Abstract
Laparoscopic surgery technology continues to advance. However, much less attention has been focused on how alteration of the laparoscopic surgical environment might improve clinical outcomes. We conducted a randomized, 2 × 2 factorial trial to evaluate whether low intraperitoneal pressure (IPP) (8 mmHg) and/or warmed, humidified CO2 (WH) gas are better for minimizing the adverse impact of a CO2 pneumoperitoneum on the peritoneal environment during laparoscopic surgery and for improving clinical outcomes compared to the standard IPP (12 mmHg) and/or cool and dry CO2 (CD) gas. Herein we show that low IPP and WH gas may decrease inflammation in the laparoscopic surgical environment, resulting in better clinical outcomes. Low IPP and/or WH gas significantly lowered expression of inflammation-related genes in peritoneal tissues compared to the standard IPP and/or CD gas. The odds ratios of a visual analogue scale (VAS) pain score >30 in the ward was 0.18 (95% CI: 0.06, 0.52) at 12 hours and 0.06 (95% CI: 0.01, 0.26) at 24 hours in the low IPP group versus the standard IPP group, and 0.16 (95% CI: 0.05, 0.49) at 0 hours and 0.29 (95% CI: 0.10, 0.79) at 12 hours in the WH gas group versus the CD gas group.
Similar content being viewed by others
Introduction
Laparoscopic surgery technology has evolved dramatically over the past 3 decades, and continues to advance. However, much less attention has been focused on how alteration of the laparoscopic surgical environment might improve clinical outcomes.
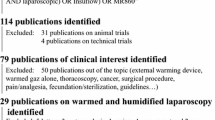
We previously investigated the impact of IPP during a CO2 pneumoperitoneum on expression levels of 84 genes known to encode extracellular matrix and adhesion molecules and 84 genes that encode inflammatory cytokine signaling molecules in peritoneal tissues using two real-time polymerase chain reaction (PCR)-based assay panels1, 2. We hypothesized that a high IPP during a CO2 pneumoperitoneum might adversely affect gene expression of extracellular matrix, adhesion and inflammatory cytokine signaling molecules in peritoneal tissues3, 4, if the high IPP caused higher rates of peritoneal dissemination, peritoneal tissue hypoxia and post-operative adhesion formation, as demonstrated in animal studies5,6,7,8. We identified several differentially expressed genes (4 adhesion-formation-related genes, 4 inflammation-related genes, and 5 hyaluronan [HA]-related genes) in peritoneal tissues in the standard IPP (12 mmHg) group compared with the low IPP (8 mmHg) group. Our previous findings suggested that a low IPP (8 mmHg) might minimize the adverse impacts of IPP on the fibrinolytic system, inflammation, peritoneal fibrosis, and generation of hyaluronan (HA) fragments1, 2. However, our previous studies were not randomized1, 2. In addition, we did not evaluate whether a low IPP (8 mmHg) could improve clinical outcomes1, 2. A Cochrane review concluded that no evidence is currently available to support the use of a low-pressure pneumoperitoneum in low–anesthetic-risk patients undergoing elective laparoscopic cholecystectomy9. Regarding temperature and humidity, previous animal and in vitro experiments demonstrated that a cool and dry CO2 (CD) gas, which we use in a clinical setting, might adversely affect the surgical peritoneal environment10,11,12,13. However, a Cochrane review concluded that during laparoscopic abdominal surgery, heated gas insufflation, with or without humidification, minimally impacts patient outcomes14. However, no studies have yet evaluated the impact of the combined use of a warmed, humidified CO2 (WH) gas pneumoperitoneum and low IPP during laparoscopic surgery on the peritoneal environment and postoperative clinical outcomes.
In the present study, we hypothesized that combined use of low IPP and WH gas may be better for minimizing the adverse impact of a CO2 pneumoperitoneum on the surgical peritoneal environment during laparoscopic abdominal surgery and improving postoperative clinical outcomes, compared to the standard IPP and CD gas. To test this hypothesis, we conducted the present randomized, 2 × 2 factorial trial.
The primary objective of this study was to compare the impact of low IPP (8 mmHg) versus standard IPP (12 mmHg), and CD gas versus WH gas, on expression levels of 12 genes (4 adhesion-formation-related genes, 4 inflammation-related genes, and 4 hyaluronan [HA]-related genes) in peritoneal biopsy specimens according to our previous studies1, 2. Secondary objectives were to compare the impacts of low IPP versus standard IPP, and CD gas versus WH gas, on the quality of postoperative recovery, postoperative pain, intraoperative core body temperature, and intraoperative and postoperative complications.
