Abstract
We developed a predictive score system for 30-day mortality after palliative radiotherapy by using predictors from routine electronic medical record. Patients with metastatic cancer receiving first course palliative radiotherapy from 1 July, 2007 to 31 December, 2017 were identified. 30-day mortality odds ratios and probabilities of the death predictive score were obtained using multivariable logistic regression model. Overall, 5,795 patients participated. Median follow-up was 39.6 months (range, 24.5–69.3) for all surviving patients. 5,290 patients died over a median 110 days, of whom 995 (17.2%) died within 30 days of radiotherapy commencement. The most important mortality predictors were primary lung cancer (odds ratio: 1.73, 95% confidence interval: 1.47–2.04) and log peripheral blood neutrophil lymphocyte ratio (odds ratio: 1.71, 95% confidence interval: 1.52–1.92). The developed predictive scoring system had 10 predictor variables and 20 points. The cross-validated area under curve was 0.81 (95% confidence interval: 0.79–0.82). The calibration suggested a reasonably good fit for the model (likelihood-ratio statistic: 2.81, P = 0.094), providing an accurate prediction for almost all 30-day mortality probabilities. The predictive scoring system accurately predicted 30-day mortality among patients with stage IV cancer. Oncologists may use this to tailor palliative therapy for patients.
Similar content being viewed by others
Introduction
Many patients with metastatic cancer receive oncological treatment, and radiotherapy (RT) is an important component of palliative treatment1. RT can be an effective tool for palliation of symptoms arising from cancer, including pain from bone metastases or neurological compromise from brain or spinal metastases with cord or nerve root compression. The aim of palliative RT is to alleviate symptoms and improve quality of life. Evidence has shown that palliative RT was received by approximately 10% of patients who died of cancer near their end of life2,3. In one population-based study that included 15,287 patients who received RT in the last month of life, 17.8% received more than 10 days of treatment4. This finding corroborates with a German study which showed 50% of patients spent more than 60% of remaining 30 days of life receiving RT4.
RT can be delivered via different dosing regimens (e.g., single fraction on one day versus multiple fractions for weeks)5,6,7,8,9. The use of multi-fractionation (split up the total dose into small fractions) is often perceived to be associated with less long-term complications and need for retreatment4. While larger fraction size by single-fractionation theoretically has an increased risk of late-onset radiation toxicity. Beside radiobiological consideration, medical training and experience, departmental policies, and insurance reimbursement all influence the decision on the dose-fractionation regimens. Use of hypofractionation or single fractionation is associated with a perceived poor prognosis by the oncologist. Protracted courses of RT can become considerable demand and burden on terminal cancer patients7. Their symptoms can be aggravated by transportation to the RT facility and repeated positioning in the treatment suite. It is also costly to the healthcare system but might also preclude the trigger for end-of-life measures for this group of patients.
As highlighted in the statement by the American Society of Clinical Oncology in 2011, transition from focusing on cancer-directed therapy to palliative care often occurs within days of death10. This is possibly related to the poor accuracy of clinicians at predicting prognosis and survival of patients with advanced malignancies11,12,13. An accurate and practical short-term mortality prediction score for patients with metastatic cancer receiving palliative RT can assist clinicians in tailoring palliative RT use and for delivering appropriate dose-fractionations according to the expected short-term risk of death. Furthermore, an earlier and more thorough assessment of patient management options, goals, and preferences to facilitate personalized palliative care along the disease trajectory will be possible. When a cure is not possible, the goals of treatment change appropriately from prolonging life to controlling symptoms and improving quality of life. However, evidence has shown that clinician estimates of survival tend to be optimistic and poorly reproducible11. Prognosis overestimates may have contributed to mismatched fractionation schedules, and lots of patients needing to discontinue therapy.
The determination of prognosis and life expectancy is critical to the care of patients with advanced cancer. Prognostic factors and predictive tools have been explored and developed to improve the estimation of life expectancy over the clinician’s estimation. However, most of these studies are based on small study samples and hospital settings with short follow-up and survival times (in terms of weeks) or based on single tumor sites and are not specific to patients referred for RT14,15,16,17. Some studied the prognostic factors for survival time after palliative RT but did not develop a predictive model3,18. Palliative RT rarely affect survival time but often improves quality of life19,20. To improve palliative RT delivery and resource allocation optimization, we conducted a cohort study using routinely collected electronic data from patients with metastatic cancer receiving their first course of palliative RT. We studied the factors associated with short-term mortality and developed a predictive score model for 30-day mortality.
