visual acuity in the multifocal group and the lack of a significant difference in CIVA/CNVA and intermediate spectacle dependence between the two groups were novel results that build upon our previous report. Although many studies using modern multifocal IOLs have reported a noninferior CNVA in multifocal groups compared to monofocal groups20,21, a tendency toward better CNVA in the monofocal group is suggested again by the present study, although the results were not statistically significant. Diffractive multifocal IOLs divide light into two foci; Tecnis multifocal IOLs use 41% of incoming light for distance vision and 41% for near vision, regardless of the pupil diameter, whereas the remaining 18% is lost to higher-order scattering22,23. The 41% of light used for distance vision allows photopic, high-contrast distance acuity comparable to that provided by monofocal IOLs, as confirmed by recent studies2,24,25,26. The Array SA40N (AMO), a first-generation multifocal IOL, was a major step towards the safe and effective treatment of presbyopia and cataracts and achieved high levels of patient satisfaction13,27,28,29,30,31,32. However, a report demonstrated that even with the addition of near focus, the AMO provides poorer near contrast sensitivity than can be achieved by an appropriate monofocal near correction, regardless of the spatial frequency or illumination conditions, presumably due to the pupil constriction as a result of accommodation33 and the IOL characteristics24. The ZMB00 used in the present study is a second-generation multifocal IOL with an aspherical IOL design, which improves contrast sensitivity by reducing or cancelling the normal positive spherical aberration of the cornea, the performance of which is less dependent on pupil size. Aspherical IOLs have shown decreased wavefront spherical aberrations and improved contrast sensitivity compared with spherical IOLs16,34,35,36,37,38, and an aspherical multifocal IOL design thus reduces the incidence and severity of halos and glare, which are inherent in the design (i.e., edges of the steps of different ring zones) of diffractive multifocal IOLs and are seen more often with spherical multifocal IOLs. Likewise, improved quality of vision is also seen with monofocal aspherical IOL designs, such as that of the ZCB00 used in the present study39. Thus, we compared the two types of new-generation aspherical IOLs, and it was difficult to determine which lens is better or worse. We concluded that at a high level of performance, they have different characteristics in terms of various visual parameters.
We used the CGT1000 instrument to measure contrast sensitivity. In this method, patients are asked whether they can distinguish any changes in the brightness contrast of a circular optotype of variable size consisting of three coloured concentric circles. This device can measure contrast sensitivity at 6 sizes and 13 contrast levels with or without glare40. In this study, the contrast sensitivity measured with the CGT1000 was better in the monofocal group at most frequencies both with and without glare (Figs. 1, 2), a finding that is consistent with the findings of previous reports18,41,42. Although contrast sensitivity can theoretically deteriorate with the use of diffractive multifocal IOLs, our results indicate better contrast sensitivity, both with and without glare, in patients in the multifocal group than in the normal 60-year-old Japanese subjects evaluated by Takahashi43, as stated in our previous report19. In both the monofocal IOL and multifocal IOL groups, the heatmaps of the correlation coefficients between all possible combinations of variables, which were adjusted by multiple regression with the explanatory variables in Table 1, demonstrated that contrast sensitivity (with/without glare) and UDVA/CDVA/CNVA were strongly correlated with each other (Figs. 3, 4). In other words, contrast sensitivity (with/without glare) is suggested to play a very important role in UDVA/CDVA/CNVA. The tendency toward superior CNVA in the monofocal group might be due to the superior contrast sensitivity (with/without glare) in this group.
Approximately 82.2% of patients in the multifocal group were perfectly spectacle independent in our study, which is consistent with the finding of 85% in our previous report18 and the findings of other study reports on Tecnis multifocal IOLs, in which the percentage ranged from 82.6 to 92.8%2,20,42,44. In contrast, the rate of spectacle independence in the monofocal group was approximately 10.8% in our study. Near spectacle independence was significantly higher and distance spectacle independence was likely higher in the multifocal group. Multifocal glasses are a very common solution for presbyopia in Japan; thus, patients who undergo implantation with monofocal IOLs often use multifocal glasses after cataract surgery. This may help explain the higher ratio of distance spectacle dependence of patients in the monofocal IOL group, whose UDVA was sufficient.