Methods
The study was designed as a prospective, 2 × 2 factorial, four–parallel-group, single-center, single-blinded (patients), superiority randomized trial. Patients were recruited at CHU Clermont-Ferrand from September 2013 through June 2016. The study protocol was approved by the Consultative Committee for Protection of Persons in Biomedical Research (CPP) of the Auvergne (France) region and registered by the competent French authority (ANSM, Saint Denis, France). Informed written consent was obtained from each patient prior to surgery. Methods were carried out in accordance with the approved guidelines and regulations. This trial is registered with ClinicalTrials.gov on 24/06/2013, trial number NCT01887028.
During study recruitment, all patients who underwent laparoscopic sub-total hysterectomy with promontofixation for uterine prolapse were assessed for eligibility to participate by the principal investigators (S.M. and R.B.). The full trial protocol can be found in the Supplement (see Supplementary Methods). After obtaining informed written consent, participants are allocated in a 1:1:1:1 ratio by a remote 24-hour-a-day computer-generated randomization system hosted at the Institute for Medical Informatics, Statistics and Documentation, Medical University of Graz, in Graz, Austria (https://www.randomizer.at/) using an algorithm with BMI (<25 vs. ≥25), height (<160 vs. ≥160 cm), and age (<65 vs. ≥65 years) as minimization covariates. This randomized trial employed a 2 × 2 factorial design, with IPP and types of CO2 gas as factors, resulting in four experimental arms: 1) 12-mmHg IPP with CD gas, 2) 12-mmHg IPP with WH gas, 3) 8-mmHg IPP with CD gas, and 4) 8-mmHg IPP with WH gas. After randomization, patients can only be excluded if pathological peritoneal tissues such as adhesions are detected just after insertion of the four trocars, a different surgical technique is needed because the sacral promontory is not clearly identified, IPP is changed during the surgery, conversion to laparotomy, or withdrawal of consent. Enrollment in this study is voluntary and patients are allowed to withdraw at any time.
Patients were blinded for the allocated treatment arm until the end of the study. The nurse anesthetists in the postanesthesia care unit (PACU) and the ward nurses, who evaluated postoperative pain using a visual analogue scale (VAS), were also blinded. The database was submitted for analysis to independent statisticians who were blinded and were neither involved in the trial management nor employed by the trial sponsor.
Anesthetic management was performed by 8 staff anesthesiologists (L.V., M.B., A.F., G.R., A.L., C.C., A.B., B.S.) and anesthesiology residents or nurse anesthetists under their supervision. In the operating room, standard ASA anesthetic monitors were placed. All patients received a standardized general anesthetic consisting of premedication with oral administration of 1 mg/kg hydroxyzine hydrochloride suspension 1 hour preoperatively and induction with target-controlled infusion of 0.2 mcg/kg sufentanil and 3 to 5 mg/kg IV propofol. Two mg/kg IV cisatracurium were used to facilitate tracheal intubation. The patient’s lungs were ventilated with a 40:60 mixture of oxygen to nitrous oxide. Desflurane and target-controlled infusion of sufentanil were added for maintenance. To assure suitable operating conditions, neuromuscular blockade was maintained using cisatracurium. After induction of anesthesia, all patients received intraoperative forced-air warming, which was placed on the patient by the anesthesia staff. Intraoperative core temperature was measured at 15-minute intervals using an esophageal probe. For prevention of postoperative nausea and vomiting, 8 mg IV dexamethasone at the beginning of intervention, and 1 mg IV droperidol 1 and 4 mg IV ondansetron at the end of intervention were administrated. 30 minutes before the end of intervention, all patients received 1 g IV paracetamol and 50 mg IV ketoprofene for prevention of postoperative pain.
