Abstract
Several studies in patients with chronic kidney disease or normal renal function have shown that high levels of tissue non-specific alkaline phosphatase (ALP) are associated with an increased risk of all cause and cardiovascular (CV) mortality. Considering the independent prognostic role of renal function, we investigated the possible association between ALP levels and estimated glomerular filtration rate (e-GFR) in a large cohort of hypertensive subjects. We enrolled 2157 never-treated uncomplicated hypertensive patients with ALP levels within normal range. In the whole population, e-GFR was strongly related to ALP (r = −0.43, P < 0.0001) with similar magnitude in females and in males, resulting ALP the second independent predictor of renal function. In a multiple linear regression model, both on crude (P < 0.001) and adjusted (P = 0.01) analyses age significantly modified the effect of a fixed increase in ALP (20 UI/L) on renal function so that the reduction in e-GFR associated to a 20 UI/L increase in ALP was of lower magnitude in younger patients and progressively of higher extent from 20 years of age onwards. In conclusion, present data indicate a significant relationship between ALP levels and e-GFR in uncomplicated hypertensive patients that is modulated by age and that persisted after adjusting for several confounders.
Similar content being viewed by others
Introduction
Tissue non-specific alkaline phosphatase (ALP), routinely measured in clinical practice for the diagnosis and monitoring of bone and hepatobiliary diseases, is a widely expressed hydrolase enzyme in human tissues, particularly in the liver, bone and kidney. The main action of ALP is to catalyse the hydrolysis and therefore the inactivation of inorganic pyrophosphate (PPi), a potent endogenous inhibitor of calcification1
Several evidences suggest a possible role of ALP as emerging marker of cardiovascular (CV) risk. In particular, numerous studies in patients with chronic kidney disease (CKD) have shown that high levels of ALP are associated with an increased risk of CV and all-cause mortality2,3,4. In addition, high values of ALP are associated with increased risk of kidney disease progression in a heterogeneous population of patients with CKD stages 3-45. Moreover, ALP has been demonstrated to be an independent predictor of death and CV events in both the general population and patients with coronary artery disease (CAD) with preserved renal function6,7.
Several possible mechanisms have been hypothesized to explain the possible role of ALP in CV risk, including subclinical inflammation8,9, vascular calcification10,11, and endothelial dysfunction12,13. Recently, a strong association between serum ALP levels and reduced endothelium-dependent vasodilation, an independent predictor of CV events, was demonstrated in a large cohort of hypertensive patients12.
It is well known the strong link between renal function and CV outcome across all CKD stages. Indeed, several studies have shown that both advanced and subclinical renal damage are independent predictors of CV events and hospitalization in different settings of patients14,15. Of interest, experimental evidence suggests that ALP may directly affect renal function by increasing adenosine production and enhancing reno-vascular responses to norepinephrine in the kidney16. Moreover, subclinical inflammation and endothelial dysfunction, also promoted by ALP, may furtherly favour renal damage. However, whether serum ALP levels are associated with renal function in hypertensive patients without kidney and CV complications as well as the potential effect modification of aging on this relationship have not been settled. In the present study, this hypothesis was analyzed in a large cohort of never-treated hypertensive subjects participating in the CATAnzaro MEtabolic RIsk factors (CATAMERI) Study.
Results
Study population
Main demographic, clinical and biochemical data of the whole study group as well as separately by gender are reported in Table 1. There were no significant differences between males and females for ALP as well as for SBP, DBP, LDL-cholesterol and smoking. However, males were significantly older and displayed higher values of BMI, PP, fasting glucose, triglycerides, and hs-CRP than females. On the contrary, HDL-cholesterol values were significantly lower in males than in females. Furthermore, serum levels of phosphorus, calcium, and UA were significantly higher in males, so as e-GFR, that resulted normal in both groups (all eGFR values>60 ml/min/1.73 m2).