The NEI VFQ-25 is a questionnaire used for scoring the self-reported, vision-targeted health status of people with chronic eye diseases45,46. It has been used in normal subjects as well as those with ocular diseases, such as age-related macular degeneration, cataracts, glaucoma, and Graves’ ophthalmopathy45,47,48,49,50,51,52. Changes in the NEI VFQ-25 score have been reported after surgery for cataracts, glaucoma, primary vitreous floaters, vitreomacular adhesion and macular holes53,54,55,56,57. The NEI VFQ-25 has been translated into several languages (including Italian, French, German, Spanish, Turkish, Chinese, Greek, Portuguese, Arabic, and Serbian), and the Japanese version of the NEI VFQ-25 was validated by Suzukamo et al.58. In our study, the VFQ-25 score for driving at night was significantly better in the monofocal group, and the VFQ-25 scores for driving in general, driving during the day, and driving in adverse conditions were likely better in the monofocal group. The actual VFQ-25 scores for driving at night, driving in general, driving during the day, and driving in adverse conditions in the monofocal and multifocal groups, however, showed no compromise, even in the multifocal group. Interestingly, the VFQ-25 score for mental health was likely better in the monofocal group, while the VFQ-25 score for general health was likely better in the multifocal group. The heatmap of the correlation coefficients in the monofocal IOL group demonstrated that the VFQ-25 score for general health significantly correlated with UDVA/CDVA, contrast sensitivity, and most ocular/internal higher-order aberrations scaled to a pupil size of 4 mm (Fig. 3). On the other hand, the heatmap of the correlation coefficients showed that the VFQ-25 score for mental health significantly correlated with contrast sensitivity in the multifocal group (Fig. 4). Considering the lack of significant correlations of the VFQ-25 score for mental health with UDVA/CDVA and any ocular/internal higher-order aberrations scaled to a pupil size of 4 mm in both IOL groups (Figs. 3, 4), we can conclude that different characteristics affect the factors related to these psychological evaluation items.
Alio et al.21 reported that the VFQ-25 scores for near vision are significantly better in patients with multifocal IOLs than in those with monofocal IOLs and that there are no significant differences in scores for night-time driving between the two groups. We hypothesize that the probable reasons for these discrepancies from our results are differences in the monofocal IOLs used in the study, i.e., Alio evaluated the Acri.Smart 48S (Carl Zeiss Meditec AG), a single-piece, spherical, foldable, acrylic IOL, and we evaluated aspherical monofocal IOLs, which achieve improved contrast sensitivity by reducing or cancelling the normal positive spherical aberration of the cornea and the incidence and severity of halos and glare. As mentioned above, two types of second-generation IOLs were compared with each other at a high level of performance. National differences in attitudes towards eyewear could also be a contributing factor. All of the subjects in our study were Japanese patients who had little psychological resistance against wearing glasses, especially those patients who opted for the implantation of monofocal IOLs. In Japanese culture, glasses are quite common, and many people do not feel inconvenienced if they must use glasses to read books or newspapers. We consider this phenomenon to partially explain why the VFQ-25 score for near vision of patients in the monofocal group was not inferior to that of patients in the multifocal group, who had better UNVA and UIVA and a higher rate of spectacle independence.
In conclusion, we compared the visual performance of monofocal IOLs and multifocal IOLs of the same material and basic design. Patients in the multifocal group had better uncorrected intermediate/near visual acuity and higher spectacle independence, whereas patients in the monofocal group had better contrast sensitivity and higher scores for night-time driving. The superior uncorrected intermediate visual acuity in the multifocal group and the lack of a significant difference in CIVA/CNVA and intermediate spectacle dependence between the two groups were novel results that build upon our previous report. At a high performance level, both IOL groups had different characteristics in terms of various visual parameters.
Methods
Design
Retrospective comparative case series.
Setting
Ophthalmology, Tsukazaki Hospital, Japan.
