Abstract
Asian population is a low-risk group for basal cell carcinoma (BCC) and there is little data available in this setting. Sun-exposed BCC (SEBCC) may possess a different pathogenic mechanism from non-sun-exposed BCC (NSEBCC). To compare the histopathological profiles and outcomes between SEBCC and NSEBCC, and to assess the risk factors for tumor recurrences. Retrospective cohort study on 372 patients with pathologically diagnosed BCC from January 1, 1990 to August 31, 2017. Data were derived from a single medical center in Taiwan. SEBCC presented with higher Clark level and more high-risk factors for recurrence than NSEBCC. Nodular, micronodular, infiltrating/mixed infiltrating, basosquamous, and adenoid types were predominant in SEBCC, as superficial type in NSEBCC. Risk factors for recurrence included infiltrating/mixed-infiltrating subtypes and synchronous basosquamous cell carcinoma. No recurrence events were observed in NSEBCC. Our study showed an acceptable recurrence rate (4.2%) of the whole population after excision even under a smaller surgical margin width than suggested by current guidelines. SEBCC had a higher recurrence rate with a significantly different tumor characteristic from NSEBCC and a greater tumor depth than NSEBCC. A wider surgical margin in SEBCC than NSEBCC is suggested.
Similar content being viewed by others
Introduction
Basal cell carcinoma (BCC) is the most common skin cancer and has an increasing incident worldwide1. Although the incidence is relatively low (2-4%) in Asian populations compared to Caucasian ones, studies have suggested a disproportionately high morbidity and mortality associated with the diagnosis of BCC in people with skin of color2,3,4. There is little data available about the characteristics and outcomes of BCC in Asian people. In Taiwan, non-melanoma skin cancer (NMSC) has often been ranked among the top ten most common types of cancer5.
Ultraviolet (UV) radiation has been viewed as one of the most important factors of BCC development6,7,8, as various epidemiological studies found the most common anatomical site of BCC to be head and neck. On the other hand, the pathogenesis of BCC on non-sun-exposed body area remains unclear. Studies have hypothesized a follicular stem cell or hair bulge origin of BCC9,10. Other factors including radiation, intermittent UV light exposure, chemical carcinogens, and infection with human papillomaviruses have also been reported11,12,13,14. To this date, most studies regarding the histopathologic features and outcomes of BCC were grouped by anatomical site rather than by areas that are prone to sun-exposure. Considering the potential differences in pathogenesis between sun-exposed BCC (SEBCC) and non-sun-exposed BCC (NSEBCC), this study aims to compare the histopathologic profiles and outcomes between SEBCC and NSEBCC and to investigate the risk factors for tumor recurrence.
Results
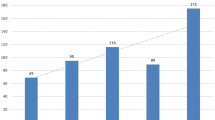
Of all 372 patients, 338 (90.9%) had SEBCC while the other 34 (9.1%) had NSEBCC. The mean age (±standard deviation) of index lesion was 71.8 (±13.7) years and 70.5 (±12.1) years in the SEBCC group and the NSEBCC group, respectively. No significant differences were found regarding the length of follow-up in the two groups (4.93 vs 4.51 years). Patients in the NSEBCC group had a significantly higher association with chronic kidney disease (CKD) (17.6% vs 7.1%, p < 0.001) and rheumatoid arthritis (RA) (5.9% vs 0%, p = 0.031) than with those in the SEBCC group. Details of the characteristics and comorbidities of the population are described in Table 1.
From the pathology reports, we identified 403 primary BCC lesions among 372 patients (Table 2). The most commonly diagnosed sites were on the head and neck (88.1%), with the most common subsites being nose or surroundings of the nose (29.5%), followed by cheeks and zygomatic area (13.9%), then eyebrows or area surrounding the eye (12.4%). Of the remaining, 6.0% of the lesions were from the trunk, 4.5% from extremities, and 1.5% from the other sites.
