Abstract
The dietary intake of methyl donors is favorably associated with many diseases, but the findings regarding primary liver cancer (PLC) risk are limited. This study investigated the association between the intake of choline, betaine and methionine and PLC risk in adults. This 1:1 matched case-control study enrolled 644 hospital-based PLC patients and 644 community-based controls who were matched by sex and age, in Guangzhou, China. An interviewer-administered questionnaire and a food-frequency questionnaire were used to collect general information and dietary intake information. Conditional logistic regression showed a significantly inverse association between total choline and betaine intakes and PLC risk. The multivariable-adjusted odds ratios (ORs) and their 95% confidence intervals (CIs) for PLC for the top (vs. bottom) tertile were 0.34 (0.24–0.49; P -trend < 0.001) for total choline and 0.67 (0.48–0.93; P -trend = 0.011) for betaine. No significant association was observed between the intake of methionine and PLC risk (P > 0.05). For individual choline compounds, higher consumptions of free choline, glycerophosphocholine, phosphocholine, phosphatidylcholine and sphingomyelin were associated with a lower PLC risk (all P-trend < 0.05). The studied associations were not significantly modified by the folate intake (P-interactions: 0.488–0.890). Our findings suggest that higher choline and betaine intakes may be associated with a lower risk of PLC.
Similar content being viewed by others
Introduction
Primary liver cancer (PLC), one of the most highly malignant tumors with a poor prognosis, is the sixth most common cancer and the third leading cause of cancer-related mortality worldwide1. Additionally, half of the cases and deaths are estimated to occur in China1. Previous studies have shown that persistent infection with hepatitis B or C virus (HBV/HCV) is the leading cause of PLC2. Other established risk factors include aflatoxin-contaminated foods, excessive alcohol consumption, fatty liver, metabolic syndrome, and tobacco smoking3, 4. However, many studies have shown that dietary factors may also play an important role in the development of PLC5,6,7.
Choline, which is an essential nutrient, may protect against PLC through its effect on the one-carbon metabolism, structural integrity and signaling functions of cell membranes8. Choline can be irreversibly oxidized to betaine, providing one-carbon units in the conversion of homocysteine (Hcy) to methionine and the generation of the universal methyl donor S-adenosylmethionine (SAM)9. Previous studies have shown that one-carbon metabolism involves alterations in the biosynthesis of nucleotides and DNA methylation, which are thought to be implicated in carcinogenesis10, 11. Thus, it was hypothesized that the dietary intake of one-carbon related nutrients, such as choline, betaine and methionine, may play an important role in the development and progression of cancer.
Several prospective and retrospective studies have addressed choline, betaine and methionine intake in relation to cancer risk. For breast, colorectal and lung cancer, associations have been inverse12,13,14,15,16,17 or null18, 19. However, for colorectal adenoma20 and lethal prostate cancer21, an adverse association for choline has been reported. Reduced risks at higher intakes have also been reported for renal cell22, nasopharyngeal23 and pancreatic cancers24. However, for gynecological malignancies19, 25, associations have consistently been null. A recent meta-analysis showed that an increase of 100 mg/day of choline plus betaine intake might reduce the cancer incidence by 11% (0.89, 95% CI, 0.87 to 0.92)26. To the best of our knowledge, however, only one case-control study has examined the associations between the serum concentrations of betaine, choline, methionine and risk of hepatocellular carcinoma in the Chinese population in Shanghai27. No study has yet examined the associations between the dietary intake of choline, betaine and methionine and risk of PLC in humans. To address this issue, we investigated the associations between the intake of choline, betaine, and methionine and risk of PLC in a Chinese population.
