Abstract
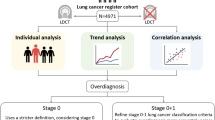
Screening programs for lung cancer aim to allow diagnosis at the early stage, and therefore the decline in mortality rates. Thus, the aim of this retrospective cohort study was to the comparison of screened and non-screened lung cancer in terms of lung cancer characteristics, overdiagnosis and survival rate. A retrospective study in which 2883 patients with 2883 lung cancer diagnosed according to the hospital-based lung cancer register database between 2007 and 2017. A comparison was performed in term of clinical characteristics and outcomes of lung cancer between the screened and non-screening patient groups. 2883 subjects were identified (93 screened and 2790 non-screened). Screened group patients were younger (59.91 ± 8.14 versus 67.58 ± 12.95; p < 0.0001), and were more likely to be female than non-screened group (61.3% versus 36.8%; p < 0.0001). The screened group showed significantly better outcomes in overall mortality than the non-screened group (10.75% versus 79.06%; <0.0001). In a Cox proportional hazard model, lung cancer in the screened group proved to be an independent prognostic factor in lung cancer subjects. Our findings point to the improved survival outcome in the screened group and might underline the benefit of low-dose computed tomography (LDCT) screening program in Asian populations with the high prevalence of non–smoking-related lung cancer. Further study aimed at the LDCT mass screening program targeting at light smokers and non-smoker outside of existing screening criteria is warranted.
Similar content being viewed by others
Introduction
In Taiwan, lung cancer is the leading cause of cancer-related deaths and among both men and women over the last decade. 5884 males and 3348 females died of lung cancer in 2015, accounting for the most common cancer-related mortality rate among 10 most common cancers according to the Taiwan Cancer Registry annual report.
The National Lung Screening Trial (NLST) demonstrated that lung cancer screening using low dose computed tomography (LDCT) resulted in a significant reduction in lung cancer-specific overall mortality rate in comparison with chest radiography in high-risk heavy smokers1. Around 70~80% of patients with lung cancer diagnosed have stage III or IV disease at presentation in Taiwan, which generally lead to poor prognosis with the high mortality rate2. Therefore it is crucial that screening and diagnosis of lung cancer at early stage because when found early, lung cancer is highly curable3.
Previous studies have demonstrated that family history and gender are two important factors associated with non-smoking related lung cancer4,5. In addition, the average PM2.5 levels in Taiwan were much higher than the levels in European cities according to the European Study of Cohorts for Air pollution Effects (ESCAPE), especially in Kaohsiung city6. Therefore, genetic factors and environmental pollution may play an important role in the development of non-smoking related lung cancer. Therefore, the LDCT screening selection criteria should be modified due to regional genetic and environmental differences. In Kaohsiung Veterans General Hospital (Kaohsiung, Taiwan), self-paid LDCT for lung cancer screening has been conducted for population-based mass screening aged 40~80 years since 2007 in a population with the high prevalence of non-smoking-related lung cancer4,7. However, all screening programs involve the trade-offs between potential benefits and potential harms. There are still many unresolved problems about the benefits, harms and the cost of the mass screening, included light smokers and non-smokers8,9,10,11.
Thus, the aim of this retrospective cohort study was to a comparison of screened and non-screened lung cancer in terms of lung cancer characteristics, overdiagnosis and survival rate.
Materials and Methods
Between January 2007 and September 2017, 2883 patients were diagnosed with lung cancer at Kaohsiung Veterans General Hospital. The focus in this present study is on clinical characteristics and outcomes of lung cancer between screened and non-screening patient groups. The institutional review board approved this retrospective study, and thus informed consent was waived. All research was performed in accordance with the relevant guidelines and regulations and all Institutional Review Board requirements.
