Abstract
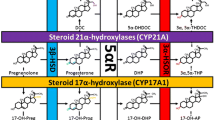
Finasteride and dutasteride, synthetic 5α-reductase inhibitors (5ARIs) are recommended in many guidelines for the treatment of benign prostatic hyperplasia/lower urinary tract symptoms and alopecia despite a variety of side effects like sexual, neurological, psychiatric, endocrinological, metabolic and ophthalmological dysfunctions and the increased incidence of high grade prostate cancer. The sexual side effects are common during the use of the drug but in a small subgroup of patients, they can persist after stopping the drug. This so-called post-finasteride syndrome has serious implications for the quality of life without a clear etiology or therapy. Three types of 5α-reductases are present in many organs in- and outside the brain where they can be blocked by the two 5ARIs. There is increasing evidence that 5ARIs not only inhibit the conversion of testosterone to 5α-dihydrotestosterone (DHT) in the prostate and the scalp but also in many other tissues. The lipophilic 5ARIs can pass the blood-brain barrier and might block many other neurosteroids in the brain with changes in the neurochemistry and impaired neurogenesis. Further research and therapeutic innovations are urgently needed that might cure or relieve these side effects. More awareness is needed for physicians to outweigh these health risks against the benefits of 5ARIs.


Similar content being viewed by others
References
Access data. https://www.fda.gov/drugs/information-drug-class/5-alpha-reductase-inhibitor-information. Assessed 18 April 2023.
Cather JC, Lane D, Heaphy MR, Nelson BR. Finasteride—an update and review. Cutis. 1999;64:167–72. https://pubmed.ncbi.nlm.nih.gov/10500917/.
Taylor BC, Wilt TJ, Fink HA, Lambert LC, Marshall LM, Hoffman AR. et al. Prevalence, severity, and health correlates of lower urinary tract symptoms among older men: the MrOS study. Urology. 2006;68:804–9. https://pubmed.ncbi.nlm.nih.gov/17070357/.
Severi G, Sinclair R, Hopper JL, English DR, McCredie MRE, Boyle P. et al. Androgenetic alopecia in men aged 40–69 years: prevalence and risk factors. Br J Dermatol. 2003;149:1207–13. https://pubmed.ncbi.nlm.nih.gov/14674898/.
Rittmaster RS, Norman RW, Thomas LN, Rowden G. Evidence for atrophy and apoptosis in the prostates of men given finasteride. J Clin Endocrinol Metab. 1996;81:814–9. https://pubmed.ncbi.nlm.nih.gov/8636309/.
Naslund MJ, Miner M. A review of the clinical efficacy and safety of 5α-reductase inhibitors for the enlarged prostate. Clin Ther. 2007;29:17–25. https://pubmed.ncbi.nlm.nih.gov/17379044/.
McConnell JD, Bruskewitz R, Walsh P, Andriole G, Lieber M, Logan Holtgrewe H. et al. The effect of finasteride on the risk of acute urinary retention and the need for surgical treatment among men with benign prostatic hyperplasia. N Engl J Med. 1998;338:557–63. https://pubmed.ncbi.nlm.nih.gov/9475762/.
Roehrborn CG, Boyle P, Nickel JC, Hoefner K, Andriole G. Efficacy and safety of a dual inhibitor of 5-alpha-reductase types 1 and 2 (dutasteride) in men with benign prostatic hyperplasia. Urology. 2002;60:434–41. https://pubmed.ncbi.nlm.nih.gov/12350480/.
Nickel JC, Fradet Y, Boake RC, Pommerville PJ, Perreault J-P, Afridi SK, et al. Efficacy and safety of finasteride therapy for benign prostatic hyperplasia: results of a 2-year randomized controlled trial (the PROSPECT study). PROscar Safety Plus Efficacy Canadian Two year Study. Can Med Assoc J. 1996;155:1251–9.
Roehrborn CG, Siami P, Barkin J, Damião R, Major-Walker K, Nandy I, et al. The effects of combination therapy with dutasteride and tamsulosin on clinical outcomes in men with symptomatic benign prostatic hyperplasia: 4-year results from the CombAT study. Eur Urol. 2010;57:123–31.
McClellan KJ, Markham A. Finasteride: a review of its use in male pattern hair loss. Drugs. 1999;57:111–26. https://pubmed.ncbi.nlm.nih.gov/9951956/.