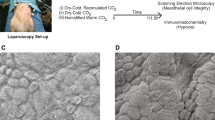
This study involved 1 staff surgeon (R.B.) who performed all operations with the assistance of a gynecological surgical resident. Insufflation of CO2 gas was performed using a Storz electronic endoflator (Karl Storz Endoscopy & GmbH, Tuttlingen, Germany). CO2 gas was warmed to 37 °C and humidified to 98% RH using the Fisher & Paykel MR860 Laparoscopic Humidification System (HumiGard, Fisher & Paykel Healthcare, Auckland, New Zealand). For the groups receiving WH gas, 180 mL sterile water was added to the chamber and the humidifier was switched on. For the groups receiving standard CD gas, sterile water was not added to the chamber and the humidifier was not switched on, and CO2 gas was delivered at room temperature (21 °C) and 0% relative humidity
When the IPP reached 15 mmHg, four trocars were inserted, immediately after which the IPP was decreased to 12 or 8 mmHg and then maintained at these levels throughout surgery. For all patients, 5 mL ropivacaine hydrochloride solution (2 mg/mL) were infiltrated around the trocar wounds. All incisions were made after ropivacaine infiltration. In addition, 20 mL ropivacaine solution (2 mg/mL) were infused at the beginning of the operation under the right hemidiaphragm. Laparoscopic sub-total hysterectomy with promontofixation used the same surgical technique previously described by our group was performed15. Macroscopically normal peritoneum was collected from the anterior parietal wall at the beginning of surgery and every 60 minutes thereafter as previously described1, 2.
All patients received our standardized post-operative pain management. On arrival in the PACU, patients were asked to rate their pain at rest using a VAS. After the initial rating, pain ratings were repeated every 20 minutes during the remainder of the PACU stay. When the pain score was >30 of 100, postoperative pain was treated with an IV bolus of 2 to 3 mg morphine, and then 1 to 2 mg IV every 10 minutes to achieve a pain score ≤30 of 100. Intravenous patient-controlled analgesia (IV-PCA) was prepared using morphine (1 mg/mL) and droperidol (0.05 mg/mL). On arrival in the ward, patients were asked to rate their pain at rest using a VAS. Then, the intensity of postoperative pain at rest and/or on moving was assessed using a VAS every 4 hours until 24 hours postoperatively, then 3 times/day until discharge. All patients received 1 g paracetamol and 50 mg of ketoprofene IV every 6 hours until 24 hours postoperatively. Then, pain was managed using oral paracetamol and ketoprofene.
The quality of postoperative functional recovery was assessed using the QoR-40 questionnaire16. The QoR-40 was originally designed to assess recovery in five dimensions 24 h after surgery (emotional state, physical comfort, psychological support, physical independence and pain)16. It may be most suitable for use in clinical trials or for inpatients17. The QoR-40 was administered four times, the day before surgery (between 7:00 and 8:00 pm, baseline score), 24 hours and 48 hours postoperatively, and at the first postoperative visit (30 days after surgery). Intraoperative and postoperative complications were recorded and postoperative complications were classified according to the Clavien-Dindo classification18.
Quality of surgical conditions, including the operative technical difficulty, working space, visibility, and pain experienced by the surgeon such as shoulder pain, backache, and hand/finger joint pain during surgery, was rated by the operating surgeon at the end of each procedure using visual analogue scales consisting of 100-mm lines anchored at both ends with 0 and 100.
mRNA levels of 12 genes (connective tissue growth factor [CTGF], matrix metalloproteinase-9 [MMP-9], plasminogen activator inhibitor-1 [PAI-1], tissue plasminogen activator [tPA], thrombospondin-2 [TSP-2], chemokine (C-X-C motif) ligand 2 [CXCL-2], E-selectin, interleukin-10 [IL-10], hyaluronic acid synthase-1 [HAS-1], HAS-2, HAS-3, and hyaluronidase-1 [Hyal-1]) were measured by quantitative real-time RT-PCR with a Light Cycler (Roche, Mannheim, Germany) as previously described1, 2.
Statistical analysis
The STATA program version 13.1 (StataCorp, College Station, TX, USA) was used for statistical analysis. The power calculation of the present trial was based on our previous studies1, 2 and our pilot study. The standard deviation was calculated from these gene expression level results for 12 genes and differences that we considered biologically plausible with a significance level of 0.05; 40 patients for each group enabled a power of 91–95% for each gene.
The global QoR-40 scores and the dimensions of the QoR-40 questionnaire were analyzed using the generalized linear mixed model to allow for repeat measurements over time from each patient. The baseline score was considered as a covariate in the analysis, and three main factors were used in the analysis: IPP, type of CO2 gas, and time point. The results were summarized as the mean difference in scores between groups, after adjusting for levels at baseline.
