Abstract
To explore the factors (including knowledge and attitude) influencing the decision to follow a low-carbohydrate diet (LCD) or not in a sample of the UK population. An online questionnaire was distributed electronically to adults who had either followed LCD or not (February–December 2019). Demographics and self-reported “LCD-status” (current, past and non-follower) were collected. Multivariable linear regression was used with carbohydrate knowledge, dietary guideline agreement and theory of planned behaviour (TPB) constructs (all as predictors) to explain the intention to follow a LCD (outcome). Respondents (n = 723, 71% women, median age 34; 85% white-ethnicity) were either following (n = 170, 24%) or had tried a LCD in the preceding 3 months (n = 184, 25%). Current followers had lower carbohydrate knowledge scores (1–2 point difference, scale − 11 to 11) than past and non-followers. A majority of current LCD followers disagreed with the EatWell guide recommendations “Base meals on potatoes, bread, rice and pasta, or other starchy carbohydrates. Choose whole grains where possible” (84%) and “Choose unsaturated oils and spreads and eat in small amounts such as vegetable, rapeseed, olive and sunflower oils” (68%) compared to past (37%, 10%, respectively) and non-followers (16%, 8%, respectively). Weight-loss ranked first as a motivation, and the internet was the most influencial source of information about LCDs. Among LCD-followers, 71% reported ≥ 5% weight loss, and over 80% did not inform their doctor, nurse, or dietitian about following a diet. Approximately half of LCD followers incorporated supplements to their diets (10% used multivitamin/mineral supplements), despite the restrictive nature of the diet. TPB constructs, carbohydrate knowledge, and guideline agreement explained 60% of the variance for the intention to follow a LCD. Attitude (std-β = 0.60), perceived behavioural control (std-β = 0.24) and subjective norm (std-β = 0.14) were positively associated with the intention to follow a LCD, while higher knowledge of carbohydrate, and agreeing with national dietary guidelines were both inversely associated (std-β = − 0.09 and − 0.13). The strongest primary reason behind UK adults’ following a LCD is to lose weight, facilitated by attitude, perceived behavioural control and subjective norm. Higher knowledge about carbohydrate and agreement with dietary guidelines are found among people who do not follow LCDs.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Low-carbohydrate and reduced carbohydrate diets (LCD) have become popular for weight loss and as a possible strategy for type 2 diabetes management1. Although not superior to conventional weight-loss diets, LCD interventions can generate weight loss, and improve glucose control in people with obesity and/or diabetes2, 3. LCDs have been used intermittently for centuries but gained recent popularity ever since the Atkins diet was first introduced in 19724. Successful weight loss journeys with LCDs by celebrities have been highlighted in the media, partly driving the renewed appeal of LCDs for the public5, 6. Media polls have estimated that 3 million people in the UK, approximately 7% of men and 10% of women, have tried LCDs7, similar to 7% in a population survey in Finland8, and up to 17% in surveys from the US9 and Australia10. A recent Food and Health survey11 of 1,009 Americans in 2018 also showed that 16% of respondents had followed a LCD, similar to findings in 20089.
There is a lack of a consensus what constitutes a diet “low” in carbohydrates, with references to carbohydrate-reduced diets, low-carbohydrate diets (LCDs), low-carbohydrate high-fat diets (LCHF), creating a major issue when communicating about these diets. A group of experts in the field has recommended that a carbohydrate content < 26% of energy (or < 130 g/day) could qualify as a criterion for LCDs12. However, our recent systematic review of published meta-analyses of LCDs found that the criteria for LCDs in the literature varied significantly2. Some authors defined LCDs based on a maximum intake of carbohydrate from 60 g per day13,14,15,16, to a maximum of 120 g per day17 without energy restriction (most trials of LCDs used ad libitum recommendation), while other authors defined LCDs based on maximum percentage energy contribution from carbohydrate ranging from 20% of energy13, 15, to 45% of energy per day18,19,20. With this range of criteria and definitions, understanding of what constitutes a LCD in the lay population is likely to vary, and are likely to include diets such as the Atkins diet, ketogenic diet or Paleolithic diet.
Despite the increasing popularity of LCDs, little is known about the nutritional behaviour of people who identify as LCD followers, including their socio-economic backgrounds21. Analysis of the possible impacts on health may be confounded by reverse causality in surveys, as these individuals may have pre-existing illness, and many other determinants could influence a decision to try to follow, or not follow, a particular diet22. Poor or incomplete knowledge on the nutritional compositions of foods and the balance of an overall diet, coupled with incorrect beliefs about food and health, may put people who attempt to follow a LCD at risk if their diet is not guided professionally1, 23, 24. National dietary guidelines are compiled by independent scientific and medical experts, based on the totality of the nutritional evidence, and there is evidence that higher adherence to dietary guidelines is linked with a reduction in chronic disease risks25,26,27. Knowledge of guideline recommendations is intended to improve individuals’ food choices, but journalistic scepticism and a lack of understanding of scientific evidence can lead to inappropriate rejection of guidelines in many fields28, 29.
Among the theoretical models/theories commonly used to explain human behaviours, in this case food choice, the Theory of Planned Behaviour (TPB) is widely accepted as valid and has been extensively used to study dietary behaviour and to design interventions for behavioural change30,31,32. The other popular model is the transtheoretical model of behaviour change (TMBC), which is used to identify people’s stage of change and to tailor interventions to changes in their behaviour. The rationale for including the TPB over the TMBC is that the aim of this paper is to explore the factors influencing following a LCD (or not), with the TPB specifically identifying intention as a central concept and exploring explicit factors explaining the intention to perform the chosen behaviour33. The TPB model identifies intention as the most powerful psychological determinant to eat a LCD or not, predicted by three other psychological constructs: attitude towards the LCD behaviour (i.e. the perception of benefits or harms of following a LCD), subjective norm (i.e. the social pressure or the perception of others would want one to follow or not to follow a LCD), and perceived behavioural control over the behaviour (i.e. the perception of self-efficacy or ability, or the perception of ease or difficulty to follow a LCD)30, 31.