Cornu JN, Gacci M, Hashim H, Herrmann TRW, Malde S, Netsch C, et al. Non-neurogenic male lower urinary tract symptoms (LUTS), including benign prostatic obstruction (BPO). EAU guidelines. Presented at the EAU Annual Congress Milan. The Netherlands; 2023.
Mysore V, Shashikumar BM. Guidelines on the use of finasteride in androgenetic alopecia. Indian J Dermatol Venereol Leprol. 2016;82:128–34. http://www.ncbi.nlm.nih.gov/pubmed/26924401.
Irwig MS, Kolukula S. Persistent sexual side effects of finasteride for male pattern hair loss. J Sex Med. 2011;8:1747–53. https://pubmed.ncbi.nlm.nih.gov/21418145/.
Kiguradze T, Temps WH, Yarnold PR, Cashy J, Brannigan RE, Nardone B, et al. Persistent erectile dysfunction in men exposed to the 5α-reductase inhibitors, finasteride, or dutasteride. PeerJ. 2017;5:e3020 https://doi.org/10.7717/peerj.3020.
Corona G, Tirabassi G, Santi D, Maseroli E, Gacci M, Dicuio M, et al. Sexual dysfunction in subjects treated with inhibitors of 5α-reductase for benign prostatic hyperplasia: a comprehensive review and meta-analysis. Andrology. 2017;5:671–8. https://pubmed.ncbi.nlm.nih.gov/28453908/.
Traish AM. Health risks associated with long-term finasteride and dutasteride use: it’s time to sound the alarm. World J Mens Health. 2020;38:323. https://pubmed.ncbi.nlm.nih.gov/32202088/.
Diviccaro S, Melcangi RC, Giatti S. Post-finasteride syndrome: an emerging clinical problem. Neurobiol Stress. 2019;12:100209. https://pubmed.ncbi.nlm.nih.gov/32435662/.
Thompson IM, Goodman PJ, Tangen CM, Lucia MS, Miller GJ, Ford LG, et al. The influence of finasteride on the development of prostate cancer. N Engl J Med. 2003;349:215–24.
Andriole GL, Bostwick DG, Brawley OW, Gomella LG, Marberger M, Montorsi F. et al. Effect of dutasteride on the risk of prostate cancer. N Engl J Med. 2010;362:1192–202. https://pubmed.ncbi.nlm.nih.gov/20357281/.
Sarkar RR, Parsons JK, Bryant AK, Ryan ST, Kader AK, McKay RR, et al. Association of treatment with 5α-reductase inhibitors with time to diagnosis and mortality in prostate cancer. JAMA Intern Med. 2019;179:812–9.
Yamana K, Fernand L, Luu-The V, Luu-The V. Human type 3 5α-reductase is expressed in peripheral tissues at higher levels than types 1 and 2 and its activity is potently inhibited by finasteride and dutasteride. Horm Mol Biol Clin Investig. 2010;2:293–9. https://pubmed.ncbi.nlm.nih.gov/25961201/.
Wilson EM, French FS. Binding properties of androgen receptors. Evidence for identical receptors in rat testis, epididymis, and prostate. J Biol Chem. 1976;251:5620–9.
Siiteri PK, Wilson JD. Testosterone formation and metabolism during male sexual diflferentiation in the human embryo. J Clin Endocrinol Metab. 1974;38:113–25. https://pubmed.ncbi.nlm.nih.gov/4809636/.
Baldinotti F, Majore S, Fogli A, Marrocco G, Ghirri P, Vuerich M, et al. Molecular characterization of 6 unrelated Italian patients with 5α-reductase type 2 deficiency. J Androl. 2008;29:20–8.
MacLaughlin DT, Donahoe PK. Sex determination and differentiation. N Engl J Med. 2004;350:367–78. https://www.nejm.org/doi/10.1056/NEJMra022784.
Andriole G, Bruchovsky N, Chung LWK, Matsumoto AM, Rittmaster R, Roehrborn C. et al. Dihydrotestosterone and the prostate: the scientific rationale for 5α-reductase inhibitors in the treatment of benign prostatic hyperplasia. J Urol. 2004;172:1399–403. https://pubmed.ncbi.nlm.nih.gov/15371854/.