ALP and eGFR: univariate and multivariate analyses
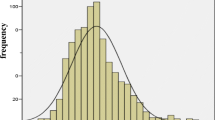
In the whole group, e-GFR was strongly inversely related to ALP (r = −0.43, P < 0.0001, Fig. 1), and the strength of this relationship was identical in both females (r = −0.50, P < 0.001) and males (r = −0.50, P < 0.001). Data adjustment for hs-CRP reduced the strength of the ALP - eGFR relationship (adjusted r = − 0.38, P < 0.001) suggesting that inflammation lies in the causal pathway between high ALP and low eGFR.
In a multiple linear regression model (dependent variable: e-GFR) including traditional and non-traditional risk factors, BMI (β = 0.35, P < 0.001), hs-CRP (β = −0.24, P < 0.001), male gender (β = −0.18, P < 0.001), age (β = −0.18, P < 0.001), UA (β = −0.15, P < 0.001), phosphate (β = −0.12, P < 0.001), LDL cholesterol (β = 0.07, P = 0.03), systolic BP (β = −0.04, P = 0.015) and triglycerides (β = 0.05, P = 0.005) had an independent relationship with e-GFR whereas smoking (β = 0.02, P = 0.16), and total cholesterol (β = −0.03, P = 0.36) did not (Table 2). All these variables explained 38% of the total variance in e-GFR (R2 = 0.38). The inclusion of ALP into this model provided a 6% increase in the explained variance in e-GFR (from 38% to 44%) and ALP (β = −0.26, P < 0.001) resulted to be the second factor, in rank order after BMI, explaining the variability in e-GFR (β = −0.26, P < 0.001).
Effect modification by age on the relationship between ALP and e-GFR: univariate and multivariate analyses
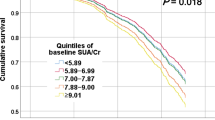
On univariate analysis (P < 0.001) as well as in a multiple linear regression model (P = 0.01), including the same set of covariates listed in Table 2, age significantly modified the effect of a fixed increase in ALP (20 UI/L) on e-GFR, so that such an increase in ALP triggered a decrease in e-GFR which was closely dependent on age (Fig. 2). The analysis of the “age-ALP interaction” showed that the reduction in e-GFR associated to a 20 UI/L increase in ALP was of lower magnitude in younger patients and progressively of higher extent from 20 years of age onwards. To put this in perspective, the estimated reductions in eGFR, adjusted for risk factors listed in Table 2, associated to a 20 UI/L increase in ALP was 1.7 ml/min/1.73 m2 when patients were 20 years old and 3.1 ml/min/1.73 m2 when patients were 70 years old (Fig. 2).
Effect modification by age on the relationship between alkaline phosphatase (ALP) and estimated-glomerular filtration rate (e-GFR). Data are expressed as estimated decrease (and 95% CI) in e-GFR associated to 20 UI/L increase in ALP at predefined values of age Equations of both crude and adjusted effect modification models: Crude effect modification model: e-GFR = 111.66 + 0.224*ALP_20 (20 units step)+0.041*Age (continuous variable)−0.075*interaction; where “interaction” is the product between “ALP_20” and “Age” as preliminary calculated. Adjusted effect modification model: eGFR= 115.68-1.070*ALP_20 - 0.032*Age - 0.029*interaction - 5.782*Gender + 1.111*Smoking +0.561*BMI - 0.025*systolic blood pressure -0.018*Total cholesterol + 0.032*LDL + 0.012*triglycerides - 1.229*uric acid -1.995*phosphate - 1.30*C reactive protein (see Methods- Statistical Analysis for more details).
Discussion
The results of this study, conducted in a well characterized cohort of non-diabetic, newly-diagnosed, never-treated hypertensive patients without CKD or CV complications, showed an association between serum ALP levels and renal function. Indeed, an inverse correlation between ALP and e-GFR values has been demonstrated both in the whole population and in sub-groups stratified by gender. Moreover, ALP was a strong correlate of e-GFR even after adjusting for traditional and non-traditional risk factors for renal impairment.
