Abstract
Reactive metabolites of anti-tuberculosis (anti-TB) drugs can result in excessive reactive oxygen species (ROS), which are responsible for drug-induced liver injury. The nuclear factor erythroid 2-related factor 2 (Nrf2) - antioxidant response elements (ARE) (Nrf2-ARE) signaling pathway plays a crucial role in protecting liver cells from ROS, inducing enzymes such as phase II metabolizing enzymes and antioxidant enzymes. Based on a Chinese anti-TB treatment cohort, a nested case-control study was performed to explore the association between 13 tag single-nucleotide polymorphisms (tagSNPs) in the NRF2, KEAP1, MAFF, MAFK genes in Nrf2-ARE signaling pathway and the risk of anti-TB drug-induced liver injury (ATLI) in 314 cases and 628 controls. Conditional logistic regression models were used to calculate odds ratios (ORs) and 95% confidence intervals (CIs) after adjusting weight and usage of hepatoprotectant. Patients carrying the TC genotype at rs4243387 or haplotype C-C (rs2001350-rs6726395) in NRF2 were at an increased risk of ATLI (adjusted OR = 1.362, 95% CI: 1.017–1.824, P = 0.038; adjusted OR = 2.503, 95% CI: 1.273–4.921, P = 0.008, respectively), whereas patients carrying TC genotype at rs2267373 or haplotype C-G-C (rs2267373-rs4444637-rs4821767) in MAFF were at a reduced risk of ATLI (adjusted OR = 0.712, 95% CI: 0.532–0.953, P = 0.022; adjusted OR = 0.753, 95% CI: 0.587–0.965, P = 0.025, respectively). Subgroup analysis also detected a significant association between multiple tagSNPs (rs4821767 and rs4444637 in MAFF, rs4720833 in MAFK) and specific clinical patterns of liver injury under different genetic models. This study shows that genetic polymorphisms of NRF2, MAFF and MAFK may contribute to the susceptibility to ATLI in the Chinese anti-TB treatment population.
Similar content being viewed by others
Introduction
Tuberculosis (TB) has existed throughout human history and remains a serious public health conce1. In 2017, an estimated 10.0 million people fell ill with TB and about 1.3 million patients died1. The Directly Observed Treatment Short-course (DOTS), an international recommendation strategy, remains the cornerstone of TB control in developing countries. TB can be treated by taking several anti-TB drugs for a minimum of 6 months: daily oral doses with a combination of rifampicin (RIF/R), isoniazid (INH/H), pyrazinamide (PZA/Z), and ethambutol (EMB/E) for 2 months, followed by 4 months of RIF and INH2. However, many studies have shown that utilization of multidrug regimens can cause unbearable adverse drug reactions (ADRs), such as gastrointestinal disorders, hepatotoxicity, allergic reactions, arthralgia, neurological disorders and so on3. These ADRs lead to non-adherence and treatment interruption, and they contribute to eventual treatment failure, relapse or the emergence of drug-resistance4. Among these ADRs, the most serious adverse reaction is anti-TB drug-induced liver injury (ATLI), which is often fatal5.
The pathophysiology of ATLI is still unclear5. However, most studies show that the development of ATLI is a complicated process related to drug, host and genetic susceptibility6. The experimental and clinical research indicates that reactive metabolites, rather than direct toxicity of the anti-TB drugs, are responsible for ATLI7, which occurs when these metabolites irreversibly bind to and modify many cellular components, particularly enzymes, and induce the production of excessive reactive oxygen species (ROS)6,8. Furthermore, ROS induce lipid peroxidation and cell death6. For example, recent research showed ROS accumulation and apoptosis could be induced by INH in HepG2 as well as THLE-2 cells9. Oxidative stress and beyond may contribute to the hepatic toxicity induced by first-line anti-TB drugs10. Liver cells can neutralize the extra ROS by antioxidant activities involving a variety of non-enzymatic and enzymatic mechanisms, such as glutathione S-transferases, NAD(P)H: quinone oxidoreductase, and glutamate-cysteine ligase11,12. Zhang et al. observed that the level of antioxidant enzymes and non-enzymatic antioxidants (superoxide dismutase, total antioxidant capacity, glutathione and malondialdehyde (MDA)) were changed in PZA-treated Wistar rats13. Additionally, in young rats, INH-RIF can directly increase ROS and consume glutathione, damaging the hepatic cell14. In a population-based study, the activity of glutathione was reduced and the level of MDA was increased in an ATLI group15. All these studies suggest that the accumulation of ROS in the liver is a potential mechanism of drug-induced liver injury16. Numerous mammalian studies have shown that the nuclear factor erythroid 2-related factor 2 (Nrf2) signaling molecules, activated by ROS, play an important role in transcriptional activation of downstream genes such as antioxidant and detoxification genes17.