Definition of screened and non-screened lung cancer
Patients were classified two groups: Group 1 (screened group): patients who had no clinical symptoms and incidentally detected lung cancers by self-paid LDCT exam aged 40–80 years. Group 2 (non-screened group): patients with the clinical scenario of lung cancer-related symptoms or abnormal finding (highly suspicion of lung cancer) in the chest radiograph were further diagnosed as lung cancer. Patients were assigned to screened and non-screened subgroups based on the stringent definition. Our database included the following clinical characters: age, sex, tumor size, histopathologic type, adenocarcinoma spectrum classification, lung cancer clinical stage, death, survival time, mortality rate, smoking habit, betel nut and alcohol drinking habit. The histological diagnosis was described according to the World Health Organization classification. All the patients were staged according to the 7th edition of the TNM staging system published in 200912. Data regarding curative surgical treatment and targeted therapy use were also recorded.
Statistics
All statistical analyses were performed with SPSS 17.0 for Windows (SPSS Inc, Chicago, IL), STATA 13.0 package (StataCorp, College Station, TX, USA) and MedCalc 13.2.2.0 (MedCalc Software, Ostend, Belgium). Differences in continuous variables between 2 groups were compared by the independent Student t test. Categorical variables were summarized as frequencies and percentages and compared using the chi-square test to examine differences in demographic characteristics. Fisher’s exact test was used to analyze when the smallest expected value is less than 5. Overall survival time was defined as the period from the date of lung cancer diagnosed until the date of death from any cause or until the date of the last follow-up at which point the data were censored. Overall survival was estimated using the Kaplan-Meier method. A log rank test was used to compare prognosis between screened and non-screening groups. Cox regression analysis was performed to calculate and compare the survival rate. A multivariate analysis was used to estimate the hazard ratios (HRs) based on the Cox regression model, adjusted for age, gender, smoking, alcohol, betel nut, tumor size, curative surgery, target therapy, histology and screened or not. A p value of 0.05 was regarded as significant.
Ethics approval
The study protocol was approved by the Institutional Review Board of Kaohsiung Veterans General Hospital (VGHKS19-CT2–09). The need for informed consent was waived by the institutional review board due to the minimal risk retrospective study.
Results
Baseline characteristics
During the study period, 2883 lung cancer patients were analyzed according to the hospital-based cancer registry dataset. The screened group consisted of 93 subjects, and the non-screened group consisted of 2790 subjects. The general characteristics of the lung cancer subjects between the two groups are summarized in Table 1.
The mean age in the screened group was significantly younger than that in the non-screened group (59.91 ± 8.14 years old versus 67.58 ± 12.95 years old, p < 0.0001; median age 60 years-old versus 69 years-old). The screened patients had a significantly greater proportion of female gender than the non-screened group (61.3% versus 36.8%; p < 0.0001). Patients in the non-screening group had the significantly higher proportion of smoking habit (p < 0.0001), surgery (p = 0.0001) and target therapy (p = 0.001) than the screened group. There were no significant differences between the two groups in terms of alcohol drinking and betel nut habits. For survival interval analysis, the mean survival date in the screened group was significantly higher than that in the non-screened group (860.31 ± 502.20 versus 574.94 ± 558.48 days; median survival days 793 versus 404, p < 0.0001).
Comparison of histopathology and clinical lung cancer stage distribution
The comparison of the difference in histopathology and clinical lung cancer stage distribution between the two groups are summarized in Table 1. A significant difference in stage at diagnosis was seen between screened and non-screened groups.
Stage I was the most frequent stage in the patients with screened group. In comparison, patient in the non-screened group presented with stage IV in most cases.
For carcinoma in situ, the screened patients had a significantly greater proportion of carcinoma in situ than the non-screened group (15% vs. 0.14%; p < 0.0001).
