Abstract
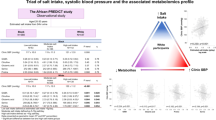
The contrasting relationships of plant and animal protein intake with blood pressure (BP) may be partially attributed to the differential non-protein (e.g., saturated fat and fibre) and amino acid (AA) compositions. This study determined whether animal and plant protein intake were related to differential metabolomic profiles associated with BP. This study included 1008 adults from the African-PREDICT study (aged 20–30 years). Protein intake was determined using 24-h dietary recalls. Twenty-four-hour ambulatory BP was measured. Amino acids and acylcarnitines were analysed in spot urine samples using liquid chromatography-tandem mass spectrometry-based metabolomics. Participants with a low plant, high animal protein intake had higher SBP (by 3 mmHg, p = 0.011) than those with high plant, low animal protein intake (low-risk group). We found that the relationships of plant and animal protein intake with 24-h SBP were partially mediated by BMI and saturated fat intake, which were independently associated with SBP. Protein intake was therefore not related to SBP in multiple regression analysis after adjusting for confounders. In the low-risk group, methionine (Std. β = −0.217; p = 0.034), glutamic acid (Std. β = −0.220; p = 0.031), glycine (Std. β = −0.234; p = 0.025), and proline (Std. β = −0.266; p = 0.010) were inversely related to SBP, and beta-alanine (Std. β = −0.277; p = 0.020) to DBP. Ultimately a diet high in animal and low in plant protein intake may contribute to higher BP by means of increased BMI and saturated fat intake. Conversely, higher levels of urinary AAs observed in adults consuming a plant rich diet may contribute to lower BP.

Similar content being viewed by others
Introduction
Dietary intervention is an established non-pharmacological strategy that plays an integral part in the prevention and management of hypertension [1], one of the largest public health concerns affecting over 1 billion adults globally [2]. The continued development of comprehensive dietary recommendations therefore remains a major priority. Although regional dietary patterns are linked with food availability, affordability, tradition, and culture, there is global consensus, aligning with WHO recommendations, with regard to what is considered elements of a healthy diet (e.g., increasing plant-based food intake and limiting saturated fat and sugar intake) [3, 4]. Metabolomics is a useful tool in nutrition science that may assist in the future development of more attainable and impactful dietary recommendations [5]. Continuing advances in the field of metabolomics have provided exciting new opportunities to gain better insights into metabolic pathways that may be involved in the link between nutrition and disease development [5, 6].
Dietary habits that contribute to increased cardiovascular risk include the inadequate consumption of plant- based proteins (whole grains, legumes, nuts, and seeds) [7, 8] as well as excessive animal protein intake, specifically red meat and processed meat [7]. In the different regions of Sub-Saharan Africa, low fruit, vegetable, whole grains, and legume consumption, together with high sodium intake, were the leading dietary risk factors for cardiovascular disease (CVD) death and disability-adjusted life years [7]. Although there are some discrepancies in the literature, the consumption of high-quality plant-based diets have often been associated with a decrease in blood pressure (BP) [9] and a lower risk of CVD mortality [10, 11]. Higher animal protein intake, on the other hand, is associated with a greater risk of hypertension [12] and CVD mortality [13]. The contrasting relationships of plant and animal protein intake with CVD risk may be attributed to the differential intrinsic amino acid (AA), fat, micronutrient, haem-iron, dietary fibre, and phytochemical compositions as well as their interactions with the gut microbiome [14, 15]. Using data from the USDA database [16], Lépine et al. [14] demonstrated that animal protein sources contain higher levels of essential amino acids (EAAs), including branched-chain amino acids (BCAAs) and aromatic amino acids, while plant protein sources are rich in nonessential AAs [14]. Evidently, higher levels of BCAAs [17, 18] and their short-chain acylcarnitine byproducts [19], as well as lower levels of certain nonessential AAs such as glycine [18, 20], serine [20], histidine [21] and others [22], have been associated with elevated BP and an increased risk of hypertension. This data suggests a link between the type of protein intake, the metabolome, and BP. However, ancillary research in different population groups is required to reinforce these findings. Corroborating evidence is needed to validate biomarkers that may be used to strengthen and support dietary recall data when assessing dietary risk.