VAS pain scores were grouped into three categories; ≤30, 31–70, and >70. A study showed that grouping VAS scores into categories (≤30, 31–70, and >70) provides greater clinical relevance for comparisons than using the full spectrum of measured values or changes in value, when pain is an outcome measure in postoperative patients19. During the PACU stay, the maximum pain score before receiving morphine was assessed at a single time point. Logistic regression was used for the analysis. During the inpatient ward stay, pain scores were measured at multiple time points. To allow for multiple measurements over time, the analysis was performed using mixed logistic regression methods. Two-level models were used, with individual measurements nested within patients. To allow for varying pain scores over time, terms for time were included in the regression model. Linear, squared, and cubic terms for time were all included to allow modelling of a flexible relationship between time and pain score. Interactions between the two treatments (IPP and type of CO2 gas) and time were included to allow the treatment effects to vary over the course of the inpatient stay. The regression models were simplified to omit non-significant interactions from the final model. Mixed logistic regression was used for the analysis.
The gene expression levels in peritoneal biopsy specimens relative to levels of a reference gene (GAPDH) were assessed at 0 hours, and at 1 and 2 hours during a CO2 pneumoperitoneum. This analysis approach considered the 1- and 2-hour values as separate outcomes, which were thus analyzed separately. Linear regression was used for the analysis, with the baseline (0 hours) values included as a covariate.
For the remaining analyses, groups were compared using Fisher’s exact test for categorical variables, the Mann-Whitney U test for nonparametric continuous variables, and the t test for parametric continuous variables. Statistical significance was accepted at the 0.05 level.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Results
A total of 144 patients were assessed for eligibility and 93 patients consented and were randomly assigned into the study. Nine patients were excluded after randomization. We therefore collected and analyzed data from 82 patients. The detailed patient flow is shown in the CONSORT diagram in Fig. 1. Patient and surgical characteristics by randomization group and by treatment group are presented in Tables 1 and 2, respectively. Patient and surgical characteristics did not differ between the 12-mmHg and 8-mmHg groups, or between the CD gas and WH gas groups, except for the CO2 volume used during CO2 pneumoperitoneum between the 12-mmHg and 8-mmHg groups: the CO2 volume used in the 8-mmHg group was significantly smaller than that used in the 12-mmHg group (Table 2).
Gene expression in peritoneal biopsy specimens
Results are shown in Table 3.
Adhesion-formation–related genes
At 1 hour, a significant effect of IPP on expression of CTGF, MMP 9, and PAI-1 was observed. At 2 hours, significant effects of IPP and type of CO2 gas on CTGF, MMP 9, and PAI-1 expression were observed.
Inflammation-related genes
At 1 hour, no significant effect of either IPP or type of CO2 gas was observed on CXCL-2, E-selectin, IL-10 expression or TSP2. At 2 hours, significant effects of IPP and type of CO2 gas on these four genes were observed.
Hyaluronic acid (HA)-related genes
At 1 hour, a significant effect of IPP and/or type of gas was observed on HAS-1, HAS-2, HAS-3, and Hyal-1 expression. At 2 hours, significant effects of IPP and type of CO2 gas were observed on HAS-1, HAS-3, HAS-2, and Hyal-1 expression.
Quality of postoperative recovery
Results are shown in Table 4. No differences in basal global QoR-40 scores were observed between the 12-mmHg and 8-mmHg groups, or between the WH gas and CD gas groups (Table 2). For all outcomes (global, five dimensions), no statistically significant interactions were observed between IPP and type of CO2 gas. For the global QoR-40 score and for the four dimensions of the QoR-40, “emotional state,” “physical comfort,” “physical independence,” and “psychological support,” no significant time by IPP interaction or time by type of CO2 gas interaction was observed. Global QoR-40 scores were higher in the 8-mmHg group than in the 12-mmHg group (mean difference: 1.4, p = 0.006). No significant differences in global QoR-40 scores were observed between the CD gas and WH gas groups. “Psychological support” was significantly higher in the 8-mmHg group than in the 12-mmHg groups (p = 0.04). However, the mean difference was only 0.07 between groups. For the “pain” dimension, a significant time by IPP interaction was observed (p = 0.008), but no significant time by type of CO2 gas interaction was noted. The score for the “pain” dimension was significantly higher in the 8-mmHg group than in the 12-mmHg group at 24 hours (mean difference: 2.3, p < 0.001) and at 48 hours (mean difference: 1.6, p = 0.008) postoperatively. No significant difference in “pain” was observed between the 8-mmHg and 12-mmHg groups 30 days postoperatively. Furthermore, no significant difference in “pain” was observed between the CD gas and WH gas groups.