Materials and Methods
Study population
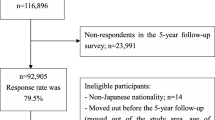
From September 2013 to January 2016, a 1:1 matched case-control study was conducted in Guangzhou, China. One thousand forty PLC cases aged 18–80 years were recruited from the Sun Yat-Sen University Cancer Center. All PLC cases were newly diagnosed within one month and were confirmed using tissue evaluation or liver Magnetic Resonance Imaging (MRI) according to the National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology: Hepatobiliary Cancers 28. We excluded PLC patients if they had any of the following conditions: (1) history of PLC or any other cancer (49 cases); (2) chronic diseases, such as hospital-confirmed diabetes, stroke, myocardial infarction or heart failure, kidney failure, chronic liver diseases, physical or mental disabled, or other diseases/conditions that may have changed their dietary habits or affected their routine activities within the previous 5 years (122 cases); (3) refusal to participate or incompletion of the survey (215 cases). We screened all inpatients with a PLC diagnosis indicated in the first page of the case report form for their eligibility during the study period. We further excluded those who completed the dietary survey with an implausible total energy intake (<500 or >3500 kcal per day for women and <700 or >4200 kcal per day for men) (10 cases). A total of 644 (559 men, 85 women) eligible patients were included in the analysis. Among the case patients, 292 (45.3%) were diagnosed by tissue biopsy, and 352 (54.7%) were diagnosed by MRI imaging. Of those with tissue evaluation, 272 (93.2%) were hepatocellular carcinoma (HCC) (both ICD-9 code 155.0 and ICD-O-2 Morphology code 8170/3), 16 (5.5%) were cholangiocellular carcinoma (CC) (both ICD-9 code 155.0 and ICD-O-2 Morphology code 8180/3), and 4 (1.4%) were the mixed type of HCC and CC (both ICD-9 code 155.0 and ICD-O-2 Morphology code 8180/3).
One-to-one matched control subjects by sex and age (5-year interval) were selected from the “apparently healthy” people participating in a community-based diet and health survey in urban Guangzhou at that time. In that survey, the following conditions had already been excluded and further confirmed by the interview in this study: the abovementioned chronic diseases, extreme dietary intake, liver cirrhosis and cancer. A total of 1297 subjects recruited through community advertisements, written invitations, flyers and subjects’ referrals was screened. If more than one subject could be matched to one of the cases, the best-matched one was chosen for the controls. The final analysis included 644 case-patients and 644 matched control subjects (men 559 pairs, women 85 pairs). Written informed consent was obtained from each individual. The study was approved by the Ethics Committee of the School of Public Health at Sun Yat-sen University and was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Data collection
A personal interview was conducted by a trained research interviewer for each subject using a structured questionnaire. Except for hospital-documented data (e.g., clinical characteristics, clinical laboratory tests and instrument examinations) for PLC cases, the same questionnaires were used to collect the dietary data, general and health-related information, and other covariates mentioned below for both cases and controls in this study. Information on the socio-demographic characteristics (sex, age, education level, occupation, and household income), lifestyle behaviors (smoking, alcohol use, and drinking tea), physical activities, relevant diseases, and medications used over the previous 12 months was collected during the interview. The education levels were grouped into primary school or below, secondary school, and high school or above. Household income was divided into four levels (≤2000, 2001–4000, 4001–6000 and >6000 yuan/month/person). Occupations were grouped into light, moderate, and heavy activity levels according to the labor intensity. Smoking or alcohol use was defined as individuals who had smoked at least one cigarette/day or consumed any alcoholic beverages at least one time/week in six consecutive months. Individuals who drink tea at least twice a week were considered tea drinkers. Anthropometrics, including weight, height, and circumference at the waist and hips, were determined. The body mass index (BMI, kg/m2) was calculated.
Dietary assessment
Dietary intake was ascertained using a quantitative 79-item Food Frequency Questionnaire (FFQ)23. Participants were asked to report the frequency (never, per year, per month, per week or per day) of intake and the portion size of their usually consumed foods over the past year before PLC was diagnosed for cases or interview for controls. We provided common food photographs of standard portion sizes to help the participants estimate the amount of food they had consumed. Daily food intake was calculated in grams per day. Total energy and individual nutrient content (folate, methionine and other related nutrients) were calculated based on the China Food Composition Table 2004 29. Daily choline and betaine intake were determined according to the food composition data analyzed by Zeisel et al. and the U.S. Department of Agriculture (USDA) Database30, 31. To evaluate choline intake, we calculated the contents of total choline and their components of free choline, phosphatidylcholine, phosphocholine, glycerophosphocholine and sphingomyelin. The energy-adjusted correlation coefficients for betaine and methionine ranged from 0.44 to 0.67 comparing the two FFQs six months apart and six 3-day dietary records23.