Notably, after adjusting for several confounders, age significantly modified the effect of a fixed increase in ALP on e-GFR with a lower magnitude in younger patients, which progressively raise from 20 years of age onwards, showing an “age-ALP interaction”. This is clinically relevant because epidemiological studies have shown that even a modest impairment of renal function may be associated with CV morbidity and mortality14,15. For instance, in the Hoorn study a loss of 5 ml/min/m2 in e-GFR was associated with a 22% increase in the risk of CV death17. Taken together, these results may be helpful to improve the stratification of global CV risk in hypertensive patients.
Several pathophysiological mechanisms including subclinical inflammation, vascular calcification, and endothelial dysfunction may explain these findings. ALP is closely associated with CRP, a commonly used inflammatory index, and there is evidence that CRP attenuates the association between ALP and CV outcome in multivariable regression models8,18,19. According with this, data adjustment for CRP reduced the strength of the ALP - eGFR relationship, also in our population, suggesting an involvement in the causal pathway between high ALP and low eGFR. Thus, it is possible that low-grade inflammation, characterizing chronic clinical conditions such as essential hypertension, may play a role in the association between ALP and renal damage. In addition, vascular calcification is now recognized as an active, cell-mediated process linked to an imbalance between promoters and inhibitors of mineralization1. ALP is able to affect the Pi:PPi ratio, which plays an undisputed role in promoting vascular calcification. According with this, ALP activity has been associated with medial vascular calcification in experimental models10,11.
Moreover, the association between ALP and renal damage may be, at least in part, explained by endothelial dysfunction, a strong and independent predictor of CV events in different clinical conditions, including essential hypertension20. Endothelial dysfunction, characterised by a reduced nitric oxide (NO) bioavailability, may be promoted by both inflammation and vascular calcification, thus favouring renal damage. In the kidney, NO exerts multiple roles including regulation of renal haemodynamic, maintenance of medullary perfusion, mediation of pressure–natriuresis, blunting of tubule-glomerular feedback, inhibition of tubular sodium reabsorption, and modulation of renal sympathetic neural activity with the net effect of promoting natriuresis and diuresis21,22. An association between acetylcholine (ACh)-stimulated vasodilation and renal function decline after adjustment for traditional cardiovascular risk factors has been previously reported in a cohort of never-treated uncomplicated hypertensive patients thus pointing to an important pathophysiological mechanism linking vascular dysfunction and mild renal impairment23. In addition, it has been shown that endothelial vasomotor dysfunction in the brachial artery is independently associated with progression from normal to early stage of renal dysfunction within twelve months of follow-up in patients with CAD. Thus, endothelial dysfunction evaluated in the brachial artery reflects a reduction in NO activity also in the renal vasculature with a consequent decline in renal function24 and ALP may be an active player in this association.
Mechanisms linking ALP to endothelial dysfunction may include inhibition of tyrosine kinase activity into endothelial cells with consequent impairment of endothelial NO synthase function, promotion of high production of reactive oxygen species (ROS), and apoptosis due to increased degradation of pyrophosphate promoting atherosclerotic lesions in vascular wall12,25,26,27.
Notably, we found that age acts as modifier of the relationship between ALP and e-GFR. As matter of the fact a 20 UI/L increase in ALP was associated with 1.7 ml/min/1.73 m2 reduction of e-GFR when patients were 20 years old and 3.1 ml/min/1.73 m2 when patients were 70 years old. It is known that ageing is associated with a proinflammatory status that is characterized by high levels of pro-inflammatory markers, a condition named “inflammageing”, that represents a potential risk factor for CV and renal diseases28,29. In hypertensive patients, fibrosis, perivascular inflammation with increased ROS production, and arterial calcification may be favoured not only by ageing but also by ALP activity, thus promoting vascular damage in both the micro- and macro-circulation in different organs and tissues, including kidney30,31.