VAS pain score
There were no patients with a VAS score >30 the day before surgery (between 7:00 and 8:00 pm, baseline score). In the present analysis, we only analyzed VAS pain scores at rest, because during the early postoperative period up to 12 hours, many patients stayed at rest; thus, pain scores on movement could not be sufficiently evaluated during this period. No patients had shoulder pain. We have been systematically performing infusion of ropivacaine solution under the right hemidiaphragm for over 10 years. During this time, we have had no or few complaints about shoulder pain after laparoscopic surgery.
In the present study, there were very few patients with a VAS score >70 postoperatively. Thus, pain scores were categorized as either ≤30 (no or mild pain) or >30 (clinically relevant moderate to severe pain), giving a binary measure19.
In the PACU, no significant differences in the number of patients who required morphine and morphine dose infused were observed between the 12-mmHg IPP and 8-mmHg IPP groups or between the WH gas and CD gas groups (Table 2) (Table 5). No significant interaction in VAS pain scores was observed between IPP and type of CO2 gas (p = 0.81). Neither IPP nor the type of gas was associated with the likelihood of a high VAS pain score >30 in the PACU (p = 0.81 and p = 0.70, respectively) (Table 5).
In the ward, few patients required morphine injections by a PCA (Tables 1 and 2). A non-significant three-way interaction was observed between IPP, type of CO2 gas and time (p = 0.21), and a non- significant-two-way interaction was observed between IPP and type of CO2 gas (p = 0.22). No significant difference was observed in the likelihood of a VAS pain score >30 between the 8-mmHg and 12-mmHg groups at 0 hours (p = 0.29) (Fig. 2A and B, Table 6). However, there was a significant difference between the 8-mmHg and the 12-mmHg groups was observed at 12 hours (p = 0.001) and at 24 hours (p < 0.001) (Fig. 2A and B, Table 6). The odds ratios of a VAS pain score > 30 was 0.18 (95% CI: 0.06, 0.52) at 12 hours and 0.06 (95% CI: 0.01, 0.26) at 24 hours when comparing the 8-mmHg group relative to the 12-mmHg group (Fig. 2A and B, Table 6). In addition, significant differences in in the likelihood of a VAS pain score > 30 were observed at 0 hours (p = 0.001) and at 12 hours (p = 0.02) between the CD gas and WH gas groups (Fig. 2A and B, Table 6). The odds ratios of a VAS pain score of >30 was 0.16 (95% CI: 0.05, 0.49) at 0 hours and 0.29 (95% CI: 0.10, 0.79) at 12 hours when comparing the WH gas group relative to the CD gas group (Fig. 2A and B, Table 6). No significant difference between the CD gas and WH gas groups were observed at 24 hours (Fig. 2A and B, Table 6).
Odds ratios (A and B) of a VAS pain score of >30 in the ward. aOdds ratios when comparing the 8-mmHg group relative to the 12-mmHg group. bOdds ratios when comparing the WH group relative to the CD group. Number of patients. 12-mmHg group: n = 41 at 0 hours, n = 41 at 12 hours; n = 41 at 24 hours. 8-mmHg group: n = 41 at 0 hours, n = 41 at 12 hours; n = 41 at 24 hours. CD group: n = 42 at 0 hours, n = 42 at 12 hours; n = 42 at 24 hours. WH group: n = 40 at 0 hours, n = 40 at 12 hours; n = 40 at 24 hours.
Intraoperative core temperature
No significant differences in the start, minimum, maximum, mean, or final intraoperative core body temperatures were observed between the CD gas and WH gas groups (Table 2).
Intraoperative and postoperative complications
One patient in the 8-mmHg with CD gas group had an intraoperative complication (perforation of the stomach by the Veress needle). Postoperatively, the patient had an uneventful recovery and was discharged on postoperative day 3. No patients had postoperative complications.
