Abstract
The kidney tubules constitute two-thirds of the cells of the kidney and account for the majority of the organ’s metabolic energy expenditure. Acute tubular injury (ATI) is observed across various types of kidney diseases and may significantly contribute to progression to kidney failure. Non-invasive biomarkers of ATI may allow for early detection and drug development. Using the SomaScan proteomics platform on 434 patients with biopsy-confirmed kidney disease, we here identify plasma biomarkers associated with ATI severity. We employ regional transcriptomics and proteomics, single-cell RNA sequencing, and pathway analysis to explore biomarker protein and gene expression and enriched biological pathways. Additionally, we examine ATI biomarker associations with acute kidney injury (AKI) in the Kidney Precision Medicine Project (KPMP) (n = 44), the Atherosclerosis Risk in Communities (ARIC) study (n = 4610), and the COVID-19 Host Response and Clinical Outcomes (CHROME) study (n = 268). Our findings indicate 156 plasma proteins significantly linked to ATI with osteopontin, macrophage mannose receptor 1, and tenascin C showing the strongest associations. Pathway analysis highlight immune regulation and organelle stress responses in ATI pathogenesis.
Similar content being viewed by others
Introduction
The tubules play a crucial role in optimal functioning of the kidneys, and their impairment is responsible for substantial morbidity and mortality from conditions such as acute kidney injury (AKI) and progressive chronic kidney disease (CKD) culminating in kidney failure1,2. Tubular lesions on histopathology have been described across virtually all forms of chronic and acute kidney diseases. The kidney tubules comprise > 60% of the kidneys’ cellular mass and have among the highest density of mitochondria and metabolic workloads of any cell type in the body3,4. The high energy requirements of the tubules result from ATP-consuming reabsorption of over 99% of filtered sodium, glucose, and amino acids from the glomerular ultrafiltrate3. Several studies suggest that kidney function decline is more closely correlated with tubulointerstitial damage than glomerular injury5,6,7.
Acute tubular injury (ATI) describes a combination of pathologic findings, including tubular dilatation and epithelial flattening, tubular cell sloughing, and loss of nuclei, that reflect the morphologic responses of the tubules to a diverse range of insults8,9,10. ATI stands as a hallmark in the diagnosis of AKI but also manifests in the context of CKD10. Episodes of ATI and subsequent maladaptive repair can lead to the development and progression of CKD2,11. Therapies focusing on preventing or treating the consequences of ATI are lacking, but could play key roles in preventing morbidity and mortality from various kidney diseases.
Several studies have illustrated how large-scale proteomics approaches can identify important protein markers to prognosticate the risk of adverse clinical outcomes in patients with kidney disease12,13,14,15,16,17,18. Few studies have used this approach to determine non-invasive correlates of kidney histopathology, which could potentially lead to the identification of new therapeutic targets19.
In the present study, we used an unbiased proteomics assay to measure 6592 plasma proteins in the Boston Kidney Biopsy Cohort (BKBC), a cohort study of individuals with biopsy-confirmed kidney disease and adjudicated semi-quantitative assessment of ATI. We first assessed associations of each protein biomarker with ATI severity and determined enriched pathways that may have biological relevance for ATI pathogenesis. We then investigated the expression of biomarker proteins and corresponding biomarker-genes in regional proteomics and transcriptomics as well as single-cell RNA sequencing (scRNA-seq) from human kidney. Lastly, we explored associations between our findings and the development of AKI in three additional cohort studies with available proteomic profiling: the Kidney Precision Medicine Project (KPMP), the Atherosclerosis Risk in Communities (ARIC) study, and a cohort of critically ill patients from an intensive care unit (COVID-19 Host Response and Clinical Outcomes (CHROME)) study.
Results
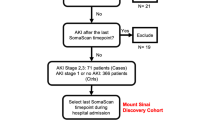
As outlined in Fig. 1, we analyzed data from (i) individuals with biopsy-confirmed ATI, (ii) individuals biopsied for AKI and healthy controls, (iii) individuals from the general population at risk for developing AKI, and (iv) critically ill individuals at risk of severe AKI.
Identification and characterization of plasma biomarkers of ATI
Baseline characteristics of the BKBC study cohort are shown in Table 1. The mean age was 54 ± 16 years and 48% were women. The mean eGFR was 51 ± 33 ml/min/1.73m2 and the median proteinuria (IQR) was 1.4 (0.3, 3.9) g/g creatinine. The most common primary clinicopathologic diagnoses were glomerulopathies (40%), diabetic nephropathy (16%), advanced chronic changes (15%), vascular disease (12%), and tubulointerstitial disease (11%). Figure 2a shows the breakdown of ATI severity by clinicopathologic diagnosis: 53% of BKBC participants had no ATI, 30% had mild ATI, 13% had moderate ATI, and 4% had severe ATI.
a Distribution of semiquantitative severity scores for ATI by clinicopathologic diagnostic category in the Boston Kidney Biopsy Cohort (BKBC), Study 1. b Circulating plasma proteins associated with ATI severity in native kidney biopsy specimens. Beta coefficients are derived from multivariable linear regression models, adjusted for age, sex, race, and eGFR. The horizontal dotted line shows the Bonferroni-adjusted significance threshold. P-values are two-sided. ATI: acute tubular injury, BKBC: Boston Kidney Biopsy Cohort, eGFR: estimated glomerular filtration rate, GN: glomerulonephritis, GP: glomerulopathy.
Associations between plasma biomarkers and ATI severity are shown in Fig. 2b and Supplemental Data 1. After multivariable adjustment and correction for multiple testing, 156 unique proteins (170 aptamers; some proteins are measured by 2 or more aptamers) were associated with ATI. Among those, higher levels of 126 proteins and lower levels of 30 proteins were independently associated with ATI severity. Higher levels of the following plasma biomarkers were associated with greater ATI severity (top 5 findings in the order of level of significance): osteopontin (SPP1), macrophage mannose receptor 1 (MRC-1), tenascin C (TNC), netrin-4 (NTN4), and marginal zone B- and B1-cell-specific protein (MZB1). The top five plasma proteins negatively associated with ATI severity were plasma serine protease inhibitor (SERPINA5), cholinesterase (BCHE), neuropeptide S (NPS), kallistatin (SERPINA4) and alpha-2-HS-glycoprotein (AHSG). Additional proteins associated with ATI with biological relevance in kidney disease include kidney injury molecule-1 (KIM-1; HACVR1), WAP four-disulfide core domain protein 2 (HE4; WFDC2), growth/differentiation factor-15 (GDF-15), serum amyloid A-1 protein (SAA1), and serum amyloid A-2 protein (SAA2).