Risk factors for multiple BCC
22 (5.9%) patients were recorded with multiple BCCs, including 18 from the SEBCC group and 4 from the NSEBCC group. The associations between whether the lesions being sun-exposed or not, patient demographics, comorbidities, and the development of multiple BCCs using single and multivariate logistic regression analyses are shown in Table 3. Patients with dementia had a significantly higher association with the development of multiple BCCs (aOR=5.84, CI = 1.34-25.58, p = 0.019). Although patients with NSEBCC tended to have a higher association with developing multiple lesions than those with SEBCC, no significant differences were found. No significant associations regarding age, sex, diabetes mellitus, hypertension, chronic kidney disease, gout, and Arsenism were found to affect the development of multiple BCCs.
Histopathological profiles of BCC lesions
The histopathologic characteristics of all 403 BCC lesions are shown in Table 4, with 363 (90.1%) lesions being SEBCC and 40 (9.9%) being NSEBCC. NSEBCC had a significantly larger mean dimension measured than that of SEBCC (1.96 vs. 1.10 cm, p = 0.002). SEBCC had a greater depth measured (3.34 vs 3.19 mm), and had a significantly greater Clark level comparing to NSEBCC (p < 0.001). SEBCC had a significantly higher number of high-risk factors for recurrence than did NSEBCC (1.63 vs. 1.04, p < 0.001). Although NSEBCC had a significantly wider surgical margin than that of SEBCC, no significant difference was found regarding the margin free rates.
As for histopathologic types, nodular type was the most common type in both groups. Significant differences in the distribution of each subtypes were found between these two groups, with nodular, micronodular, infiltrating or mixed infiltrating, basosquamous, adenoid types being more predominant in SEBCC, while superficial types were more predominant in NSEBCC.
Risk factors for recurrent BCC
17 lesions had recurrence during our study period with a total recurrence rate of 4.2% of all patients. All of the recurrent lesions were SEBCC. No case involving distant metastasis was recorded. The associations between patient demographics, comorbidities, synchronous basosquamous cell carcinoma, and recurrence of BCC using Cox proportional hazards model are shown in Table 5. Patients with infiltrating or mixed-infiltrating subtype (aHR = 6.17, CI = 1.07-35.64, p = 0.042) and synchronous basosquamous cell carcinoma (aHR = 16.84, CI = 1.31-216.92, p = 0.030) had a significantly higher association with developing recurrent lesions of BCC. Age, sex, diabetes mellitus, hypertension, and end-stage renal disease had no significant association with developing recurrence after adjustment of covariates in the model. Survival curves regarding recurrence rate of BCC associated with synchronous basosquamous cell carcinoma and infiltrating or mixed-infiltrating type BCC are shown in Fig. 1.
Discussion
In this study, we analyzed the histopathological profiles and outcomes of BCC between sun-exposed and non-sun-exposed areas.
Our study showed that SEBCC had a greater depth and presented with more high-risk features of recurrence than did NSEBCC. The tendency of recurrence in SEBCC may be contributed to a predominant ratio in nodular, morpheaform, basosquamous, micronodular, and infiltrating or mixed infiltrating subtypes. Previous studies reported that anatomic location may favor the development of particular BCC subtypes15,16,17,18,19, and certain pathological subtypes were prone to having recurrences20,21,22.
In this study, the risk factors associated with tumor recurrence were synchronous basosquamous cell carcinoma and infiltrating or mixed-infiltrating subtype. Basosquamous cell carcinoma is an uncommon subtype that behaves with a high tendency of local recurrence or metastasis. Changing to basosquamous carcinoma in an initially ordinary BCC has also been reported23. Armstrong et al. found that incomplete and close excision margins, infiltrating and micronodular subtypes, and previous excision were strong risk factors for facial BCC recurrence24. In our study, no significant differences in the margin free rate between the two groups were found. Current guidelines suggested an excision with 4-mm clinical margins should be made in well-circumscribed, low-risk BCC lesions less than 2 cm in diameter20,25. Our study showed a relatively low recurrence rate after excision comparing to previous study26, even under a smaller surgical margins in average (2.01 mm in SEBCC, 3.77 mm in NSEBCC).