Quality of surgical conditions
Scores rated by the surgeon for operative technical difficulty and working space for dissection and suturing were significantly worse in the 8-mmHg group than in the 12-mmHg group (Supplementary Table S1). No significant differences in scores for surgical field visibility were observed between the 8-mmHg group and the 12-mmHg group, or between the CD gas group and the WH gas group Supplementary Table S1). The surgeon experienced low back pain/discomfort during surgery. No significant difference in scores for this pain/physical discomfort rated by the surgeon was observed between the 8-mmHg and 12-mmHg groups (Supplementary Table S1).
Discussion
Effects of low IPP may be clinically significant for “pain” among the five dimensions of the QoR-4020. The present study showed that the odds of a VAS pain score >30 in the ward was over 10 times lower in the 8-mmHg group at 24 hours in agreement with the present analysis of QoR-40 scores. Postoperative pain is correlated with quality of recovery. These findings suggest that low IPP may result in a better quality of postoperative recovery by decreasing postoperative pain. Morphine requirement in the PACU did not differ between the 12-mmHg and 8-mmHg groups. However, the effects did trend in favor of low IPP. Because the power analysis was designed to detect a difference in the gene expression levels, a higher-powered study might have detected a difference in this clinical outcome measure. In the present study, we observed no significant difference in the percentage of patients with VAS pain scores >30 at 24 hours postoperatively between the WH gas group and the CD gas group, which is consistent with the present QoR-40 score analysis. However, we observed that the odds of a VAS pain score >30 was over five times lower in the WH gas group compared to the CD gas group when patients arrived in the ward approximately 2 hours postoperatively. A meta-analysis revealed a statistically significant reduction in VAS pain scores in the WH gas group within 6 hours, but not at 24 hours, postoperatively21. Laparoscopic surgery has been considered to cause less postoperative pain than laparotomy. However, one study showed that laparoscopic surgery may be more painful in the immediate postoperative period (0–4 hours) compared to laparotomy22. The present findings and a previous meta-analysis21 suggest that a WH gas may be effective in reducing pain scores during the immediate postoperative period after laparoscopic surgery. The present molecular analysis indicated that low IPP significantly decreased expression of pro-inflammatory genes (CXCL-2, E-selectin) and significantly increased that of anti-inflammatory genes (IL-10, TSP2) compared to the standard IPP. In addition, low IPP and WH gas significantly increased the HA synthase genes HAS-1 and HAS-2 compared to the standard IPP and CD gas. HA, a major component of the extracellular matrix (ECM), plays a key role in regulating inflammation23. HAS-1 and HAS-2 encode high–molecular-weight HA, which suppresses the inflammatory response23. These findings suggest that low IPP and WH gas decreased the likelihood of a clinically significant high VAS pain score in the first 24 hours after laparoscopic surgery by reducing inflammation in the surgical laparoscopic peritoneal environment. Further studies to investigate the molecular mechanisms underlying the different effects of low IPP and WH gas on postoperative pain may provide useful information for developing strategies to reduce pain after laparoscopic abdominal surgery. A limitation of the present molecular analysis is that it is unclear whether similar effects of a low IPP and/or WH gas on these 12 genes would be observed, if the surgical procedure was much longer than that in the present study. In addition, it is ethically impossible to perform serial laparoscopies to collect peritoneal biopsy specimens and/or to evaluate the clinical significance of the present molecular findings on clinical outcomes such as postoperative adhesion formation.
A major disadvantage of using a low IPP is that surgical conditions are worse than with the standard IPP. A Cochrane review concluded that the safety of low-pressure pneumoperitoneum has yet to be established9. The surgeon’s laparoscopic skills represent a risk factor for perioperative complications of laparoscopic surgery24. A major advantage of low IPP is that it requires no additional cost during laparoscopic surgery if the duration of surgery is not affected. The results of the present study and previous studies suggested that experienced surgeons may not need a longer duration of surgery at low IPP even if they realize that surgical conditions may be worse9. The present findings may support a clinical benefit of low IPP; however, use of low IPP should be recommended only for skilled, experienced surgeons.
In contrast, use of a WH gas requires no technical effort and could be applied to any abdominal laparoscopic surgery and by any surgeon. In the present study, no significant interactions were observed between IPP and the type of CO2 gas used for VAS pain scores. In addition, the present molecular analysis showed that adhesion-formation–related and inflammation-related gene expression levels were less affected when using WH gas at the standard IPP. Thus, when low IPP may not be feasible, use of WH gas at the standard IPP may be a clinically useful alternative for reducing postoperative pain and minimizing adverse effects of a CO2 pneumoperitoneum at the standard IPP on the surgical peritoneal environment. However, a major disadvantage of using WH gas is the additional cost. Further studies are required to perform a cost-benefit analysis on the use of WH gas during laparoscopic abdominal surgery.