Patients
We reviewed the cases of cataract patients who underwent bilateral implantation of Tecnis monofocal IOLs (ZCB00) or Tecnis multifocal IOLs (ZMB00) from December 13, 2010, to July 29, 2019, with the right and left lenses implanted within 3 months of each other. The exclusion criteria were a history of other ocular diseases that could affect visual function, |subjective equivalent (SE)|> 2.00 dioptres, |subjective refraction cylinder (CYL)|> 3.00 dioptres and |corneal astigmatism (keratometric cylinder)|> 3.00 dioptres at 10 weeks after surgery.
Preoperative examination
Preoperatively, all patients received full ophthalmologic examinations, including evaluations of the corneal curvature radius, corneal astigmatism, axial length, refractive status, ocular aberrations, pupil diameter, distance/intermediate/near visual acuity, contrast sensitivity, and contrast sensitivity under glare, as well as anterior segment evaluations using a slit lamp, tonometry and indirect fundoscopy. The quality of vision was evaluated using the Japanese version of the 25-item National Eye Institute Visual Function Questionnaire (NEI VFQ-25)58. The NEI VFQ-25 was administered by experienced technicians or nurses in a face-to-face setting. Spectacle use was also evaluated by inquiring how often the patient used spectacles for distance, intermediate and near vision (with possible responses of ‘never,’ ‘sometimes’ or ‘always’).
Uncorrected distance visual acuity (UDVA) and corrected distance visual acuity (CDVA) were measured at 5.0 m. Uncorrected intermediate visual acuity (UIVA) and corrected intermediate visual acuity (CIVA) were measured at 0.5 m. Uncorrected near visual acuity (UNVA) and corrected near visual acuity (CNVA) were measured at 0.3 m. Visual acuity was measured using the decimal visual acuity chart, and the measured decimal values were converted to the logarithm of the minimum angle of resolution (logMAR) scale. The corneal curvature radius, corneal astigmatism and objective refractive status were measured using a KR-8900 autorefractor keratometer (Topcon, Tokyo, Japan). The axial length was measured using IOL Master (Carl Zeiss, Oberkochen, Germany) and AL-3000 (TOMEY, Nagoya, Japan) biometers. Contrast sensitivity and contrast sensitivity under glare were measured using a CGT-1000 contrast glare tester (Takagi Seiko, Nakano, Japan), and the pupil diameter and ocular aberrations were measured using a KR-1W Wavefront Analyzer (Topcon, Tokyo, Japan). All measurements were obtained by experienced technicians.
IOLs and surgical technique
The patients chose to undergo implantation with either monofocal or multifocal IOLs after they had been informed of the advantages and disadvantages associated with each type. Patients in the monofocal group received Tecnis monofocal IOLs (ZCB00) bilaterally, while those in the multifocal group received Tecnis multifocal IOLs (ZMB00) bilaterally. ZCB00 and ZMB00 have an aspherical, modified prolate anterior surface designed to minimize spherical aberrations and improve contrast sensitivity under mesopic conditions after cataract surgery16,17,18. Except for the additional bifocal diffraction gratings in multifocal IOLs with + 4.0 dioptres, they have the same design: both are clear acrylic optics measuring 6.0 mm in diameter.
Cataract surgeries were performed by 19 experienced cataract surgeons using the same standard technique of sutureless microincision phacoemulsification and the same protocol. The surgical procedures consisted of topical anaesthesia, the creation of a scleral or corneal incision of 1.8 to 2.8 mm, 5 mm of continuous capsulorhexis, phacoemulsification cataract extraction and IOL implantation with an injector.
Postoperative examination
Patients were evaluated at 10 weeks postoperatively. The postoperative examination protocol at 10 weeks was identical to the preoperative protocol.