Nrf2, a transcription factor that resists oxidative stress, belongs to the Cap-n-collar (CNC) basic leucine zipper family18. Under normal conditions, Nrf2 combines with kelch-like ECH associating protein 1 (Keap1) in the cytosol, which results in the activity of Nrf2 being temporarily inhibited. Upon exposure to oxidative stress or electrophilic, Nrf2 is released from Keap1 translocates to the nucleus, where it heterodimerizes with one of the small musculoaponeurotic fibrosarcoma (sMaf) proteins17. The highly homologous sMafs, MafF, MafK and MafG, are localized predominantly in the nucleus and previous studies have linked their functions, by virtue of their heterodimerization with the CNC family of transcription factors, to the stress response and detoxification pathways19. Heterodimers of Nrf2 and sMaf bind to antioxidant response elements (AREs) that boost the expression and transcription of phase II metabolizing enzymes and antioxidant proteins20. So, liver tissue can scavenge ROS by phase II metabolizing enzymes and antioxidant enzymes to keep oxidation and antioxidant balance, and the expression of these enzymes is mediated by the Nrf2-ARE signaling pathway.
In the Nrf2-ARE signaling pathway, it is the first and the crucial step that Nrf2 detaches from Keap1 in cytoplasm, moves to heterodimerizes with sMaf in nucleus. This process involves translocation of some relevant genes, such as NRF2, KEAP1, MAFF, MAFK and MAFG gene. It is reasonable to speculate that genetic variation in these genes may affect signal transduction during oxidative stress, resulting in ROS not being cleared in a timely fashion. So, in present study, we hypothesized that the genetic polymorphisms in the Nrf2-ARE signaling pathway may play an important role in susceptibility to ATLI. To test this hypothesis, 13 tag single-nucleotide polymorphisms (tagSNPs) in NRF2, KEAP1, MAFF, MAFK genes were analyzed to determine the role of tagSNPs in Chinese ATLI patients.
Results
Demographical and clinical data
Between April 2014 and December 2016, 3046 newly diagnosed TB patients were initially identified from hospitals, and 2209 patients finished the anti-TB treatment. A total of 314 ATLI cases and 628 non-ATLI controls was included in present study from the cohort. Among the 314 ATLI cases, 150 patients (47.8%) had a hepatocellular type; 23 patients (7.3%) had a cholestatic type, and 40 patients (12.7%) had a mixed type of liver injury, with the rest of 101 cases classified as unclear type due to lack of test results of alkaline phosphatase (ALP). The distribution of basic characteristics between ATLI cases and non-ATLI controls are summarized in Table 1 (The basic characteristics in Table 1 has been reported in our previous study)21. We used 1:2 individual matching of case: control, and there was no significant difference in age, sex and treatment history, disease severity and drug dosage between the two groups. Before anti-TB treatment, all patients’ liver biochemical parameters were in the normal range and there was no significant difference between the two groups (P > 0.05). However, during the treatment period, the peak serum alanine transaminase (ALT), aspartate aminotransaminase (AST) and total bilirubin levels were significantly higher in the ATLI group than in the controls (P < 0.001).