Finally, recent evidence supports the notion that ALP is capable to modulate renal function and haemodynamic parameters. ALP has been involved in the regulation of renovascular and blood pressure responses to norepinephrine by modulating adenosine production in the kidney16. Endogenous adenosine, through the activation of A1-receptors highly expressed in the pre-glomerular microcirculation, is able to modulate the renovascular responses to renal sympathetic nerve stimulation as well as to exogenous norepinephrine. In the renal vasculature, in fact, adenosine and norepinephrine synergistically activate phospholipase C, contributing to renal vasoconstriction induced by sympathetic stimulation32,33. On the other hand, ALP is able to catalyse the conversion from ATP to adenosine in various organs including the kidney as evidenced by studies with isolated, perfused rat kidneys showing that the use of ALP specific inhibitors can attenuate the renovascular response to both exogenous and endogenous norepinephrine16.
The study strengths include the large number of patients enrolled with a complete clinical and laboratory assessment. Moreover, we included only never-treated patients without liver, bone, or renal disease, diabetes or excessive alcohol intake thus excluding potential confounding conditions. In addition, measurements of ALP and other biomarkers were made in a single laboratory using fresh collected blood samples. However, there are some limitations that should be considered. First, the cross-sectional design of the study does not allow to conclude a causal relationship between ALP and renal function and to define which pathophysiological mechanism plays a main role in this association. Furthermore we can not exclude that e-GFR could act also as determinant of ALP, so as evident in the advanced stages of CKD. In addition, even if our study population shows a relatively normal renal function, another important limitation is that we did not measure fibroblast growth factor (FGF)−23 and parathyroid hormone levels. These represent two well-known biomarkers of CKD and bone metabolism, thus they could affect ALP increase.
Further prospective and interventional studies are needed to confirm the observed relationship. Additionally, the present results were obtained in hypertensive patients and further studies in different patients’ settings are necessary to validate our observations. Finally, data on isoforms of ALP and measurements of mineral balance regulating factors such as vitamin D and parathyroid hormone were not available.
In conclusion, the present data indicate, in a large cohort of never-treated hypertensive patients with relatively normal renal function, a significant relationship between ALP levels and e-GFR that is modulated by age and that persisted after adjusting for several confounders. Thus, a potential involvement of ALP in the development of renal damage may be envisioned. However, further studies are needed to confirm our findings in the general population, to determine the pathophysiological mechanism, and to appraise the cause-effect relationship.
Methods
Study population
In this cross-sectional study, the enrolled group includes 2157 uncomplicated hypertensive outpatients (1057 males and 1100 females; mean age, 53.1 ± 13.5 years) participating in the Catanzaro Metabolic Risk Factors Study (CATAMERIS)34,35. All patients were Caucasian and underwent physical examination and review of their medical history. Causes of secondary hypertension were excluded by appropriate clinical and biochemical tests according to a standard diagnostic protocol. Other exclusion criteria were as follows: history or clinical evidence of CV complications, diabetes mellitus, history of any malignant disease or liver failure, calcium-phosphorus metabolism disorders, alcohol or drug abuse, and use of drugs interfering with ALP concentrations. All subjects showed a normal renal function and none of them had ever been treated with antihypertensive drugs. They underwent anthropometrical evaluation with measurement of weight, height, and body mass index (BMI). The local Ethical Committee (Comitato Etico Azienda Ospedaliera “Mater Domini”) approved the protocol and informed written consent was obtained from all participants. All the investigations were performed in accordance with the principles of the Declaration of Helsinki.
Blood pressure measurements
Measurements of clinic blood pressure (BP) were obtained in the left arm of the supine patients, after 5 min of quiet rest, with a validated sphygmomanometer. A minimum of three BP readings were taken on three separate occasions at least 2 weeks apart. Systolic and diastolic BP was recorded at the first appearance (phase I) and the disappearance (phase V) of Korotkoff sounds. Baseline BP values were the average of the last two of the three consecutive measurements obtained at intervals of 3 minutes. Patients with a clinic systolic BP (SBP) > 140 mmHg and/or diastolic BP (DBP) > 90 mmHg were defined as hypertensive36. Clinical pulse pressure (PP) was measured as the difference between SBP and DBP.