Statistical analyses
The two groups (monofocal IOL and multifocal IOL) were compared in terms of the following postoperative parameters at 10 weeks after surgery for both eyes: (1) mixed-effects linear regression: visual acuity (uncorrected/corrected, distance/intermediate/near), contrast sensitivity (with/without glare), and higher-order aberrations (ocular/internal, scaled to a pupil size of 4 mm/6 mm); (2) linear regression model or logistic regression: VFQ-25 score; and (3) cumulative logistic regression: spectacle dependence (distance/intermediate/near). Both groups were adjusted for age, sex, axial length, subjective refraction spherical equivalent, subjective refraction cylinder, corneal astigmatism, corneal higher-order aberrations and pupil diameter. In the regression analysis (2) and (3), the data were divided into two parts (left-eye data and right-eye data), and the regression model was applied to each data set. Since discrete scores were observed for “Peripheral_Vision”, “Color_Vision”, “Driving_Daytime”, “Driving_Nighttime”, “Driving_Adverse_Conditions” in VFQ-25, we treated them as binary data. We divided the patients into two groups (those with scores of 75 or lower and those with scores above 75) and applied the logistic regression model to them. The results of the left- and right-eye analyses were combined using the inverse variance method; the corrected values were calculated for the left- and right-eye datasets, and the average values were used.
In the regression analysis, the Wald test was applied to evaluate the significance of differences in postoperative parameters between the two groups, and the significance level was set to 0.00068 after Bonferroni’s correction. Correlation analysis between postoperative parameters was applied for the monofocal and multifocal groups, and a heatmap of Pearson’s correlation coefficients was generated for each group. In the correlation analysis, the t-test was used to evaluate whether the correlation coefficient was significantly different from zero, and the significance level was set to 0.00002 after Bonferroni’s correction.
The statistical analyses were performed using a commercially available software program (R, version 3.6.1; R Core Team, 2019, Vienna, Austria)59.
Ethics statement
This study conformed to the tenets of the Declaration of Helsinki and was approved by the Ethics Committee of Tsukazaki Hospital. Written informed consent was obtained from each subject. This study was registered as UMIN000035630: ‘‘Performance comparison among different intraocular lenses in cataract surgery’’.
Data availability
All data relevant to the study are included in this article or have been uploaded as supplementary information.
Change history
05 November 2020
An amendment to this paper has been published and can be accessed via a link at the top of the paper.
References
Pepose, J. S. et al. Visual performance of patients with bilateral vs combination crystalens, ReZoom, and ReSTOR intraocular lens implants. Am. J. Ophthalmol. 144, 347–357 (2007).
Mester, U., Hunold, W., Wesendahl, T. & Kaymak, H. Functional outcomes after implantation of Tecnis ZM900 and Array SA40 multifocal intraocular lenses. J. Cataract Refract. Surg. 33, 1033–1040 (2007).
Alio, J. L. et al. Near vision restoration with refractive lens exchange and pseudoaccommodating and multifocal refractive and diffractive intraocular lenses: Comparative clinical study. J. Cataract Refract. Surg. 30, 2494–2503 (2004).
Alio, J. L., Elkady, B., Ortiz, D. & Bernabeu, G. Clinical outcomes and intraocular optical quality of a diffractive multifocal intraocular lens with asymmetrical light distribution. J. Cataract Refract. Surg. 34, 942–948 (2008).
Zelichowska, B., Rekas, M., Stankiewicz, A., Cervino, A. & Montes-Mico, R. Apodized diffractive versus refractive multifocal intraocular lenses: Optical and visual evaluation. J. Cataract Refract. Surg. 34, 2036–2042 (2008).
Alfonso, J. F., Fernandez-Vega, L., Baamonde, M. B. & Montes-Mico, R. Prospective visual evaluation of apodized diffractive intraocular lenses. J. Cataract Refract. Surg. 33, 1235–1243 (2007).
Kohnen, T. et al. European multicenter study of the AcrySof ReSTOR apodized diffractive intraocular lens. Ophthalmology 113, 584 (2006).
Weghaupt, H., Pieh, S. & Skorpik, C. Visual properties of the foldable array multifocal intraocular lens. J. Cataract Refract. Surg. 22, 1313–1317 (1996).
Leyland, M. & Zinicola, E. Multifocal versus monofocal intraocular lenses in cataract surgery: A systematic review. Ophthalmology 110, 1789–1798 (2003).