Walsh PC, Madden JD, Harrod MJ, Goldstein JL, Macdonald PC, Wilson JD. Familial incomplete male pseudohermaphroditism, type 2: decreased dihydrotestosterone formation in pseudovaginal perineoscrotal hypospadias. N Engl J Med. 1974;291:944–9. https://pubmed.ncbi.nlm.nih.gov/4413434/.
Imperato-McGinley J, Guerrero L, Gautier T, Peterson RE. Steroid 5α-reductase deficiency in man: an inherited form of male pseudohermaphroditism. Science. 1974;186:1213–5. https://pubmed.ncbi.nlm.nih.gov/4432067/.
Melcangi RC, Santi D, Spezzano R, Grimoldi M, Tabacchi T, Fusco ML, et al. Neuroactive steroid levels and psychiatric and andrological features in post-finasteride patients. J Steroid Biochem Mol Biol. 2017;171:229–35.
Godoy A, Kawinski E, Li Y, Oka D, Alexiev B, Azzouni F. et al. 5α-reductase type 3 expression in human benign and malignant tissues: a comparative analysis during prostate cancer progression. Prostate. 2011;71:1033–46. https://onlinelibrary.wiley.com/doi/full/10.1002/pros.21318.
Finn DA, Beadles-Bohling AS, Beckley EH, Ford MM, Gililland KR, Gorin-Meyer RE, et al. A new look at the 5α-reductase inhibitor finasteride. CNS Drug Rev. 2006;12:53–76. https://pubmed.ncbi.nlm.nih.gov/16834758/.
Traish AM, Melcangi RC, Bortolato M, Garcia-Segura LM, Zitzmann M. Adverse effects of 5α-reductase inhibitors: what do we know, don’t know, and need to know? Rev Endocr Metab Disord. 2015;16:177–98. https://pubmed.ncbi.nlm.nih.gov/26296373/.
Frye SV, Bramson HN, Hermann DJ, Lee FW, Sinhababu AK, Tian G. Discovery and development of GG745, a potent inhibitor of both isozymes of 5 alpha-reductase. Pharm Biotechnol Pharm Biotechnol. 1998;11:393–422. https://pubmed.ncbi.nlm.nih.gov/9760689/.
Roberts JL, Fiedler V, Imperato-McGinley J, Whiting D, Olsen E, Shupack J, et al. Clinical dose ranging studies with finasteride, a type 2 5α-reductase inhibitor, in men with male pattern hair loss. J Am Acad Dermatol. 1999;41:555–63.
Rittmaster R, Hahn RG, Ray P, Shannon JB, Wurzel R. Effect of dutasteride on intraprostatic androgen levels in men with benign prostatic hyperplasia or prostate cancer. Urology. 2008;72:808–12. https://pubmed.ncbi.nlm.nih.gov/18718641/.
Kligman AM. The comparative histopathology of male pattern baldness and senescent baldness. In: Clinics in Dermatology. Philadelphia: Lippincot. p. 2008;108–13.
Hoffmann R van. Recent findings with computerized methods for scalp hair growth measurements. J Investig Dermatol Symp Proc. 2005;10;285–8.
Kaufman KD, Olsen EA, Whiting D, Savin R, DeVillez R, Bergfeld W. et al. Finasteride in the treatment of men with androgenetic alopecia. J Am Acad Dermatol. 1998;39:578–89. https://pubmed.ncbi.nlm.nih.gov/9777765/.
Brenner S, Matz H. Improvement in androgenetic alopecia in 53-76-year-old men using oral finasteride. Int J Dermatol. 1999;38:928–30. https://pubmed.ncbi.nlm.nih.gov/10632776/.
Stoffel-Wagner B. Neurosteroid metabolism in the human brain. Eur J Endocrinol. 2001;145:669–79. https://pubmed.ncbi.nlm.nih.gov/11720889/.
Duskova M, Hill M, Hanuš M, Matoušková M, Stárka L. et al. Finasteride treatment and neuroactive steroid formation. Prague Med Rep. 2009;110:222–30. https://pubmed.ncbi.nlm.nih.gov/19655698/.
Melcangi RC, Caruso D, Abbiati F, Giatti S, Calabrese D, Piazza F, et al. Neuroactive steroid levels are modified in cerebrospinal fluid and plasma of post-finasteride patients showing persistent sexual side effects and anxious/depressive symptomatology. J Sex Med. 2013;10:2598–603.