Of the 156 ATI biomarkers identified in the BKBC, 78 were analyzed within the KPMP regional proteomics dataset. Comparison with glomerular expression revealed elevated protein expression of several ATI biomarkers in the tubulointerstitium (Fig. 3a). When comparing regional protein expression between individuals with AKI and healthy controls, we observed protein expression of eight ATI biomarkers. All except one (apolipoprotein A-1; APOA1) showed protein expression in direction concordant with greater ATI severity as observed in Study 1 (BKBC). We observed protein expression of our top ATI biomarker findings, osteopontin (SPP1), macrophage mannose receptor 1 (MRC-1), and tenascin C (TNC), in the tubulointersitium of kidneys with AKI (Fig. 3b). Utilizing regional transcriptomics data, 42 of the 156 ATI biomarkers were found to be expressed in kidney tubules, 29 of which showed higher tubular compared to glomerular expression. We observed the highest tubular expression for WFDC2, GDF15, and SPP1 when compared to glomerular expression (Fig. 3c). Detailed expression of these three markers in different kidney cell types is shown in Supplemental Fig. 1. We observed prominent expression of WFDC2, GDF15, and SPP1 in cell clusters of the thick ascending limb. SPP1 was also strongly expressed in distal convoluted tubule cell clusters, while GDF15 and WFDC2 expression was prominent in clusters of connecting tubule cells.
a ATI biomarkers with elevated protein expression comparing tubulointerstitial to glomerular levels in KPMP regional proteomics data (AKI, CKD, HRT combined). b Protein expression of ATI biomarkers in the tubulointerstitium of individuals with AKI compared to healthy controls using Wilcoxon Rank Sum Test and Benjamini–Hochberg FDR to account for multiple comparisons. Shown are all proteins with a two-sided p < 0.05. c Gene expression of ATI biomarkers in KPMP regional transcriptomics data (AKI, CKD, HRT combined) using ANOVA. Two-sided p-values are adjusted for multiple comparisons using Benjamini–Hochberg FDR. d Pathway analysis of biomarkers associated with ATI severity. The top-ranked pathways are listed in black (one-sided p < 0.05) and gray (one-sided p < 0.25) following Benjamini–Hochberg correction. ATI: acute tubular injury, AKI: acute kidney injury, CKD: chronic kidney disease, HRT: healthy reference tissue, NES: normalized enrichment score, R-HSA: Reactome-Homo sapiens, GO: Gene Ontology, COPII: Coat Protein II.
Of the 156 unique proteins linked to ATI, several play roles in the regulation of the immune system and intracellular pathways. We identified seven key pathways (all p < 0.05) with relevance for ATI pathogenesis. Of these, the top-ranked pathways were: ‘Intracellular Organelle Lumen’, ‘Endoplasmic Reticulum Lumen’, and ‘Immune System’ (Fig. 3d). Additional pathways that had immunoregulatory capacities included ‘Interactions Between Lymphoid and Non-Lymphoid Cells’ and ‘Neutrophil Degranulation.’ Proteins involved in these pathways included several cytokines, interleukins, members of the TNF receptor superfamily, and regulators of the complement cascade (Supplemental Data 2).
Difference of ATI biomarker levels in individuals with AKI and healthy controls
In the KPMP study, we analyzed plasma concentrations of the 156 ATI biomarkers comparing individuals with AKI to healthy subjects. After Bonferroni correction, 93 unique ATI biomarkers had significantly different plasma levels in AKI vs. healthy plasma (Fig. 4a). Of those, 77 ATI biomarkers were elevated and 16 were lower in individuals with AKI. The direction of these changes in all 93 biomarkers was consistent with the observations made in the BKBC (Fig. 4d). We observed the largest differences comparing AKI to healthy plasma levels for kidney injury molecule-1 (HACVR1), WAP four-disulfide core domain protein 2 (WFDC2), and growth/differentiation factor-15 (GDF-15).
a Comparison of ATI biomarker levels between healthy participants and those with AKI in the KPMP study using Student’s t-test. b Plasma ATI biomarkers associated with incident AKI in ARIC. Hazard ratios are derived from Cox proportional hazards models, adjusted for age, sex, Black race, hypertension, diabetes, systolic blood pressure, current smoking, eGFR, and log(UACR). p-values were calculated using the Wald test. c Plasma ATI biomarkers associated with severe AKI 7 days after ICU admission in a cohort of critically ill patients (CHROME). Odds ratios are derived from multivariable logistic regression models, adjusted for age, sex, and COVID-19 status. p-values were calculated using the Wald test. The horizontal dotted lines (a–c) show the Bonferroni-adjusted significance thresholds. p-values (a–c) are two-sided. d The heatmap illustrates the associations of 156 ATI biomarkers with specific outcomes across studies. Each biomarker is represented by a color: red signifies a statistically significant positive association, blue denotes a statistically significant negative association, and gray indicates that the biomarker was not available in the respective cohort. The biomarkers are organized based on their frequency of associations across studies and are further ordered according to the magnitude of their association with ATI severity in Study 1 (BKBC). ARIC: Atherosclerosis Risk in Communities study, ATI: acute tubular injury, BKBC: Boston Kidney Biopsy Cohort, CHROME: COVID-19 Host Response and Clinical Outcomes study, eGFR: estimated glomerular filtration rate, KPMP: Kidney Precision Medicine Project, UACR: urine albumin to creatinine ratio.
Associations of ATI biomarkers with incident AKI
The baseline characteristics of ARIC participants are shown in Supplemental Data 3. Over a median of 6.8 years, 1084 ARIC participants developed AKI. Of the 156 unique proteins identified as ATI biomarkers in Study 1 (BKBC), 122 proteins were measured in ARIC. Of those, 35 were significantly associated with higher risks and 10 with lower risks of incident AKI after multivariable adjustment (Fig. 4b and Supplemental Data 4). The direction of these associations was found to be consistent (Fig. 4d): the same 35 proteins associated with elevated risks of AKI in ARIC were also linked to more severe ATI in the BKBC. Among those were osteopontin (SPP1), tenascin C (TNC), as well as WAP four-disulfide core domain protein 2 (HE4; WFDC2) and growth/differentiation factor-15 (GDF-15). Similarly, the 10 proteins associated with lower risks of AKI in ARIC corresponded to less severe ATI in the BKBC (Fig. 4d).