Few studies have explored dietary intake or motivations in self-reported LCD followers8, 21, 34, and the empirical evidence is lacking to explain low-carbohydrate dieting behaviour using the TPB theoretical framework. Furthermore, the perceptions or opinions regarding LCDs among people who are not following this diet are not documented. Therefore, the present study investigates the possible factors which might help understand decisions to follow a LCD, or not, in UK adults.
Results
Respondents’ characteristics
A total of 723 respondents (515 women, 71%) completed the online questionnaire, with a median age of 34 years and 85% identifying as ‘white’ ethnicity (Table 1). Nearly half of all respondents were either following (n = 170) or had previously tried any LCDs (n = 184). Median body mass index (BMI) of current LCD followers (25.5 kg/m2) and past followers (26.4 kg/m2) were higher than non-followers (23.7 kg/m2, p < 0.001; Table 1). Current and past LCD followers also had a higher number of co-morbidities than non-followers. Type 2 diabetes and dyslipidaemia were more prevalent in current followers compared to past and non-followers (Table 1).
Nearly 60% of current LCD followers reported an annual household income level of at least £30,000 (UK) per year (approximately $35,000 US), compared to 47% of past followers and 39% of non-followers (Table 1). There was no difference in education level among LCD followers and non-followers, while confidence in cooking abilities was higher in current LCD followers (Table 1). Interestingly, those with a study background in medicine were represented in a greater proportion among current LCD followers (9%) than past (4%) or non-followers (4%; p = 0.01; Table 1).
Nutritional supplement use
Nearly half of current LCD followers took nutritional supplements, compared to 37% of past followers and 34% of non-followers (p < 0.001; Table 1). Among them, 20% of current LCD followers took 3 or more supplements, double the proportion of past (8%) and non-followers (7%) (Table 1). Vitamin D was the most used supplement overall (13% of study respondents), highest in current LCD followers (22%), compared to past (12%) and non-followers (9%; p < 0.001; Table 1). Folate (4%), calcium (4%), magnesium (17%) and zinc (6%) were all used more often by current LCD followers than past and non-followers (all p < 0.05; Table 1). Approximately 10% across LCD-followers and non-followers used multivitamins/minerals supplements.
Frequency of consumption and estimation of foods and nutrient intake as assessed by Dietary Targets Monitor (DTM)
Dietary assessment using the DTM food frequency questionnaire enabled monitoring of dietary targets, rather than assessing actual intakes. The tool allowed a comparison of the estimated intake and frequency of consumption between groups of respondents. Consumption of starchy foods (breads, cereals, pasta, rice, and potatoes excluding chips) was low (median intake of 0.9 times/week; IQR 0.5–4.5) in current LCD followers compared to past followers (12 times/week; IQR 7.6–16.5) and non-LCD followers (14.5 times/week; IQR 10–20; p < 0.001; Table 2).
The DTM was not designed to calculate absolute intake of starchy foods, so we assumed that a strict LCD would limit starchy foods to ≤ 1 time/day. With this assumption, 81% of current LCD followers strictly consumed starchy foods ≤ 1 time/day. Approximately 20% of past-LCD followers still limited their starchy food intake to ≤ 1 time/day. Interestingly, 10% of non-LCD followers also reported starchy foods consumption of ≤ 1 time/day. Considering other carbohydrate-rich foods (fruits, sweets and chocolates, ice cream, crisps and snacks, cake and pastries, biscuit, fruit juice, and soft drinks) in combination to starchy foods intake, we found that 48% of current LCD followers strictly limited all carbohydrate-rich foods intake to ≤ 1 time/day.
In contrast, consumption of meat and processed meat, cheese, and fish were greater in current LCD followers than past and non-followers. There was no difference in the frequency of chicken, beans and pulse intake between LCD followers and non-followers (median intakes of 3 times/week, Table 2). Current LCD followers reported consumption of sweet, chocolates, ice cream, snacks, cake and pastries, biscuit and soft drinks (0.13 times/week across all food items) lower than past and non-followers (consumption ranging from 0.13 to 3 times/week, Table 2).
The DTM estimates the absolute intakes of fish, fruit and vegetables and fat, in order to evaluate whether they met the dietary targets. Greater amounts of fish were consumed by current LCD followers (median 371 g/week) compared to past followers (134 g/week) and non-followers (119 g/week) (Table 2). Approximately half of current LCD followers met the target for total fish intake, compared to 20% of past and non-followers (p < 0.001; Table 2).
Fruits and vegetables intakes were also lower in current LCD followers (median 338 g/day), compared to 494 g/day and 425 g/day in past followers and non-followers (p < 0.001). Similarly, 42% of current LCD followers met the target for fruits and vegetables intakes (≥ 400 g/day), which was lower than past (62%) and non-followers (70%; p = 0.001; Table 2). When looking at the frequency of consumption, we found that fruit was consumed less by current followers than past and non-followers, while there was no difference in vegetable consumption (Table 2). Consumption of saturated fat was higher in current followers (median 35 g/day; IQR 25–51) than past followers (median 30 g/day; IQR 19–41), while there was no difference in total fat intake across all groups (median intake ranged from 65 to 69 g/day, p = 0.22).
Perceived understanding and knowledge of carbohydrates
When asking about perceived understanding of carbohydrates, 89% of current LCD followers reported that they had a very good idea about carbohydrates, higher than past (59%) and non-LCD followers (47%; Table 3). However, the median carbohydrate knowledge score of current LCD followers (6; IQR 5–8) was lower than scores of past (8; IQR 6–9) and non-LCD followers (7; IQR 5–9; Table 3).
We further explored whether the level of perceived understanding of carbohydrates aligned with knowledge. Among past LCD followers and non-followers, respondents who had higher confidence about their understanding of carbohydrates also had higher knowledge score (r = 0.27 and 0.37, p < 0.001). This correlation was not evident among current LCD followers (r = − 0.05, p = 0.54), with knowledge scores similar across levels of perceived understanding (Supplemental Figure S1). Notably, although 89% of current followers reported ‘very good’ idea about carbohydrates, only 28% (n = 47) of them achieved an above-median knowledge score (Table 3).