Caruso D, Abbiati F, Giatti S, Romano S, Fusco L, Cavaletti G, et al. Patients treated for male pattern hair with finasteride show, after discontinuation of the drug, altered levels of neuroactive steroids in cerebrospinal fluid and plasma. J Steroid Biochem Mol Biol. 2015;146:74–9. https://pubmed.ncbi.nlm.nih.gov/24717976/.
Li L, Kang YX, Ji XM, Li YK, Li SC, Zhang XJ. et al. Finasteride inhibited brain dopaminergic system and open-field behaviors in adolescent male rats. CNS Neurosci Ther. 2018;24:115–25. https://pubmed.ncbi.nlm.nih.gov/29214729/.
Roberto Frau R, Mosher LJ, Bini V, Pillolla G, Pes R, Saba P, et al. The neurosteroidogenic enzyme 5α-reductase modulates the role of D1 dopamine receptors in rat sensorimotor gating. Psychoneuroendocrinology. 2016;63:59–67. https://pubmed.ncbi.nlm.nih.gov/26415119/.
Bradshaw WG, Baum MJ, Awh CC. Attenuation by a 5α-reductase inhibitor of the activational effect of testosterone propionate on penile erections in castrated male rats. Endocrinology. 1981;109:1047–51. https://pubmed.ncbi.nlm.nih.gov/7285860/.
Traish AM, Hassani J, Guay AT, Zitzmann M, Hansen ML. Adverse side effects of 5α-reductase inhibitors therapy: persistent diminished libido and erectile dysfunction and depression in a subset of patients. J Sex Med. 2011;8:872–84. http://www.ncbi.nlm.nih.gov/pubmed/21176115.
Moinpour CM, Darke AK, Donaldson GW, Thompson IM, Langley C, Ankerst DP. et al. Longitudinal analysis of sexual function reported by men in the Prostate Cancer Prevention Trial. J Natl Cancer Inst. 2007;99:1025–35. https://pubmed.ncbi.nlm.nih.gov/17596576/.
Irwig MS. Depressive symptoms and suicidal thoughts among former users of finasteride with persistent sexual side effects. J Clin Psychiatry. 2012;73:1220–3. https://pubmed.ncbi.nlm.nih.gov/22939118/.
Jim Thornton. The Truth about Propecia. https://www.menshealth.com/health/a19531052/hair-raising-effect/ 18, 2011.
Post-Finasteride Syndrome Foundation. https://www.pfsfoundation.org/about-post-finasteride-syndrome-foundation/. Accessed 16 Jan 2023.
Healy D, Bahrick A, Bak M, Barbato A, Calabrò RS, Chubak BM, et al. Diagnostic criteria for enduring sexual dysfunction after treatment with antidepressants, finasteride and isotretinoin the Creative Commons Attribution-NonCommercial License (CC BY-NC 4.0). 66 D. Healy et al. / Diagnostic criteria for enduring sexual dysfunction after treatment. Int J Risk Saf Med. 2022;33:65–76.
Pereira AFJR, Coelho TODA. Post-finasteride syndrome. Bras Dermatol. 2020;95:271–7.
Belknap SM, Aslam I, Kiguradze T, Temps WH, Yarnold PR, Cashy J. et al. Adverse event reporting in clinical trials of finasteride for androgenic alopecia ameta-analysis. JAMA Dermatol. 2015;151:600–6. https://pubmed.ncbi.nlm.nih.gov/25830296/.
Favilla V, Russo GI, Privitera S, Castelli T, Giardina R, Calogero AE, et al. Impact of combination therapy 5-alpha reductase inhibitors (5-ARI) plus alpha-blockers (AB) on erectile dysfunction and decrease of libido in patients with LUTS/BPH: a systematic review with meta-analysis. Aging Male. 2016;19:175–81. https://pubmed.ncbi.nlm.nih.gov/27310433/.
Hagberg KW, Divan HA, Persson R, Nickel JC, Jick SS. Risk of erectile dysfunction associated with use of 5-α reductase inhibitors for benign prostatic hyperplasia or alopecia: population based studies using the Clinical Practice Research Datalink. BMJ. 2016;354:i4823. https://pubmed.ncbi.nlm.nih.gov/27659058/.