Laboratory determinations
All laboratory measurements were carried out after at least 12 hours fasting. Serum ALP (normal range, 40–129 IU/L) and calcium (normal range, 8.5–10.3 mg/dL) levels were measured with standard assays implemented on the COBAS C501 Roche auto-analyzer. The quantitative concentration of inorganic phosphate (normal range, 2.3–4.5 mg/dL) was measured by spectrophotometric determination based on the formation of ammonium molybdophosphate with subsequent reduction to molybdenum blue, using the diagnostic assay COBAS INTEGRA Phosphate 2 (Roche diagnostics). Plasma glucose was measured by the glucose oxidase method (Beckman Glucose Analyzer II; Beckman Instruments, Milan, Italy). Triglyceride, total, low- (LDL) and high-density lipoprotein (HDL) cholesterol concentrations were measured by enzymatic methods (Roche Diagnostics GmbH, Mannheim, Germany). High-sensitivity C-reactive protein (hs-CRP) was measured by a turbidimetric immunoassay (Behring).
Markers of renal function
Serum creatinine and uric acid (UA) were measured by an automated technique based on the measurement of Jaffe chromogen and by the URICASE/POD method (Boehringer Mannheim, Mannheim Germany) implemented in an auto-analyzer. Values of e-GFR were calculated by the CKD-Epidemiology Collaboration proposed equation that is more accurate in subjects with e-GFR > 60 ml/min/1.73 m2,37.
Statistical analysis
Normally distributed variables were expressed as mean ± SD and non-normally distributed variables as median and interquartile range. Categorical data were summarised as absolute numbers and percentage. Comparisons between two groups were performed by unpaired Student’s t-test, Mann Whitney U test, or Chi Square Test, as appropriate. The association between two continuous variables considered simultaneously was investigated by Pearson product moment correlation coefficient (r) and P values. The relationship between the key risk factor (ALP) and e-GFR was investigated by univariate (crude) analysis as well as by a multiple linear regression model including age, male gender, smoking (0=no; 1=yes), BMI (kg/m2), SBP (mmHg), total cholesterol (mg/dL), LDL-cholesterol (mg/dL), triglycerides (mg/dL), UA (mg/dL), phosphate (mg/dL), and hs-CRP (mg/L). To assess at what extent the inclusion of ALP into a multiple linear model (including standard risk factors – Model 1) increases the proportion of explained variance of eGFR (dependent variable), two multiple linear models were constructed: Model 1, not including ALP and Model 2, including ALP. The explained variance in the dependent variable (e-GFR) provided by tested covariates (before and after the inclusion of ALP) was assessed by the squared of the coefficient of determination (R2). In multiple linear regression models data were expressed as standardised regression coefficient (beta) and P value. The effect modification38 by age on the ALP/e-GFR relationship was investigated by the standard approach, i.e. by simultaneously introducing ALP, age and their interaction (multiplicative) term (age x ALP) into the same linear regression model also adjusting for a series of potential confounders. The estimated decrease (and 95% CI) in e-GFR associated to a fixed increase (20 UI/L) in ALP at predefined values of age was investigated by the linear combination method. All analyses were performed by two standard statistical packages (SPSS for Windows Version 22, IBM, USA; STATA/IC 13.0 StataCorp P, TX, USA).
Data availability
Data are available upon reasonable request from corresponding author.
References
Schoppet, M. & Shanahan, C. M. Role for alkaline phosphatase as an inducer of vascular calcification in renal failure? Kidney International 73, 989–991 (2008).
Regidor, D. L. et al. Serum alkaline phosphatase predicts mortality among maintenance hemodialysis patients. J. Am. Soc. Nephrol. 19, 2193–2203 (2008).
Drechsler, C. et al. Bone alkaline phosphatase and mortality in dialysis patients. Clin. J. Am. Soc. Nephrol. 6, 1752–1759 (2011).