From our results, we demonstrated that NSEBCC had a significantly larger mean dimension measured and a wider surgical margin than that of SEBCC. This suggests that surgeons always cut a wider surgical margin in NSEBCC due to the large size of the tumors. As nodular, micronodular, infiltrating or mixed infiltrating, basosquamous, and adenoid types were more predominant in SEBCC, superficial types were more predominant in NSEBCC. A total recurrence rate of 4.2% was noted in all patients with no recurrence in patients with NSEBCC. Further subgroup analysis was conducted regarding recurrence rate of the SEBCC and NSEBCC group. SEBCC had a higher recurrence rate than NSEBCC in subgroup which the surgical margin of tumor was less than or equal with 3 mm. No recurrence event was found in subgroup which the surgical margin of tumor was larger than 3 mm. In SEBCC, no significant difference of recurrence rate was found between groups that had surgical margin less than or above 3 mm. This supports our hypothesis that the tendency of recurrence in SEBCC might have to do with its histopathological nature or pathogenic mechanism, rather than its differences in surgical margin width in this study. Altogether, we conclude that unlike SEBCC, NSEBCC might not need a wider surgical margin as current guideline suggested and that a wider safe margin for SEBCC than NSEBCC is indicated.
The existence of NSEBCC may imply a different pathogenesis other than UV light exposure. Our study showed that patients with NSEBCC had a significantly higher association with RA and CKD. Tseng et al. found an increased association with NMSC in RA patients, especially in those using disease-modifying anti-rheumatic drugs27. Wang et al. reported that patients with CKD are at a higher risk of developing NMSC28, and previous studies implied that accumulation of uremic toxins, oxidative stress, and systemic inflammation in CKD patients may act as important roles in developing malignancy29,30. In our study, the different distribution observed in comorbidities between the two groups may suggest a relatively systemic pathogenesis involved in NSEBCC. However, these results should be carefully interpreted given that there was only a limited number of patients in these subgroups and the design of study was a retrospective cohort study rather than a case-control study.
Our study observed an association between immunosuppression status with the development of NSEBCC. Although previous study showed that immunosuppression act as a risk factor of developing non-melanoma skin cancer31, we did not observe a significantly higher risk for BCC recurrence among patients with immunosuppression. This discrepancy may result from the following reasons. First, our study design was different from previous studies, as our study aims at comparing patients with SEBCC and NSEBCC, rather than comparing the incidence rate of BCC between immunocompetent and immunosuppressive patients. Since NSEBCC had a lower recurrence rate than SEBCC, this may affect the recurrence rate observed in immunosuppressed patients. Second, the patient’s demographics were different among each study, as our study focusing on Asian population.
Our study showed that patients with dementia had a higher association with developing multiple BCC tumors. A. J. Schmidt et al. reported that NMSC was associated with reductions in risks of dementia32. We assumed that the seemingly contrary results may be explained by delayed visits to the hospital or even negligence due to decreased self-awareness on skin condition in patients with cognitive impairment. Selection bias from the surgeons cannot be excluded as well. Further studies to elucidate the causation between dementia and multiple BCC should be done.
This study was conducted at a single medical center with retrospective chart review. To our knowledge, no previous studies have been published, comparing histopathological profiles, risks of multiple tumor and recurrence between SEBCC and NSEBCC in an Asian population. However, this study still has a number of limitations. First, the exact duration and intensity of UV light exposure were impossible to quantify by chart review and the results should be interpreted with caution due to other unmeasured factors attributing to developing multiple BCC or recurrence, such as occupation and lifestyle. Second, lesions that had not yet recurred or recurred after the study period would not have been included in the analysis. Since this was a single medical center study, loss of follow up or referral of patients to local hospitals and clinics may cause potential bias. Third, not all BCC lesions had a comprehensive description of histopathological features in the pathological report. Finally, due to the limited patient numbers and demographic profiles, the results should be carefully applied to other ethnic populations. Future investigation should aim at comparing the optimal surgical margin width in both SEBCC and NSEBCC group under a prospective study design with a larger number of patients and in different ethnic groups.