Agreement with dietary guidelines
Approximately half of the study sample was aware of existing national dietary guidelines (Table 3). Current LCD followers were more aware of the Eatwell guide (67%) than past (48%) and non-followers (40%). A minority (5%) of current LCD followers reported following the guideline, 3-time less than past and non-followers (13% and 15%; Table 3).
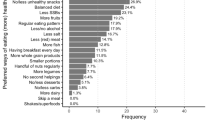
Main disagreement of current LCD followers with individual UK Eatwell guide statements, focused on ‘base meals on potatoes, bread, rice, pasta or other starchy carbohydrates. Choose wholegrain where possible’ (84%), followed ‘choose unsaturated oils and spreads and eat in small amounts such as vegetable, rapeseed, olive and sunflower oils’ (68%). On the other hand, a majority of past and non-followers agreed with the statement about vegetable oils (82% and 81%), 5-a-day fruit and vegetable intake (93% and 94%) and recommendation to eat less foods high in fat, salt and sugars (e.g. cake, biscuit, soft drinks) (74% and 80%). The statement about starchy foods was the most divergent finding between groups (Fig. 1).
Nutritional behaviour of current and past LCD followers
The most common type of LCD followed (past and current) were individual variations on the concept, not aligned with any specific named diet (57%), followed by the ketogenic diet (40%), and the Atkins diet (27%). The median of duration following the diet was 8 months (Table 4). Top three motivations to follow a LCD included losing weight (59%), perception of LCDs being better for health (22%), and for diabetes management (10%) (Table 4). Most respondents consumed a LCD every day at every meal (48%), 4–5 days a week (32%), weekday only (10%) and up to 3 days a week (6%). Nearly 60% reported that the portion size of their meals was smaller while following a LCD, while 22% reported bigger portion sizes (Table 4).
Most current and past LCD followers (n = 200, 71%) reported a weight loss of at least 5% of their baseline body weight, with n = 13 reporting weight loss higher than 30% after LCDs. A minority of respondents (6–10%) reported receiving any support from doctors or other health care professionals (HCP; i.e. dietitian, nurse, nutritionist). Specifically, current followers (n = 27; 16%) had more support from doctors than past followers (n = 6; 4%; Table 4). In contrast, over 80% of both current and past followers reported that their doctors/HCPs did not know that they were following a LCD (Table 4).
Experiences while following a LCD differed between current and past followers (Fig. 2). Among current LCD followers, improvements in all experiences were reported more often than worsening, with an improvement in energy the most common (85%), followed by happiness and confidence (83%; Fig. 2A). A different profile of experiences was reported by past followers, with most of the experiences reported to worsen, with perception of hunger the most often reported negative perceived consequence (56%). Happiness and confidence (52%), blood sugar (20%), and blood lipids (10%) were three experiences reported more often as improving rather than worsening (15%, 11%, and 2% respectively) in past followers (Fig. 2B).
Psychological constructs and health beliefs of the theory of planned behaviour
The TPB model was applied to explore the attitude, subjective norms, and perceived control over the behaviour. Current followers had the greatest intention to follow a LCD (median 7: strongly agree; IQR 7–7), followed by past followers (median 5: slightly agree; IQR 3–6), whereas non-followers’ intention was in disagreement with following a LCD (median 3: slightly disagree; IQR 1–4; p < 0.001; Table 5).
Attitude and behavioural beliefs (indirect measurement of attitude)
Current followers displayed the most positive attitude toward following a LCD (median 7: strongly agree; IQR 6–7), compared to past followers (5: slightly agree; IQR 4–6) and non-followers (4: neutral; IQR 3–5; p < 0.001). Regarding behavioural beliefs, current followers were most in favour with following a LCD (behavioural belief composite score median 36; IQR 23–42), followed by past followers (median 12; IQR 0–27), while non-followers had neutral attitude toward LCD (median 0; IQR − 12.5 to 10; p < 0.001; Table 5).
Specifically, behavioural beliefs about “good for weight management” and “reduced risk of chronic disease” of current followers were at the maximum positive scores (both median 21; IQR 12, 21), representing positive attitude in favour of following a LCD. On the other hand, non-LCD followers had negative attitude toward following a LCD explained by negative scores regarding behavioural beliefs about unfavourable consequences of LCD, namely “LCD and risk of micronutrient inadequacy” and “side effects of LCD” (Table 5).
Subjective norm and normative beliefs (indirect measurement of subjective norm)
Current followers had the greatest subjective norm scores (median 6: agree; IQR 4–7), while past and non-followers showed neutral agreement with subjective norm statements (both median 4) to follow a LCD. Similarly, current followers showed the highest positive normative belief composite scores (median 19; IQR 8–32), followed by past followers (median 3.5; IQR − 10 to 19) reflecting that they perceived positive social pressure to follow a LCD, whereas non-followers had negative composite score reflecting negative social pressure against following a LCD (median − 11; IQR − 21 to 0; p < 0.001; Table 5).
Further insight into sources of social pressure (each normative belief, i.e. family, friends, doctors, books, and the internet) showed that the internet was the main positive social pressure (median 10; IQR 4–18) to follow a LCD in current followers and past followers, while the other four normative beliefs showed neutral or negative effect. On the other hand, non-followers perceived negative social pressure from family, books, and the internet against following a LCD (Table 5).
Perceived behavioural control and control beliefs (indirect measurement of perceived behavioural control)
Perceived behavioural control is the perception of self-efficacy or ability to carry out a given behaviour. Again, current followers showed the greatest perceived behavioural control over following a LCD (median 7: strongly agree; IQR 6–7) compared to past (median 6: agree; IQR 5–7) and non-followers (median 5.5: between slightly agree to agree; IQR 4–6; p < 0.001; Table 5). Regarding control beliefs, current followers felt in control to follow a LCD (control belief composite score median 9; IQR − 6 to 22) while past followers (median − 12; IQR − 28 to 3) and non-followers (median − 10; IQR − 26 to 10; p < 0.001) did not (Table 5).