Associations of ATI biomarkers with severe AKI
Among the 268 critically ill patients enrolled into the CHROME study, 34 developed severe AKI on day 7 after ICU admission (Supplemental Data 5). Of the previously identified ATI biomarkers, 38 unique markers were significantly associated with severe AKI after adjustment for age, sex, and COVID-19 status. Of those, 36 were associated with higher risks and 2 with lower risks of severe AKI (Fig. 4c, d, and Supplemental Data 6) and were in a direction concordant with that observed in Study 1 (BKBC). Thirteen ATI biomarkers associated with severe AKI were also associated with higher risks of incident AKI in the general population (Study 3, ARIC) and had higher plasma levels in patients with AKI compared to healthy controls (Study 2, KPMP). These included osteopontin (SPP1), tenascin C (TNC), and mannose-binding lectin 2 (LMAN2), among others (Fig. 4d).
Discussion
This study provides an assessment of the plasma proteome in a cohort of individuals with biopsy-confirmed ATI followed by further study of the proteomic results in external cohorts. We identified biomarkers of ATI severity, assessed their tubular expression, and conducted pathway enrichment analyses that highlighted immune regulation and organelle stress responses as central mechanisms in ATI pathogenesis. Additionally, we expanded our investigation to examine associations between our findings and the development or prognosis of AKI in three distinct cohorts with available proteomic data.
Previous proteomics research has mainly centered on analyzing the plasma proteome to assess risks of adverse clinical outcomes in individuals with kidney disease18,20,21,22. Fewer studies have utilized proteomics to interrogate associations between circulating proteins and kidney histopathologic changes including ATI19,23,24. Kidney tubular injury can lead to a significant decrease in kidney function. While it is commonly linked to the clinical syndrome of AKI, it may also influence the onset and progression of CKD25. Some of the individual proteins we investigated have previously been identified to be associated with ATI. Among those, plasma KIM-1 stands as the most extensively studied marker12,26. In prior studies using both ELISA and proximity extension assay (Olink platform)27, we observed consistent associations of plasma KIM-1 with the degree of ATI19,28. Many other findings from the present study unveil new insights that may pave the foundation for future investigation.
The biomarker most strongly associated with more severe ATI was osteopontin (OPN; SPP1). OPN is a 44 kD glycoprotein predominantly secreted in bone and epithelial tissues. In the kidney, expression increases during injury29,30. Recent mechanistic studies have identified circulating OPN derived from kidney tubule cells as a key mediator of AKI-induced acute lung injury31. Another study showed that plasma OPN levels in individuals recovering from AKI were significantly higher when compared to individuals with irreversible loss of kidney function after AKI32. In the setting of CKD, higher serum OPN levels were associated with worse kidney function and greater risk of kidney failure and death33. Our results provide further evidence for a strong association of OPN with tubular injury and suggest its potential as a specific tool to assess for the degree of ATI. Similarly, we found a consistent relationship between higher tenascin C (TNC; TNC) levels, more severe ATI, and greater risk of AKI across cohorts. TNC, an extracellular matrix protein, is upregulated in the tubulointerstitium of CKD patients and has been shown to be involved in the transition from AKI to CKD by impairing tubular integrity through αvβ6 integrin signaling34.
We also observed strong associations between ATI severity and human epididymis protein-4 (HE4; WFDC2) and growth differentiation factor-15 (GDF-15; GDF-15). Both markers had higher levels in AKI, were associated with incident AKI, and were also among the top markers expressed in kidney tubules. HE4 is a serine protease inhibitor that has recently been shown to promote kidney fibrosis by inhibiting the degradation of type I collagen35. Studies also found a positive correlation between higher HE4 levels and more severe kidney fibrosis36,37. A prior investigation in diabetic kidney disease demonstrated that higher HE4 levels associated with increased risks of future kidney function decline38. Our study adds that HE4 may play an important role in the development of ATI. Additionally, the upregulation of this marker in both CKD (as shown in prior studies) and AKI underscores the interconnectedness between the two conditions and may provide additional evidence for the importance of kidney tubular injury in CKD progression12,13,26,39.
GDF-15 is a member of the TGF-β superfamily and has recently been described as a marker of oxidative stress in mitochondrial diseases40,41. In the kidney, GDF-15 exhibits a range of functions that are variably antagonistic or complementary, contingent upon the cellular state and surrounding microenvironment42,43,44,45. While some studies have found a potentially nephroprotective role for GDF-15 through the regulation of tubular Klotho expression43 and downregulation of inflammatory activities45,46,47,48, elevated levels of circulating and urinary GDF-15 have been linked to increased risks of incident CKD, CKD progression, and death in individuals with kidney disease44,45, as well as higher risk of cardio-renal outcomes in individuals with type 2 diabetes49. After ischemia-reperfusion injury, GDF-15-deficient mice had more severe ATI whereas recombinant GDF-15 attenuated kidney injury50. It is possible that in patients with kidney disease, GDF-15 levels may not have a pathogenic role but rather reflect a compensatory response to acute or chronic injury that is present in the setting of oxidative stress. To our knowledge, this is the first study to investigate the association between biopsy-confirmed ATI and GDF-15 in a large cohort of individuals with a diverse spectrum of kidney diseases. The observed association between higher GDF-15-levels and more severe ATI may yield further confirmation for the central role of mitochondrial dysfunction in acute and chronic kidney disease where GDF-15 may act as an important mediator of mitochondrial stress responses41.
Another ATI marker associated with AKI across all cohort studies was LMAN2, which has been previously shown by Mendelian Randomization (MR) analyses to be causally associated with kidney function. LMAN2, a protein also known as vesicular integral-membrane protein (VIP36), is implicated in transport processes and metabolic activities occurring on the apical surface of kidney epithelial cells51. Prior studies have demonstrated that LMAN2 correlates with albuminuria and is associated with kidney function decline51,52. A number of biomarkers identified in this study, especially those with previously demonstrated significant MR findings, merit additional evaluation for their therapeutic potential in a range of kidney diseases.