The present study showed no significant difference in the length of hospital stay between the 12-mmHg IPP and 8-mmHg IPP groups or between the WH gas and CD gas groups. However, length of hospital stay after surgery would be influenced by many different factors such as preoperative counseling regarding expected length of stay, supports in place at home for patient upon discharge and distance from the hospital to home25, 26. In the present study, all patients were informed about the expected discharge 3 days after operation.
The external validity of randomized controlled trials (RCTs) is often low27. Previous studies have also suggested that a low IPP may reduce postoperative pain compared to the standard IPP9, 28, 29. However, almost all of these previous studies were conducted during laparoscopic cholecystectomy;9, 28, 29 thus, it is not clear whether the present findings may be generalized to different surgical procedures for other pathologies. In the present study, only patients with a macroscopically normal peritoneum were included. Whether low IPP and/or WH gas would have the same impact on peritoneal gene expression levels and postoperative pain in patients with pathological peritoneum remains to be clarified.
In conclusion, the present randomized 2 × 2 factorial trial showed that low IPP and/or WH gas significantly lowered expression of inflammation-related genes in peritoneal tissues compared to the standard IPP and/or CD gas. Low IPP and WH gas independently decreased the likelihood of a high VAS pain score (>30) after surgery.
References
Matsuzaki, S. et al. Impact of intraperitoneal pressure and duration of surgery on levels of tissue plasminogen activator and plasminogen activator inhibitor-1 mRNA in peritoneal tissues during laparoscopic surgery. Hum. Reprod. 226, 1073–1081 (2011).
Matsuzaki, S. et al. Impact of intraperitoneal pressure of a CO2 pneumoperitoneum on the surgical peritoneal environment. Hum. Reprod. 27, 1613–1623 (2012).
Novitsky, Y. W., Litwin, D. E. & Callery, M. P. The net immunologic advantage of laparoscopic surgery. Surg. Endosc. 18, 1411–1419 (2004).
Jayne, D. Molecular biology of peritoneal carcinomatosis. Cancer Treat. Res. 2134, 21–33 (2007).
Wittich, P., Steyerberg, E. W., Simons, S. H., Marquet, R. L. & Bonjer, H. J. Intraperitoneal tumor growth is influenced by pressure of carbon dioxide pneumoperitoneum. Surg. Endosc. 14, 817–819 (2000).
Bourdel N et al. Peritoneal tissue-oxygen tension during a carbon dioxide pneumoperitoneum in a mouse laparoscopic model with controlled respiratory support. Hum. Reprod. 22, 1149–1155 (2007).
Matsuzaki, S. et al. Molecular mechanisms underlying postoperative peritoneal tumor dissemination may differ between a laparotomy and carbon dioxide pneumoperitoneum: a syngeneic mouse model with controlled respiratory support. Surg. Endosc. 23, 705–714 (2009).
Matsuzaki, S. et al. Carbon dioxide pneumoperitoneum, intraperitoneal pressure, and peritoneal tissue hypoxia: a mouse study with controlled respiratory support. Surg. Endosc. 24, 2871–2880 (2010).
Gurusamy, K. S., Vaughan, J. & Davidson, B. R. Low pressure versus standard pressure pneumoperitoneum in laparoscopic cholecystectomy. Cochrane Database Syst. Rev. 18, CD006930 (2014).
Volz, J. et al. Pathophysiologic features of a pneumoperitoneum at laparoscopy: a swine model. Am. J. Obstet. Gynecol. 174, 132–140 (1996).
Neuhaus, S. J. & Watson, D. I. Pneumoperitoneum and peritoneal surface changes: a review. Surg. Endosc. 18, 1316–1322 (2004).
Erikoglu, M., Yol, S., Avunduk, M. C., Erdemli, E. & Can, A. Electron-microscopic alterations of the peritoneum after both cold and heated carbon dioxide pneumoperitoneum. J. Surg. Res. 125, 73–77 (2005).
Rosário, M. T. et al. Does CO2 pneumoperitoneum alter the ultra-structuture of the mesothelium? J. Surg. Res. 133, 84–88 (2006).