Beddhu, S., Ma, X., Baird, B., Cheung, A. K. & Greene, T. Serum alkaline phosphatase and mortality in African Americans with chronic kidney disease. Clin. J. Am. Soc. Nephrol. 4, 1805–1810 (2009).
Taliercio, J. J. et al. Prognostic importance of serum alkaline phosphatase in CKD stages 3-4 in a clinical population. Am. J. Kidney Dis. 62, 703–710 (2013).
Park, J. B. et al. Serum alkaline phosphatase is a predictor of mortality, myocardial infarction, or stent thrombosis after implantation of coronary drug-eluting stent. Eur. Heart J. 34, 920–931 (2013).
Li, J. W., Xu, C., Fan, Y., Wang, Y. & Xiao, Y. Bin. Can serum levels of alkaline phosphatase and phosphate predict cardiovascular diseases and total mortality in individuals with preserved renal function? A systemic review and meta-analysis. PLoS One 9 (2014).
Kunutsor, S. K. et al. Serum alkaline phosphatase and risk of incident cardiovascular disease: Interrelationship with high sensitivity C-reactive protein. PLoS One 10 (2015).
Wannamethee, S. G., Sattar, N., Papcosta, O., Lennon, L. & Whincup, P. H. Alkaline phosphatase, serum phosphate, and incident cardiovascular disease and total mortality in older men. Arterioscler. Thromb. Vasc. Biol. 33, 1070–1076 (2013).
Sheen, C. R. et al. Pathophysiological role of vascular smooth muscle alkaline phosphatase in medial artery calcification. J. Bone Miner. Res. 30, 824–836 (2015).
Savinov, A. Y. et al. Transgenic overexpression of tissue-nonspecific alkaline phosphatase (TNAP) in vascular endothelium results in generalized arterial calcification. J. Am. Heart Assoc. 4 (2015).
Perticone, F. et al. Serum alkaline phosphatase negatively affects endothelium-dependent vasodilation in naïve hypertensive patients. Hypertension 66, 874–880 (2015).
Schutte, R. et al. Alkaline phosphatase and arterial structure and function in hypertensive African men: The SABPA study. Int. J. Cardiol. 167, 1995–2001 (2013).
Go, A. S., Chertow, G. M., Fan, D., McCulloch, C. E. & Hsu, C. Y. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N. Engl. J. Med. 351 (2004).
Schillaci, G., Reboldi, G. & Verdecchia, P. High-normal serum creatinine concentration is a predictor of cardiovascular risk in essential hypertension. Arch. Intern. Med. 161, 886–891 (2001).
Jackson, E. K., Zhang, Y. & Cheng, D. Alkaline phosphatase inhibitors attenuate renovascular responses to norepinephrine. Hypertension 69, 484–493 (2017).
Stam, F. et al. Endothelial dysfunction contributes to renal function-associated cardiovascular mortality in a population with mild renal insufficiency: The Hoorn study. J. Am. Soc. Nephrol. 17, 537–545 (2006).
Webber, M., Krishnan, A., Thomas, N. G. & Cheung, B. M. Y. Association between serum alkaline phosphatase and C-reactive protein in the United States National Health and Nutrition Examination Survey 2005-2006. Clin. Chem. Lab. Med. 48, 167–173 (2010).
Cheung, B. M. Y. et al. Association between plasma alkaline phosphatase and C-reactive protein in Hong Kong Chinese. Clin. Chem. Lab. Med. 46, 523–527 (2008).
Perticone, F. et al. Prognostic significance of endothelial dysfunction in hypertensive patients. Circulation 104, 191–196 (2001).
Satoh, M. Endothelial dysfunction as an underlying pathophysiological condition of chronic kidney disease. Clinical and Experimental Nephrology 16, 518–521 (2012).
Mount, P. F. & Power, D. A. Nitric oxide in the kidney: Functions and regulation of synthesis. Acta Physiologica 187, 433–446 (2006).
Perticone, F. et al. Endothelial dysfunction and subsequent decline in glomerular filtration rate in hypertensive patients. Circulation 122, 379–384 (2010).