We found lower levels of seven plasma proteins to be associated with more severe ATI that were also significantly lower in individuals with AKI and conferred a potentially protective effect against AKI. Among those was plasma kallikrein (KLKB1), a serine protease inhibitor implicated in coagulation and blood pressure regulation53. Concordant with our observations, another investigation in type 1 diabetes revealed that plasma kallikrein activity decreased in more advanced stages of diabetic nephropathy, reaching its lowest levels in individuals undergoing dialysis54. Additionally, a recent genome-wide association study in the German CKD Study on OPN revealed a significant association at a locus within KLKB1, suggesting a potential link between OPN and the kallikrein-kinin system55. We also found that levels of complement C1q tumor necrosis factor-related protein 3 (C1QTNF3; C1QTNF3), a member of the C1q/TNF-related protein family, were lower in individuals with AKI. This is congruent with a smaller investigation focused on diabetic patients, which reported lower serum levels of C1QTNF3 in those with type 2 diabetes when compared to healthy controls56. These findings are further supported by in vitro experiments demonstrating that C1QTNF3 mitigates TGF-β1-mediated kidney fibrosis57 and ameliorates lipid accumulation and necroinflammation induced by high glucose concentrations in renal tubular cells58.
While the functional significance and potential prognostic value of these proteins remain to be fully investigated, many of them are involved in common biological pathways relevant to tubular injury such as regulation of immune and cellular stress responses. The leading pathways in our study related to cellular organelle stress including mitochondrial or endoplasmic reticulum damage. These pathways are critical in AKI onset and can also drive inflammation and fibrosis, key factors in the transition from AKI to CKD when stress is sustained59. In fact, several markers found in this study are markers involved in the pathogenesis of both AKI and CKD. Traditionally, ATI parameters have not been systematically assessed in biopsies obtained for CKD evaluation. It is possible, however, that the extent of ATI could serve as a valuable prognostic indicator for assessing the likelihood of transitioning from acute to chronic kidney injury, underscoring the potential benefit of incorporating routine ATI assessment in CKD biopsies to enhance prognostic accuracy.
Significant strengths of our study include the large number of protein biomarkers included in the analyses. Detailed adjudicated histopathologic scores by two kidney pathologists allowed us to test associations between markers and the degree of ATI. We were able to replicate our findings in three independent study cohorts and evaluated the expression of biomarker proteins and genes in regional proteomics, transcriptomics, and single-cell analyses, confirming many of our findings. Our study has several limitations that warrant consideration as well. Given the intrinsic limitations of cross-sectional studies, which prevent the establishment of causality, additional experimental and clinical studies are needed to establish the causal role of the ATI biomarkers identified in this study. While our study cohort underwent comprehensive phenotypic characterization, enabling extensive multivariable adjustment, we cannot exclude the potential influence of unmeasured confounding variables on our results. Our study delineates several proteins that warrant further investigation in animal models to elucidate their tissue-specific function within the kidney.
In conclusion, our proteomics study identified over 150 proteins in the plasma of individuals with histologically confirmed tubular injury, with subsequent interrogation of findings in separate cohort studies with plasma proteomics, regional proteomics, and single-cell transcriptomics.
Methods
Ethical compliance
We have complied with all ethical regulations related to this study. All studies included received approval from their respective institutional review boards (IRB) at each participating center which included the Mass General Brigham IRB (BKBC study), the University of North Carolina at Chapel Hill IRB (ARIC Study), the Johns Hopkins University IRB (ARIC Study), the University of Minnesota IRB (ARIC Study), the University of Mississippi Medical Center IRB (ARIC Study), and the University of Washington IRB (KPMP and CHROME studies). Informed consent was obtained from participants of the BKBC, ARIC, and KPMP studies. In the CHROME study, participants were enrolled under an IRB-approved waiver of informed consent. All studies were conducted in accordance with the principles of the Declaration of Helsinki.
Study populations
The BKBC is a prospective, observational cohort study of patients who underwent native kidney biopsy at three tertiary care hospitals in Boston, Massachusetts, including Brigham and Women’s Hospital, Massachusetts General Hospital, and Beth Israel Deaconess Medical Center. The study includes adults ≥18 years of age who underwent a clinically indicated kidney biopsy between September 2006 and October 2018. Exclusion criteria were the inability to provide written consent, severe anemia, pregnancy, and enrollment in competing studies. Details of the study design have been previously described60. Patients provided blood samples on the day of kidney biopsy. For this study, we evaluated 434 participants with available plasma samples. The KPMP is a multicenter prospective cohort study of people with CKD or AKI who undergo a protocol kidney biopsy at study entry as part of the KPMP consortium (https://KPMP.org)61. For plasma proteomics analyses, we evaluated protein measurements of 44 participants (26 with AKI and 18 who provided healthy reference tissue). The ARIC study is a prospective cohort study of individuals recruited from four US communities62. Participants were enrolled between 1987 and 1989, with subsequent visits in 1990–1992 (visit 2), 1993–1995 (visit 3), 1996–1998 (visit 4), 2011–2013 (visit 5), 2016–2017 (visit 6), and 2018–2019 (visit 7), visit 8 (2020), visit 9 (2021–2022), and visit 10 (2023). In this study, we included 4,610 participants from visit 5 who had available plasma proteomic profiling and non-missing covariates at baseline. The CHROME study is a prospective cohort study of critically ill patients admitted to three hospitals affiliated with the University of Washington in Seattle, WA between March 2020 and May 2021. Details of the study design have been previously described63. In brief, patients were eligible if admitted to a medical intensive care unit (ICU) with signs or symptoms of acute respiratory illness. Exclusion criteria included being under 18 years of age, incarcerated, pregnant, or undergoing chronic maintenance hemodialysis. In this study, we included 268 individuals with available SOMAScan plasma proteomic profiling. All studies included in this manuscript received approval from their respective institutional review boards at each participating center.
Sample collection and proteomics assays
Proteomic profiling was performed on blood samples from the baseline visit of the BKBC, KPMP, and CHROME cohort, as well as visit 5 of the ARIC study. After collection, blood samples were aliquoted and stored at −80 °C. The SOMAscan assay was utilized for proteomic measurements64. This assay employs SOMAmers (selective single-stranded deoxyoligonucleotides) for protein binding and quantifies proteins based on fluorescence intensity, indicative of relative protein concentrations. The ARIC and CHROME plasma samples were analyzed using the SOMAscan 5k platform (approximately 5000 proteins), while the BKBC and KPMP samples were assessed using the SOMAscan 7k platform (approximately 7000 proteins). In the BKBC, 6592 aptamers passed quality control metrics and were included in subsequent analyses; the mean coefficient of variation (CV) on 8 blind duplicate pairs was 4.7%. In ARIC, KPMP, and the CHROME cohort, we evaluated only those proteins that were significantly associated with ATI in the BKBC (156 unique proteins). For ARIC visit 5, the mean Bland Altman coefficient of variation was 6.6% from 26 samples in blind triplicate. In KPMP, the mean CVs on 2 sets of 4 blind duplicates was 4.9%. For all studies, protein aptamers were log2-transformed and winsorized at mean±5×SD and adaptive normalization was performed by maximum likelihood as previously described64.