Methods
Data source
We retrieved data for our patient cohort on April 1, 2019. All RT episodes were identified using the MOSAIQ information system42, which archives and integrates RT planning and treatment details. These data were then linked to the entries maintained by the Clinical Data Analysis and Reporting System, which is an electronic medical record (EMR) database operated by the Hospital Authority of Hong Kong. The International Classification of Diseases, ninth revision (ICD-9), was used for disease coding. We followed the transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD) guideline for model development and validation43,44. The Research Ethics Committee, New Territories West Cluster, Hospital Authority, Hong Kong approved the study on October 1, 2018, and waived patient consent requirement (reference no: NTWC/REC/18093). The research was conducted in accordance with the 1964 Declaration of Helsinki and its later amendments.
Patients, data, and settings
We included patients with metastatic cancer who received palliative RT at Tuen Mun Hospital, Hong Kong, between July 1, 2007 and December 31, 2017, and had not received palliative radiotherapy at the center before July 1, 2007. The definition of first course palliative RT fraction was based on a combination of the receipt of an identified palliative dose-fractionation and the treating oncologist’s indication; a RT course is defined as one or more fractions of external beam RT, delivered to a defined area.
Short-term mortality predictive risk factors
To transform raw EMR data into variables usable in a prediction model, we first collected all data from the 180- to 365-day period (depending on particular variables), ending the day before palliative RT initiation (we did not exclude patients based on absence of data during the period). Raw data were aggregated into potential predictors in the following categories: demographics, prescribed medications, comorbidities and other grouped ICD-9 diagnoses, surgical procedures, health care resource use, and laboratory results. No data on the first course palliative RT itself (e.g., dose-fractionation and techniques) were used in the predictive model. More precise information on the variables used as short-term mortality predictors are provided in Appendix 1 and Supplementary Table 3.
Outcomes
Our primary outcome was 30-day overall mortality, which was calculated from the start of the first course palliative RT until death or when censored (April 1, 2019). The start date of RT was used because it was closer to the date when the clinical decision to treat was made than that of the end of treatment and provides a uniform time point across all fractionation regimens.
Model selection, performance, and scoring
We used multivariable logistic regression models to evaluate the predictive performance of the primary outcome, 30-day mortality45,46. The model’s predictor functions were pre-specified a priori based on subject matter knowledge (Table 2). We assumed a pattern of randomness and created one imputed dataset using a fully conditional specification based on a multivariate normal distribution47. Different combinations of the 13 covariates were chosen for the regression models (Table 2). The 13 covariates were age, sex, Royal College of Surgeons modified comorbidity score48, log peripheral white blood cell count, log peripheral blood neutrophil lymphocyte ratio (NLR), log plasma urea, log serum bilirubin, serum albumin, lactate dehydrogenase (LDH), red cell distribution, attendance to emergency room, sites receiving palliative RT, and primary lung cancer.
Data-adaptive methods based on cross-validation and mean absolute error for predictions (MAE) were used to evaluate the predictive performance of different model specifications. We used ten-fold cross-validation to reduce the risk of overfitting the final model to the training set49. The cross-validation procedure involved fitting a candidate model for the primary outcome, using data from nine of the ten blocks (the “derivation set”), and evaluating its performance in the held-out block (the “validation set”). We repeated this process ten times, each time using a different block as the validation set, and then averaged the performance over the ten validation sets.
As the overall performance metric, we used the MAE, which measures the average of the difference between predicted and observed outcome in the test, i.e., the average prediction error50. This represents the closeness of the prediction to the eventual outcomes. Our measure of model discrimination was the cross-validated areas under the receiver operating characteristic (ROC) curves51,52. An ROC curve is a plot of the sensitivity of a model (the vertical axis) vs 1 minus the specificity (the horizontal axis) for all possible cut-off values that might be used to classify patients predicted to have 30-day mortality compared with patients who will not die within 30 days51. Given any 2 random patients, one died within 30 days and one did not, the probability that the model will correctly classify the patient with the outcome as higher risk is equal to the area under the ROC curve (AUC)53. We calculated 95% confidence intervals (CIs) of the AUC following the method of DeLong et al.54. We evaluated the model calibration by observing the agreement between observed outcomes and predictions55. We used a graphical assessment of calibration, with predictions on the x-axis and the observed outcome on the y-axis. We performed a sensitivity analysis to evaluate the robustness of model performance by testing different model specifications.