The main aim of this study was to determine whether plant and animal protein intake may be differentially related to non-protein components (e.g., fibre, saturated fat or salt intake) or a metabolomic profile which in turn is associated with BP. We hypothesised that there will be a significant difference in the BP, body composition, non-protein component levels, and metabolomic profiles of participants consuming a low animal, high plant protein intake (low-risk dietary group) compared with those consuming a high animal, low plant protein intake (high-risk dietary group).
Methods
Study design and participant selection
The African Prospective study on the Early Detection and Identification of CVD and Hypertension (African-PREDICT) included 1202 young adults from communities in and around the Potchefstroom area in the North West Province of South Africa [23]. Inclusion criteria for the African-PREDICT study were 20–30 years of age, clinic BP < 140/90 mmHg during the screening phase, no self-reported chronic diseases or treatment thereof, HIV-uninfected, not pregnant or lactating. This study included N = 1008 participants from the African-PREDICT study with metabolomics and protein intake data. There was an equal sex (49.8% women and 50.2% men) and racial (49.9% Black and 50.1% White) distribution within the cohort.
All participants gave written informed consent prior to data collection. The African-PREDICT study complies with the Declaration of Helsinki, was approved by the Health Research Ethics Committee of the North-West University (NWU-00001-12-A1) and is registered on ClinicalTrials.gov (NCT03292094).
Questionnaire, anthropometric, and physical activity data
Self-reported age, sex (male/female), race (Black/White) and socioeconomic status (SES) data were obtained from validated General Health and Demographic Questionnaires. Dietary protein, fibre, and fat intakes were determined by three 24-h dietary recall interviews (including 1 weekend day) using a standardised dietary collection kit (example pictures, packages, measurement tools, and food models) and the five-step multiple-pass approach. Participants’ body weight (kg) (SECA electronic scales, SECA, Birmingham, UK), height (m) (SECA stadiometer, SECA, Birmingham, UK) and waist circumference (WC, cm) (anthropometric nonflexible tape measure, Holtain, Ltd, Crymych, UK) were measured in triplicate, with the average of the three measurements used, and body mass index (BMI) calculated [(kg)/height (m2)]. Participants wore a triaxial accelerometer for seven days during which total energy expenditure (TEE) was measured as an estimate of participants’ physical activity (ActiHeart; CamNtech, Cambridge, UK), and corrected for body weight (TEE/kg/day).
Ambulatory blood pressure monitoring
Ambulatory BP was measured in 30-min intervals during the day (06:00 to 22:00) and hourly at night (22:00 to 06:00). Participants were fitted with an appropriately sized brachial BP cuff on the non-dominant arm (Card(X)plore device, Meditech, Budapest, Hungary). In this study N = 979 participants had ≥12 successful day and ≥4 successful night inflations [24]. The mean successful inflation rate over the 24-h period was 88% with a standard deviation of 12.1%.
Biological sampling and biochemical analyses
Participants fasted from 22:00 on the evening prior to the day of data collection. Early morning spot urine and blood samples were collected from participants and immediately taken to the onsite laboratory for preparation and storage (stored at −80 ▫C). Serum total cholesterol, high- (HDL-C) and low- (LDL-C) density lipoprotein cholesterol, gamma-glutamyl transferase (GGT) and C-reactive protein (CRP) as well as glycated haemoglobin (HbA1c) from EDTA whole blood were measured using the Cobas Integra 400plus (Roche, Basel Switzerland). Amino acids and acylcarnitines were measured from spot urine samples using liquid chromatography-tandem mass spectrometry (LC-MS/MS) (Agilent 6410 LC-MS/MS system with 1200 series LC front-end) as previously described [19]. We applied a 50% CV filter to the data, and metabolites with more than 50% zero values were removed from the data matrix. Twenty-four-hour urine samples were collected from participants according to WHO/PAHO guidelines [25] to measure urinary sodium and potassium (Cobas Integra 400plus, Roche, Basel Switzerland). Estimated salt intake was calculated.