The control belief factor, “People around me have carbohydrates in their diets” and “no time to cook/prepare meals” were not recognised as barriers by LCD followers (median score 6 and 2 respectively), unlike past and non-followers (median scores ranging from − 2 to − 7; Table 5). The control belief “LCD products are expensive and less available” was also not recognised as a barrier by LCD followers, while past and non-followers held a neutral opinion on the matter (Table 5).
Path analysis explaining low-carbohydrate dieting behaviour
Path analysis was applied to investigate the TBP psychological constructs, carbohydrate knowledge and dietary guideline agreement explaining the intention to follow a LCD (Fig. 3). As proposed in the TPB model, intention is the strongest determinant in performing behaviour, although perceived behavioural control could also influence the behaviour performance. In this study, we defined behaviour using the frequency of starchy food intake as an outcome variable and intention and perceived behaviour control as predictor variables. We found that higher intention to follow a LCD was associated with a lesser frequency of starchy food intake (standardized β − 0.38, p < 0.001). Perceived behavioural control was also associated with frequency of consumption with lesser effect size (standardized β − 0.10, p < 0.01; Supplemental Table S1).
Path analysis of the theory of planned behaviour constructs with their corresponding health beliefs, carbohydrate knowledge and dietary guideline agreement to explain intention and behaviour to follow a low-carbohydrate diet. Values are standardized β-coefficients; **p < 0.01, ***p < 0.001; LCD low-carbohydrate diet, CHO carbohydrate.
The TPB model also indicates that intention can be predicted by attitude, subjective norm, and perceived behavioural control. We found that attitude, subjective norm and perceived behavioural control were also positively associated with intention to follow a LCD (adjusted R2 = 0.58, p < 0.001), with influence of attitude on intention to follow a LCD the strongest (standardized β 0.60, p < 0.001), followed by perceived behavioural control (standardized β 0.24, p < 0.001) and subjective norm (standardized β 0.14, p < 0.001; Supplemental Table S1, model 1). Adding carbohydrate knowledge and dietary guideline agreement in the model 1, both knowledge score and guideline agreement were negatively associated with intention to follow a LCD (standardized β − 0.09 and − 0.13, all p < 0.001), with no impact on the coefficients of TPB constructs (Supplemental Table S1, model 2). All health beliefs behind the three TPB constructs showed that behavioural beliefs, normative beliefs, and control beliefs significantly predicted the attitude, subjective norms, and perceived behavioural control respectively (Fig. 3).
Discussion
To our knowledge, this is the first study that has comprehensively explored the factors behind food choices not only in self-identified LCD followers but also in past and non-LCD followers in UK adults. The application of TPB model demonstrated the hypothesized associations between psychological factors and intention to follow a LCD, which was mostly driven by attitude, aligning with previous meta-analysis of TPB and healthy eating pattern showing that attitude had the strongest association with intention32.
Knowledge about carbohydrate foods in terms of nutrition and health, and perceived benefits of dietary guideline could also influence the intention to follow a LCD22, and we found that knowledge and guideline agreement had negative influences on intention to follow a LCD. Respondents who had high knowledge about carbohydrates, and their role in nurition and health, were more concerned about the unfavourable consequences of LCDs on micronutrient inadequacy. Foods recommended in LCDs also conflict with dietary guidelines recommendations25.
Compared to non-LCD followers, current followers consumed less starchy foods, fruits and vegetables, but more meat, fish, and cheese, similar to a previous study21. Current LCD followers consumed starchy foods as little as 0.9 time/day. Assuming that 1 time per day is equivalent to 1 average portion of starchy foods, this would be equivalent to a carbohydrate content of 40 g in 1 cup of cooked pasta or rice, 27 g in 2 slices of breads or in 1 cup of bran cereals, and 54 g in 2 medium size potatoes. This level of carbohydrate intake is to some extent in line with a very low-carbohydrate diet (< 50 g/day)1, 12. Although other carbohydrate-rich foods (e.g. cake, ice cream, biscuit, etc.) contribute to overall carbohydrate intake, LCD followers consumed these foods as little as 0.13 times/week (equivalent to never or less than once a month—the minimum frequency of intake in the DTM; this may be partly explained by conscious or unconscious under-reporting of these discretionary items). Cutting out starchy foods and fruits could result in micronutrient inadequacy23, especially if this is not guided appropriately35. Although supplementation could top up vitamins and minerals intake during LCD, only 10% of LCD followers reported use of multivitamins/minerals supplements.
Our findings also highlighted that there were differences in perceived experiences during LCD between current and past followers. The experience of current followers highlighted improvement in all experiences more often than worsening, often (but not always) unlike past followers. While some of these contrasting experiences may explain why some people do well and can maintain specific diet, it also provides confirmation that there is not one single best diet for all. Weight loss, health, and diabetes management were the most reported motivations to follow a LCD in our study, similar to previous studies8, 34. These motivations could be influenced by perceived benefits of LCDs for weight loss and prevention for chronic diseases. Diets restricting carbohydrate intake take a wide range of format, and can work for some people, as shown by the diverse and opposite perception of symptoms that improved or worsened during dieting. More importantly, either for weight loss or because of pre-existing health risk, over 80% of LCD followers reported that their doctor/HCP did not know that they were following a LCD, higher than previously reported in a study from the USA (50%)24 highlighting a potential concern regarding engagement with primary care and allied health professionals regarding diet and lifestyle. The internet was the most frequently reported source of information and inspiration regarding LCDs, which in part could be explained by the availability of successful weight loss stories online5, 6.
Our findings could help inform practice as we highlighted several challenges associated with following a LCD. The access to support from doctors or dietitians was low, and the internet was the most commonly cited source guiding or influencing LCD behaviour, indicating that there is limited reliable resources for those who want to follow a LCD. Provision of reliable resources online or increased access to healthcare support on how to follow a LCD, especially in terms of nutrient-dense food selection, would support knowledge and ability to follow a LCD while preventing the risk of inadequate vitamin and mineral intake23, 35, 36. Although our study found that individuals practicing medicine (doctors) were more likely to follow a LCD, this was not true for dietitians, food scientists, or other healthcare professionals. The motivations for following a LCD, in individuals practicing medicine (e.g. knowledge, income), is an interesting area to be explored further. Determinants for dietary behaviours or food choices have mostly been debated in Western countries, however, this is a debate also relevant to other regions (e.g. Asia) where different barriers and opportunities could arise depending on local food systems and culture. This is something that remains to be investigated.