Statistical analyses
All analyses were performed for men and women combined. The dietary intakes of choline, betaine and methionine were adjusted for total calories using the residual method32. The Wilcoxon signed-rank or McNemar’s test was used to test differences in the socio-demographic and nutrient intakes between the case and control subjects, as appropriate. Energy-adjusted choline, betaine and methionine intake were categorized into tertiles based on the distribution of these compounds in controls. We also calculated the total risk score by simply summing each score of the studied components. We assigned 0 or 1 point to each half of the participants according to the median (0 = <median, 1 = ≥median) for choline and betaine with linear association with PLC risk, or according to the quartiles (0 for extreme quartiles [Q1 and Q4], 1 for the middle quartile [Q2 and Q3]) of methionine with a U-shaped association. The subjects were then classified into four groups according to their values of the total risk score (0, 1, 2, and 3, higher point lower risk).
Conditional logistic regression was used to estimate the odds ratios (OR) and corresponding 95% confidence intervals (CIs) of PLC for the middle and high (v. low) tertiles for the intake of total choline, individual choline-containing compounds betaine, and methionine. In addition to matching by age and sex, we adjusted for the log-transformed energy intake (kcal/day) in Model 1, and we further adjusted for BMI, education (primary school or below, secondary school, high school or above), occupation (light, moderate or heavy activity), household income (≤1500, 1501–3000, 3000–6000, and >6000 yuan/month/person), currently smoking (yes or no), currently drinking (yes or no), tea drinking (yes or no) (a rich source of antioxidative polyphenols), physical activity (MET-h/day), and dietary folate intake (μg/d) in Model 2. The linear trends across increasing tertiles were tested by assigning tertile values as continuous variables in the regression analyses. We selected and considered the above covariates as potential confounders based on the theoretical relevance in the multivariable models.
We conducted stratified analyses and used multivariable unconditional logistic regression models to determine whether the aforementioned associations were modified by the folate intake (<309 [tertile 1] v. ≥309 [tertile 2 and 3] μg/d in controls), lifestyle behaviors (smoking [Yes/No], alcohol use [Yes/No], tea drinking [Yes/No]), BMI (<25 v. ≥25 kg/m2), age [≤54 v. >54 year], physical activity [≤33.3 v. >33.3 MET· h per day], education level [low/high] (low = secondary school or below; high = high school or above), HBV infection [Yes/No], diagnosis [Tissue evaluation/MRI imaging] and to calculate the multiplicative interactions by including each interaction item. All of the data were analyzed using SPSS, version 19.0. P-values were based on 2-sided tests and were considered significant at <0.05.
Results
Characteristics of the participants
Some selected characteristics of the 644 case-control pairs (559 male pairs and 85 female pairs) are shown in Table 1. The median age was 54.0 years in the PLC group and 54.0 years in the control group. PLC patients have lower BMI, physical activity, education level and a lower proportion of tea drinking, but there was a higher proportion of smokers, alcohol users, and workers with moderate or heavy labor jobs than that of the controls (all P < 0.05). HBV infection was found in 81.2% of the cases.
Dietary intake
The PLC patients consumed a slightly lower intake of total energy (1523 v. 1566, kcal/d, P = 0.004) and had a lower energy-adjusted intake of betaine and total choline, but they had a higher intake of methionine than that of the controls (all P < 0.001). There was no significant difference in folate intake between the two groups. Of the total choline intake, phosphatidylcholine made the greatest contribution (61.8%), followed by free choline (17.4%), glycerophosphocholine (9.7%), phosphocholine (5.1%) and sphingomyelin (4.8%) in the controls (Table 1). The top five food sources for total choline were eggs (21.5%), streaky pork (13.0%), lean hogs (10.8%), Chinese flowering cabbage, mustard greens, collard greens and broccoli (8.7%) and poultry (4.0%). Grain products contributed to more than half of betaine intake (50.5%), followed by spinach. Rice, porridge and lean hogs were the main food sources of methionine (Supplemental Table S1).