Methods
Data sources
A retrospective review of Kaohsiung Veterans General Hospital’s medical database was performed. Patients with pathologically verified BCC between January 1, 1990 and August 31, 2017 were included (ICD9:173, ICD10: C44.01, C44.11, C44.21, C44.31, C44.41, C44.51, C44.61, C44.71, C44.81, C44.91). All patients in this study were admitted to ward for examinations and surgical excision after receiving biopsy in outpatient department. Patients admitted without pathology to prove BCC with or without recurrence were excluded. Patients were also excluded if they had other skin lesions or tumors, or lost medical records. Both electronic and paper charts within this period of time were reviewed.
Study design
Patients were divided into two groups: those with SEBCC, and those with NSEBCC. Sun-exposed body parts included head and neck, forearms, wrists, and lower legs. In order to compare the differences between the two groups, patients with both SEBCC and NSEBCC were excluded from this study. Figure 2 shows the patient selection flowchart.
Data were derived from chart review and pathology reports, including sex, age at diagnosis, relevant medical comorbidities, anatomic tumor site, surgical data, staging, and histopathological profile. Multiple BCC, recurrence, and metastasis were also recorded. Multiple BCC is defined as more than one tumor diagnosed at different anatomic sites synchronously or asynchronously. Recurring lesions were observed from the time period of January 1990 until the patient’s latest visit to the hospital and are defined as a tumor re-occurring in the primary tumor site after excision.
Histopathological profile
Both the width and depth of the lesions were documented according to the pathology report. Pathological type, Clark level, tumor staging, surgical margin status, and high-risk features of recurrence were also obtained from the pathology report. The staging of BCC is defined according to the American Joint Committee on Cancer (AJCC) 7th edition of cutaneous squamous cell carcinoma (cSCC) extrapolated in BCCs.
Statistical analysis
Differences in the distribution of demographic data, comorbidities and BCC characteristics were compared using the t-test for continuous variables, and the Pearson χ2 test or Fisher’s exact test for categorical variables. Logistic regression models were used to calculate crude and adjusted odds ratios (aOR) with 95% confidence intervals (CI) for the development of multiple BCC lesions. No significant interactions were found among variables that were selected for the multivariate logistic regression model. Cox proportional hazards model was used to estimate hazards ratios (HR) and 95% CIs for the recurrence of BCC lesions. SPSS statistical software, version 19.0 for Windows, was used for all data analysis. All methods were performed in accordance with the relevant guidelines and regulations. This retrospective study adhered to the tenets of the Declaration of Helsinki and was approved by the Institutional Review Board of Kaohsiung Veterans General Hospital (approved number: VGHKS19-CT7-02). A waiver of informed consent was granted by the approving Institutional Review Board.
Conclusion
In conclusion, our study found that SEBCC had a higher recurrence rate with a significantly different tumor characteristic from NSEBCC and a greater tumor depth than NSEBCC. As the superficial type is predominant in NSEBCC and no recurrence in NSEBCC patients was found in this study, we suggested NSEBCC might not need a wider surgical margin as current guideline suggested and a wider safe margin for SEBCC than NSEBCC is indicated. The risk factors for BCC recurrence included infiltrating or mixed-infiltrating subtype and the existence of synchronous basosquamous cell carcinoma. Patients with NSEBCC had a significantly higher association with chronic kidney disease and rheumatoid arthritis than with those in the SEBCC group.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding authors on reasonable request.
References
Lomas, A., Leonardi-Bee, J. & Bath-Hextall, F. A systematic review of worldwide incidence of nonmelanoma skin cancer. The British journal of dermatology 166, 1069–1080, https://doi.org/10.1111/j.1365-2133.2012.10830.x (2012).