For lung cancer histopathology distribution, a significant difference in histopathology distribution was seen between screened and non-screened groups. With regard to histological subtype, adenocarcinoma was significantly more prevalent in the patients with screened group (94.62% vs. 72.15%; p < 0.0001). In contrast to that, the subjects with non-screened group have a significantly greater proportion of the patients with small cell carcinoma (15.91% vs. 3.22%; p < 0.0001) and squamous cell carcinoma (9.20% vs. 1.07%; p < 0.0001). With regard to histological subtype of adenocarcinoma spectrum, a significant difference in histological subtype of adenocarcinoma spectrum was seen between the screened and non-screened groups. Invasive pulmonary adenocarcinoma was the most frequent histological subtype in the patients with non-screened group. In comparison, the patients in screened group presented with higher portion of minimally invasive adenocarcinoma, adenocarcinoma in situ or its precursor lesions.
Table 2 summarizes the mortality and survival analysis according to screened and non-screened groups in term of overall, 1-year and 5-year mortality rates.
Patients in the screened group had a lower overall mortality than that in the non-screened group. One-, and Five-year mortality rates increased significantly from the screened group to the non-screened group (P < 0.0001 for all). The mean survival time for the screened group was 860.31 ± 502.20 days (median 793 days), and the mean survival for the non-screened group was 574.94 ± 558.48 days (median 404 days). After exclusion of AAH or AAH/AIS patients, the screened group still showed significantly better outcomes in overall mortality than the non-screened group shown in Supplement Tables 1 and 2.
Association of clinical prognostic variables with survival
Survival analysis for lung cancer using Cox regression model for multivariate effects, the hazard ratio for lung cancer mortality was determined adjusting for age, gender, smoking, alcohol, betel nut and screened status (Table 3). Multivariate survival analysis using Cox’s regression model showed age (HR = 1.017, P = 0.001), gender (HR = 0.824, P = 0.0001), smoking status (HR = 1.281, P = 0.0001), screened status (HR = 0.329, P = 0.0001), target therapy (HR = 1.009, P = 0.0001), curative surgery (HR = 0.348, P = 0.0001), Tumor size (HR = 1.000304, P = 0.009), and histologic type (HR = 0.790, P = 0.0001) were as identified independent prognostic factors of overall survival for lung cancer patients shown in Table 3. Survival times were determined as of May 2018. During this period, 2206 patients (79.1%) died, and 584 patients (20.9%) were censored in the non-screened group. In addition, 10 patients (10.8%) died, and 83 patients (89.2%) were censored in the screened group. Comparing survival curves of two groups using the log rank test, survival was significantly superior in the patients with screened group compared with the patients in non-screened group shown in Fig. 1 (P = 0.0001).
Discussion
The focus of the present study is to compare between screened and non-screened lung cancer in terms of lung cancer characteristics, overdiagnosis and survival rate. In this study, we demonstrated four major findings. The first one is that we observed that adenocarcinoma was significantly more frequent in patients in the screened group. The second finding is that stage I was significantly more frequent in patients in the screened group. Third, favorable overall survival was significantly superior in the screened group and lead to a reduction of 68.31% compared with non-screened group.
Fourth, there was an obvious increase of carcinoma in situ lesions in the screened group and lead to an increase of 14.86% compared with the non-screened group in regard to overdiagnosis.
In 2011, the NLST reported a reduction in lung cancer mortality of 20% in subjects who underwent annual LDCT exam compared with annual chest x-ray exam during the time period of 5 years1. In this present study, we found a significant decrease in the overall mortality rate of 68.31% in the screened group compared with the non-screened group. Our present result is similar to the findings of this previous study1. Further, in accordance with our results, lung cancer subjects in the screened group also had smaller primary tumor size and lower clinical stage at the time of initial diagnosis. These finding were associated with the lower mortality rate, longer survival periods, and an increased surgical treatment rate. However, there are also a number of important differences between the NLST population and our screened group. Our screening population found a higher proportion of non-smoking women with lung cancer diagnosed. These findings also support that there appears to be an increasing trend of non-smokers related lung cancer in Asian population such as China, Japan, Korea and Taiwan in recent years4,7. Currently most of the society recommends that lung cancer screening targeted in adults age 55 to 80 year who have a 30 pack-year smoking history and currently smoke or have quitted within the past 15 years11,13,14.