Finally, we produced a point score system from the best model we developed. In the system, points were assigned based on the predictor values for a patient; the total scores correspond to the risks of the 30-day overall mortality56. The steps to develop the point score system have been summarized in the Appendix 2. For each point score we summarized the positive predictive value (PPV) and negative predictive value (NPV) which respectively represented the probability that the disease is present given a positive test result and that the disease is absent given a negative test result57.
Statistical analysis
Descriptive analyses were conducted to describe the cohort of patients receiving first course palliative RT. We used frequencies and proportions for categorical variables and means with standard deviations (when normally distributed) or medians with interquartile ranges (when not normally distributed) for continuous variables. To describe the association between patient factors and an increased or decreased short-term mortality, we reported odds ratios (OR) from univariable and multivariable logistic regressions with their respective 95% CI.
The analysis was performed using Stata v.15.1 (StataCorp LLC, College Station, Texas, USA) and R v. 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria)58,59.
Results
Description of the cohort
We identified 5,795 patients who commenced palliative RT between July 1, 2007 and December 31, 2017. Patient characteristics are summarized in Table 1. The median age was 64 (interquartile range: 55–75) years; 61.8% were male. Patients with lung cancer (39.7%) constituted the highest proportion of the cohort. In all, 55.1%, 29.2%, and 15.7% were classified as having score 0, 1, and ≥2, according to the Royal College of Surgeons modified Charlson score, respectively. A total of 5,291 patients died during the follow-up period (median follow-up 3 months), of which 995 patients (17.2%) died within 30 days from the start of RT. Data were complete except for those on albumin, peripheral blood cell counts, urea, bilirubin, and LDH, which were imputed21.
Thirty-day mortality and model performance
Of the 5,795 patients receiving their first course palliative RT, 995 (17.2%) died within 30 days. Model 2 was chosen as the best performing model among candidate models 1–4 from the regression analyses (Table 2). The most important predictors of short-term mortality were primary lung cancer (OR: 1.73, 95% CI: 1.47–2.04), log peripheral blood NLR (OR: 1.71, 95% CI 1.52–1.92), and log plasma urea (OR: 1.55, 95% CI: 1.32–1.82).
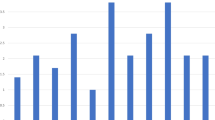
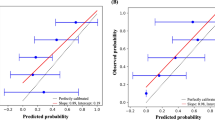
Figure 1 shows good model discriminations from the candidate models by the ROC curves. Figure 2 shows the 10-fold cross-validated receiver-operating characteristics (cv-ROC) curve for 30-day mortality prediction from the best model (model 2 in Table 2). Model 2 showed the highest discrimination, i.e., its predictive accuracy was good, with a cross-validated-area under curve (cvAUC) of 0.81 (95% CI: 0.79–0.82) (Figs. 1,2).
Model discriminations from the four candidate models by the receiver-operating characteristics (ROC) curves, as shown by the respective areas under curve. (created using Stata v.15.1, https://www.stata.com/).
10-fold cv-ROC curves for 30-day mortality prediction from the best candidate model (model 2), which has a cv-area under curve of 0.811. SD: standard deviation; cv-ROC: cross-validated receiver-operating characteristics. (created using Stata v.15.1, https://www.stata.com/).
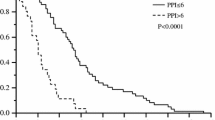
Tables 3 and 4 show the point score and average predicted probabilities of 30-day mortality based on model 2, respectively. For ease of interpretation, values of the predictors in log-scale were back-transformed to their original scale. A point score cut-off value of 6 (positive predictive value: 33.0%; negative predictive value: 94.2%; sensitivity: 80.3%; specificity: 66.2%) showed the greatest Youden’s index (46.5), corresponding to maximum joint sensitivity and specificity on the ROC curve.