Shin YS, Karna KK, Choi BR, Park JK. Finasteride and erectile dysfunction in patients with benign prostatic hyperplasia or male androgenic alopecia. World J Mens Health. 2019;37:157–65.
Nguyen DD, Herzog P, Cone EB, Labban M, Zorn KC, Chughtai B, et al. Disproportional signal of sexual dysfunction reports associated with finasteride use in young men with androgenetic alopecia: a pharmacovigilance analysis of VigiBase. J Am Acad Dermatol. 2023;88:179–81. https://pubmed.ncbi.nlm.nih.gov/35351540/.
Nguyen DD, Marchese M, Cone EB, Paciotti M, Basaria S, Bhojani N. et al. Investigation of suicidality and psychological adverse events in patients treated with finasteride. JAMA Dermatol. 2021;157:35–42. https://jamanetwork.com/journals/jamadermatology/fullarticle/2772818.
Surendran P, Stewart ID, Yeung VPWA, Pietzner M, Raffler J, Wörheide MA, et al. Rare and common genetic determinants of metabolic individuality and their effects on human health. Nat Med. 2022;28:2321–32. https://doi.org/10.1038/s41591-022-02046-0.
Baas WR, Butcher MJ, Lwin A, Holland B, Herberts M, Clemons J. et al. A review of the FAERS data on 5-alpha reductase inhibitors: implications for postfinasteride syndrome. Urology. 2018;120:143–9. https://pubmed.ncbi.nlm.nih.gov/29960004/.
Dowman JK, Hopkins LJ, Reynolds GM, Armstrong MJ, Nasiri M, Nikolaou N. et al. Loss of 5α-Reductase Type 1 accelerates the development of hepatic steatosis but protects against hepatocellular carcinoma in male mice. Endocrinology. 2013;154:4536–47. https://pubmed.ncbi.nlm.nih.gov/24080367/.
Livingstone DEW, Barat P, Di Rollo EM, Rees GA, Weldin BA, Rog-Zielinska EA. et al. 5α-Reductase type 1 deficiency or inhibition predisposes to insulin resistance, hepatic steatosis, and liver fibrosis in rodents. Diabetes. 2015;64:447–58. https://pubmed.ncbi.nlm.nih.gov/25239636/.
Hazlehurst JM, Oprescu AI, Nikolaou N, Di Guida R, Grinbergs AEK, Davies NP. et al. Dual-5α-reductase inhibition promotes hepatic lipid accumulation in man. J Clin Endocrinol Metab. 2016;101:103–13. https://pubmed.ncbi.nlm.nih.gov/26574953/.
Upreti R, Hughes KA, Livingstone DEW, Gray CD, Minns FC, Macfarlane DP, et al. 5α-reductase type 1 modulates insulin sensitivity in men. J Clin Endocrinol Metab. 2014;99. https://pubmed.ncbi.nlm.nih.gov/24823464/.
Li K, Zhang C, Yang Z, Wang Y, Si H. Evaluation of a novel dry eye model induced by oral administration of finasteride. Mol Med Rep. 2017;16:8763–70. https://pubmed.ncbi.nlm.nih.gov/29039509/.
Zhang C, Li K, Yang Z, Wang Y, Si H. The effect of the aqueous extract of Bidens pilosa L. on androgen deficiency dry eye in rats. Cell Physiol Biochem. 2016;39:266–77. https://pubmed.ncbi.nlm.nih.gov/27337217/.
Baig MS, Kolasa-Wołosiuk A, Pilutin A, Safranow K, Baranowska-Bosiacka I, Kabat-Koperska J, et al. Finasteride-induced inhibition of 5α-reductase type 2 could lead to kidney damage—animal, experimental study. Int J Environ Res Public Health. 2019;16. https://pubmed.ncbi.nlm.nih.gov/31100850/.
Mahony MC, Swanlund DJ, Billeter M, Roberts KP, Pryor JL. Regional distribution of 5α-reductase type 1 and type 2 mRNA along the human epididymis. Fertil Steril. 1998;69:1116–21.
Amory JK, Wang C, Swerdloff RS, Anawalt BD, Matsumoto AM, Bremner WJ. et al. The effect of 5alpha-reductase inhibition with dutasteride and finasteride on semen parameters and serum hormones in healthy men. J Clin Endocrinol Metab. 2007;92:1659–65. https://pubmed.ncbi.nlm.nih.gov/17299062/.