Statistical analyses
All data analyses were performed using SPSS statistical software (IBM Corp. Released 2021. IBM SPSS Statistics for Windows, Version 28.0. Armonk, NY: IBM Corp). Data distributions in the total population were inspected using skewness, kurtosis, histograms, and Q-Q normality plots. We stratified participants into low- and high-risk groups according to dietary protein intakes. Firstly, we determined the tertiles of plant and animal protein intake within Black men, Black women, White men, and White women respectively, since consumption patterns differed between these groups. All participants within the lowest tertile of animal protein intake and highest tertile of plant protein intake from the respective sex and racial group stratifications were classified as being in the low-risk group. Conversely, all participants within the lowest tertile of plant protein intake and highest tertile of animal protein intake from the respective sex and racial group stratifications were classified as being in the high-risk group. Comparisons of SES, anthropometric, BP, biochemical, and dietary intake profiles between low- and high-risk dietary groups were performed using independent-T tests (normally distributed data) and Mann–Whitney U tests (skewed data including protein intake and metabolite data). Analysis of covariance (ANCOVA) was used to determine whether BP differed significantly between the low- and high-risk groups (adjusted for BMI, total cholesterol, LDL-C, salt intake, potassium excretion, Na+/K+ ratio, total energy intake, dietary fibre intake, or saturated fat intake). In the total group, we investigated the relationships of total, plant, and animal protein intake with 24-h BP using Spearman correlations and multiple linear regression analyses (pairwise deletion of data) adjusting for sex, race, SES, age, BMI, TEE, Na+/K+ ratio, LDL-C, dietary fibre intake, and saturated fat intake. Mediation analyses were performed to determine whether the relationship of plant and animal protein intake with 24-h SBP was mediated by any of the measured covariates. The associations of amino acid and acylcarnitine profiles with the different dietary protein intakes in the total cohort were determined using Spearman correlations (unadjusted and adjusted for sex, race, age, BMI, TEE, and total energy intake). We subsequently determined if AA and acylcarnitine levels differed between the low-risk and high-risk dietary protein intake groups using Mann–Whitney U test. ANCOVA was performed, adjusting for BMI and total protein intake, or BMI and total energy intake, to determine whether metabolomic differences between groups were confounded by these covariates. The matrix subcommand was used to compute partial correlations based on Spearman Rho’s. To lower the false discovery rate of statistically significant relationships we calculated the adjusted p values using the Benjamini-Hochberg procedure (reported as q-values). Lastly, we investigated the associations between 24-h BP and metabolites that were found to be significantly different between the low- and high-risk protein intake groups (Spearman correlations and multiple linear regression analyses adjusting for sex, race, age, BMI, TEE, and total energy intake). Although protein intake and metabolite data were skewed, P–P plots in multiple linear regression models were examined to ensure normal distribution of residuals as well as inspecting the homoscedasticity of the data. The main dependent variable, 24-h BP, was normally distributed.
Results
The characteristics of this study cohort, aged 24 ± 3.12 years, are presented in Table 1. There was an equal sex and racial distribution between the low-risk (low animal, high plant protein intake) and high-risk (low plant, high animal protein intake) dietary groups. A greater proportion of the participants in the high-risk protein intake group were from a high SES (40% vs. 30% from low SES) while greater proportion of the low-risk protein intake group were from a low SES (45.5% vs. 25.7% from high SES).
Relationship between dietary protein intake and 24-h blood pressure
Participants within the high-risk protein intake group had higher 24-h SBP, but not DBP, than participants in the low-risk protein intake group (p = 0.011). Considering possible confounding factors (BMI, total cholesterol, LDL-C, salt intake, potassium excretion, Na+/K+ ratio, total energy intake, dietary fibre intake, and saturated fat intake), the difference between groups became non-significant after adjustment for BMI (p = 0.19), LDL-C (p = 0.053), potassium excretion (p = 0.26), Na+/K+ ratio (p = 0.09), or saturated fat intake (p = 0.15) (Supplementary Table 1).