There are limitations in this study. The aims of the study were exploratory rather than to determine prevalence. As the nature of the online survey, representativeness cannot be completely assured: the proportion of LCD followers could not be inferred as representing the prevalence of LCD use in the UK or elsewhere. The dietary assessment was limited to frequency of consumption, it was unable to generate the amount of carbohydrate intake. Therefore, we could not explore the number of LCD followers who were in line with the more conservative LCD definition (e.g. carbohydrate of less than 26% of energy intake per day)1, 12. The lack of a standard definition for LCDs may impact on the study findings. In practice, reducing carbohydrate intake may imply (or not) caloric restriction; to balance for a lower contribution of carbohydrate towards energy intake, either fat or protein may be increased. The perceptions (health beliefs, lived experience) of these very different variations of a LCD, from an energy, macronutrient and possibly micronutrient point of view would be expected to differ and deserves further attention. The TPB has been used to predict intention and future behaviour31, 32, for example, the intention to eat a healthful diet and the actual behaviour of eating a healthful diet further down in time. Due to the cross-sectional design of this study, we cannot reflect on actual behaviour change post survey.
Conclusions
The current study provides better understanding of the nutritional behaviour and motivations to follow a LCD, with losing weight and health listed as the primary reasons. It also provides an overview of the experience of dieters, highlighting both positive and negative experiences while following the diet. The findings could help design individually preferred weight management programmes, moving away from one-size fits all. Application of the TPB helps elucidate factors explaining the intention to follow a LCD among UK adults. Positive attitude (e.g. perception that a LCD is effective for weight management and reduced risk of chronic disease) is the most powerful determinant for intention to follow a LCD, while carbohydrate knowledge and agreeing with dietary guideline are negative determinants. It is of concern that a majority of LCD followers do not have explicit support from HCPs and that a minority takes multivitamins/minerals supplement despite the restrictive nature of the diet. As there is no specific best weight loss diet, LCDs may suit some people’s preference2, 3, 37, indicating a place for better professional guidance and support on weight loss diet, and improved knowledge about high nutrient-dense food selection to minimize the health risk generated from LCDs. Weight regain after a LCD as well as reasons why past followers stopped, or why non-followers chose not to follow the diet deserve further investigation.
Methods
Study design and population
A cross-sectional online survey was conducted between February to December 2019 in a sample of UK adults, aged 18 years and older. The survey included participants who self-identified either as LCD followers, or non-followers. Entering the survey was incentivized with a £50 Amazon voucher prize, drawn every 100 entries. Participants were recruited via social media i.e. Twitter, Facebook, Instagram, and web service for online survey recruitment (i.e. callforparticipants.com and prolific.co). Written informed consent was obtained from all the participants. The study was approved by the University of Glasgow Research Ethics Committee (project no. 200180040).
Sample size
The sample size was calculated using the equation for estimated proportion for an infinite population38. With 95% confidence level (alpha 0.05), 2.5% absolute precision (margin of error), and a design effect of one as suggested by Gorstein et al., a margin of error should not be more than 3 percentage points if an estimated prevalence is less than 20%39. We assumed an overall 10% prevalence of LCD followers in the UK, based on a media poll in the UK7 showing that 7% of men and 10% of women had tried this diet. Based on this calculation, the minimum sample required was 555 UK adults, which should provide 56 respondents as LCD followers. We aimed to recruit over this number to ensure a sufficient sample size, assuming 20% of responses would be incomplete. Therefore, a final number of at least 694 UK adults was targeted, expecting at least 70 LCD followers.
Questionnaire instrument
All data collected in this study were self-reported data. The questionnaire gathered socio-demographics data (i.e. age, sex, weight and height, education, income, ethnicity, smoking status, co-morbid diseases, supplement use). BMI was calculated by weight (kg) divided by the square of height (m). Other components included self-reported “LCD status” (current, past and non-follower), dietary intake, knowledge and perceived understanding of carbohydrates, and awareness of current national dietary guidelines. The questionnaire also included the psychological constructs determining behavioural intention to follow a LCD, with the application of the TPB model (Supplementary File).
Dietary assessment
Dietary intake was assessed using the Dietary Targets Monitor (DTM)40. The DTM is an easily administered, short food frequency list, which was designed to assess habitual intake of the foods in comparison to Dietary Targets for Scotland40. The commonly consumed foods listed in the DTM were fruits and vegetables, carbohydrate-rich foods (e.g. breads, cereals, pasta, potatoes), meat, chicken, fish, pastries and savoury snacks. The DTM can estimate the amount of food and nutrient intake for fruits and vegetables (g/day), fish (g/week), and fat and saturated fat (g/day) using calibrated formulas40. The remaining individual food items can be reported as frequency of consumption (times/day or times/week). Further details of the DTM are described in Lean et al.40.
Nutritional behaviour of low-carbohydrate diet followers
Nutritional behaviour of current and past LCD followers was collected as following: names of LCD followed, source of information about LCD, reasons to follow a LCD, timescale of following a LCD, meal portion size while following a LCD, frequency of eating LCD (e.g. every day, only weekday, only weekend, etc.), experience of benefits and adverse events during LCD, as well as source of support while following a LCD (e.g. healthcare professionals, including doctors and dietitians).
Perceived understanding and knowledge about carbohydrates
Perceived understanding about carbohydrate was assessed using the question “Do you understand what the term ‘carbohydrate’ means?” with four response answers: (1) yes, very good idea; (2) yes, vague idea; (3) no, not really, but I know what foods contain carbohydrate; and (4) no, not at all. Knowledge about carbohydrate-rich food was derived from 11 items designed around type and source of carbohydrate, food processing, and nutrition. Each item was scored 1 point for correct answer, − 1 for incorrect, and zero point if participants selected ‘do not know’. The score was summed, giving a range from − 11 to 11.