Histopathologic outcome
In the BKBC, kidney biopsy specimens were adjudicated under light microscopy by two experienced kidney pathologists who provided semiquantitative scores of ATI scored from 0 to 3 reflecting none, mild, moderate, and severe lesion severity. Methods to evaluate and score histopathologic lesion severity were previously described in detail60. The weighted kappa statistic (95% CI) from 26 randomly selected biopsies for repeat review months after the initial scoring for ATI was 0.67 (0.45–0.89)60. All participants’ charts were reviewed alongside histopathologic evaluations to provide the final primary clinicopathologic diagnosis.
Outcome of acute kidney injury
In KPMP, patients eligible for percutaneous kidney biopsy for AKI must have elevated serum creatinine that is either sustained or accompanied by evidence of parenchymal injury. Detailed inclusion criteria for AKI biopsies were previously described in detail61. In ARIC, individuals included in this study were free of AKI at baseline and followed prospectively for incident AKI. Incident cases of AKI were identified by International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 584.5 to 584.9 and Tenth Revision, Clinical Modification (ICD-10-CM) codes N17.0 to N17.9 or a 50% increase from outpatient serum creatinine during hospitalization. ICD codes were retrieved from hospital discharge billing and death certificates65. In the CHROME Cohort, the primary outcome was severe AKI within 7 days, defined by either initiation of kidney replacement therapy (KRT) or a doubling of serum creatinine from ICU admission63. In the ARIC and CHROME studies, blood samples were collected prior to the diagnosis of AKI or severe AKI, respectively.
Covariates
In the BKBC, detailed patient information was collected at the biopsy visit, including demographics, medical history, medication lists, and pertinent laboratory data and stored using REDCap electronic data capture tools hosted at Partners Health Care. We obtained serum creatinine (SCr) from the electronic medical record (EMR) on the day of biopsy. In participants for whom this was unavailable, we measured SCr in available blood samples collected on the day of the biopsy. We obtained spot urine protein-to-creatinine ratio (UPCR) or urine albumin-to-creatinine ratio (UACR) from the date of kidney biopsy to 3 months before biopsy from the EMR. If both were available, the UACR was used. If a participant did not have any of these values, we measured urine albumin-to-creatinine ratio from urine collected on the day of the kidney biopsy. SCr and urine creatinine were measured using a Jaffe-based method and urine albumin was measured by an immunoturbidometric method. The creatinine-based Chronic Kidney Disease Epidemiology Collaboration 2021 equation was used to calculate the eGFR66. In ARIC, covariates included age, sex, self-reported race, systolic blood pressure (SBP), UACR, smoking status, diabetes (fasting glucose of ≥126 mg/dL or non-fasting glucose level of ≥200 mg/dL, self-reported history of diabetes diagnosed by a physician, or use of medications for diabetes), hypertension (SBP ≥ 140 mm Hg and DBP ≥ 90 mm Hg, or use of medication for high BP), and eGFR (calculated using the CKD-EPI 2021 equation, which takes both serum creatinine and cystatin C into account)66. Serum creatinine was measured using a Roche enzymatic method (visit 5) and serum cystatin C was measured using the Roche Cobas 6000 chemistry analyzer. The UACR was calculated using urine albumin and creatinine (measured using an immunoturbidometric method on the ProSpec nephelometric analyzer and the Roche enzymatic method, respectively). In CHROME, covariates including age, sex, and COVID-19 status were extracted from the EMR.
Regional proteomics
We investigated the expression of ATI biomarker proteins in regional tissue proteomics from KPMP kidney biopsy samples (https://atlas.kpmp.org/explorer/regionalpro; access date: April 20, 2024). Detailed protocols and dataset information are available at https://www.kpmp.org/help-docs/technologies. In brief, kidney tissue was laser-microdissected to isolate glomerular and tubulointerstitial compartments. Following protein extraction from targeted tissue sections, proteins were analyzed using high-performance liquid chromatography coupled with mass spectrometry (HPLC-MS) for comprehensive identification and quantification. The study included tissue samples from 31 individuals (12 with AKI, 14 with CKD, and 5 healthy controls). We analyzed and compared the expression profiles of ATI biomarkers between the tubulointerstitial and glomerular compartments across all participants, and separately, evaluated differences in tubulointerstitial protein expression between healthy controls and those with AKI.
Kidney gene expression analysis
To map biomarker proteins to gene expression data, we investigated the expression of ATI biomarker-corresponding genes using regional transcriptomics and scRNA-seq data from KPMP (https://atlas.kpmp.org/explorer; access date: August 1, 2023). Tissue samples used for regional transcriptomics were drawn from living donor biopsy participants and used to compare expression (Fold Change) of our ATI biomarker genes of interest in the tubulointerstitium (n = 36; 9 healthy reference, 22 CKD, 5 AKI). Tissue samples analyzed using scRNA-seq were drawn from 47 participants (12 with AKI, 15 with CKD, and 20 healthy controls) and used to test for differential gene expression in kidney cell types. Details on these datasets have been described previously67,68.
Pathway analysis
To obtain basic functional information on biomarker proteins that were significantly associated with ATI severity and to investigate potentially relevant biological pathways, we applied Pathway Enrichment Analysis using gene sets obtained from publicly available databases including Gene Ontology, KEGG, and Reactome69,70. We ranked proteins based on their strength of association with ATI. We then calculated normalized enrichment scores to identify pathways with significant overrepresentation of ATI biomarkers. The Benjamini–Hochberg approach was employed to account for multiple testings and used to rank pathways based on the obtained p-value. Analyses were performed using the R package fgsea.