Although total (ρ = 0.225; p < 0.001), plant (ρ = 0.074; p = 0.021) and animal (ρ = 0.193; p < 0.001) protein intake correlated positively with SBP (Fig. 1), the relationships lost significance with backward stepwise multiple regression models (adjusting for sex, race, SES, age, BMI, TEE, Na+/K+ ratio, LDL-C, dietary fibre intake, and saturated fat intake). In the total cohort, male sex, BMI (adj. R2 = 0.44; Std. β = 0.44; p < 0.001) and saturated fat (adj. R2 = 0.44; Std. β = 0.082; p = 0.008) were significantly and positively associated with 24-h SBP. Performing mediation analyses in the total group (Fig. 2, Supplementary Table 2), the relationship between plant protein intake and SBP was partially mediated by BMI (mediation: −63.3%) (Fig. 2A) and fully mediated by saturated fat intake (mediation: 49.6%) (Fig. 2C). The relationship between animal protein intake and SBP was partially mediated by both BMI (mediation: 16.7%) (Fig. 2B) and saturated fat intake (mediation: 35.5%) (Fig. 2D). When performing backward stepwise multiple regression in the low and high-risk groups respectively, we found that male sex and BMI remained significantly associated with SBP in both groups.
Mediating effect of BMI and saturated fat intake on the relationship of plant and animal protein intake with 24-hour systolic blood pressure. A Mediating effect of BMI on the relationship between plant protein intake and SBP; B Mediating effect of BMI on the relationship between animal protein intake and SBP; C Mediating effect of saturated fat intake on the relationship between plant protein intake and SBP; D Mediating effect of saturated fat intake on the relationship between animal protein intake and SBP. BMI Body mass index, M Mediator, SBP Systolic blood pressure, X independent variable, Y dependent variable
Relationship of dietary protein intake with urinary amino acids and acylcarnitines
Spearman correlations revealed opposing relationships of animal and plant protein intake with amino acids and acylcarnitines (Fig. 3). After adjusting for sex, race, BMI, and total protein intake, animal protein intake correlated positively with C0 [free]-carnitine (r = 0.142) and short-chain acylcarnitines C2 [acetyl]- (r = 0.163), C3 [propionyl]- (r = 0.113) and C5 [isovaleryl]-carnitine (r = 0.137) (all p and q < 0.05). Conversely, plant protein intake correlated positively with histidine (r = 0.093), methionine (r = 0.112), alanine (r = 0.127), beta-alanine (r = 0.090), glutamic acid (r = 0.090), glutamine (r = 0.096), glycine (r = 0.127), and proline (r = 0.132), but negatively with C2-carnitine (r = −0.123) (all p and q < 0.05).
Relationships of protein intake with urinary amino acids and acylcarnitines. A Unadjusted Spearman correlations of total, animal, and plant protein intake with urinary amino acids and acylcarnitines. B Partial Spearman correlations of animal and plant protein intake with amino acids and acylcarnitines adjusted for sex, ethnicity, BMI, TEE, and total protein intake. Solid bars present correlations with significant p < 0.05. *Indicates significant q < 0.05
Metabolite profiles of low animal, high plant protein intake (low-risk) vs. low plant, high animal protein intake (high-risk) groups
Comparisons of the metabolic profiles between the low-risk and high-risk dietary protein intake groups are shown in Supplementary Table 3. Participants within the high-risk group exhibited lower AA (EAAs: methionine and phenylalanine; non-essential AAs: alanine, aspartic acid, beta-alanine, glutamic acid, glutamine, glycine, proline, serine; AA derivatives: GABA and pyroglutamic acid) and C6 [hexanoyl] -carnitine levels, but higher C0-carnitine and short-chain acylcarnitines (C2- and C3-carnitine) levels (all p and q values < 0.05) compared to the low-risk group. After adjustment for BMI and total protein intake, which were significantly higher in the high-risk group, only beta-alanine levels remained significantly lower in the high-risk compared to the low-risk group (q < 0.001). Given the high collinearity of total protein intake and total energy intake (r = 0.731; p < 0.001), we did not adjust for both covariates simultaneously. After adjusting for BMI and total energy intake in sensitivity analyses, beta-alanine and glycine were significantly lower in the high-risk compared to the low-risk group (q = 0.018).