Association between choline, betaine and methionine intake and PLC risk
There were significant dose-dependent, favorable associations between the intake of choline and betaine with the PLC risk in both Models 1 and 2 (all P -trend < 0.05). In Model 2, the ORs (95% CI) of PLC for the middle and high (vs. low) tertiles were 0.50 (0.36, 0.69) and 0.34 (0.24, 0.49) for total choline, and 0.67 (0.49, 0.92) and 0.67 (0.48, 0.93) for betaine. However, a significant association between the intake of methionine and PLC risk remained only in men (OR 1.71 [95% CI, 1.22, 2.39]) (Supplemental Table S3), but not in total subjects (OR 1.27 (95% CI, 0.93, 1.73)) in Model 2. (Table 2).
We further analyzed the association between individual choline compounds and PLC risk (Table 3). All of the individual choline compounds (free choline, glycerophosphocholine, phosphocholine, phosphatidylcholine, and sphingomyelin) were inversely associated with the risk of PLC (all P-trend < 0.01) in Model 2.
Total risk score and PLC risk
Both Model 1 and Model 2 showed a very significantly graded association between higher scores and a lower risk of PLC. The ORs (95% CI) of PLC for the categories of a total risk score of 0, 1, 2 and 3 were 1.00, 0.57 (0.38, 0.84), 0.31 (0.21, 0.47), and 0.21 (0.13, 0.34), respectively. The association tended to be more significant than those of each individual one-carbon-related nutrient (Table 2).
Stratified and sensitivity analyses
We found that the favorable associations between the intake of betaine, total choline and PLC risk were not significantly different according to the subgroups of folate intakes (<309 v ≥309 μg/d) (P -interaction = 0.238–0.618) (Table 4), gender, education, BMI, physical activity, smoking, alcohol drinking, and tea drinking (p-interactions: all >0.05/36 tests). However, the unfavorable association between higher methionine and PLC risk tended to be significant in older subjects (age: >54 vs. ≤54 years) (p-interaction < 0.001). Because there were no data of the HBV status and PLC tissue evaluation in the control group, we separately analyzed the relevant associations according to the PLC subjects’ status of HBV infectious (yes/no) and tissue evaluation (vs. MRI) using the same 644 control subjects. Similar trends were observed in the PLC subjects with/without HBV or using tissue evaluation. (Supplemental Table S2).
Discussion
In this case-control study, we found that a higher intake of total choline, as well as that of betaine, was associated with a reduced PLC risk. A high intake of methionine tended to be associated with a greater PLC risk. To the best of our knowledge, this was the first study to report the favorable association between choline and betaine consumption with PLC risk in humans. Our findings suggested that increasing the intakes of choline and betaine may be associated with a lower risk of PLC in humans.
Many studies have examined the associations between the consumption of dietary choline and betaine with cancer risk in animal models and humans. In the 1980s, it was reported that choline- and methionine-deficient diets could independently act as a complete carcinogen to develop hepatocellular carcinoma in rats without the administration of carcinogens33, 34. Some13, 14, 17, 23, 35 but not all18, 20, 21, 25 human studies have found a favorable association between dietary or circulating levels of choline and betaine and the risk of some cancers. A case-control study, nested within the European Prospective Investigation into Cancer and Nutrition (EPIC)35, including 1,367 colorectal cancer (CRC) cases and 2,323 controls, showed an inverse association between the plasma choline concentration and CRC risk in women (but not in men) and between the plasma betaine level and CRC risk in people with a lower plasma folate concentration35. Favorable associations between the dietary intakes of choline and betaine were also observed with respect to the risks of nasopharyngeal carcinoma (NPC)23, breast cancer13 and lung cancer14, although null18, 20, 25 or adverse18, 21 associations were also found in some other cancer studies. To date, only one case-control study has reported the relationship between the levels of choline or betaine in the diet or blood and the risk of hepatocellular carcinoma27. A recent meta-analysis showed that the pooled relative risks (95% CIs) of cancer for the highest versus lowest range of dietary intake were 0.82 (0.70 to 0.97) for choline, 0.86 (0.76 to 0.97) for betaine, and 0.60 (0.40 to 0.90) for choline and betaine combined26. Generally, consistent with the results of many other cancer studies, our findings support the hypothesis that a greater consumption of choline and betaine is associated with a lower risk of PLC in humans.