Genotype analysis
No significant deviations from the Hardy-Weinberg equilibrium (HWE) in the distributions of genotypes and alleles were observed for the eleven tagSNPs among the control group [rs2886161, χ2 = 1.904, P = 0.168; rs4243387, χ2 = 0.479, P = 0.489; rs6726395, χ2 = 2.868, P = 0.090; rs1962142, χ2 = 0.002, P = 0.960; rs2001350, χ2 = 1.354, P = 0.245; rs1048290, χ2 = 2.064, P = 0.151; rs2267373, χ2 = 0.450, P = 0.502; rs4444637, χ2 = 1.456, P = 0.228; rs4821767, χ2 = 0.129, P = 0.720; rs4720833, χ2 = 0.289, P = 0.591 and rs3808337, χ2 = 0.362, P = 0.548], but not in the remaining two tagSNPs (rs11545829 and rs4608623) (Table 2).
The genotype distributions of thirteen tagSNPs between ATLI cases and controls are shown in Table 3. Patients carrying TC genotype at rs4243387 in NRF2 were at a higher risk of liver injury than with TT genotype (adjusted OR = 1.362, 95% CI: 1.017–1.824, P = 0.038). However, patients carrying TC genotype at rs2267373 in MAFF were at a lower risk of liver injury than with TT genotype (adjusted OR = 0.712, 95% CI: 0.532–0.953, P = 0.022), and these statistically significant differences were also found using a dominant model (P = 0.014) and an additive model (P = 0.022).
Haplotype analysis
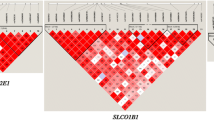
Five potential linkage disequilibrium (LD) blocks were constructed based on the r-square value and log-odds score (Fig. 1), and statistical analysis results indicated that patients carrying haplotype C-C in block 4 (rs2001350–rs6726395, in NRF2) had a higher risk of liver injury (adjusted OR = 2.503, 95% CI: 1.273–4.921, P = 0.008), and patients carrying haplotype C-G-C in block 3 (rs2267373-rs4444637-rs4821767, in MAFF) had a lower risk of liver injury (adjusted OR = 0.753, 95% CI: 0.587–0.965, P = 0.025) (Table 4).
Linkage disequilibrium (LD) block constructed from 13 tagSNPs in NRF2, KEAP1, MAFF and MAFK. This LD plot was generated with the Haploview 4.2 software. Markers with LD (D′ < 1 and LOD > 2) are shown in red through pink (color intensity decreases with decreasing D′ value). D′ value shown within each square represents a pairwise LD relationship between the two polymorphisms.
Subgroup analysis
The association between tagSNPs and ATLI among different clinical patterns of liver injury are shown in Supplementary Tables 1, 2, 3 and 4. Patients carrying polymorphisms of rs4444637 in MAFF had a reduced risk of hepatocellular liver injury (dominant model, adjusted OR = 0.601, 95% CI: 0.363–0.994, P = 0.047), and a similar relationship existed between polymorphisms of rs4821767 in MAFF and cholestatic liver injury (dominant model, adjusted OR = 0.250, 95% CI: 0.074–0.841, P = 0.025; additive model, adjusted OR = 0.353, 95% CI: 0.142–0.878, P = 0.025). However, patients carrying polymorphisms of rs4720833 in MAFK had an increased risk of mixed liver injury (recessive model, adjusted OR = 4.127, 95% CI: 1.054–16.16, P = 0.042; additive model, adjusted OR = 2.000, 95% CI: 1.096–3.650, P = 0.024) (Table 5).