Associations of 24-h blood pressure with urinary amino acids and acylcarnitines related to protein intake
We subsequently determined whether metabolites that differed significantly between the high- and low-risk protein intake groups (Fig. 4) were associated with higher 24-h SBP. Analyses were adjusted for race, age, BMI, TEE, and total energy intake. In the total group, glycine (adj. R2 = 0.23; Std. β = −0.089; p = 0.005), GABA (adj. R2 = 0.23; Std. β = −0.103; p = 0.002), C0- (adj. R2 = 0.23; Std. β = 0.103; p = 0.001) and C3- (adj. R2 = 0.24; Std. β = 0.129; p < 0.001) levels associated with SBP (Table 2). Additionally, 24-h DBP inversely associated with beta-alanine (adj. R2 = 0.13; Std. β = −0.071; p = 0.036) and GABA (adj. R2 = 0.13; Std. β = −0.087; p = 0.015). All relationships lost significance with additional adjustment for sex. Stratified according to risk groups (Supplementary Table 4), we found that methionine (adj. R2 = 0.31; Std. β = −0.217; p = 0.034), glutamic acid (adj. R2 = 0.31; Std. β = −0.220; p = 0.031), glycine (adj. R2 = 0.31; Std. β = −0.234; p = 0.025), and proline (adj. R2 = 0.33; Std. β = −0.266; p = 0.010) associated inversely with SBP, and beta-alanine (adj. R2 = 0.15; Std. β = −0.277; p = 0.020) with DBP, in the low-risk protein intake group. The latter relationship between beta-alanine and DBP remained significant after additional adjustment for sex. In the high-risk group, serine associated inversely with SBP (adj. R2 = 0.23; Std. β = −0.223; p = 0.042).
Discussion
The main findings of this study included that (1) animal protein intake correlated positively with BMI and saturated fat intake which were the main determinants of higher SBP; (2) participants with a low animal, high plant protein intake (low-risk dietary group) had higher AAs and hexanoyl-carnitine, but lower free carnitine and short-chain acylcarnitine levels compared to the high-risk group; (3) in the low-risk group, higher levels of methionine, glutamic acid, glycine, proline and beta-alanine were related to BP. Ultimately, the means by which dietary protein intake contributes to BP may be attributed to the distinct protein characteristics.
Evidently, high animal protein intake [12], specifically red meat and processed meat [26,27,28,29,30], has been associated with higher BP and hypertension, while plant-based diets are associated with lower BP [9]. The contrasting relationships of plant and animal protein intake with CVD risk has been ascribed to the unique protein characteristics associated with different protein sources — including non-protein components (fibre, micronutrients, fats, carbohydrates, phytochemicals) and AA composition [14, 15, 31]. Plant-based protein sources typically contain less saturated fatty acids and more cardioprotective micronutrients, while animal protein sources are rich in saturated fats that contribute to an adverse cholesterol profile [15, 31]. In this study, participants with a high animal, low plant protein intake (high-risk) indeed had higher 24-h SBP compared to those with low animal, high plant protein intake (low-risk). However, the difference in SBP between the groups was mediated by BMI, LDL-C, potassium excretion (a proxy marker of potassium intake), and saturated fat intake—all of which were higher in the high-risk compared to the low-risk protein intake group. Unexpectedly, salt intake did not differ between the low-and high-risk protein intake groups and was not related to SBP. Although we found that the protein type itself was not an independent predictor for SBP when considering mediating factors, a diet high in animal protein intake likely increases SBP by increasing saturated fat intake and BMI.
While animal protein sources are reportedly comprised of higher EAAs and less non-essential AAs than plant protein sources [14], we found that total plant protein intake was positively associated with almost all AAs (EAAs, non-essential AAs, and AA derivatives) in the current study. It is possible that our observation may be attributed to specific animal and plant protein food sources consumed by the participants in this study population, however assessing the metabolic profiles with different animal and plant protein food sources was beyond the scope of this study and should therefore be investigated in the future. In the low-risk group, the AAs methionine, glutamic acid, glycine, proline, and beta-alanine were inversely related to BP. It is therefore likely that higher levels of these AAs observed in those with a plant rich diet may be protective against higher SBP. In the high-risk group, serine associated inversely with SBP. In the total study cohort, glycine, beta-alanine, GABA, free carnitine, and propionyl-carnitine were related to BP. Although it is beyond the scope of this study, sex had a confounding effect on the relationship between metabolites and BP. It is thus recommended that future studies investigate the role of sex on metabolomic pathways related to BP.