Dietary guideline awareness and agreement
To assess awareness of the current dietary guidelines, participants were asked whether they had heard of the UK Eatwell plate/guide (or MyPlate, USA) and whether they were following one of these guidelines. They were also asked whether they agreed with these guidelines, including agreement on each of the four statements in the UK Eatwell guide (i.e. carbohydrate foods, fruits and vegetables, oils, and foods high in fat, salt and sugar). To assess the level of agreement on UK Eatwell guide, each of four statements scored 1 point if respondents answered ‘agree’, − 1 for ‘disagree’, and no point for ‘not sure’. The score was summed, giving a range from − 4 to 4.
The theory of planned behaviour
The TBP model was applied to assess the low-carbohydrate dieting behaviour and the intention to follow a LCD. The model includes intention to follow a LCD, attitude towards following a LCD, subjective norm, and perceived behavioural control over low-carbohydrate dieting behaviour. In addition, there are beliefs underlying attitude, subjective norm, and perceived behavioural control41.
-
1.
Behavioural beliefs are the beliefs about the expected outcomes (e.g. good or bad) of the behaviour and then produce a favourable or unfavourable attitude towards the behaviour. Four behavioural beliefs were investigated as follow: LCD for weight management, risk of micronutrient inadequacy following a LCD, reduced risk of chronic diseases following a LCD, and the side-effects of LCD. There was also an outcome evaluation corresponding to each behavioural belief. Outcome evaluation indicates respondents’ expression either positive or negative evaluation of the behavioural belief. For example, a behavioural belief of ‘following a LCD can keep body weight in a healthy range’ corresponds to an outcome evaluation of ‘having a normal body weight is desirable or undesirable’.
-
2.
Normative beliefs are the beliefs about the expectation or influence of others (normative referent) on performing the behaviour and result in perceived social pressure or subjective norm. Five normative referents were assessed as follow: family, friends and colleagues, doctor, books, and the internet. There was also a motivation to comply corresponding to each normative belief. Motivation to comply indicates the importance of normative referent on doing a behaviour. For example, a normative belief of ‘family think that I should follow a LCD’ corresponds to a motivation to comply of ‘what family think I should do matters to me’.
-
3.
Control beliefs are the beliefs about the factors that could facilitate or inhibit the behaviour and result in perceived behavioural control. Three control beliefs were assessed as follow: joining mealtime with other people who have starchy foods in their diets, high price and lack of ready to eat LCD foods, and a lack of time to cook or prepare meals. There was also a power of control factor corresponding to each control beliefs. Power of control factor indicates the power of control belief to influence the behaviour. For example, a control belief of ‘people round me have starchy foods in their diets’ corresponds to a power of control factor of ‘joining mealtime with other people who have starchy foods makes it more difficult to follow a LCD’.
Belief statements were derived from review of the literature as well as online discussion forum and social media (Twitter, Facebook groups). The list of belief statements was then given to a small convenient sample to check and complete. The final TPB questionnaire consisted 29 question-items, assessing intention, attitude, subjective norm, perceived behavioural control, and the three types of beliefs above. The strength of intention, attitude, subjective norm, perceive behavioural control, and all beliefs were measured using 7-point bipolar rating scales, ranging from strongly disagree (1) to strongly agree (7). The statements about outcome evaluation, motivation to comply, and power of control factor were measured using the same responses but different scoring system, ranging from − 3 for strongly disagree to + 3 for strongly agree.
Before analysis, each behavioural belief was multiplied by its corresponding outcome evaluation, normative beliefs multiplied by motivation to comply, and control beliefs multiplied by power of control factor, as described in Francis et al.42. Then each belief in its category was summed to create a composite score, for example four behavioural beliefs were summed to create a behavioural belief composite score. Similar process was done for normative belief composite score and control belief composite score. Positive score of behavioural beliefs means that the respondent is in favour of the behaviour, while negative score means disagreeing with the behaviour. Similarly, positive (or negative) score of normative beliefs means that respondent feels social pressure to execute the behaviour (or not). Positive (or negative) score of control beliefs means that respondent feel (or does not feel) in control of doing the behaviour.
Questionnaire validation
The questionnaire was assessed for face and content validity among colleagues in Human Nutrition, University of Glasgow (n = 18), who were informed about the objectives of the survey. Feedback focused on readability, feasibility, clarity of wording and layout and style, and whether it was an objective tool to answer the questions. An average time spent on questionnaire was 22 min (SD 3). The final questionnaire version was created using the Online Survey System (www.onlinesurveys.ac.uk). The online version of the questionnaire was tested in a group of people outside nutrition field (n = 5) for readability and understanding before launching.
Statistical analysis
Descriptive statistics were used to describe sample characteristics, knowledge score, awareness of dietary guidelines, dietary intake and TPB constructs. Group differences between LCD followers and non-LCD followers were assessed with t-test or ANOVA for continuous data and Chi-square test for categorical data. Non-parametric statistics were used where appropriate.
Path analysis43 was used to test the hypothesized TPB model, using multiple linear regression analysis to determine psychological constructs of the TPB (independent variables: attitude, subjective norm, and perceived behavioural control) that influence participants’ intention (dependent variable) towards following a LCD (model 1, the independent variables were adjusted to each other). Then in the model 2, carbohydrate knowledge and guideline agreement were added in the model 1 (further adjustment), to determine their associations with intention to follow a LCD, and to investigate whether these variables affect the associations between TPB constructs and the intention.
Path analysis was also applied for analysis of the influence of intention (independent variable) on low-carbohydrate dieting behaviour (dependent variable). We defined behaviour as the frequency of consumption of starchy foods and used it as a dependent variable in a linear regression analysis. Perceived behavioural control variable was also added in the model predicting behaviour as shown in the TPB.
Ethical declaration
Written informed consent was obtained from all the participants prior to their inclusion in the study. The study was approved by the University of Glasgow Research Ethics Committee (project no. 200180040), and have been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki.