Regarding the individual components of the total dietary choline, phosphatidylcholine contributed more than 60% of the total choline, which was followed by free choline, glycerophosphocholine, phosphatidylcholine and sphingomyelin. We observed a significantly favorable association between consumption and PLC risk for these five components in our study. Favorable associations of these five components with total choline were also observed with respect to the risks of NPC, breast cancer and colorectal cancer in three different case-control studies that were conducted in the same geographic area12, 13, 23; although an inverse association with breast cancer risk was only observed for free choline intake in a cohort study36. Different choline components have different characteristics and varied food sources. Free choline, phosphocholine and glycerophosphocholine are water soluble and rich in cruciferous vegetables, whereas the other two types (phosphatidylcholine and sphingomyelin) are fat soluble and are mainly found in egg and animal foods (Supplemental Table 1). The strong internal consistency of the results for the different choline types that are present in different foods suggests that choline, rather than other co-existing food components, is most likely responsible for the favorable association between the total choline intake and PLC risk.
Biological explanations for the beneficial associations between high choline and betaine intake and PLC risk are still unclear. One potential mechanism that mediates the relationship between choline, betaine intake and primary liver cancer may be from their potential role in one-carbon metabolism. One-carbon metabolism can affect DNA methylation levels, particularly methylation at the CpG site, which plays an important role in genome regulation37, 38. The disruption of DNA methylation and impaired DNA repair induced by the deficiency of methyl donors (choline, betaine or methionine) in one-carbon metabolism was considered to contribute to the underlying mechanism of carcinogenesis39. Animals that are fed diets that lack choline and/or folic acid could induce profound changes in the expression of genes in the liver40 and development of hepatocellular carcinoma41. Next, choline, especially phosphatidylcholine, which is a predominant component of phospholipids in VLDL cholesterol, is necessary for TG transport from the liver, which may protect against liver fat accumulation42. On the other hand, some studies have suggested that high choline or betaine intake would improve the mitochondrial membrane and protect against oxidative stress and inflammation43, 44. Both fat accumulation and oxidative stress seem to be critical factors in the pathogenesis of chronic liver injury, including liver cancer.
Methionine, which is an indispensable amino acid, plays many key roles in mammalian metabolism, such as in protein synthesis, oxidative stress protection, DNA methylation and polyamine synthesis45. Conflicting results were observed between methionine and human cancers. In the Shanghai Women’s Health Study, subjects with a higher intake of methionine (>vs. <the median) had a 22% lower risk (HR: 0.78; 95% CI: 0.60–0.99) of lung cancer16. A prospective study comprising 81,922 individuals in a Swedish population with a mean follow-up of 7.2 years also found that a higher methionine intake could reduce the risk of pancreatic cancer24. Similar favorable associations between methionine intake and breast cancer were observed in a case-control study in women with positive estrogen receptor (ER+) status15. However, there were null associations between the dietary intake of methionine and cancer risk in the breast, endometrium, ovary, colorectal and lung in a large cohort of Canadian women who were followed-up for an average of 16.4 years19. Moreover, an adverse relationship between serum methionine and hepatocellular carcinoma risk was found in a nested case-control study in a cohort of 18,244 men in Shanghai27. In the present study, no significant relationship was observed between the dietary intake of methionine and PLC risk, and this result needs to be confirmed by more studies.
Folate and choline (through betaine) share methylation pathways (Supplemental Figure S1). Studies among animals and humans have shown that the folate and choline pathways may affect each other. Rats that were fed a folate-deficient diet showed depletion of the hepatic choline concentrations46. In the Framingham Offspring Study, higher intake levels of dietary choline and betaine were related to lower tHcy concentrations, which were limited to participants with low folate intake (<250 μg/d; P-interaction < 0.0001)47. In this study, however, no significant interactions were observed between folate intake and the intake of choline, betaine and methionine. Further studies are needed to clarify whether choline and folate may exert complementary cancer prevention effects.