Statistical analysis
We summarized descriptive statistics as count with percentages for categorical variables and mean ± standard deviation or median with interquartile range for continuous variables. For skewed data distributions, we performed logarithmic transformation as appropriate. In the BKBC, multivariable linear regression models were used to assess associations of each plasma biomarker protein with ATI severity. In these models, the ATI severity score was used as the independent variable and each log2-transformed biomarker as the dependent variable. The adjusted model included the covariates age, race, sex, and eGFR. A prespecified α level of 7.58×10−6 set by Bonferroni correction (0.05/6592 proteins) was used to determine statistical significance. In ARIC, we used Cox proportional hazards models to test associations between the ATI biomarkers identified in the BKBC and the outcome of incident AKI. Models were adjusted for age, sex, self-reported race, SBP, smoking status, diabetes, hypertension UACR, and eGFR. In KPMP, we compared plasma levels of the ATI biomarkers in individuals with AKI and healthy controls using Analysis of Variance (ANOVA). In the CHROME cohort, we explored associations between the ATI biomarkers and severe AKI within 7 days of ICU admission using logistic regression models adjusted for age, sex, and COVID-19 status. In KPMP, we used a Bonferroni-corrected significance threshold of p < 3.21 × 10−4 (0.05/156 proteins). In ARIC and CHROME, we adjusted this threshold to p < 4.1 × 10−4 (0.05/122 proteins) and p < 3.79 × 10−4 (0.05/132 proteins), respectively, reflecting that only measurements of 122 (ARIC) and 132 (CHROME) of the 156 ATI biomarkers were available. In other analyses, we considered a two-sided p-value < 0.05 statistically significant. Statistical analyses were performed using R Version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria) and STATA 18.0 (STATACorp, College Station, TX).
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
Access to ARIC data follows NIH data sharing policies. Anonymized data can be obtained from the NHLBI Biologic Specimen and Data Repository Information Coordinating Center (https://biolincc.nhlbi.nih.gov/studies/aric/). Data access requests can also be submitted to the ARIC Publications Committee at aricpub@unc.edu. This process involves completing an ARIC manuscript proposal form, which can be found at the following link: https://aric.cscc.unc.edu/aric9/publications/policies_forms_and_guidelines. The review and approval of data access requests usually take about one month. To share ARIC data, a data use agreement (DUA) must be signed with the ARIC coordinating center at the University of North Carolina. Data from the BKBC and the CHROME study are not publicly available due to data privacy laws. Access to these datasets can be provided upon request to the study PIs in line with the IRB guidelines at each study’s institution and following approval of a DUA. Data sharing requests should be directed to the respective principal investigators Dr. Sushrut Waikar (BKBC; swaikar@bu.edu) and Dr. Pavan K. Bhatraju (CHROME; bhatraju@uw.edu). The data generated in this study are provided in the Supplementary Data file. All data from the Kidney Precision Medicine Project (KPMP) are publicly available and can be accessed at https://www.kpmp.org/doi-collection and https://www.kpmp.org/available-data.
Code availability
No new software packages were developed as part of this research. The analyses were conducted using standard regression models, implemented through readily available code in common statistical software platforms. As such, the code used in this study does not involve proprietary or custom algorithms that are central to the conclusions. The code utilized for these analyses can be provided upon request to ensure transparency and reproducibility.
References
Zuk, A. & Bonventre, J. V. Acute kidney injury. Annu Rev. Med 67, 293–307 (2016).
Hsu, R. K. & Hsu, C. Y. The role of acute kidney injury in chronic kidney disease. Semin Nephrol. 36, 283–292 (2016).
Chevalier, R. L. The proximal tubule is the primary target of injury and progression of kidney disease: role of the glomerulotubular junction. Am. J. Physiol. Ren. Physiol. 311, F145–F161 (2016).
Balzer, M. S., Rohacs, T. & Susztak, K. How many cell types are in the kidney and what do they do? Annu Rev. Physiol. 84, 507–531 (2022).
Matovinović, M. S. 1. Pathophysiology and classification of kidney diseases. Ejifcc 20, 2–11 (2009).
Gilbert, R. E. & Cooper, M. E. The tubulointerstitium in progressive diabetic kidney disease: more than an aftermath of glomerular injury? Kidney Int 56, 1627–1637 (1999).
Sun, M. et al. Clinical characteristics and prognosis of patients with idiopathic membranous nephropathy with kidney tubulointerstitial damage. Ren. Fail 45, 2205951 (2023).
Moeckel, G. W. Pathologic perspectives on acute tubular injury assessment in the kidney biopsy. Semin Nephrol. 38, 21–30 (2018).
Wen, Y., Yang, C., Menez, S. P., Rosenberg, A. Z. & Parikh, C. R. A systematic review of clinical characteristics and histologic descriptions of acute tubular injury. Kidney Int Rep. 5, 1993–2001 (2020).
Gaut, J. P. & Liapis, H. Acute kidney injury pathology and pathophysiology: a retrospective review. Clin. Kidney J. 14, 526–536 (2021).
Muiru, A. N. et al. Risk for chronic kidney disease progression after acute kidney injury: findings from the chronic renal insufficiency cohort study. Ann. Intern Med 176, 961–968 (2023).
Sabbisetti, V. S. et al. Blood kidney injury molecule-1 is a biomarker of acute and chronic kidney injury and predicts progression to ESRD in type I diabetes. J. Am. Soc. Nephrol. 25, 2177–2186 (2014).
Waikar, S. S. et al. Relationship of proximal tubular injury to chronic kidney disease as assessed by urinary kidney injury molecule-1 in five cohort studies. Nephrol. Dial. Transpl. 31, 1460–1470 (2016).
Niewczas, M. A. et al. A signature of circulating inflammatory proteins and development of end-stage renal disease in diabetes. Nat. Med 25, 805–813 (2019).
Isakova, T. Fibroblast growth factor 23 and adverse clinical outcomes in chronic kidney disease. Curr. Opin. Nephrol. Hypertens. 21, 334–340 (2012).
Bonomini, M. et al. Proteomic investigations into hemodialysis therapy. Int J. Mol. Sci. 16, 29508–29521 (2015).
Tsalik, E. L. et al. Renal systems biology of patients with systemic inflammatory response syndrome. Kidney Int 88, 804–814 (2015).
Feldreich, T. et al. Circulating proteins as predictors of cardiovascular mortality in end-stage renal disease. J. Nephrol. 32, 111–119 (2019).
Schmidt, I. M. et al. Circulating plasma biomarkers in biopsy-confirmed kidney disease. Clin. J. Am. Soc. Nephrol. 17, 27–37 (2022).
Carlsson, A. C. et al. Use of proteomics to investigate kidney function decline over 5 years. Clin. J. Am. Soc. Nephrol. 12, 1226–1235 (2017).
Glorieux, G. et al. New insights in molecular mechanisms involved in chronic kidney disease using high-resolution plasma proteome analysis. Nephrol. Dial. Transpl. 30, 1842–1852 (2015).
Kammer, M. et al. Integrative analysis of prognostic biomarkers derived from multiomics panels helps discrimination of chronic kidney disease trajectories in people with type 2 diabetes. Kidney Int 96, 1381–1388 (2019).