Supplementary Figure 1 shows the predicted probabilities of 30-day mortality by mortality status. The model calibration suggests a reasonably good fit for the model (Supplementary Fig. 2, likelihood-ratio statistic: 2.81, P = 0.094), which provides accurate predictions for almost the entire range of the death probability. The predicted probabilities stay close to the ideal calibration line for low and high probabilities of death. Sensitivity analyses showed no association between comorbidities and 30-day mortality or interaction between comorbidities and age; no association between systemic treatments, including chemotherapy, and null increase in predictive performance was observed, regardless of whether comorbidity was included in the model. Additionally, in sensitivity analysis we assessed whether our model was consistent to different windows of time (0–29, 0–35 and 0–45 days) and we applied our point score system to predict 3- and 6-month mortality in the same patient cohorts. We found similar values of NPV and PPV (Supplementary Tables 1 and 2).
Discussion
We found that primary lung cancer, peripheral blood NLR, and plasma urea were strong predictors of short-term mortality among patients with stage IV cancer. Our score system was a good predictor of short-term mortality; performance metrics by ROC curves and calibration curves showed high model discrimination and calibration, respectively.
More recent and successful studies on predictive models for survival after palliative RT in patients with advanced cancer were conducted by Chow et al. and Kristnan et al.22,23,24. These studies are similar; however, ours has important advantages. We developed a scoring system that uses objective measurements (complete blood counts, liver and renal function tests within 180 days) to determine the 30-day mortality of patients receiving palliative RT. Furthermore, our data were obtained from routine practice; this increased the model’s clinical applicability, unlike those by Chow et al., whose Radiotherapy Rapid Response Programme was established with an aim to provide quick palliative RT for patients with terminal cancer mostly referred from medical oncologists and palliative care doctors22,23. Our model for prediction of 30-day mortality was developed based on a large population of unselected adults referred for palliative RT (5,795 patients versus 395 in Chow et al. and 862 in Krishnan et al.). The concordance (C)-statistic is a measure of goodness-of-fit for binary outcomes in a logistic regression model. It represents the probability that the predicted and observed outcomes are concordant for a randomly selected pair of patients in the predictive model25. The C-statistic for TEACHH model and Chow’s model based on 3 risk factors were 0.59 and 0.65 respectively23,24, while the AUC (equivalent to C-statistic) in our model was 0.81 which is better. The AUC was cross-validated which reduces the optimism bias of the other two and was internally validated to provide higher consistency in absence of an external validation. It is an easy-to-calculate tool for patients with metastatic cancer who were referred for palliative RT and who account for 20–40% of patients treated in radiation oncology departments26,27,28,29. Furthermore, given the mandatory status of death certification in Hong Kong and the automated nature of RT and vital status data collection, data on the dates of the first course of palliative RT and death were reliable. The referring clinician’s indication was included in our definition of palliative RT, which was better than merely using predefined dose and fractionation schedules. Our model performed reasonably well across a range of cancer types and other variables, despite lacking genetic data, cancer-specific biomarkers, or any detailed information beyond EMR. This emphasized that commonly available data in EMR contain important predictors to identify clinically relevant outcomes in patients with cancer under palliative care. Most of the inputs to the model are standard structured data components in EMR. The model’s algorithm could easily integrate into existing clinical management systems, importing the data directly from the EMR without specialized infrastructure. Additionally, implementing the tool can continuously and independently validate the predictive power from an ongoing prospective cohort. This is important to reflect the secular trend in cancer epidemiology changes, treatment variations, and referral patterns in an evolving real-world setting.
The model outperformed clinician estimates of survival to guide appropriate clinical judgment in treatment, resource allocation, and early palliative care referrals with advanced care planning30. The NPV exceeded 90% which means patients have very high chance of staying alive beyond 30 days if predicted so by the model. This could be a better standpoint to start dialogue with patients. Realistic and honest disclosure of prognosis can encourage shared decision-making between the patient and the care team, with which the patient can settle personal, family, and financial issues earlier, instead of embarking on another course of treatment based on inaccurate prognosis. However, after thorough discussions with the patient and family, if the patient still opts for RT despite reasonable chance of early mortality, we argue that hypofractionation is preferred to avoid a protracted course of RT near death, given the well-documented evidence for equivalent effects in a range of symptoms31.