Battie, C., Gohara, M., Verschoore, M. & Roberts, W. Skin cancer in skin of color: an update on current facts, trends, and misconceptions. Journal of drugs in dermatology: JDD 12, 194–198 (2013).
Gupta, A. K., Bharadwaj, M. & Mehrotra, R. Skin Cancer Concerns in People of Color: Risk Factors and Prevention. Asian Pac J Cancer Prev 17, 5257–5264, https://doi.org/10.22034/APJCP.2016.17.12.5257 (2016).
Wu, X. C. et al. Racial and ethnic variations in incidence and survival of cutaneous melanoma in the United States, 1999-2006. Journal of the American Academy of Dermatology 65, S26–37, https://doi.org/10.1016/j.jaad.2011.05.034 (2011).
Chiang, C. J. et al. Cancer trends in Taiwan. Jpn J Clin Oncol 40, 897–904, https://doi.org/10.1093/jjco/hyq057 (2010).
van Dam, R. M. et al. Risk factors for basal cell carcinoma of the skin in men: results from the health professionals follow-up study. American journal of epidemiology 150, 459–468 (1999).
Vitasa, B. C. et al. Association of nonmelanoma skin cancer and actinic keratosis with cumulative solar ultraviolet exposure in Maryland watermen. Cancer 65, 2811–2817 (1990).
Zanetti, R. et al. Comparison of risk patterns in carcinoma and melanoma of the skin in men: a multi-centre case-case-control study. British journal of cancer 94, 743–751, https://doi.org/10.1038/sj.bjc.6602982 (2006).
Tilli, C. M., Van Steensel, M. A., Krekels, G. A., Neumann, H. A. & Ramaekers, F. C. Molecular aetiology and pathogenesis of basal cell carcinoma. The British journal of dermatology 152, 1108–1124, https://doi.org/10.1111/j.1365-2133.2005.06587.x (2005).
Wang, G. Y., Wang, J., Mancianti, M. L. & Epstein, E. H. Jr. Basal cell carcinomas arise from hair follicle stem cells in Ptch1(+/-) mice. Cancer Cell 19, 114–124, https://doi.org/10.1016/j.ccr.2010.11.007 (2011).
Choudhury, M. I. M. et al. Cutaneous Malignancy due to Arsenicosis in Bangladesh: 12-Year Study in Tertiary Level Hospital. Biomed Res Int 2018, 4678362, https://doi.org/10.1155/2018/4678362 (2018).
Pfister, H. & Ter Schegget, J. Role of HPV in cutaneous premalignant and malignant tumors. Clinics in dermatology 15, 335–347 (1997).
Preston, D. S. & Stern, R. S. Nonmelanoma cancers of the skin. N Engl J Med 327, 1649–1662, https://doi.org/10.1056/NEJM199212033272307 (1992).
Wollenberg, A., Peter, R. U. & Przybilla, B. Multiple superficial basal cell carcinomas (basalomatosis) following cobalt irradiation. The British journal of dermatology 133, 644–646 (1995).
Abeldaño, A. et al. Basal Cell carcinoma of unusual localization. Dermatología Argentina 16, 25–33 (2010).
Bastiaens, M. T. et al. Differences in age, site distribution, and sex between nodular and superficial basal cell carcinoma indicate different types of tumors. J Invest Dermatol 110, 880–884, https://doi.org/10.1046/j.1523-1747.1998.00217.x (1998).
Betti, R. et al. Anatomic location of Basal cell carcinomas may favor certain histologic subtypes. J Cutan Med Surg 14, 298–302, https://doi.org/10.2310/77502010.09081 (2010).
Dahl, E., Aberg, M., Rausing, A. & Rausing, E. L. Basal cell carcinoma. An epidemiologic study in a defined population. Cancer 70, 104–108 (1992).