Discussion
In present study, the role of 13 tagSNPs in NRF2, KEAP1, MAFF and MAFK in the Nrf2-ARE signaling pathway were examined among Chinese anti-TB treatment patients. Two single variants, namely, the TC genotype at rs4243387 in NRF2 and TC genotype at rs2267373 in MAFF, together with two haplotypes of C-C (rs2001350-rs6726395, in NRF2) and C-G-C (rs2267373-rs4444637-rs4821767, in MAFF), were identified as being associated with ATLI development. To our knowledge, there has been only one study conducted in Japanese to explore the relationship of the genetic polymorphisms in the oxidative stress signaling pathway and the occurrence of ATLI22. In that study, Nanashima et al. performed a candidate gene-based association study between thirty-four tagSNPs in 10 genes in the antioxidant pathway and ATLI susceptibility with 18 ATLI patients and 82 controls22. The results revealed that a CC genotype at rs11080344 in nitric oxide synthase 2A (NOS2A), a CC genotype at rs2070401 in BTB domain and CNC homologue 1 (BACH1), and a GA or AA genotype at rs4720833 in MAFK independently conferred ATLI susceptibility22. Together with the Japanese study, the present study further confirms the role of related genetic polymorphisms of the Nrf2-ARE signaling pathway in ATLI.
Nrf2 is a central regulator which mediates antioxidant gene expression23, and a potential target to prevent or cure drug-induced liver injury24. Our study suggested that a TC genotype at rs4243387 in NRF2 is associated with increased risk of ATLI (Adjusted OR = 1.362, 95% CI: 1.017–1.824, P = 0.038). A previous functional study of polymorphisms in NRF2 indicated that genetic variants would lead to a significant reduction of NRF2 gene expression and a less efficient binding of Nrf2 to ARE, and increase the risk of acute lung injury25. However, the same variant was not found to be statistically significant in the Japanese study, which may be related to the low sample size22. The sMafs are crucial regulators of mammalian gene expression that are essential for DNA binding of Nrf2 and other processes, including the localization and stabilization of Nrf219,26. Our study indicated that TC genotype at rs2267373 in MAFF was associated with reduced risk of ATLI (Adjusted OR = 0.712, 95% CI: 0.532–0.953, P = 0.022); significant differences were also found using a dominant model (P = 0.014) and an additive model (P = 0.022). Other two tagSNPs (rs4821767 and rs4444637) in MAFF were also associated with reduced risk of specific clinical types of liver injury under different genetic models. However, the function of tagSNPs rs2267373, rs4821767 and rs4444637 in intron 1 of MAFF remains unknown. We performed bioinformatics analysis of three tagSNPs in MAFF using online database (HaploReg v4.1)27, and the result indicated that rs2267373, rs4821767 and rs4444637 contained H3K4me1 and H3K27ac in liver tissue, and appear to change known motifs. H3K4me1 and H3K27ac are the predominant histone modification found in nucleosomes around enhancer element, and associated with transcriptional regulation of genes28. Perhaps the variants in MAFF could regulate the expression of MAFF. Higher expression of MAFF facilitates it binding to Nrf2, leading to increased expression of subsequent antioxidant enzymes and reducing the occurrence of ATLI26. The role of these genetic variations in ATLI needs further research.
Although both the present study and Japanese study revealed that genetic polymorphisms in Nrf2-ARE signaling pathway may contribute to the susceptibility to ATLI, there are some difference between two studies. Our study indicated that tagSNP rs2267373 in MAFF was associated with a reduced susceptibility to ATLI (Dominant model, Adjusted OR = 0.704, 95% CI: 0.532–0.931, P = 0.014), whereas the Japanese study conferred tagSNP rs4720833 in MAFK was associated with an increased susceptibility to ATLI (Dominant model, OR = 3.162, 95% CI: 1.033–9.686, P = 0.037)22. In the present study, rs4720833 in MAFK was found to increase the risk of ATLI only in mixed patients under a recessive model (adjusted OR = 4.127, 95% CI: 1.054–16.16, P = 0.042) and an additive model (adjusted OR = 2.000, 95% CI: 1.096–3.650, P = 0.024), but not under a dominant model. Because of sequence similarity, no functional differences have been observed among the sMafs (MafF, MafG and MafK) in terms of their bZIP structures29. The sequencing results of each MAF gene suggested that MAFF was the most polymorphic of the MAF genes followed by MAFK, whereas MAFG had the lowest molecular plasticity30. Additionally, animal studies have also revealed that maff and mafk knockout mice, as well as the double knockout maff:mafk, did not have major phenotypical effects31. The accumulating lines of evidence unequivocally illustrated the importance and complexity of sMafs in the CNC-sMaf transcription factor network. Further research is needed on the role of these genetic variants in liver injury, especially in different ethnic populations.