Woodward, M. A., Randleman, J. B. & Stulting, R. D. Dissatisfaction after multifocal intraocular lens implantation. J. Cataract Refract. Surg. 35, 992–997 (2009).
Montes-Mico, R. & Alio, J. L. Distance and near contrast sensitivity function after multifocal intraocular lens implantation. J. Cataract Refract. Surg. 29, 703–711 (2003).
Pieh, S. et al. Halo size under distance and near conditions in refractive multifocal intraocular lenses. Br. J. Ophthalmol. 85, 816–821 (2001).
Steinert, R. F., Aker, B. L., Trentacost, D. J., Smith, P. J. & Tarantino, N. A prospective comparative study of the AMO ARRAY zonal-progressive multifocal silicone intraocular lens and a monofocal intraocular lens. Ophthalmology 106, 1243–1255 (1999).
Sato, M. et al. JSCRS clinical survey. IOL&RS 33, 453–473 (2019).
Khandelwal, S. S., Jun, J. J., Mak, S., Booth, M. S. & Shekelle, P. G. Effectiveness of multifocal and monofocal intraocular lenses for cataract surgery and lens replacement: A systematic review and meta-analysis. Graefe’s Arch. Clin. Exp. Ophthalmol. 257, 863–875 (2019).
Packer, M., Fine, I. H., Hoffman, R. S. & Piers, P. A. Improved functional vision with a modified prolate intraocular lens. J. Cataract Refract. Surg. 30, 986–992 (2004).
Bellucci, R. et al. Visual acuity and contrast sensitivity comparison between Tecnis and AcrySof SA60AT intraocular lenses: A multicenter randomized study. J. Cataract Refract. Surg. 31, 712–717 (2005).
Denoyer, A., Le Lez, M. L., Majzoub, S. & Pisella, P. J. Quality of vision after cataract surgery after Tecnis Z9000 intraocular lens implantation: Effect of contrast sensitivity and wavefront aberration improvements on the quality of daily vision. J. Cataract Refract. Surg. 33, 210–216 (2007).
Yamauchi, T. et al. Comparison of visual performance of multifocal intraocular lenses with same material monofocal intraocular lenses. PLoS ONE 8, e68236 (2013).
Cillino, S. et al. One-year outcomes with new-generation multifocal intraocular lenses. Ophthalmology 115, 1508–1516 (2008).
Alio, J. L. et al. Quality of life evaluation after implantation of 2 multifocal intraocular lens models and a monofocal model. J. Cataract Refract. Surg. 37, 638–648 (2011).
Hutz, W. W., Eckhardt, H. B., Rohrig, B. & Grolmus, R. Reading ability with 3 multifocal intraocular lens models. J. Cataract Refract. Surg. 32, 2015–2021 (2006).
Pieh, S. et al. Quantitative performance of bifocal and multifocal intraocular lenses in a model eye: Point spread function in multifocal intraocular lenses. Arch. Ophthalmol. 120, 23–28 (2002).
Montes-Mico, R., Espana, E., Bueno, I., Charman, W. N. & Menezo, J. L. Visual performance with multifocal intraocular lenses: Mesopic contrast sensitivity under distance and near conditions. Ophthalmology 111, 85–96 (2004).
Sen, H. N., Sarikkola, A. U., Uusitalo, R. J. & Laatikainen, L. Quality of vision after AMO array multifocal intraocular lens implantation. J. Cataract Refract. Surg. 30, 2483–2493 (2004).
Richter-Mueksch, S., Weghaupt, H., Skorpik, C., Velikay-Parel, M. & Radner, W. Reading performance with a refractive multifocal and a diffractive bifocal intraocular lens. J. Cataract Refract. Surg. 28, 1957–1963 (2002).
Brydon, K. W., Tokarewicz, A. C. & Nichols, B. D. AMO array multifocal lens versus monofocal correction in cataract surgery. J. Cataract Refract. Surg. 26, 96–100 (2000).