Chiba K, Yamaguchi K, Li F, Ando M, Fujisawa M. Finasteride-associated male infertility. Fertil Steril. 2011;95:1786.e9–1786.e11. http://www.fertstert.org/article/S0015028210029250/fulltext.
Irwig MS. Androgen levels and semen parameters among former users of finasteride with persistent sexual adverse effects. JAMA Dermatol Am Med Assoc. 2014;150:1361–3. https://pubmed.ncbi.nlm.nih.gov/25229565/.
Samplaski MK, Lo K, Grober E, Jarvi K. Finasteride use in the male infertility population: effects on semen and hormone parameters. Fertil Steril. 2013;100:1542–6.
Traish AM. 5α-reductases in human physiology: an unfolding story. Endocr Pract Am Assoc Clin Endocrinol. 2012;18:965–75. https://pubmed.ncbi.nlm.nih.gov/23246684/.
Bull HG. Mechanism-based inhibition of human steroid 5 alfa-reductase by finasteride: enzyme-catalyzed formation of NADP-dihydrofinasteride, a potent bisubstrate analog inhibitor. J Am Chem Soc. 1996;118:2359–65.
Giatti S, Foglio B, Romano S, Pesaresi M, Panzica G, Garcia-Segura LM. et al. Effects of subchronic finasteride treatment and withdrawal on neuroactive steroid levels and their receptors in the male rat brain. Neuroendocrinology. 2016;103:746–57. https://pubmed.ncbi.nlm.nih.gov/26646518/.
Römer B, Pfeiffer N, Lewicka S, Ben-Abdallah N, Vogt MA, Deuschle M. et al. Finasteride treatment inhibits adult hippocampal neurogenesis in male mice. Pharmacopsychiatry. 2010;43:174–8. https://pubmed.ncbi.nlm.nih.gov/20486040/.
Hercher C, Turecki G, Mechawar N. Through the looking glass: examining neuroanatomical evidence for cellular alterations in major depression. J Psychiatr Res. 2009;43:947–61. https://pubmed.ncbi.nlm.nih.gov/19233384/.
Diviccaro S, Giatti S, Borgo F, Barcella M, Borghi E, Trejo JL, et al. Treatment of male rats with finasteride, an inhibitor of 5alpha-reductase enzyme, induces long-lasting effects on depressive-like behavior, hippocampal neurogenesis, neuroinflammation and gut microbiota composition. Psychoneuroendocrinology. 2019;99:206–15. https://pubmed.ncbi.nlm.nih.gov/30265917/.
Azzouni F, Godoy A, Li Y, Mohler J. The 5 alpha-reductase isozyme family: a review of basic biology and their role in human diseases. Adv Urol. 2012;2012. http://blast.ncbi.nlm.nih.gov/Blast.cgi.
Da Silva MHA, Costa WS, Sampaio FJB, De Souza DB. The corpus cavernosum after treatment with dutasteride or finasteride: a histomorphometric study in a benign prostatic hyperplasia rodent model. Asian J Androl. 2018;20:505–10. https://pubmed.ncbi.nlm.nih.gov/29893293/.
Lugg JA, Rajfer J, González-Cadavid NF. Dihydrotestosterone is the active androgen in the maintenance of nitric oxide-mediated penile erection in the rat. Endocrinology. 1995;136:1495–501. https://pubmed.ncbi.nlm.nih.gov/7534702/.
Zhang MG, Wang XJ, Shen ZJ, Gao PJ. Long-term oral administration of 5α-reductase inhibitor attenuates erectile function by inhibiting autophagy and promoting apoptosis of smooth muscle cells in corpus cavernosum of aged rats. Urology. 2013;82:743.e9–.e15. https://pubmed.ncbi.nlm.nih.gov/23876578/.
Kang HJ, Imperato-Mcginley J, Zhu YS, Rosenwaks Z. The effect of 5α-reductase-2 deficiency on human fertility. Fertil Steril. 2014;101:310–6. https://pubmed.ncbi.nlm.nih.gov/24412121/.
Mondaini N, Gontero P, Giubilei G, Lombardi G, Cai T, Gavazzi A, et al. Finasteride 5 mg and sexual side effects: How many of these are related to a Nocebo phenomenon? J Sex Med. 2007;4:1708–12.