The present results also support previous studies concerning broadly expanding inclusion criteria to include never-smokers in lung cancer screening program in Asian population with the high prevalence of non-smoking related lung cancer4,5,7,8,15. Recent research has demonstrated that lung cancer screening using LDCT resulted in a 43% decrease in all-cause death in comparison with chest radiography in a population-based cohort including non-smoker and light smoker in Hitachi city, Japan15,16. Therefore, the effectiveness of lung cancer screening program specifically targeting at non-smoking Asian population with the high prevalence of non-smoking related lung cancer should be further investigated.
The issue of overdiagnosis and overmanagement
In this study, we assessed the factors affecting the prognosis of lung cancer between the screened and non-screened groups. In the multivariable Cox regression model, lung cancer in the screened group is the most important factor responsible for improved survival prognosis. Therefore, it is crucial that widely implementation of LDCT lung cancer screening program in Asian population including non-smoker and light smoker based on the lung cancer risk prediction model. However, overdiagnosis is always an important concern in cancer screening because it potentially leads to overtreatment and potential harmful treatments17,18. In this study, we attempted to estimate the proportion of carcinoma in situ or the proportion of early adenocarcinoma spectrum lesions to assess the extent of overdiagnosis. For carcinoma in situ, the screened patients had a significantly greater proportion of carcinoma in situ than the non-screened group (15% vs. 0.14% p < 0.0001). For adenocarcinoma lesions, the screened patients had a significantly greater proportion of precursor lesions of adenocarcinoma spectrum (including AAH, AIS, and MIA) than the non-screened group (23.65% vs. 0.19% p < 0.0001). To estimate the percentage of overdiagnosis in NLST trial, Patz et al. estimated that more than 18% of all lung cancers detected by LDCT in the NLST seem to be indolent17. Our findings also support the same results.
There is even a more obvious trend because of the higher prevalence of non-smoking lung adenocarcinoma spectrum lesions in Asia4,7,19,20. Recent evidences have demonstrated that a strong correlation between radiologic features and adenocarcinoma spectrum lesions21,22. In addition to the rapid development of computer image processing and radiomics technology, recent studies have also demonstrated that use of CT radiomic texture analysis such as tumor size, morphology, attenuation, entropy and volumetric doubling time analysis could facilitate more accurate differentiation between pre-invasive lesions and invasive pulmonary adenocarcinomas23,24,25,26,27,28,29. Our previous studies also have shown that novel subclassification of subsolid nodules has the high positive predictive value to rule in invasive pulmonary adenocarcinoma, which manifesting as part-solid nodules23,24. Incorporation of these CT radiomic features can help further refine the management of subsolid nodules in the Asian lung cancer screening program with the high prevalence of non-smoking related lung cancer4,7,30. The goal of lung cancer screening program is to reduce mortality rate from lung cancer death and avoid overdiagnosis/overmangement. Thus, we should always be aware of overdiagnosis as a counterpart of lung cancer screening program in Asia. Because of more indolent growth for preinvasive lesions which manifesting as pure groundglass nodules, the combination strategies of shared decision making and watchful waiting with annual or biannual follow-up for a period of at least 5 years a would be a safe option to allow early detection of disease progression and to avoid the potential harms of overdiagnosis and overtreatment25,31,32. These strategies could improve the efficacy of lung cancer screening programs in Asian populations with the high prevalence of non–smoking-related lung cancer7,25.
Strength and limitations
The main strength of this study is the hospital-based lung cancer registry database, which mainly reflect the entire lung cancer population in a hospital-based cohort. Therefore, the large hospital-based cohort could result in sufficient power to detect small differences in patient outcomes and prognosis. Several previous studies investigated the difference between screened and symptomatic group for surgically diagnosed lung cancer subjects, which can’t represent the entire distribution of lung cancer in the population33,34.
This study also has its limitations. First, this study is a retrospective cohort study design. Therefore, the retrospective aspect may introduce selection bias and information bias, which could bias this study’s results. Second, it is uncertain that the current study results could be widely generalized to other hospitals in Asia. Thus further large multicenter studies are needed to investigate the effect of implementation of mass lung cancer screening program at target-risk population based on lung cancer-risk prediction model to establish the generalizability in Asia9,30.