Azuaje F., Kim S. Y., Perez Hernandez D., Dittmar G. Connecting Histopathology Imaging and Proteomics in Kidney Cancer through Machine Learning. J Clin Med. 2019;8.
Sethi, S. et al. Glomeruli of dense deposit disease contain components of the alternative and terminal complement pathway. Kidney Int. 75, 952–960 (2009).
Chawla, L. S., Eggers, P. W., Star, R. A. & Kimmel, P. L. Acute kidney injury and chronic kidney disease as interconnected syndromes. N. Engl. J. Med 371, 58–66 (2014).
Nowak, N. et al. Increased plasma kidney injury molecule-1 suggests early progressive renal decline in non-proteinuric patients with type 1 diabetes. Kidney Int 89, 459–467 (2016).
Assarsson, E. et al. Homogenous 96-plex PEA immunoassay exhibiting high sensitivity, specificity, and excellent scalability. PLoS One 9, e95192 (2014).
Schmidt, I. M. et al. Plasma kidney injury molecule 1 in CKD: findings from the Boston Kidney Biopsy Cohort and CRIC studies. Am. J. Kidney Dis. 79, 231–243.e231 (2022).
Mansour, S. G. et al. Uromodulin to osteopontin ratio in deceased donor urine is associated with kidney graft outcomes. Transplantation 105, 876–885 (2021).
Xie, Y. et al. Expression, roles, receptors, and regulation of osteopontin in the kidney. Kidney Int 60, 1645–1657 (2001).
Khamissi, F. Z. et al. Identification of kidney injury released circulating osteopontin as causal agent of respiratory failure. Sci. Adv. 8, eabm5900 (2022).
Lorenzen, J. M. et al. Osteopontin predicts survival in critically ill patients with acute kidney injury. Nephrol. Dial. Transpl. 26, 531–537 (2011).
Steinbrenner, I. et al. Association of osteopontin with kidney function and kidney failure in chronic kidney disease patients: the GCKD study. Nephrol. Dial. Transpl. 38, 1430–1438 (2023).
Zhu, H. et al. Tenascin-C promotes acute kidney injury to chronic kidney disease progression by impairing tubular integrity via αvβ6 integrin signaling. Kidney Int 97, 1017–1031 (2020).
LeBleu, V. S. et al. Identification of human epididymis protein-4 as a fibroblast-derived mediator of fibrosis. Nat. Med 19, 227–231 (2013).
Wan, J. et al. Elevated serum concentrations of HE4 as a novel biomarker of disease severity and renal fibrosis in kidney disease. Oncotarget 7, 67748–67759 (2016).
Chen, P., Yang, Q., Li, X. & Qin, Y. Potential association between elevated serum human epididymis protein 4 and renal fibrosis: A systemic review and meta-analysis. Med. (Baltim.) 96, e7824 (2017).
Ihara, K. et al. Profibrotic circulating proteins and risk of early progressive renal decline in patients with type 2 diabetes with and without albuminuria. Diabetes Care 43, 2760–2767 (2020).
Schmidt I. M., et al. Plasma Kidney Injury Molecule 1 in CKD: Findings From the Boston Kidney Biopsy Cohort and CRIC Studies. Am J Kidney Dis. 2021).
Matsuhashi, T. et al. Mitochonic Acid 5 (MA-5) Facilitates ATP Synthase Oligomerization and Cell Survival in Various Mitochondrial Diseases. EBioMedicine 20, 27–38 (2017).
Fujita, Y., Ito, M. & Ohsawa, I. Mitochondrial stress and GDF15 in the pathophysiology of sepsis. Arch. Biochem Biophys. 696, 108668 (2020).
Perez-Gomez, M. V. et al. Urinary Growth Differentiation Factor-15 (GDF15) levels as a biomarker of adverse outcomes and biopsy findings in chronic kidney disease. J. Nephrol. 34, 1819–1832 (2021).
Valiño-Rivas, L. et al. Growth differentiation factor-15 preserves Klotho expression in acute kidney injury and kidney fibrosis. Kidney Int 101, 1200–1215 (2022).
Zhou, Z. et al. Circulating GDF-15 in relation to the progression and prognosis of chronic kidney disease: A systematic review and dose-response meta-analysis. Eur. J. Intern Med 110, 77–85 (2023).
Delrue, C., Speeckaert, R., Delanghe, J. R. & Speeckaert, M. M. Growth differentiation factor 15 (GDF-15) in kidney diseases. Adv. Clin. Chem. 114, 1–46 (2023).
Luan, H. H. et al. GDF15 is an inflammation-induced central mediator of tissue tolerance. Cell 178, 1231–1244.e1211 (2019).
Abulizi, P. et al. Growth differentiation factor-15 deficiency augments inflammatory response and exacerbates septic heart and renal injury induced by lipopolysaccharide. Sci. Rep. 7, 1037 (2017).
Wang, D. et al. GDF15: emerging biology and therapeutic applications for obesity and cardiometabolic disease. Nat. Rev. Endocrinol. 17, 592–607 (2021).
Sen, T. et al. Association between circulating GDF-15 and cardio-renal outcomes and effect of canagliflozin: results from the CANVAS trial. J. Am. Heart Assoc. 10, e021661 (2021).
Liu, J. et al. Renoprotective and immunomodulatory effects of GDF15 following AKI invoked by ischemia-reperfusion injury. J. Am. Soc. Nephrol. 31, 701–715 (2020).
Kiernan, E. et al. Alterations in the circulating proteome associated with albuminuria. J. Am. Soc. Nephrol. 34, 1078–1089 (2023).
Grams, M. E. et al. Proteins associated with risk of kidney function decline in the general population. J. Am. Soc. Nephrol. 32, 2291–2302 (2021).
Renné, T. The vascular side of plasma kallikrein. Blood 125, 589–590 (2015).
Härma, M. A. et al. Decreased plasma kallikrein activity is associated with reduced kidney function in individuals with type 1 diabetes. Diabetologia 63, 1349–1354 (2020).
Cheng, Y. et al. Genetics of osteopontin in patients with chronic kidney disease: The German Chronic Kidney Disease study. PLoS Genet 18, e1010139 (2022).
Moradi, N. et al. Serum levels of CTRP3 in diabetic nephropathy and its relationship with insulin resistance and kidney function. PLoS One 14, e0215617 (2019).
Chen, X. et al. C1q/tumor necrosis factor-related protein-3 improves renal fibrosis via inhibiting notch signaling pathways. J. Cell Physiol. 234, 22352–22364 (2019).