Some limitations of our study should be considered when interpreting the results. First, the case-control study design prevents conclusions concerning causality. We could not eliminate recall bias, i.e. knowledge of PLC diagnosis affecting dietary reporting by cases, or reverse causation, i.e. the disease affecting actual dietary intake, but we attempted to account for the design weaknesses in several ways. We enrolled only incident PLC cases, diagnosed within 1 month of survey. We used a food frequency questionnaire to assess dietary intake over the relatively long term (one year prior to PLC diagnosis), and we calculated energy-adjusted choline, betaine and methionine intakes to account for possible appetite changes due to PLC. Furthermore, recall bias is unlikely to be a problem, because the public was unfamiliar with the studied risk factors choline, betaine and methionine, which come from a large variety of “healthy” and “unhealthy” food sources. We also excluded people diagnosed with a major chronic disease within 5 years prior to survey, which probably minimized substantial dietary change. However, the cases and controls were thus healthier than the source population, which might lower the generalizability of our results. Our findings require further verification in a large sample of prospective cohort studies. Second, random recall error of habitual diets may be unavoidable in retrospective studies, although we used a large number of food photographs with standardized portion sizes to help participants estimate the amount of food they consumed to control for potential random errors and bias due to their recall ability. However, the potential bias was unlikely to be differential because the public was unfamiliar with the studied risk factors for choline, betaine and methionine with a large variety of different food sources, whereas non-differential recall bias tended to attenuate the association to null. Therefore, it is unlikely that we overestimated the favorable association in this study. Third, PLC patients were recruited from Sun Yat-Sen University Cancer Center, while the controls were recruited from local communities, which may influence the representativeness of the results. However, there were no significant differences in the studied associations between the pairs with the local cases and nonlocal cases (P-interactions between geographic area and choline/betaine: 0.332/0.838), suggesting the influence of different geographic regions would be limited. Fourth, case-control studies are prone to various selection biases. We reduced the prevalence-incidence bias by only including incident cases. Case admission and detection were unlikely to be related to the intake of choline, betaine, or methionine mainly consumed from usual foods. The studied PLC cases included in this study had a similar age (52 vs. 52* years, *this study), proportion of males (86% vs. 86.8%), and proportion with HBV infection (77% vs. 71.3%) but a relatively higher proportion of tobacco use (36% vs. 53.6%) and alcohol drinking (24% vs 32.3%), compared to a large HCC study containing 8,683 patients from 10 cities in China48 However, the studied associations were not significantly modified by BMI, education level, physical activity, smoking, alcohol drinking, tea drinking and HBV status, although we could not exclude the differences between the studied and target populations due to the convenient sampling. Fifth, we could not exclude the possible influence of HBV infection due to the lack of data in the controls. HBV infection was unlikely to be a significant confounder because no statistical association was found between the intake of choline, betaine and methionine and HBV infection among the cases (all P > 0.10). Sensitivity analysis showed that the studied associations were similar in patients with/without HBV infection. Finally, the limited study size did not allow us to obtain precise results in women.
In conclusion, our study suggested that higher intakes of dietary choline and betaine were inversely associated with primary liver cancer risk. Prospective studies are needed to confirm these findings.
References
Torre, L. A. et al. Global cancer statistics, 2012. CA Cancer J Clin 65, 87–108 (2015).
Parkin, D. M. The global health burden of infection-associated cancers in the year 2002. Int J Cancer 118, 3030–3044 (2006).
Turati, F. et al. Alcohol and liver cancer: a systematic review and meta-analysis of prospective studies. Ann Oncol 25, 1526–1535 (2014).
Welzel, T. M. et al. Metabolic syndrome increases the risk of primary liver cancer in the United States: a study in the SEER-Medicare database. Hepatology 54, 463–471 (2011).
Fedirko, V. et al. Consumption of fish and meats and risk of hepatocellular carcinoma: the European Prospective Investigation into Cancer and Nutrition (EPIC). Ann Oncol 24, 2166–2173 (2013).
Kurozawa, Y. et al. Dietary habits and risk of death due to hepatocellular carcinoma in a large scale cohort study in Japan. Univariate analysis of JACC study data. Kurume Med J 51, 141–149 (2004).
Talamini, R. et al. Food groups and risk of hepatocellular carcinoma: A multicenter case-control study in Italy. International journal of cancer. J Int Cancer 119, 2916–2921 (2006).
Zeisel, S. H. Choline: critical role during fetal development and dietary requirements in adults. Annu Rev Nutr 26, 229–250 (2006).