Methionine
The EAA, methionine, is generally lower in plant-based compared with animal-based protein sources (1% vs. 2.5% of the total protein), although, concentrations may vary amongst plant-based food sources [32]. The methionine content of potato, hemp, corn, and brown rice, for instance, were shown to be higher than that of oats, soy, and wheat [32]. It is possible that higher methionine levels in the low-risk group of this study, consuming a plant rich diet, may be attributed to the specific plant-based food sources consumed by the participants in this group. Our observation that increased methionine was inversely associated with BP in adults consuming a plant-rich diet contrasts with evidence from animal studies that suggest that a high methionine diet may increase CVD risk by promoting oxidative stress, inflammation, and vascular matrix remodelling [33]. Further research is needed to determine whether methionine from plant- and animal-based food sources may be differentially related to BP.
Glycine
Glycine is a conditional EAA and a major structural component of collagen [34]. Glycine is required to maintain healthy collagen turnover [34], and has anti-inflammatory and anti-oxidative functions [35]. In addition, glycine has been shown to promote endothelial nitric oxide synthase expression in aortic rings of Sprague-Dawley rats, which increases the bioavailability of vasodilatory nitric oxide (NO) [36]. Higher levels of glycine were previously observed in younger adults with decreased arterial stiffness [37], and has also been associated with lower central SBP [21]. In the total group, and particularly in the low-risk protein intake group, glycine was inversely related to 24-h SBP. In accordance with our findings, others have also reported an inverse relationship of glycine with BP and the risk of hypertension [20, 38,39,40].
Serine and proline
Serine may be obtained through dietary intake (soybeans, nuts, eggs, lentils, meat, and fish), or endogenously synthesised from glycine or glucose [41]. With regard to proline, ref. [42] reported that animal protein intake decreased significantly across increasing tertiles of dietary proline intake, while plant protein intake increased. Interestingly, the authors further demonstrated that proline from cheese or legumes were associated with increased BP, while proline from red meat was associated with lower SBP [42]. In this study cohort we found that serine and proline were significantly higher in adults consuming a diet rich in plant protein. Serine and proline were inversely associated with SBP in the high-risk and low-risk groups, respectively. The inverse relationships of serine and proline with SBP agree with findings from the INTERMAP study [22]. Our research group has also previously demonstrated that serine and proline levels are higher in young adults with decreased arterial stiffness [37], and that serine is inversely associated with central SBP [21].
Beta-alanine
Beta-alanine is a non-essential and non-proteinogenic AA, synthesised endogenously in the liver but may also be acquired through dietary intake of meat [43]. Beta-alanine is the rate limiting precursor of carnosine that exerts several protective roles in the vasculature [44]. In a recent review, ref. [44] outlined the physiological activities of carnosine (increased NO bioavailability, improved angiogenesis, inhibition of advanced glycation end products, anti-oxidative and anti-inflammatory) that impacts vascular health and thereby BP. Whether the inverse association between beta-alanine and DBP in this study (total group and low-risk group) may be mediated by the vascular effects of carnosine is unknown. It has been shown that increased DBP is strongly related to increased arterial stiffness [45], and that lower levels of beta-alanine is associated with increased arterial stiffness in children [46] and young adults [37] who exhibit early vascular aging.