Du, C. et al. C1q/tumour necrosis factor-related protein-3 alleviates high-glucose-induced lipid accumulation and necroinflammation in renal tubular cells by activating the adenosine monophosphate-activated protein kinase pathway. Int J. Biochem Cell Biol. 149, 106247 (2022).
Inagi, R. The implication of organelle cross talk in AKI. Nephron 144, 634–637 (2020).
Srivastava, A. et al. The prognostic value of histopathologic lesions in native kidney biopsy specimens: results from the Boston Kidney Biopsy Cohort study. J. Am. Soc. Nephrol. 29, 2213–2224 (2018).
de Boer, I. H. et al. Rationale and design of the kidney precision medicine project. Kidney Int 99, 498–510 (2021).
Wright, J. D. et al. The ARIC (Atherosclerosis Risk In Communities) study: JACC Focus Seminar 3/8. J. Am. Coll. Cardiol. 77, 2939–2959 (2021).
Sathe, N. A. et al. Biomarker signatures of severe acute kidney injury in a critically Ill cohort of covid-19 and non-covid-19 acute respiratory illness. Crit. Care Explor 5, e0945 (2023).
Gold, L. et al. Aptamer-based multiplexed proteomic technology for biomarker discovery. PLoS One 5, e15004 (2010).
Grams, M. E. et al. Performance and limitations of administrative data in the identification of AKI. Clin. J. Am. Soc. Nephrol. 9, 682–689 (2014).
Inker, L. A. et al. New creatinine- and cystatin C-based equations to estimate GFR without race. N. Engl. J. Med 385, 1737–1749 (2021).
Lake, B. B. et al. An atlas of healthy and injured cell states and niches in the human kidney. Nature 619, 585–594 (2023).
Barwinska D., et al. Molecular characterization of the human kidney interstitium in health and disease. Sci Adv. 2021;7.
Mootha, V. K. et al. PGC-1alpha-responsive genes involved in oxidative phosphorylation are coordinately downregulated in human diabetes. Nat. Genet 34, 267–273 (2003).
Subramanian, A. et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl Acad. Sci. USA 102, 15545–15550 (2005).
Acknowledgements
We thank the members of the laboratory of S.S.W. for their invaluable assistance in the Boston Kidney Biopsy Cohort. I.M.S. is supported by the American Society of Nephrology Carl W. Gottschalk Research Scholar Award, the Boston University Department of Medicine Research Accelerator Program Award, and the Else Kroener-Fresenius Stiftung iPRIME-CS Scholarship (2021_EKFK.15). P.S. is supported by the German Research Foundation (DFG) Project-ID 530592017 (SCHL 2292/3–1), Project-ID 431984000—CRC 1453 NephGen, and Germany ́s Excellence Strategy (CIBSS – EXC-2189 – Project-ID 390939984). S.E.C. is supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health under Award Number R38HL143584. D.G.M. is supported by K23DK117065. Figure 1 in this manuscript was created with BioRender.com and released under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International license.
This study was supported by the National Institute of Diabetes and Digestive and Kidney Diseases (Grant / Award Number: 5R01DK108803-07, M.E.G., S.S.W., and E.R. and R01DK124399, M.E.G.). The Atherosclerosis Risk in Communities study has been funded in whole or in part with Federal funds from the National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services, under Contract nos. (75N92022D00001, 75N92022D00002, 75N92022D00003, 75N92022D00004, 75N92022D00005). The authors thank the staff and participants of the ARIC study for their important contributions. SomaLogic Inc. conducted the SomaScan assays in exchange for use of ARIC data. This work was supported in part by NIH/NHLBI grant R01 HL134320. The KPMP is funded by the following grants from the NIDDK: U01DK133081, U01DK133091, U01DK133092, U01DK133093,U01DK133095, U01DK133097, U01DK114866, U01DK114908, U01DK133090, U01DK133113, U01DK133766, U01DK133768, U01DK114907, U01DK114920, U01DK114923, U01DK114933, U24DK114886, UH3DK114926, UH3DK114861, UH3DK114915, UH3DK114937. The content of this paper is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Part of this work was presented as an oral presentation at the 2023 American Society of Nephrology Scientific Session on November 3rd.
Author information
Authors and Affiliations
Consortia
Contributions
I.M.S., M.E.G., E.P.R., J.C., and S.S.W. were responsible for the concept and design of the study. P.S., C.H., A.S., R.P., T.K., I.E.S., J.B., J.H., D.M., S.E.R., S.C., A.V., Y.W., M.L., T.B.H., N.A.S., P.B., and the Kidney Precision Medicine Project (KPMP), made important contributions to data collection, acquisition, analysis, and adjudication of histopathology. M.T.E., T.M. El-A., D.B., S.V.P., J.P.S, and B.R. were responsible for regional proteomics and transcriptomics data generation and analysis. I.M.S., A.L.S., R.Z., I.B.S., D.U., W.-J. Y., and S.S.W. were responsible for the statistical analysis. All authors interpreted the data. I.M.S. and S.S.W. drafted the manuscript. All authors contributed to critical revisions of the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Competing interests
S.S.W. reports personal fees from Public Health Advocacy Institute, CVS, Roth Capital Partners, Kantum Pharma, Mallinckrodt, Wolters Kluewer, GE Health Care, GSK, Allena Pharmaceuticals, Mass Medical International, Barron and Budd (vs Fresenius), JNJ, Venbio, Strataca, Takeda, Cerus, Pfizer, Bunch and James, Harvard Clinical Research Institute (aka Baim), Oxidien, Sironax, Metro Biotechnology, Biomarin, and Bain. S.E.R reports grant support to Joslin from Bayer and AstraZeneca. In addition, she has participated as advisory member for Bayer and AstraZeneca. D.G.M. is named co-inventor on a pending patent, “Methods and Systems for Diagnosis of Acute Interstitial Nephritis” and is a co-founder of the diagnostics company Predict AIN, LLC. Y.W. reports being an employee of Genentech and having stock and stock options in Roche at the time of final manuscript revision. The remaining authors declare that they have no competing interests.
Peer review
Peer review information
Nature Communications thanks Ying-Yong Zhao and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Schmidt, I.M., Surapaneni, A.L., Zhao, R. et al. Plasma proteomics of acute tubular injury. Nat Commun 15, 7368 (2024). https://doi.org/10.1038/s41467-024-51304-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-024-51304-x
- Springer Nature Limited