References
Churuangsuk, C., Lean, M. E. J. & Combet, E. Low and reduced carbohydrate diets: challenges and opportunities for type 2 diabetes management and prevention. Proc. Nutr. Soc. 1, 1–16. https://doi.org/10.1017/S0029665120000105 (2020).
Churuangsuk, C., Kherouf, M., Combet, E. & Lean, M. Low-carbohydrate diets for overweight and obesity: a systematic review of the systematic reviews. Obes. Rev. 19, 1700–1718. https://doi.org/10.1111/obr.12744 (2018).
van Zuuren, E. J., Fedorowicz, Z., Kuijpers, T. & Pijl, H. Effects of low-carbohydrate- compared with low-fat-diet interventions on metabolic control in people with type 2 diabetes: a systematic review including GRADE assessments. Am. J. Clin. Nutr. 108, 300–331. https://doi.org/10.1093/ajcn/nqy096 (2018).
Atkins, R. C. Dr. Atkins' Diet Revolution: The High Calorie Way to Stay Thin Forever., (David McKay, Inc, 1972).
Hawkins, L. K., Farrow, C. & Thomas, J. M. Do perceived norms of social media users’ eating habits and preferences predict our own food consumption and BMI?. Appetite 149, 104611. https://doi.org/10.1016/j.appet.2020.104611 (2020).
Lawler, M. 12 Celebrities Who Can’t Get Enough of the Ketogenic Diet, Everyday Health Group https://www.everydayhealth.com/ketogenic-diet/diet/celebrities-cant-get-enough-ketogenic-diet (2018).
BBC. Three million follow Atkins diet, https://news.bbc.co.uk/1/hi/health/3197627.stm (2003).
Jallinoja, P., Niva, M., Helakorpi, S. & Kahma, N. Food choices, perceptions of healthiness, and eating motives of self-identified followers of a low-carbohydrate diet. Food Nutr. Res. 58, 23552. https://doi.org/10.3402/fnr.v58.23552 (2014).
Finney Rutten, L. J., Lazarus Yaroch, A., Colon-Ramos, U. & Uriyoan, A. A. Awareness, use, and perceptions of low-carbohydrate diets. Prev. Chronic Dis. 5, A130 (2008).
Crowe, T. C. & Cameron-Smith, D. Low-carbohydrate diets in Australia: prevalence and public perceptions. Med. J. Aust. 182, 594–595 (2005).
International Food Information Council. 2018 Food & Health Survey. https://foodinsight.org/wp-content/uploads/2018/05/2018-FHS-Report-FINAL.pdf (2018).
Feinman, R. D. et al. Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutrition 31, 1–13. https://doi.org/10.1016/j.nut.2014.06.011 (2015).
Bueno, N. B., de Melo, I. S., de Oliveira, S. L. & da Rocha Ataide, T. Very-low-carbohydrate ketogenic diet vs low-fat diet for long-term weight loss: a meta-analysis of randomised controlled trials. Br. J. Nutr. 110, 1178–1187. https://doi.org/10.1017/S0007114513000548 (2013).
Hession, M., Rolland, C., Kulkarni, U., Wise, A. & Broom, J. Systematic review of randomized controlled trials of low-carbohydrate vs. low-fat/low-calorie diets in the management of obesity and its comorbidities. Obes. Rev. 10, 36–50. https://doi.org/10.1111/j.1467-789X.2008.00518.x (2009).
Mansoor, N., Vinknes, K. J., Veierod, M. B. & Retterstol, K. Effects of low-carbohydrate diets vs low-fat diets on body weight and cardiovascular risk factors: a meta-analysis of randomised controlled trials. Br. J. Nutr. 115, 466–479. https://doi.org/10.1017/S0007114515004699 (2016).
Nordmann, A. J. et al. Effects of low-carbohydrate vs low-fat diets on weight loss and cardiovascular risk factors: a meta-analysis of randomized controlled trials. Arch. Intern. Med. 166, 285–293. https://doi.org/10.1001/archinte.166.3.285 (2006).
Sackner-Bernstein, J., Kanter, D. & Kaul, S. Dietary intervention for overweight and obese adults: comparison of low-carbohydrate and low-fat diets: a meta-analysis. PLoS ONE 10, e0139817. https://doi.org/10.1371/journal.pone.0139817 (2015).
Hu, T. et al. Effects of low-carbohydrate diets versus low-fat diets on metabolic risk factors: a meta-analysis of randomized controlled clinical trials. Am. J. Epidemiol. 176(Suppl 7), S44-54. https://doi.org/10.1093/aje/kws264 (2012).
Johnston, B. C. et al. Comparison of weight loss among named diet programs in overweight and obese adults: a meta-analysis. JAMA 312, 923–933. https://doi.org/10.1001/jama.2014.10397 (2014).
Naude, C. E. et al. Low carbohydrate versus isoenergetic balanced diets for reducing weight and cardiovascular risk: a systematic review and meta-analysis. PLoS ONE 9, e100652. https://doi.org/10.1371/journal.pone.0100652 (2014).
Elidottir, A. S., Halldorsson, T. I., Gunnarsdottir, I. & Ramel, A. Dietary intake and cardiovascular risk factors in icelanders following voluntarily a low carbohydrate diet. PLoS ONE 11, e0156655. https://doi.org/10.1371/journal.pone.0156655 (2016).
Brug, J. Determinants of healthy eating: motivation, abilities and environmental opportunities. Fam. Pract. 25(Suppl 1), i50-55. https://doi.org/10.1093/fampra/cmn063 (2008).
Churuangsuk, C., Griffiths, D., Lean, M. E. J. & Combet, E. Impacts of carbohydrate-restricted diets on micronutrient intakes and status: a systematic review. Obes. Rev. 20, 1132–1147. https://doi.org/10.1111/obr.12857 (2019).
Feinman, R. D., Vernon, M. C. & Westman, E. C. Low carbohydrate diets in family practice: what can we learn from an internet-based support group. Nutr. J. 5, 26. https://doi.org/10.1186/1475-2891-5-26 (2006).