Conclusions
In summary, a very high proportion of non-smoking related lung adenocarcinoma is detected at the early stage in patient underwent mass lung cancer screening program, which lead to significantly improved survival outcome. These results suggest that broadly expanding inclusion criteria to include never-smokers in lung cancer screening program in Asian population may be crucial in reducing mortality rate and improving survival outcome. To maximize the cost-effectiveness and health benefits of LDCT screening and reduce the potential risk in over-diagnosis and over-management among non-smokers, further prospective-cohort studies should address the effectiveness of implementation of LDCT lung cancer screening program targeting at high-risk population based on lung cancer prediction risk model.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Change history
16 September 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41598-021-98096-4
References
National Lung Screening Trial Research, T. et al. Reduced lung-cancer mortality with low-dose computed tomographic screening. The New England journal of medicine 365, 395–409, https://doi.org/10.1056/NEJMoa1102873 (2011).
Wang, B.-Y. et al. Lung Cancer and Prognosis in Taiwan: A Population-Based Cancer Registry. Journal of Thoracic Oncology 8, 1128–1135, https://doi.org/10.1097/JTO.0b013e31829ceba4 (2013).
Shieh, Y., Bohnenkamp, M. & Low-Dose, C. T. Scan for Lung Cancer Screening: Clinical and Coding Considerations. CHEST 152, 204–209, https://doi.org/10.1016/j.chest.2017.03.019 (2017).
Wu, F.-Z. et al. Assessment of Selection Criteria for Low-Dose Lung Screening CT Among Asian Ethnic Groups in Taiwan: From Mass Screening to Specific Risk-Based Screening for Non-Smoker Lung Cancer. Clinical Lung Cancer 17, e45–e56, https://doi.org/10.1016/j.cllc.2016.03.004 (2016).
Lin, K.-F. et al. Propensity score analysis of lung cancer risk in a population with high prevalence of non-smoking related lung cancer. BMC pulmonary medicine 17, 120–120, https://doi.org/10.1186/s12890-017-0465-8 (2017).
Tseng, C.-H. et al. The Relationship Between Air Pollution and Lung Cancer in Nonsmokers in Taiwan. Journal of Thoracic Oncology 14, 784–792, https://doi.org/10.1016/j.jtho.2018.12.033 (2019).
Hsu, H.-T. et al. Modified Lung-RADS Improves Performance of Screening LDCT in a Population with High Prevalence of Non–smoking-related Lung Cancer. Academic Radiology 25, 1240–1251, https://doi.org/10.1016/j.acra.2018.01.012 (2018).
Naidich, D. P. Low Dose Lung CT Screening in an Asian Population. Academic Radiology 25, 1237–1239, https://doi.org/10.1016/j.acra.2018.06.002 (2018).
Kumar, V. et al. Risk-targeted lung cancer screening: A cost-effectiveness analysis. Annals of Internal Medicine 168, 161–169, https://doi.org/10.7326/M17-1401 (2018).
Ruano-Ravina, A., Perez-Rios, M., Casan-Clara, P. & Provencio-Pulla, M. Low-dose CT for lung cancer screening. The Lancet. Oncology 19, e131–e132, https://doi.org/10.1016/s1470-2045(18)30121-9 (2018).
Fintelmann, F. J. et al. The 10 Pillars of Lung Cancer Screening: Rationale and Logistics of a Lung Cancer Screening Program. RadioGraphics 35, 1893–1908, https://doi.org/10.1148/rg.2015150079 (2015).
UyBico, S. J. et al. Lung Cancer Staging Essentials: The New TNM Staging System and Potential Imaging Pitfalls. RadioGraphics 30, 1163–1181, https://doi.org/10.1148/rg.305095166 (2010).