Regarding the choice of covariates and development of the model, patients referred for palliative RT often received oncological treatment and blood work before; hence, we included commonly performed biochemical or hematological markers. Clinical experience has shown that patients with lung cancer generally die earlier than patients with other cancers, such as breast cancer14, and patients with certain sites of metastases (e.g., bone only) live longer than patients with others, such as brain and spinal metastases with cord compression32,33,34,35. Since no data were available on sites of metastatic diseases, we substituted with irradiation data. Hence, we included primary cancer site and irradiation site in the score determination. Age may influence not only recommendations for treatment but also prediction of remaining lifespan, analyzed in our model. Moreover, clinician estimates of survival were excluded because they were likely based on experience and training, poorly reproducible, and not commonly recorded in routine electronic database.
Our study had limitations. First, the prediction model was built on data from patients treated with RT and might not be accurate for untreated patients. Second, our procedure for categorizing the predictor variables may not identify the cutoff values with the best discriminating capacity. Third, some important prognostic factors may have been omitted. For example, data on performance status and patient quality of life evaluations using validated scales, or of their frailty status36,37, considered prognostic in previous studies, were not analyzed22. However, we introduced patient comorbidities as proxy for patient frailties. Fourth, palliative RT use was at the oncologists’ discretion in some cases when curative and palliative intent treatment could not be distinguished (e.g., patients having limited metastasis receiving higher dose RT for better local control). Finally, we considered the patients for first course palliative RT without considering the effects of subsequent RT courses and other treatments.
A prediction tool using EMR data, retrieved from routine clinical practice, can accurately predict short-term mortality among patients with advanced cancer starting radiotherapy. Such tool could facilitate shared decision-making among the patients, family, and medical care team. Additionally, it could help clinicians identify patients unlikely to benefit from RT beyond 30 days and those who may instead benefit from earlier palliative care referral and end-of-life planning. Machine learning techniques have the potential to improve clinical decision-making by identifying those at increased risk of poor mortality38. In 3 studies summarized by a systematic review, machine learning techniques are better than routine logistic regression in building model for mortality prediction in older and/or hospitalized adults, if enough data are obtained38,39,40,41. Future research is needed to incorporate machine learning techniques and to determine the generalizability and feasibility of the application of prediction tool in clinical settings.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Jacob, S., Wong, K., Delaney, G. P., Adams, P. & Barton, M. B. Estimation of an optimal utilisation rate for palliative radiotherapy in newly diagnosed cancer patients. Clin. Oncol. 22, 56–64, https://doi.org/10.1016/j.clon.2009.11.003 (2010).
Park, K. R. et al. Palliative radiation therapy in the last 30 days of life: A systematic review. Radiotherapy oncology: J. Eur. Soc. Therapeutic Radiology Oncol. 125, 193–199, https://doi.org/10.1016/j.radonc.2017.09.016 (2017).
Spencer, K. et al. 30 day mortality in adult palliative radiotherapy–A retrospective population based study of 14,972 treatment episodes. Radiother. Oncol. 115, 264–271, https://doi.org/10.1016/j.radonc.2015.03.023 (2015).
Gripp, S., Mjartan, S., Boelke, E. & Willers, R. Palliative radiotherapy tailored to life expectancy in end-stage cancer patients: reality or myth? Cancer 116, 3251–3256, https://doi.org/10.1002/cncr.25112 (2010).
Hartsell, W. F. et al. Randomized trial of short- versus long-course radiotherapy for palliation of painful bone metastases. J. Natl Cancer Inst. 97, 798–804, https://doi.org/10.1093/jnci/dji139 (2005).
Rades, D. et al. Is short-course radiotherapy with high doses per fraction the appropriate regimen for metastatic spinal cord compression in colorectal cancer patients? Strahlenther. Onkol. 182, 708–712, https://doi.org/10.1007/s00066-006-1578-9 (2006).
Chow, E., Harris, K., Fan, G., Tsao, M. & Sze, W. M. Palliative radiotherapy trials for bone metastases: a systematic review. J. Clin. oncology: Off. J. Am. Soc. Clin. Oncol. 25, 1423–1436, https://doi.org/10.1200/JCO.2006.09.5281 (2007).
Rades, D., Lohynska, R., Veninga, T., Stalpers, L. J. A. & Schild, S. E. Evaluation of 2 whole-brain radiotherapy schedules and prognostic factors for brain metastases in breast cancer patients. Cancer 110, 2587–2592, https://doi.org/10.1002/cncr.23082 (2007).