Hoffman KB, Dimbil M, Erdman CB, Tatonetti NP, Overstreet BM. The Weber effect and the United States Food and Drug Administration’s Adverse Event Reporting System (FAERS): analysis of sixty-two drugs. Drug Saf. 2014;37:283–94.
Irwig MS. Safety concerns regarding 5α reductase inhibitors for the treatment of androgenetic alopecia. Curr Opin Endocrinol Diabetes Obes. 2015;22:248–53. https://pubmed.ncbi.nlm.nih.gov/25871957/.
Maksym RB, Kajdy A, Rabijewski M. Post-finasteride syndrome–does it really exist?. Aging Male. 2019;22:250–9. https://pubmed.ncbi.nlm.nih.gov/30651009/.
Healy D, Le Noury J, Mangin D. Enduring sexual dysfunction after treatment with antidepressants, 5α-reductase inhibitors and isotretinoin: 300 cases. Int J Risk Saf Med. 2018;29:125–34.
Kastenmüller G, Raffler J, Gieger C, Suhre K. Genetics of human metabolism: an update. Hum Mol Genet. 2015. https://academic.oup.com/hmg/article/24/R1/R93/671706.
Howard DM, Adams MJ, Clarke T-K, Hafferty JD, Gibson J, Shirali M, et al. Genome-wide meta-analysis of depression identifies 102 independent variants and highlights the importance of the prefrontal brain regions. http://www.nature.com/authors/editorial_policies/license.html#terms.
Ganzer CA, Jacobs AR. Emotional consequences of Finasteride: fool’s gold. Am J Mens Health. 2018;12:90–5. https://pubmed.ncbi.nlm.nih.gov/26868914/.
Irwig MS. Finasteride and suicide: a postmarketing case series. Dermatology. 2020;236:540–5. https://pubmed.ncbi.nlm.nih.gov/31935720/.
Fwu CW, Eggers PW, Kirkali Z, McVary KT, Burrows PK, Kusek JW. Change in sexual function in men with lower urinary tract symptoms/benign prostatic hyperplasia associated with long-term treatment with doxazosin, finasteride and combined therapy. J Urol. 2014;191:1828–34. https://pubmed.ncbi.nlm.nih.gov/24342143/.
Traish AM, Haider KS, Doros G, Haider A. Finasteride, not tamsulosin, increases severity of erectile dysfunction and decreases testosterone levels in men with benign prostatic hyperplasia. Horm Mol Biol Clin Investig. 2015;23:85–96. https://pubmed.ncbi.nlm.nih.gov/26053014/.
Liu L, Zhao S, Li F, Li E, Kang R, Luo L, et al. Effect of 5α-reductase inhibitors on sexual function: a meta-analysis and systematic review of randomized controlled trials. J Sex Med. 2016;13:1297–310. https://pubmed.ncbi.nlm.nih.gov/27475241/.
Roehrborn CG, Manyak MJ, Palacios-Moreno JM, Wilson TH, Roos EPM, Santos JC. et al. A prospective randomised placebo-controlled study of the impact of dutasteride/tamsulosin combination therapy on sexual function domains in sexually active men with lower urinary tract symptoms (LUTS) secondary to benign prostatic hyperplasia (BPH). BJU Int. 2018;121:647–58. https://pubmed.ncbi.nlm.nih.gov/29044968/.
Kosilov K, Kuzina I, Kuznetsov V, Gainullina Y, Kosilova L, Karashchuk E, et al. The risk of sexual dysfunction and effectiveness of treatment of benign prostatic hyperplasia with severe lower urinary tract dysfunction with combination of dutasteride and solifenacin. J Sex Med. https://doi.org/10.1016/j.jsxm.2018.09.011.
Author information
Authors and Affiliations
Contributions
HL corresponding author, confirms that the two other contributing authors (2 and 3) played an important role in the final result of the manuscript, with revisions and approval of the final version. They agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Leliefeld, H.H.J., Debruyne, F.M.J. & Reisman, Y. The post-finasteride syndrome: possible etiological mechanisms and symptoms. Int J Impot Res (2023). https://doi.org/10.1038/s41443-023-00759-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41443-023-00759-5
- Springer Nature Limited
This article is cited by
-
Comment on “The post-finasteride syndrome: possible etiological mechanisms and symptoms”
International Journal of Impotence Research (2024)