Wender, R. et al. American Cancer Society lung cancer screening guidelines. CA: a cancer journal for clinicians 63, 107–117, https://doi.org/10.3322/caac.21172 (2013).
O’Dowd, E. L. & Baldwin, D. R. Lung cancer screening—low dose CT for lung cancer screening: recent trial results and next steps. The British Journal of Radiology 91, 20170460, https://doi.org/10.1259/bjr.20170460 (2017).
Nawa, T. et al. A population-based cohort study to evaluate the effectiveness of lung cancer screening using low-dose CT in Hitachi city, Japan. Japanese Journal of Clinical Oncology, hyy185–hyy185, https://doi.org/10.1093/jjco/hyy185 (2018).
Nawa, T. et al. A decrease in lung cancer mortality following the introduction of low-dose chest CT screening in Hitachi, Japan. Lung Cancer 78, 225–228, https://doi.org/10.1016/j.lungcan.2012.09.012 (2012).
Patz, E. F. Jr. et al. Overdiagnosis in low-dose computed tomography screening for lung cancer. JAMA internal medicine 174, 269–274, https://doi.org/10.1001/jamainternmed.2013.12738 (2014).
Mortani Barbosa, E. J. Jr. Lung Cancer Screening Overdiagnosis: Reports of Overdiagnosis in Screening for Lung Cancer Are Grossly Exaggerated. Academic Radiology 22, 976–982, https://doi.org/10.1016/j.acra.2014.10.011 (2015).
Detterbeck, F. C. et al. The IASLC Lung Cancer Staging Project: Summary of Proposals for Revisions of the Classification of Lung Cancers with Multiple Pulmonary Sites of Involvement in the Forthcoming Eighth Edition of the TNM Classification. Journal of Thoracic Oncology 11, 639–650, https://doi.org/10.1016/j.jtho.2016.01.024 (2016).
Travis, W. D. et al. The IASLC Lung Cancer Staging Project: Proposals for Coding T Categories for Subsolid Nodules and Assessment of Tumor Size in Part-Solid Tumors in the Forthcoming Eighth Edition of the TNM Classification of Lung Cancer. Journal of Thoracic Oncology 11, 1204–1223, https://doi.org/10.1016/j.jtho.2016.03.025 (2016).
Austin, J. H. M. et al. Radiologic Implications of the 2011 Classification of Adenocarcinoma of the Lung. Radiology 266, 62–71, https://doi.org/10.1148/radiol.12120240 (2013).
Cohen, J. G. et al. Lung adenocarcinomas: correlation of computed tomography and pathology findings. Diagnostic and Interventional Imaging 97, 955–963, https://doi.org/10.1016/j.diii.2016.06.021 (2016).
Wu, F.-Z. et al. Semiquantative Visual Assessment of Sub-solid Pulmonary Nodules ≦3 cm in Differentiation of Lung Adenocarcinoma Spectrum. Scientific Reports 7, 15790, https://doi.org/10.1038/s41598-017-16042-9 (2017).
Chen, P. A. et al. Qualitative CT Criterion for Subsolid Nodule Subclassification: Improving Interobserver Agreement and Pathologic Correlation in the Adenocarcinoma Spectrum. Academic Radiology 25, 1439–1445, https://doi.org/10.1016/j.acra.2018.01.011 (2018).
Tang, E.-K. et al. Natural History of Persistent Pulmonary Subsolid Nodules: Long-Term Observation of Different Interval Growth. Heart, Lung and Circulation, https://doi.org/10.1016/j.hlc.2018.08.015.
Son, J. Y. et al. Quantitative CT analysis of pulmonary ground-glass opacity nodules for the distinction of invasive adenocarcinoma from pre-invasive or minimally invasive adenocarcinoma. PloS one 9, e104066–e104066, https://doi.org/10.1371/journal.pone.0104066 (2014).
Hwang, I. P. et al. Persistent Pure Ground-Glass Nodules Larger Than 5 mm: Differentiation of Invasive Pulmonary Adenocarcinomas From Preinvasive Lesions or Minimally Invasive Adenocarcinomas Using Texture Analysis. Investigative radiology 50, 798–804, https://doi.org/10.1097/rli.0000000000000186 (2015).