Birch, D. W. et al. Heated insufflation with or without humidification for laparoscopic abdominal surgery. Cochrane Database Syst. Rev. 10, CD007821 (2016).
Rivoire, C. et al. Complete laparoscopic treatment of genital prolapse with meshes including vaginal promontofixation and anterior repair: a series of 138 patients. J. Minim. Invasive Gynecol. 14, 712–718 (2007).
Myles, P. S., Weitkamp, B., Jones, K., Melick, J. & Hensen, S. Validity and reliability of a postoperative quality of recovery score: the QoR-40. Br. J. Anaesth. 84, 11–15 (2000).
Herrera, F. J., Wong, J. & Chung, F. A systematic review of postoperative recovery outcomes measurements after ambulatory surgery. Anesth. Analg. 105, 63–69 (2007).
Dindo, D., Demartines, N. & Clavien, P. A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann. Surg. 240, 205–213 (2004).
Bodian, C. A., Freedman, G., Hossain, S., Eisenkraft, J. B. & Beilin, Y. The visual analog scale for pain: clinical significance in postoperative patients. Anesthesiology. 95, 1356–1361 (2001).
Myles, P. S. et al. Minimal Clinically Important Difference for Three Quality of Recovery Scales. Anesthesiology. 125, 39–45 (2016).
Sammour, T. et al. Systematic review of oxidative stress associated with pneumoperitoneum. Br. J. Surg. 96, 836–850 (2009). Review.
Ekstein, P. et al. Laparoscopic surgery may be associated with severe pain and high analgesia requirements in the immediate postoperative period. Ann. Surg. 243, 41–46 (2006).
Petrey, A. C. & de la Motte, C. A. Hyaluronan, a crucial regulator of inflammation. Front. Immunol. 5, 101 (2014).
Giger, U. F. et al. Risk factors for perioperative complications in patients undergoing laparoscopic cholecystectomy: analysis of 22,953 consecutive cases from the Swiss Association of Laparoscopic and Thoracoscopic Surgery database. J. Am. Coll. Surg. 203, 723–728 (2006).
Kelly, M., Sharp, L., Dwane, F., Kelleher, T. & Comber, H. Factors predicting hospital length-of-stay and readmission after colorectal resection: a population-based study of elective and emergency admissions. BMC Health Serv. Res. 12, 77 (2012).
Aarts, M. A. et al. Adoption of enhanced recovery after surgery (ERAS) strategies for colorectal surgery at academic teaching hospitals and impact on total length of hospital stay. Surg. Endosc. 26, 442–450 (2012).
Farrokhyar, F. et al. Randomized controlled trials of surgical interventions. Ann. Surg. 251, 409–416 (2010). Review.
Hua, J., Gong, J., Yao, L., Zhou, B. & Song, Z. Low-pressure versus standard-pressure pneumoperitoneum for laparoscopic cholecystectomy: a systematic review and meta-analysis. Am. J. Surg. 208, 143–150 (2014).
Özdemir-van Brunschot, D. M. et al. What is the evidence for the use of low-pressure pneumoperitoneum? A systematic review. Surg. Endosc. 30, 2049–2065 (2016).
Acknowledgements
We are most grateful to all the patients who participated in the present study. We also thank the gynecological surgical residents, anesthesiology residents, nurse anesthetists, and all the staff in the Department of Gynecology and operating room, CHU Clermont-Ferrand. This study was supported in part by Karl Storz Endoscopy & GmbH (Tuttlingen, Germany) and the Fondation de l’Avenir (ET4-741) (Paris, France). The funders (Karl Storz Endoscopy & GmbH and the Fondation de l’Avenir) had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
S.M., M.C., R.B. were involved in concept and design of the clinical trial. S.M., R.B., were involved in sample collection or experiments. S.M., L.V., M.B., C.H., A.F., G.R. A.L., C.C., A.B., B.S., J.B., M.C. R.B. were involved in acquisition, analysis or interpretation of data. S.M., L.V., R.B. were involved in drafting the article. All authors were involved in critical revision of the article. All authors read and approved the final version of the paper.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Matsuzaki, S., Vernis, L., Bonnin, M. et al. Effects of low intraperitoneal pressure and a warmed, humidified carbon dioxide gas in laparoscopic surgery: a randomized clinical trial. Sci Rep 7, 11287 (2017). https://doi.org/10.1038/s41598-017-10769-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-10769-1
- Springer Nature Limited