Dobbs, J. & Barrett, A. In Practical Radiotherapy Planning 62–70 (Taylor & Francis, 2009).
Peppercorn, J. M. et al. American society of clinical oncology statement: toward individualized care for patients with advanced cancer. J. Clin. Oncol. 29, 755–760, https://doi.org/10.1200/jco.2010.33.1744 (2011).
Chow, E. et al. How accurate are physicians’ clinical predictions of survival and the available prognostic tools in estimating survival times in terminally ill cancer patients? A systematic review. Clin. Oncol. 13, 209–218 (2001).
Christakis, N. A. & Lamont, E. B. Extent and determinants of error in doctors’ prognoses in terminally ill patients: prospective cohort study. BMJ 320, 469–472 (2000).
Glare, P. et al. Predicting survival in patients with advanced disease. Eur. J. Cancer 44, 1146–1156, https://doi.org/10.1016/j.ejca.2008.02.030 (2008).
Hardy, J. R., Turner, R., Saunders, M. & A’Hern, R. Prediction of survival in a hospital-based continuing care unit. Eur. J. Cancer 30, 284–288, https://doi.org/10.1016/0959-8049(94)90242-9 (1994).
Christakis, N. A. & Escarce, J. J. Survival of Medicare patients after enrollment in hospice programs. N. Engl. J. Med. 335, 172–178, https://doi.org/10.1056/nejm199607183350306 (1996).
Lassen, U. et al. Long-term survival in small-cell lung cancer: posttreatment characteristics in patients surviving 5 to 18+ years–an analysis of 1,714 consecutive patients. J. Clin. Oncol. 13, 1215–1220, https://doi.org/10.1200/jco.1995.13.5.1215 (1995).
Gwilliam, B. et al. Development of Prognosis in Palliative care Study (PiPS) predictor models to improve prognostication in advanced cancer: prospective cohort study. BMJ 343, d4920, https://doi.org/10.1136/bmj.d4920 (2011).
Williams, M., Woolf, D., Dickson, J., Hughes, R. & Maher, J. Routine clinical data predict survival after palliative radiotherapy: an opportunity to improve end of life care. Clin. Oncol. 25, 668–673, https://doi.org/10.1016/j.clon.2013.06.003 (2013).
Spencer, K., Parrish, R., Barton, R. & Henry, A. Palliative radiotherapy. BMJ 360, k821–k821, https://doi.org/10.1136/bmj.k821 (2018).
Lutz, S. T., Jones, J. & Chow, E. Role of radiation therapy in palliative care of the patient with cancer. J. Clin. oncology: Off. J. Am. Soc. Clin. Oncol. 32, 2913–2919, https://doi.org/10.1200/JCO.2014.55.1143 (2014).
Rubin, D. B. Multiple Imputation for Nonresponse in Surveys. (Wiley, 2009).
Chow, E. et al. A predictive model for survival in metastatic cancer patients attending an outpatient palliative radiotherapy clinic. Int. J. Radiat. Oncol. Biol. Phys. 53, 1291–1302, https://doi.org/10.1016/s0360-3016(02)02832-8 (2002).
Chow, E. et al. Predictive model for survival in patients with advanced cancer. J. Clin. oncology: Off. J. Am. Soc. Clin. Oncol. 26, 5863–5869, https://doi.org/10.1200/JCO.2008.17.1363 (2008).
Krishnan, M. S. et al. Predicting life expectancy in patients with metastatic cancer receiving palliative radiotherapy: the TEACHH model. Cancer 120, 134–141, https://doi.org/10.1002/cncr.28408 (2014).
Austin, P. C. & Steyerberg, E. W. Interpreting the concordance statistic of a logistic regression model: relation to the variance and odds ratio of a continuous explanatory variable. BMC Med. Res. Methodol. 12, 82, https://doi.org/10.1186/1471-2288-12-82 (2012).
Coia, L. R. et al. Practice patterns of palliative care for the united states 1984–1985. Int. J. Radiat. Oncology*Biology*Physics 14, 1261–1269, https://doi.org/10.1016/0360-3016(88)90405-1 (1988).
Huang, J. et al. Factors affecting the use of palliative radiotherapy in Ontario. J. Clin. Oncol. 19, 137–144, https://doi.org/10.1200/jco.2001.19.1.137 (2001).