Nakamura, T. et al. Endothelial vasomotor dysfunction in the brachial artery predicts the short-term development of early stage renal dysfunction in patients with coronary artery disease. Int. J. Cardiol. 148, 183–188 (2011).
Schultz-Hector, S., Balz, K., Bohm, M., Ikehara, Y. & Rieke, L. Cellular localization of endothelial alkaline phosphatase reaction product and enzyme protein in the myocardium. J. Histochem. Cytochem. 41, 1813–1821 (1993).
Boo, Y. C. & Jo, H. Flow-dependent regulation of endothelial nitric oxide synthase: Role of protein kinases. American Journal of Physiology - Cell Physiology 285 (2003).
Romanelli, F. et al. Overexpression of tissue-nonspecific alkaline phosphatase (TNAP) in endothelial cells accelerates coronary artery disease in a mouse model of familial hypercholesterolemia. PLoS One 12 (2017).
Ferrucci, L. & Fabbri, E. Inflammageing: chronic inflammation in ageing, cardiovascular disease, and frailty. Nature Reviews Cardiology 15, 505–522 (2018).
Fabbri, E. et al. Aging and the burden of multimorbidity: Associations with inflammatory and anabolic hormonal biomarkers. Journals Gerontol. - Ser. A Biol. Sci. Med. Sci. 70, 63–70 (2015).
Duca, L. et al. Matrix ageing and vascular impacts: Focus on elastin fragmentation. Cardiovascular Research 110, 298–308 (2016).
Guzik, T. J. & Touyz, R. M. Oxidative stress, inflammation, and vascular aging in hypertension. Hypertension 70, 660–667 (2017).
Jackson, E. K., Cheng, D., Tofovic, S. P. & Mi, Z. Endogenous adenosine contributes to renal sympathetic neurotransmission via postjunctional A 1 receptor-mediated coincident signaling. Am. J. Physiol. - Ren. Physiol. 302 (2012)
Jackson, E. K. et al. Role of A 1 receptors in renal sympathetic neurotransmission in the mouse kidney. Am. J. Physiol. - Ren. Physiol. 303 (2012).
Andreozzi, F. et al. Metabolic and cardiovascular risk factors in subjects with impaired fasting glucose: The 100 versus 110 mg/dL threshold. Diabetes. Metab. Res. Rev. 23, 547–550 (2007).
Marini, M. A. et al. Metabolically healthy but obese women have an intermediate cardiovascular risk profile between healthy nonobese women and obese insulin-resistant women. Diabetes Care 30, 2145–2147 (2007).
Mancia, G. et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur. Heart J. 34, 2159–2219 (2013).
Levey, A. S. et al. A new equation to estimate glomerular filtration rate. Ann. Intern. Med. 150, 604–612 (2009).
Rothman, K. J. Epidemiology. An introduction. Oxford University Press Madison (2002).
Author information
Authors and Affiliations
Contributions
Each author is expected to have made substantial contributions: V.C., G.T., A.S.: conception and design of the work; G.T., G.N.P., V.C., A.S., F.A., T.V.F., R.M.: acquisition, analysis, and interpretation of data; A.S., S.M., F.P., G.S., M.P.: have drafted the work and substantively revised it; All authors have approved the submitted version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sciacqua, A., Tripepi, G., Perticone, M. et al. Alkaline phosphatase affects renal function in never-treated hypertensive patients: effect modification by age. Sci Rep 10, 9847 (2020). https://doi.org/10.1038/s41598-020-66911-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-66911-z
- Springer Nature Limited
This article is cited by
-
Evaluation of the Protective Effects of Lugol’s Solution in Rats Poisoned with Aluminum Phosphide (Rice Tablets)
Cardiovascular Toxicology (2024)
-
Inflammatory atherosclerotic plaque identification by SPECT/CT imaging of LFA-1 using [111In] In-DANBIRT in a novel dyslipidemic rat model
Annals of Nuclear Medicine (2023)