Churuangsuk, C., Lean, M. E. J. & Combet, E. Lower carbohydrate and higher fat intakes are associated with higher hemoglobin A1c: findings from the UK National Diet and Nutrition Survey 2008–2016. Eur. J. Nutr. 59, 2771-2782. https://doi.org/10.1007/s00394-019-02122-1 (2020).
Dunkley, A. J. et al. Diabetes prevention in the real world: effectiveness of pragmatic lifestyle interventions for the prevention of type 2 diabetes and of the impact of adherence to guideline recommendations: a systematic review and meta-analysis. Diabetes Care 37, 922–933. https://doi.org/10.2337/dc13-2195 (2014).
Eriksen, R. et al. Nutrient profiling and adherence to components of the UK national dietary guidelines association with metabolic risk factors for CVD and diabetes: airwave health monitoring study. Br. J. Nutr. 119, 695–705. https://doi.org/10.1017/S0007114518000016 (2018).
Johnson, N. F. et al. The online competition between pro- and anti-vaccination views. Nature 582, 230–233. https://doi.org/10.1038/s41586-020-2281-1 (2020).
Wadman, M. Antivaccine forces gaining online. Science 368, 699. https://doi.org/10.1126/science.368.6492.699 (2020).
Ajzen, I. The theory of planned behavior. Organ. Behav. Hum. Decis. Process. 50, 179–211. https://doi.org/10.1016/0749-5978(91)90020-t (1991).
Ajzen, I. The theory of planned behaviour: reactions and reflections. Psychol. Health 26, 1113–1127. https://doi.org/10.1080/08870446.2011.613995 (2011).
McDermott, M. S. et al. The theory of planned behaviour and dietary patterns: a systematic review and meta-analysis. Prev. Med. 81, 150–156. https://doi.org/10.1016/j.ypmed.2015.08.020 (2015).
McEachan, R. R. C., Conner, M., Taylor, N. J. & Lawton, R. J. Prospective prediction of health-related behaviours with the theory of planned behaviour: a meta-analysis. Health Psychol. Rev. 5, 97–144. https://doi.org/10.1080/17437199.2010.521684 (2011).
Clarke, C. & Best, T. Food choice motivations: profiling low-carbohydrate, high-fat dieters. Appetite 141, 104324. https://doi.org/10.1016/j.appet.2019.104324 (2019).
Zinn, C., Rush, A. & Johnson, R. Assessing the nutrient intake of a low-carbohydrate, high-fat (LCHF) diet: a hypothetical case study design. BMJ Open 8, e018846. https://doi.org/10.1136/bmjopen-2017-018846 (2018).
Manousou, S. et al. A Paleolithic-type diet results in iodine deficiency: a 2-year randomized trial in postmenopausal obese women. Eur. J. Clin. Nutr. 72, 124–129. https://doi.org/10.1038/ejcn.2017.134 (2018).
Unwin, D. & Unwin, J. Low carbohydrate diet to achieve weight loss and improve HbA1cin type 2 diabetes and pre-diabetes: experience from one general practice. Pract. Diabetes 31, 76–79. https://doi.org/10.1002/pdi.1835 (2014).
Daniel, W. W. & Cross, C. L. Biostatistics: a foundation for analysis in the health sciences, 10th edn, (Wiley, New York, 2013).
Gorstein, J., Sullivan, K., Parvanta, I. & Begin, F. Indicators and methods for cross-sectional surveys of vitamin and mineral status of populations. The Micronutrient Initiative (Ottawa) and the Centers for Disease Control and Prevention. (Atlanta, 2007).
Lean, M. E., Anderson, A. S., Morrison, C. & Currall, J. Evaluation of a dietary targets monitor. Eur. J. Clin. Nutr. 57, 667–673. https://doi.org/10.1038/sj.ejcn.1601596 (2003).
Downs, D. S. & Hausenblas, H. A. Elicitation studies and the theory of planned behavior: a systematic review of exercise beliefs. Psychol. Sport. Exerc. 6, 1–31. https://doi.org/10.1016/j.psychsport.2003.08.001 (2005).
Francis, J. J. et al. Constructing questionnaires based on the theory of planned behaviour: a manual for health services researchers (University of Newcastle, Newcastle, Centre for Health Services Research, 2004).
Hankins, M., French, D. & Horne, R. Statistical guidelines for studies of the theory of reasoned action and the theory of planned behaviour. Psychol. Health 15, 151–161. https://doi.org/10.1080/08870440008400297 (2000).
Acknowledgements
The authors would like to thank our colleagues in Human Nutrition, and in the New Lister Building who helped with the questionnaire development. The authors also thank all colleagues, peers and contacts who helped share the questionnaire online. This work was supported by PhD scholarship to CC from the Prince of Songkla University, Faculty of Medicine, Thailand.
Author information
Authors and Affiliations
Contributions
C.C. developed research question, prepared study materials and conduct the study, prepared the dataset and conducted analyses with inputs from M.E.J.L. and E.C. C.C. drafted the manuscript. All authors critically reviewed and revised the manuscript and have read and approved the final version.
Corresponding author
Ethics declarations
Competing interests
CC has received PhD scholarship from the Prince of Songkla University, Faculty of Medicine, Thailand. MEJL has received departmental research support from Diabetes UK, Cambridge Weight Plan and Novo Nordisk and consultancy fees and support for meeting attendance from Novo-Nordisk, Eli Lilly, Novartis, Counterweight Ltd and Eat Balanced. EC has received research funds from Filipo Berio.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Churuangsuk, C., Lean, M.E.J. & Combet, E. Carbohydrate knowledge, dietary guideline awareness, motivations and beliefs underlying low-carbohydrate dietary behaviours. Sci Rep 10, 14423 (2020). https://doi.org/10.1038/s41598-020-70905-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-70905-2
- Springer Nature Limited
This article is cited by
-
Low thiamine status in adults following low-carbohydrate / ketogenic diets: a cross-sectional comparative study of micronutrient intake and status
European Journal of Nutrition (2024)
-
Diets for weight management in adults with type 2 diabetes: an umbrella review of published meta-analyses and systematic review of trials of diets for diabetes remission
Diabetologia (2022)