Janjan, N. A. An emerging respect for palliative care in radiation oncology. J. Palliat. Med. 1, 83–88, https://doi.org/10.1089/jpm.1998.1.83 (1998).
McCloskey, S. A., Tao, M. L., Rose, C. M., Fink, A. & Amadeo, A. M. National survey of perspectives of palliative radiation therapy: role, barriers, and needs. Cancer J. 13, 130–137, https://doi.org/10.1097/PPO.0b013e31804675d4 (2007).
Maher, E. J. How long have I got doctor? Eur. J. Cancer 30, 283–284, https://doi.org/10.1016/0959-8049(94)90241-0 (1994).
Stevens, R., Macbeth, F., Toy, E., Coles, B. & Lester, J. F. Palliative radiotherapy regimens for patients with thoracic symptoms from non‐small cell lung cancer. Cochrane Database of Systematic Reviews, https://doi.org/10.1002/14651858.CD002143.pub3 (2015).
Chen, J. The prognostic analysis of different metastatic patterns in advanced liver cancer patients: A population based analysis. PLOS ONE 13, e0200909, https://doi.org/10.1371/journal.pone.0200909 (2018).
Perez, J. E. et al. Bone-only versus visceral-only metastatic pattern in breast cancer: analysis of 150 patients. A GOCS study. Grupo Oncologico Cooperativo del Sur. Am. J. Clin. Oncol. 13, 294–298, https://doi.org/10.1097/00000421-199008000-00005 (1990).
Yamashita, K. et al. Breast cancer with bone-only metastases. Visceral metastases-free rate in relation to anatomic distribution of bone metastases. Cancer 68, 634–637, 10.1002/1097-0142(19910801)68:3<634::aid-cncr2820680332>3.0.co;2-b (1991).
Kimura, T. Multidisciplinary Approach for Bone Metastasis: A Review. Cancers 10, 156 (2018).
Coates, A., Porzsolt, F. & Osoba, D. Quality of life in oncology practice: prognostic value of EORTC QLQ-C30 scores in patients with advanced malignancy. Eur. J. cancer 33, 1025–1030, https://doi.org/10.1016/s0959-8049(97)00049-x (1997).
Loprinzi, C. L. et al. Prospective evaluation of prognostic variables from patient-completed questionnaires. North Central Cancer Treatment Group. J. Clin. Oncol. 12, 601–607, https://doi.org/10.1200/jco.1994.12.3.601 (1994).
Storick, V., O?Herlihy, A., Abdelhafeez, S., Ahmed, R. & May, P. Improving palliative care with machine learning and routine data: a rapid review [version 2; peer review: 3 approved]. HRB Open Research 2, https://doi.org/10.12688/hrbopenres.12923.2 (2019).
Einav, L., Finkelstein, A., Mullainathan, S. & Obermeyer, Z. Predictive modeling of U.S. health care spending in late life. Science 360, 1462–1465, https://doi.org/10.1126/science.aar5045 (2018).
Makar, M., Ghassemi, M., Cutler, D. M. & Obermeyer, Z. Short-term Mortality Prediction for Elderly Patients Using Medicare Claims Data. Int. J. Mach. Learn. Comput. 5, 192–197, https://doi.org/10.7763/IJMLC.2015.V5.506 (2015).
Sahni, N., Simon, G. & Arora, R. Development and Validation of Machine Learning Models for Prediction of 1-Year Mortality Utilizing Electronic Medical Record Data Available at the End of Hospitalization in Multicondition Patients: a Proof-of-Concept Study. J. Gen. Intern. Med. 33, 921–928, https://doi.org/10.1007/s11606-018-4316-y (2018).
Elekta. MOSAIQ® Radiation Oncology,https://www.elekta.com/software-solutions/care-management/mosaiq-radiation-oncology/#mosaiq-radiation-oncology-ar.
Collins, G. S., Reitsma, J. B., Altman, D. G. & Moons, K. G. Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): the TRIPOD statement. Ann. Intern. Med. 162, 55–63, https://doi.org/10.7326/m14-0697 (2015).
Moons, K. G. et al. Transparent Reporting of a multivariable prediction model for Individual Prognosis or Diagnosis (TRIPOD): explanation and elaboration. Ann. Intern. Med. 162, W1–73, https://doi.org/10.7326/m14-0698 (2015).
Armitage, P., Berry, G. & Matthews, J. N. S. Statistical methods in medical research. 4th edn, (Blackwell Science, 2002).