Featherstone, K. A. et al. Driving simulation study: Bilateral array multifocal versus bilateral AMO monofocal intraocular lenses. J. Cataract Refract. Surg. 25, 1254–1262 (1999).
Javitt, J. C. & Steinert, R. F. Cataract extraction with multifocal intraocular lens implantation: A multinational clinical trial evaluating clinical, functional, and quality-of-life outcomes. Ophthalmology 107, 2040–2048 (2000).
Javitt, J. et al. Cataract extraction with multifocal intraocular lens implantation: Clinical, functional, and quality-of-life outcomes. Multicenter clinical trial in Germany and Austria. J. Cataract Refract. Surg. 26, 1356–1366 (2000).
Pearce, J. L. Multifocal intraocular lenses. Curr. Opin. Ophthalmol. 8, 2–5 (1997).
Steinert, R. F. Visual outcomes with multifocal intraocular lenses. Curr. Opin. Ophthalmol. 11, 12–21 (2000).
Alpern, M., Mason, G. L. & Jardinico, R. E. Vergence and accommodation. V. Pupil size changes associated with changes in accommodative vergence. Am. J. Ophthalmol. 52, 762–767 (1961).
Packer, M., Fine, I. H. & Hoffman, R. S. Wavefront technology in cataract surgery. Curr. Opin. Ophthalmol. 15, 56–60 (2004).
Bellucci, R. & Morselli, S. Optimizing higher-order aberrations with intraocular lens technology. Curr. Opin. Ophthalmol. 18, 67–73 (2007).
Denoyer, A., Halfon, J., Majzoub, S. & Pisella, P. J. Quels bénéfices visuels peut-on attendre d’un implant sans aberration sphérique dans la chirurgie de la cataracte?. J. Fr. Ophtalmol. 30, 578–584 (2007).
Rocha, K. M. et al. Wavefront analysis and contrast sensitivity of aspheric and spherical intraocular lenses: A randomized prospective study. Am. J. Ophthalmol. 142, 750–756 (2006).
Munoz, G., Albarran-Diego, C., Montes-Mico, R., Rodriguez-Galietero, A. & Alio, J. L. Spherical aberration and contrast sensitivity after cataract surgery with the Tecnis Z9000 intraocular lens. J. Cataract Refract. Surg. 32, 1320–1327 (2006).
Dick, H. B. Recent developments in aspheric intraocular lenses. Curr. Opin. Ophthalmol. 20, 25–32 (2009).
Pesudovs, K. Takagi glare tester CGT-1000 for contrast sensitivity and glare testing in normal individuals and cataract patients. J. Refract. Surg. 23, 492–498 (2007).
Palmer, A. M. et al. Visual function with bilateral implantation of monofocal and multifocal intraocular lenses: A prospective, randomized, controlled clinical trial. J. Refract. Surg. 24, 257–264 (2008).
Packer, M. et al. Evaluation of the aspheric Tecnis multifocal intraocular lens: one-year results from the first cohort of the food and drug administration clinical trial. Am. J. Ophthalmol. 149, 577-584.e1 (2010).
Takahashi, Y. Contrast glare tester. IOL & RS 15, 192–199 (2001).
Goes, F. J. Visual results following implantation of a refractive multifocal IOL in one eye and a diffractive multifocal IOL in the contralateral eye. J. Refract. Surg. 24, 300–305 (2008).
Mangione, C. M. et al. Identifying the content area for the 51-item national eye institute visual function questionnaire: Results from focus groups with visually impaired persons. Arch. Ophthalmol. 116, 227–233 (1998).
Mangione, C. M. et al. Development of the 25-item national eye institute visual function questionnaire. Arch. Ophthalmol. 119, 1050–1058 (2001).
Gomi, F. et al. Vision-related quality of life in Japanese patients with wet age-related macular degeneration treated with intravitreal aflibercept in a real-world setting. Jpn. J. Ophthalmol. 63, 437–447 (2019).
Jelin, E., Wisløff, T., Jørstad, ØK., Heiberg, T. & Moe, M. C. Patient-reported outcome measures in the management of neovascular age-related macular degeneration: A 1-year prospective study. BMJ Open Ophthalmol. 4, e000353 (2019).