This study was a nested case-control design based on anti-TB treatment cohort that decreases recall bias. The ATLI sample size in the present study was relatively large (more than our estimated minimum sample size), which allowed us to increase efficiency and control potential confounders by performing 1:2 matching. Moreover, each case was strictly assessed by experts to minimize the misclassification of diagnosis. However, there were several limitations in our study. First, we did not collect the patient histories of previous hepatitis C infection, which may affect the occurrence of liver injury. Second, due to the combination therapy strategy, we cannot explain the pathogenic mechanisms of specific drugs.
In summary, it is important to determine the relationship between genetic polymorphisms of NRF2, KEAP1, MAFF, MAFK and the risk of ATLI in the Chinese population and which genetic polymorphisms of NRF2, MAFF and MAFK may contribute to the susceptibility to ATLI. Furthermore, new studies in larger and varied populations are required to validate these relationships.
Methods
Anti-TB patients’ recruitment and follow-up
The study patients were recruited from the outpatient departments of four designated TB diagnosis and treatment hospitals between April 2014 and December 2016 based on the ADACS protocol32. This cohort of anti-TB treatment patients has been described in our previous study21. In brief, before treatment, patients would finish the baseline questionnaire (sex, age, TB treatment history, sputum smear, and other complications) and receive laboratory examinations, including serum hepatitis B virus surface antigen (HBsAg), ALT, AST, direct and total bilirubin levels. TB patients received the standard anti-TB short course chemotherapy regimen under DOTS strategy, including RIF, INH, PZA, EMB and/or streptomycin (SM/S), specifically 2HRZE/4HR for primary patients and 2HRZES/6HRE for retreatment patients32. Patients were monitored for 6~9 months according to the treatment episode. During the anti-TB treatment, a method combining active self-recorded diaries and passive scheduled liver function tests was used to detect abnormal liver function in time. Patients were asked to self-record signs and/or symptoms of discomfort and the local supervising doctors often checked the records for potential ATLI. Patients also received the scheduled liver function tests every two weeks in the first two months of treatment or when patients had exhibited some symptoms of suspected hepatic toxicity32.
Patients with one or more of the following were excluded: (i) patients with abnormal serum ALT, AST or total bilirubin levels before treatment; (ii) patients with HBsAg (+) serum; (iii) patients with alcoholic liver disease; (iv) patients with concomitant use of hepatotoxic drugs or habitual alcohol consumption; and (v) patients with chronic liver disease or other diseases that can also cause elevated liver enzymes.
The study was approved by the Ethics Committee of Nanjing Medical University and conducted in accordance with the Declaration of Helsinki Principles. Written informed consent was obtained from all patients.
ATLI Cases and non-ATLI controls selection and matching
A nested case-control study was conducted based on the dynamic cohort. The diagnostic criteria of ATLI was proposed by the international consensus meeting, namely, an increase in ALT levels greater than two-times of the upper limit of normal (ULN), with/without a combined increase in AST and total bilirubin levels, provided that one of them was more than two-times of ULN during the treatment33. Furthermore, the causality assessment result was certain, probable or possible based on the WHO Uppsala Monitoring Center system34. Each ATLI case was also strictly reviewed by experts from the local ADR monitoring center. Pattern of ATLI was defined by R value where R = (ALT/ULN)/(ALP/ULN)35. If R ≥ 5, then the pattern was hepatocellular. If R > 2 and <5, then the pattern was mixed. If R ≤ 2, then the pattern was cholestatic.
The patients who did not meet the ATLI criteria were considered candidate controls. For every ALTI case, two control patients were matched by sex, age (±5 years), treatment history, disease severity and drug dosage.