Lee, S. M. et al. Invasive Pulmonary Adenocarcinomas versus Preinvasive Lesions Appearing as Ground-Glass Nodules: Differentiation by Using CT Features. Radiology 268, 265–273, https://doi.org/10.1148/radiol.13120949 (2013).
Li, W. et al. Radiomic analysis of pulmonary ground-glass opacity nodules for distinction of preinvasive lesions, invasive pulmonary adenocarcinoma and minimally invasive adenocarcinoma based on quantitative texture analysis of CT. Chinese journal of cancer research = Chung-kuo yen cheng yen chiu 30, 415–424, https://doi.org/10.21147/j.issn.1000-9604.2018.04.04 (2018).
Wu, F.-Z., Kuo, P.-L., Wu, C. C. & Wu, M.-T. The impact of patients’ preferences on the decision of low-dose computed tomography lung cancer screening. Translational lung cancer research 7, S236–S238, https://doi.org/10.21037/tlcr.2018.08.17 (2018).
MacMahon, H. et al. Guidelines for Management of Incidental Pulmonary Nodules Detected on CT Images: From the Fleischner Society 2017. Radiology 284, 228–243, https://doi.org/10.1148/radiol.2017161659 (2017).
Kakinuma, R. et al. Natural History of Pulmonary Subsolid Nodules: A Prospective Multicenter Study. Journal of Thoracic Oncology 11, 1012–1028, https://doi.org/10.1016/j.jtho.2016.04.006 (2016).
Quadrelli, S., Lyons, G., Colt, H., Chimondeguy, D. & Buero, A. Clinical characteristics and prognosis of incidentally detected lung cancers. International journal of surgical oncology 2015, 287604–287604, https://doi.org/10.1155/2015/287604 (2015).
Raz, D. J., Glidden, D. V., Odisho, A. Y. & Jablons, D. M. Clinical Characteristics and Survival of Patients with Surgically Resected, Incidentally Detected Lung Cancer. Journal of Thoracic Oncology 2, 125–130, doi:10.1097/JTO.0b013e31802f1cb1 (2007).
Acknowledgements
This study is based in part on data from the Cancer Registry Database provided by the Cancer Center of Kaohsiung Veterans General Hospital. The authors thank all doctors who responded to our screening and investigation. This study was supported by Grants from Kaohsiung Veterans General Hospital, VGHKS103-015, VGHKS104-048, VGHKS105-064, VGHKS108-159, MOST108-2314-B-075B-008-, Taiwan, R.O.C.
Author information
Authors and Affiliations
Contributions
F.Z.W. and Y.P.L. prepared the manuscript. P.L.K. and F.Z.W. participated in designing the study and performed the statistical analysis. Y.L.H., E.K.T., M.T.W. and C.S.C. provided coordination and helped to design the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this Article was revised: In the original version of this Article, Fu-Zong Wu was incorrectly listed as a corresponding author. The correct corresponding author for this Article is only Yun-Pei Lin. Correspondence and request for materials should be addressed to fc760203@gmail.com.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, FZ., Kuo, PL., Huang, YL. et al. Differences in lung cancer characteristics and mortality rate between screened and non-screened cohorts. Sci Rep 9, 19386 (2019). https://doi.org/10.1038/s41598-019-56025-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-56025-6
- Springer Nature Limited
This article is cited by
-
Immune checkpoint inhibitor-associated new-onset hypophysitis: a retrospective analysis using the FAERS
Endocrine (2024)
-
A comparative study to evaluate CT-based semantic and radiomic features in preoperative diagnosis of invasive pulmonary adenocarcinomas manifesting as subsolid nodules
Scientific Reports (2021)
-
Association of cancer screening and residing in a coal-polluted East Asian region with overall survival of lung cancer patients: a retrospective cohort study
Scientific Reports (2020)