Hyman, L. G., Komaroff, E., Heijl, A., Bengtsson, B. & Leske, M. C. Treatment and vision-related quality of life in the early manifest glaucoma trial. Ophthalmology 112, 1505–1513 (2005).
Riva, I. et al. Vision-related quality of life and symptom perception change over time in newly-diagnosed primary open angle glaucoma patients. Sci. Rep. 9, 6735 (2019).
Rulli, E. et al. Visual field loss and vision-related quality of life in the Italian primary open angle glaucoma study. Sci. Rep. 8, 619 (2018).
Bradley, E. A. et al. Evaluation of the national eye institute visual function questionnaire in graves’ ophthalmopathy. Ophthalmology 113, 1450–1454 (2006).
De Carneros-Llorente, A. M., De Carneros, A. M., De Carneros-Llorente, P. M. & Jimenez-Alfaro, I. Comparison of visual quality and subjective outcomes among 3 trifocal intraocular lenses and 1 bifocal intraocular lens. J. Cataract Refract. Surg. 45, 587–594 (2019).
Agnifili, L. et al. The ocular surface after successful glaucoma filtration surgery: A clinical, in vivo confocal microscopy, and immune-cytology study. Sci. Rep. 9, 11299 (2019).
De Nie, K. F., Crama, N., Tilanus, M. A., Klevering, B. J. & Boon, C. J. Pars plana vitrectomy for disturbing primary vitreous floaters: Clinical outcome and patient satisfaction. Graefe’s Arch. Clin. Exp. Ophthalmol. 251, 1373–1382 (2013).
Varma, R., Haller, J. A. & Kaiser, P. K. Improvement in patient-reported visual function after ocriplasmin for vitreomacular adhesion: Results of the microplasmin for intravitreous injection-traction release without surgical treatment (MIVI-TRUST) trials. JAMA Ophthalmol. 133, 997–1004 (2015).
Hirneiss, C. et al. Visual quality of life after macular hole surgery: Outcome and predictive factors. Br. J. Ophthalmol. 91, 481–484 (2007).
Suzukamo, Y. et al. Psychometric properties of the 25-item national eye institute visual function questionnaire (NEI VFQ-25), Japanese version. Health Qual. Life Outcomes 3, 65 (2005).
R Core Team. R: A Language and Environment for Statistical Computing (R Foundation for Statistical Computing, 2019).
Acknowledgements
We thank all of the staff of Tsukazaki Hospital who were involved in this study. The results of our manuscript were statistically reviewed by a professional data analysis company in Japan (StaGen Co., Ltd.).
Author information
Authors and Affiliations
Contributions
H.T. (Hirotaka Tanabe), H.T. (Hitoshi Tabuchi) and T.Y. conceived the study; T.S. and K.T. conducted the examinations and collected data; and H.T. (Hirotaka Tanabe) analysed the results and wrote the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tanabe, H., Tabuchi, H., Shojo, T. et al. Comparison of visual performance between monofocal and multifocal intraocular lenses of the same material and basic design. Sci Rep 10, 15490 (2020). https://doi.org/10.1038/s41598-020-72473-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-72473-x
- Springer Nature Limited
This article is cited by
-
Comparison of visual performance between diffractive bifocal and diffractive trifocal intraocular lenses
Scientific Reports (2024)
-
Comparison of bilateral implantation of an extended depth of focus lenses and a blend approach of extended depth of focus lenses and bifocal lenses in cataract patients
BMC Ophthalmology (2023)
-
Myope multifokale Duett-Implantation zur Korrektur von Presbyopie und Myopie
Die Ophthalmologie (2023)
-
Comparative analysis of a presbyopia-correcting intraocular lens that combines extended depth-of-focus and bifocal profiles with a standard monofocal intraocular lens
BMC Ophthalmology (2022)
-
Comparative visual performance of diffractive bifocal and rotationally asymmetric refractive intraocular lenses
Scientific Reports (2022)