Sample size calculation
The sample size in present study was calculated using the Quanto statistical program (version 1.2.4, University of Southern California, USA)36. Based on our previous matched case-control study of ATLI, the effect size (odds ratio) was set at 2.0 with at least 90 percent power under the dominance model. Moreover, the minor allele frequency (MAF) was set at 10 percent, with a type I error level of 0.05. The incidence of ATLI in the Chinese anti-TB treatment population was 11.9%32. Finally, the sample size of the two groups was 253 ATLI cases and 253 non-ATLI controls.
TagSNPs selection and genotyping
TagSNPs in five genes (NRF2, KEAP1, MAFF, MAFK and MAFG) were selected from the Haploview software 4.2 (Broad Institute, Cambridge, MA, USA), based on the Chinese Han population data of Hapmap and the following criteria: (i) MAF ≥5% in Chinese population; (ii) r-square of pairwise linkage disequilibrium (LD) ≥0.8. As a result, fourteen potential tagSNPs were selected for genotyping using the Sequenom MassARRAY iplex Platform (Sequenom Inc., Hamburg, Germany). However, one tagSNP in MAFG (rs148165792, MAF = 7.3%) was excluded from the study due to a failed probe design. Technicians who performed the genotyping were blinded to the status of case and control. More than 10% of samples were selected randomly for repeated experiments with repeatability of 100%. The overall genotyping success rate was 100%. As a result, 13 tagSNPs of four genes were analyzed in present study (Table 2).
Statistical analysis
Distributions of demographic and clinical characteristics among two groups were evaluated by two-factor analysis of variance test (for normal continuous variables) or nonparametric test (for non-normal continuous variables), or by chi-square test (for categorical variables). Hardy-Weinberg equilibrium (HWE) in the control group was assessed by the chi-square test. Haploview software 4.2 was used to select haplotype blocks in consideration of the LD between SNPs in each gene. PHASE 2.1 was used to estimate haplotype frequencies for different gene. Multivariate conditional logistic regression model was used to analysis the genotype frequency differences between two groups. Three different genetic models (additive model, dominant model and recessive model) were used to comprehensively analyze the effect of tagSNPs. The association between genotypes and the risk of ATLI was estimated by odds ratios (ORs) and 95% confidence intervals (CIs), with weight and usage of hepatoprotectant as covariates. All statistical analyses were performed using the SPSS 20.0 (IBM Inc., Chicago, IL, USA). A two-tailed P-value < 0.05 was considered statistically significant.
References
World Health Organization. Global tuberculosis report 2018. (World Health Organization, Geneva, 2018).
Nahid, P. et al. Executive Summary: Official American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America Clinical Practice Guidelines: Treatment of Drug-Susceptible Tuberculosis. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America 63, 853–867, https://doi.org/10.1093/cid/ciw566 (2016).
Lv, X. et al. Adverse reactions due to directly observed treatment strategy therapy in Chinese tuberculosis patients: a prospective study. PloS one 8, e65037, https://doi.org/10.1371/journal.pone.0065037 (2013).
Awofeso, N. Anti-tuberculosis medication side-effects constitute major factor for poor adherence to tuberculosis treatment. Bulletin of the World Health Organization 86, B–d (2008).
Devarbhavi, H. Antituberculous drug-induced liver injury: current perspective. Tropical gastroenterology: official journal of the Digestive Diseases Foundation 32, 167–174 (2011).
Ramappa, V. & Aithal, G. P. Hepatotoxicity Related to Anti-tuberculosis Drugs: Mechanisms and Management. Journal of clinical and experimental hepatology 3, 37–49, https://doi.org/10.1016/j.jceh.2012.12.001 (2013).
Roy, P. D., Majumder, M. & Roy, B. Pharmacogenomics of anti-TB drugs-related hepatotoxicity. Pharmacogenomics 9, 311–321, https://doi.org/10.2217/14622416.9.3.311 (2008).
Corsini, A. & Bortolini, M. Drug-induced liver injury: the role of drug metabolism and transport. Journal of clinical pharmacology 53, 463–474, https://doi.org/10.1002/jcph.23 (2013).