Zeisel, S. H. & Blusztajn, J. K. Choline and human nutrition. Annu Rev Nutr 14, 269–296 (1994).
Kim, Y. I. Folate and carcinogenesis: evidence, mechanisms, and implications. J Nutr Biochem 10, 66–88 (1999).
Pandey, S. et al. Nucleotide biosynthesis arrest by silencing SHMT1 function via vitamin B6-coupled vector and effects on tumor growth inhibition. Biomaterials 35, 9332–9342 (2014).
Lu, M. S. et al. Choline and betaine intake and colorectal cancer risk in Chinese population: a case-control study. PloS one 10, e0118661, doi:10.1371/journal.pone.0118661 (2015).
Zhang, C. X. et al. Choline and betaine intake is inversely associated with breast cancer risk: a two-stage case-control study in China. Cancer Sci 104, 250–258 (2013).
Ying, J. et al. Associations between dietary intake of choline and betaine and lung cancer risk. PloS one 8, e54561, doi:10.1371/journal.pone.0054561 (2013).
Yang, D. et al. Dietary intake of folate, B-vitamins and methionine and breast cancer risk among Hispanic and non-Hispanic white women. PloS one 8, e54495, doi:10.1371/journal.pone.0054495 (2013).
Takata, Y. et al. Dietary B vitamin and methionine intakes and lung cancer risk among female never smokers in China. Cancer Causes Control 23, 1965–1975 (2012).
Myte, R. et al. Components of One-carbon Metabolism Other than Folate and Colorectal Cancer Risk. Epidemiology 27, 787–796 (2016).
Lee, J. E. et al. Choline and betaine intake and the risk of colorectal cancer in men. Cancer Epidemiol Biomarkers Prev 19, 884–887 (2010).
Kabat, G. C., Miller, A. B., Jain, M. & Rohan, T. E. Dietary intake of selected B vitamins in relation to risk of major cancers in women. Br J Cancer 99, 816–821 (2008).
Cho, E. et al. Dietary choline and betaine and the risk of distal colorectal adenoma in women. J Natl Cancer Inst 99, 1224–1231 (2007).
Richman, E. L. et al. Choline intake and risk of lethal prostate cancer: incidence and survival. Am J Clin Nutr 96, 855–863 (2012).
Cho, E., Giovannucci, E. L. & Joh, H. K. Nutrients related to one-carbon metabolism and risk of renal cell cancer. Cancer Causes Control 24, 373–382 (2013).
Zeng, F. F. et al. Choline and betaine intakes are associated with reduced risk of nasopharyngeal carcinoma in adults: a case-control study. Br J Cancer 110, 808–816 (2014).
Larsson, S. C., Giovannucci, E. & Wolk, A. Methionine and vitamin B6 intake and risk of pancreatic cancer: a prospective study of Swedish women and men. Gastroenterology 132, 113–118 (2007).
Kotsopoulos, J., Hankinson, S. E. & Tworoger, S. S. Dietary betaine and choline intake are not associated with risk of epithelial ovarian cancer. Eur J Clin Nutr 64, 111–114 (2010).
Sun, S. et al. Choline and betaine consumption lowers cancer risk: a meta-analysis of epidemiologic studies. Sci Rep 6, 35547 (2016).
Butler, L. M. et al. Prediagnostic levels of serum one-carbon metabolites and risk of hepatocellular carcinoma. Cancer Epidemiol Biomarkers Prev 22, 1884–1893 (2013).
Benson, A. B. 3rd et al. NCCN clinical practice guidelines in oncology: hepatobiliary cancers. J Natl Compr Canc Netw 7, 350–391 (2009).
Zhang, H. et al. Reproducibility and relative validity of a semi-quantitative food frequency questionnaire for Chinese pregnant women. Nutr J 14, 56 (2015).
Leung, K. In Molecular Imaging and Contrast Agent Database (MICAD) (2004).
Zeisel, S. H., Mar, M. H., Howe, J. C. & Holden, J. M. Concentrations of choline-containing compounds and betaine in common foods. J Nutr 133, 1302–1307 (2003).
Willett, W. & Stampfer, M. J. Total energy intake: implications for epidemiologic analyses. Am J Epidemiol 124, 17–27 (1986).