Cox, D. R. Regression Models and Life-Tables. J. R. Stat. Soc. Ser. B Stat Methodol. 34, 187–220 (1972).
Carpenter, J. & Kenward, M. Multiple Imputation and its Application. (Wiley, 2012).
Brusselaers, N. & Lagergren, J. The Charlson Comorbidity Index in Registry-based Research. Methods Inf. Med. 56, 401–406, https://doi.org/10.3414/me17-01-0051 (2017).
Hastie, T., Tibshirani, R. & Friedman, J. H. The Elements of Statistical Learning: Data Mining, Inference, and Prediction. 2nd Ed edn, (Springer, 2009).
Willmott, C. J. & Matsuura, K. Advantages of the Mean Absolute Error (MAE) over the Root Mean Square Error (RMSE) in Assessing Average Model Performance. Clim. Res. 30, 79, https://doi.org/10.3354/cr030079 (2005).
Meurer, W. J. & Tolles, J. Logistic Regression Diagnostics: Understanding How Well a Model Predicts OutcomesLogistic Regression Diagnostics Logistic Regression Diagnostics. JAMA 317, 1068–1069, https://doi.org/10.1001/jama.2016.20441 (2017).
Steyerberg, E. W. et al. Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology 21, 128–138, https://doi.org/10.1097/EDE.0b013e3181c30fb2 (2010).
Hanley, J. A. & McNeil, B. J. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology 143, 29–36, https://doi.org/10.1148/radiology.143.1.7063747 (1982).
DeLong, E. R., DeLong, D. M. & Clarke-Pearson, D. L. Comparing the Areas under Two or More Correlated Receiver Operating Characteristic Curves: A Nonparametric Approach. Biometrics 44, 837–845, https://doi.org/10.2307/2531595 (1988).
Hilden, J., Habbema, J. D. & Bjerregaard, B. The measurement of performance in probabilistic diagnosis. II. Trustworthiness of the exact values of the diagnostic probabilities. Methods Inf. Med. 17, 227–237 (1978).
Sullivan, L. M., Massaro, J. M. & D’Agostino, R. B. Sr. Presentation of multivariate data for clinical use: The Framingham Study risk score functions. Stat. Med. 23, 1631–1660, https://doi.org/10.1002/sim.1742 (2004).
Wong, H. & Lim, G. H. Measures of Diagnostic Accuracy: Sensitivity, Specificity, PPV and NPV. Proc. Singap. Healthc. 20, 316–318, https://doi.org/10.1177/201010581102000411 (2011).
StataCorp. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC. 2017.
R Core Team R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/. (2019).
Acknowledgements
We thank the clinicians and staff members at Tuen Mun Hospital who collected the data, and Mr. KF Tsang for clerical support and data retrieval. There was no explicit funding for the development of this project. MALF is supported by a Miguel Servet I Investigator Award (grant CP17/00206 EU-FEDER) from the National Institute of Health, Carlos III (ISCIII), Madrid, Spain. His funders had no role in the study design, data collection, data analysis, data interpretation, or writing of the report.
Author information
Authors and Affiliations
Contributions
S.F.L. wrote the first draft of the manuscript under M.A.L.F.’s guidance. S.F.L., H.L., A.W. and M.A.L.F. were involved in the study design; S.F.L. and M.A.L.F. interpreted the data; S.F.L., C.K.N., F.C.S.W. and M.A.L.F. reviewed the manuscript. S.F.L. is the guarantor. S.F.L. attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lee, S.F., Luk, H., Wong, A. et al. Prediction model for short-term mortality after palliative radiotherapy for patients having advanced cancer: a cohort study from routine electronic medical data. Sci Rep 10, 5779 (2020). https://doi.org/10.1038/s41598-020-62826-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-62826-x
- Springer Nature Limited
This article is cited by
-
Palliative appropriateness criteria: external validation of a new method to evaluate the suitability of palliative radiotherapy fractionation
Strahlentherapie und Onkologie (2023)
-
Identifying patients with malignant spinal cord compression (MSCC) near end of life who can benefit from palliative radiotherapy
Radiation Oncology (2022)
-
Pre-diagnosis neutrophil-to-lymphocyte ratio and mortality in individuals who develop lung cancer
Cancer Causes & Control (2021)