Verma, A. K., Yadav, A., Singh, S. V., Mishra, P. & Rath, S. K. Isoniazid induces apoptosis: Role of oxidative stress and inhibition of nuclear translocation of nuclear factor (erythroid-derived 2)-like 2 (Nrf2). Life sciences 199, 23–33, https://doi.org/10.1016/j.lfs.2018.02.037 (2018).
Yew, W. W., Chang, K. C. & Chan, D. P. Oxidative Stress and First-Line Antituberculosis Drug-Induced Hepatotoxicity. Antimicrobial agents and chemotherapy 62, https://doi.org/10.1128/aac.02637-17 (2018).
Zhu, R., Wang, Y., Zhang, L. & Guo, Q. Oxidative stress and liver disease. Hepatology research: the official journal of the Japan Society of Hepatology 42, 741–749, https://doi.org/10.1111/j.1872-034X.2012.00996.x (2012).
Lee, J. M., Calkins, M. J., Chan, K., Kan, Y. W. & Johnson, J. A. Identification of the NF-E2-related factor-2-dependent genes conferring protection against oxidative stress in primary cortical astrocytes using oligonucleotide microarray analysis. The Journal of biological chemistry 278, 12029–12038, https://doi.org/10.1074/jbc.M211558200 (2003).
Zhang, Y. et al. Gene expression profiling reveals potential key pathways involved in pyrazinamide-mediated hepatotoxicity in Wistar rats. Journal of applied toxicology: JAT 33, 807–819, https://doi.org/10.1002/jat.2736 (2013).
Sodhi, C. P. et al. Study of oxidative-stress in isoniazid-rifampicin induced hepatic injury in young rats. Drug and chemical toxicology 20, 255–269, https://doi.org/10.3109/01480549709003881 (1997).
Chowdhury, A. et al. Induction of oxidative stress in antitubercular drug-induced hepatotoxicity. Indian journal of gastroenterology: official journal of the Indian Society of Gastroenterology 20, 97–100 (2001).
Urban, T. J., Daly, A. K. & Aithal, G. P. Genetic basis of drug-induced liver injury: present and future. Seminars in liver disease 34, 123–133, https://doi.org/10.1055/s-0034-1375954 (2014).
Bellezza, I., Giambanco, I., Minelli, A. & Donato, R. Nrf2-Keap1 signaling in oxidative and reductive stress. Biochimica et biophysica acta 1865, 721–733, https://doi.org/10.1016/j.bbamcr.2018.02.010 (2018).
Moi, P., Chan, K., Asunis, I., Cao, A. & Kan, Y. W. Isolation of NF-E2-related factor 2 (Nrf2), a NF-E2-like basic leucine zipper transcriptional activator that binds to the tandem NF-E2/AP1 repeat of the beta-globin locus control region. Proceedings of the National Academy of Sciences of the United States of America 91, 9926–9930 (1994).
Kannan, M. B., Solovieva, V. & Blank, V. The small MAF transcription factors MAFF, MAFG and MAFK: current knowledge and perspectives. Biochimica et biophysica acta 1823, 1841–1846, https://doi.org/10.1016/j.bbamcr.2012.06.012 (2012).
Copple, I. M. The Keap1-Nrf2 cell defense pathway–a promising therapeutic target? Advances in pharmacology (San Diego, Calif.) 63, 43–79, https://doi.org/10.1016/b978-0-12-398339-8.00002-1 (2012).
Yang, M. et al. Possible association of HMOX1 and NQO1 polymorphisms with anti-tuberculosis drug-induced liver injury: A matched case-control study. Journal of clinical pharmacy and therapeutics 44, 534–542, https://doi.org/10.1111/jcpt.12818 (2019).
Nanashima, K. et al. Genetic variants in antioxidant pathway: risk factors for hepatotoxicity in tuberculosis patients. Tuberculosis (Edinburgh, Scotland) 92, 253–259, https://doi.org/10.1016/j.tube.2011.12.004 (2012).