Sexton, M., Jones, D. B. & Maloney, M. E. Histologic pattern analysis of basal cell carcinoma. Study of a series of 1039 consecutive neoplasms. Journal of the American Academy of Dermatology 23, 1118–1126 (1990).
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: Basal cell skin cancer, https://www.nccn.org/professionals/physician_gls/f_guidelines.asp.Accessed 28 Nov, 2018.
Hendrix, J. D. Jr. & Parlette, H. L. Micronodular basal cell carcinoma. A deceptive histologic subtype with frequent clinically undetected tumor extension. Arch Dermatol 132, 295–298 (1996).
Lang, P. G. Jr. & Maize, J. C. Histologic evolution of recurrent basal cell carcinoma and treatment implications. Journal of the American Academy of Dermatology 14, 186–196 (1986).
Urechescu, H. C. et al. Basal cell carcinoma and basosquamous carcinoma, two faces of the same condition? Romanian journal of morphology and embryology = Revue roumaine de morphologie et embryologie 59, 989–996 (2018).
Armstrong, L. T. D., Magnusson, M. R. & Guppy, M. P. B. Risk factors for recurrence of facial basal cell carcinoma after surgical excision: A follow-up analysis. J Plast Reconstr Aesthet Surg 70, 1738–1745, https://doi.org/10.1016/j.bjps.2017.04.006 (2017).
Wolf, D. J. & Zitelli, J. A. Surgical margins for basal cell carcinoma. Arch Dermatol 123, 340–344, https://doi.org/10.1001/archderm.1987.01660270078019 (1987).
Chren, M. M. et al. Recurrence after treatment of nonmelanoma skin cancer: a prospective cohort study. Arch Dermatol 147, 540–546, https://doi.org/10.1001/archdermatol.2011.109 (2011).
Tseng, H. W. et al. The influence of disease-modifying anti-rheumatic drugs and corticosteroids on the association between rheumatoid arthritis and skin cancer: a nationwide retrospective case-control study in Taiwan. Clin Exp Rheumatol 36, 471–478 (2018).
Wang, C. C., Tang, C. H., Huang, S. Y., Huang, K. C. & Sue, Y. M. Risk of Non-melanoma Skin Cancer in Patients with Chronic Kidney Disease and its Relationship to Uraemic Pruritus. Acta Derm Venereol 97, 1230–1234, https://doi.org/10.2340/00015555-2762 (2017).
Kaysen, G. A. The microinflammatory state in uremia: causes and potential consequences. J Am Soc Nephrol 12, 1549–1557 (2001).
Schupp, N. & Heidland, A. & Stopper, H. Genomic damage in endstage renal disease-contribution of uremic toxins. Toxins (Basel) 2, 2340–2358, https://doi.org/10.3390/toxins2102340 (2010).
Zak-Prelich, M., Narbutt, J. & Sysa-Jedrzejowska, A. Environmental risk factors predisposing to the development of basal cell carcinoma. Dermatol Surg 30, 248–252 (2004).
Schmidt, S. A., Ording, A. G., Horvath-Puho, E., Sorensen, H. T. & Henderson, V. W. Non-melanoma skin cancer and risk of Alzheimer’s disease and all-cause dementia. PLoS One 12, e0171527, https://doi.org/10.1371/journal.pone.0171527 (2017).
Author information
Authors and Affiliations
Contributions
C.L.L., Y.C.C. and L.W.C. conceived and designed the study. C.L.L and Y.C.C. involved in the collection of the data. C.L.L. involved in the analysis and interpretation of the data and drafted the manuscript. C.L.L., Y.C.C., K.C.Y. and L.W.C. revised the paper. All authors approved the paper as submitted and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, CL., Chen, YC., Yang, KC. et al. Different histopathologic profiles and outcomes between sun-exposed BCC and non-sun-exposed BCC. Sci Rep 10, 7387 (2020). https://doi.org/10.1038/s41598-020-64391-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-64391-9
- Springer Nature Limited