Ghoshal, A. K. & Farber, E. The induction of liver cancer by dietary deficiency of choline and methionine without added carcinogens. Carcinogenesis 5, 1367–1370 (1984).
Mikol, Y. B., Hoover, K. L., Creasia, D. & Poirier, L. A. Hepatocarcinogenesis in rats fed methyl-deficient, amino acid-defined diets. Carcinogenesis 4, 1619–1629 (1983).
Nitter, M. et al. Plasma methionine, choline, betaine, and dimethylglycine in relation to colorectal cancer risk in the European Prospective Investigation into Cancer and Nutrition (EPIC). Ann Oncol 25, 1609–1615 (2014).
Xu, X. et al. High intakes of choline and betaine reduce breast cancer mortality in a population-based study. FASEB J 23, 4022–4028 (2009).
de Vogel, S. et al. Dietary methyl donors, methyl metabolizing enzymes, and epigenetic regulators: diet-gene interactions and promoter CpG island hypermethylation in colorectal cancer. Cancer Causes Control 22, 1–12 (2011).
Lister, R. et al. Human DNA methylomes at base resolution show widespread epigenomic differences. Nature 462, 315–322 (2009).
Futscher, B. W. et al. Aberrant methylation of the maspin promoter is an early event in human breast cancer. Neoplasia 6, 380–389 (2004).
Glen, C. D., McVeigh, L. E., Voutounou, M. & Dubrova, Y. E. The effects of methyl-donor deficiency on the pattern of gene expression in mice. Mol Nutr Food Res 59, 501–506 (2015).
Pogribny, I. P., James, S. J. & Beland, F. A. Molecular alterations in hepatocarcinogenesis induced by dietary methyl deficiency. Mol Nutr Food Res 56, 116–125 (2012).
Cole, L. K., Vance, J. E. & Vance, D. E. Phosphatidylcholine biosynthesis and lipoprotein metabolism. Biochim Biophys Acta 1821, 754–761 (2012).
Banni, S. et al. Free radicals and lipid peroxidation in liver of rats kept on a diet devoid of choline. Free Radic Res Commun 7, 233–240 (1989).
da Costa, K. A., Niculescu, M. D., Craciunescu, C. N., Fischer, L. M. & Zeisel, S. H. Choline deficiency increases lymphocyte apoptosis and DNA damage in humans. Am J Clin Nutr 84, 88–94 (2006).
Cavuoto, P. & Fenech, M. F. A review of methionine dependency and the role of methionine restriction in cancer growth control and life-span extension. Cancer treat rev 38, 726–736 (2012).
Kim, Y. I. et al. Severe folate deficiency causes secondary depletion of choline and phosphocholine in rat liver. J Nutr 124, 2197–2203 (1994).
Cho, E. et al. Dietary choline and betaine assessed by food-frequency questionnaire in relation to plasma total homocysteine concentration in the Framingham Offspring Study. Am J Clin Nutr 83, 905–911 (2006).
Park, J. W. et al. Global patterns of hepatocellular carcinoma management from diagnosis to death: the BRIDGE Study. Liver Int 35, 2155–2166 (2015).
Acknowledgements
We are grateful for the help from the doctors and nurses in Sun Yat-sen University Cancer Center to facilitate the recruitment and interviews. This study was jointly supported by the National Natural Science Foundation of China (NO. 81472966 and NO. 81273050) and Key Program of the National Natural Science Foundation of Guangdong, China (NO. 2015A030311035).
Author information
Authors and Affiliations
Contributions
H.L.Z. conceived and designed the study and had the primary responsibility for the final content; X.L.C. and R.F.Z. collected and analyzed the data and wrote the manuscript; Z.G.Z., Y.J.Z., Q.Y.L. and G.C.L. carried out the recruitment and interviewing and collected the data; Y.M.C. gave critical comments. All of the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors declare that they have no competing interests.
Additional information
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Zhou, Rf., Chen, XL., Zhou, Zg. et al. Higher dietary intakes of choline and betaine are associated with a lower risk of primary liver cancer: a case-control study. Sci Rep 7, 679 (2017). https://doi.org/10.1038/s41598-017-00773-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-017-00773-w
- Springer Nature Limited