Tang, W., Jiang, Y. F., Ponnusamy, M. & Diallo, M. Role of Nrf2 in chronic liver disease. World journal of gastroenterology 20, 13079–13087, https://doi.org/10.3748/wjg.v20.i36.13079 (2014).
Bataille, A. M. & Manautou, J. E. Nrf2: a potential target for new therapeutics in liver disease. Clinical pharmacology and therapeutics 92, 340–348, https://doi.org/10.1038/clpt.2012.110 (2012).
Marzec, J. M. et al. Functional polymorphisms in the transcription factor NRF2 in humans increase the risk of acute lung injury. FASEB journal: official publication of the Federation of American Societies for Experimental Biology 21, 2237–2246, https://doi.org/10.1096/fj.06-7759com (2007).
Katsuoka, F. et al. Genetic evidence that small maf proteins are essential for the activation of antioxidant response element-dependent genes. Molecular and cellular biology 25, 8044–8051, https://doi.org/10.1128/mcb.25.18.8044-8051.2005 (2005).
Ward, L. D. & Kellis, M. HaploReg v4: systematic mining of putative causal variants, cell types, regulators and target genes for human complex traits and disease. Nucleic acids research 44, D877–881, https://doi.org/10.1093/nar/gkv1340 (2016).
Spicuglia, S. & Vanhille, L. Chromatin signatures of active enhancers. Nucleus (Austin, Tex.) 3, 126–131, https://doi.org/10.4161/nucl.19232 (2012).
Katsuoka, F. & Yamamoto, M. Small Maf proteins (MafF, MafG, MafK): History, structure and function. Gene 586, 197–205, https://doi.org/10.1016/j.gene.2016.03.058 (2016).
Martinez-Hernandez, A. et al. Small MAF genes variants and chronic myeloid leukemia. European journal of haematology 92, 35–41, https://doi.org/10.1111/ejh.12211 (2014).
Motohashi, H., Katsuoka, F., Engel, J. D. & Yamamoto, M. Small Maf proteins serve as transcriptional cofactors for keratinocyte differentiation in the Keap1-Nrf2 regulatory pathway. Proceedings of the National Academy of Sciences of the United States of America 101, 6379–6384, https://doi.org/10.1073/pnas.0305902101 (2004).
Xia, Y. Y. et al. Design of the anti-tuberculosis drugs induced adverse reactions in China National Tuberculosis Prevention and Control Scheme Study (ADACS). BMC public health 10, 267, https://doi.org/10.1186/1471-2458-10-267 (2010).
Benichou, C. Criteria of drug-induced liver disorders. Report of an international consensus meeting. Journal of hepatology 11, 272–276 (1990).
World Health Organization. The use of the WHO-UMC system for standardized case causality assessment. (The Uppsala Monitoring, 2005).
Aithal, G. P. et al. Case definition and phenotype standardization in drug-induced liver injury. Clinical pharmacology and therapeutics 89, 806–815, https://doi.org/10.1038/clpt.2011.58 (2011).
Gauderman, W. J. & Morrison, J. M. QUANTO 1.1: A computer program for power and sample size calculations for genetic-epidemiology studies, http://hydra.usc.edu/gxe (2006).
Acknowledgements
This study is funded by National Natural Science Foundation of China (No. 81373066), Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD). We are grateful to all cooperating organizations and their staff whose hard work made this study possible.
Author information
Authors and Affiliations
Contributions
Study design (Shaowen Tang and Siyan Zhan), patients follow-up and data collection (Shixian Chen, Yongzhong Chen, Lihuan Lu, Xiaomin He and Hongbo Chen), gene detection (Shixian Chen, Hongqiu Pan and Ru Chen), data analysis (Shixian Chen and Ru Chen), manuscript writing (Shixian Chen and Shaowen Tang). All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, S., Pan, H., Chen, Y. et al. Association between genetic polymorphisms of NRF2, KEAP1, MAFF, MAFK and anti-tuberculosis drug-induced liver injury: a nested case-control study. Sci Rep 9, 14311 (2019). https://doi.org/10.1038/s41598-019-50706-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-019-50706-y
- Springer Nature Limited