GABA and glutamic acid
Plant-based foods are rich sources of GABA and glutamic acid [47]. Potatoes and tomatoes in particular have been shown to contain high quantities of GABA, while cereals, nuts, and legumes contain higher quantities of glutamic acid [47]. Advances in food technology have encouraged the use of microorganisms during food processing that will increase the GABA content of food. Generally, GABA concentrations are therefore also elevated in fermented products [48]. We found that urinary GABA and glutamic acid levels were indeed higher in adults consuming a plant protein rich compared to those consuming an animal protein rich diet. GABA is an inhibitory neurotransmitter that influences arterial pressure by regulating sympathetic outflow from the paraventricular nucleus (PVN) [49]. It is thus likely that higher levels of GABA may lead to suppressed sympathetic vasomotor outflow by the PVN, and thereby decrease vasoconstriction. Although glutamate (glutamic acid) is an excitatory neurotransmitter, the excitatory effects thereof can be attenuated by NO [49]. Stamler et al. [22] suggests that the favourable effect of dietary glutamic acid on BP, also observed in the IMTERMAP study, may be attributed to glutamate being a precursor of arginine, which, when converted to nitric oxide, is a potent vasodilator [22]. Notably, glutamic acid levels were shown to be higher in young adults with decreased arterial stiffness compared to those with increased stiffness [37].
Free carnitine
Dietary free carnitine is primarily acquired through animal protein sources but may also be synthesised endogenously from lysine and methionine [50]. In this study, we found that increased animal protein intake was associated with higher levels of urinary free carnitine (which increases in parallel with dietary free carnitine intake [50]). Dietary free carnitine is a main precursor for the gut microbiome-derived metabolite trimethylamine N-oxide (TMAO), which is associated with increased arterial stiffness and SBP [51]. Although TMAO was not determined in this study, we demonstrated that urinary free carnitine levels were associated with 24-h SBP, which is in accordance with previous findings reported by ref. [52]. Notably, it was further shown in the African-PREDICT study population that adults with greater arterial stiffness had higher levels of urinary free carnitine compared to those with less arterial stiffness [37].
Propionyl-carnitine
Propionyl-carnitine is a short-chain acylcarnitine that is derived from propionyl-CoA [53]. Propionyl-CoA can be produced through various metabolic pathways including the catabolism of BCAAs, oxidation of odd chain fatty acids, and the oxidation of cholesterol side chains [53]. In this study, urinary propionyl-carnitine, together with free carnitine and acetyl-carnitine, were higher in the group with higher animal protein consumption. Since we found no association between animal protein intake and BCAAs, it is possible that higher urinary propionyl-carnitine levels may reflect sufficient BCAA catabolism. Higher levels of short-chain acylcarnitines, but not medium- or long-chain acyl-carnitines, could reflect increased fatty acid beta-oxidation in adults consuming high animal protein diets. It is well known that fatty acid beta-oxidation plays an essential role in cardiac contractility [54], but there is also evidence that fatty acid beta-oxidation is utilised for endothelial-dependent vasodilation [55]. Our research group has previously reported a positive association between urinary propionyl-carnitine levels and left ventricular mass index [56], while also demonstrating higher levels of propionyl-carnitine in adults with increased arterial stiffness [37]. It is likely that the role of propionyl-carnitine in cardiovascular energetics may contribute to the positive association that we observed between propionyl-carnitine and 24-hour SBP in this study.
Future perspectives
This study demonstrates differential relationships of animal and plant protein intakes with AAs and acylcarnitines. Given the culturally diverse population, there may be significant value in investigating the metabolome of different food sources consumed by the different population groups in South Africa. Linking distinct metabolites, and thereby metabolic pathways, to specific food sources may assist in procuring more effective personalised approaches to dietary intervention. Additional health benefits may include the identification of metabolic pathways implicated in food allergies and gaining new perspectives on the medicinal properties of food.
Strengths and limitations
To our knowledge this is the first study investigating the triadic relationship between protein intake (total, plant, and animal), metabolites (amino acids and acylcarnitines), and 24-h BP in a young cohort from Sub-Saharan Africa. All measurements were conducted under highly controlled conditions at a well-equipped research facility. This hypothesis generating study is limited by its cross-sectional design and causality can therefore not be inferred. Limitations of 24-h dietary recall data may include errors in a participant’s memory or possible misperceptions of their food portions. The inclusion of known biomarkers associated with dietary protein intake such as urinary nitrogen would have been beneficial and should be considered in follow-up studies. This study made use of a targeted metabolomics approach, and further studies using untargeted metabolomics may identify additional metabolite classes related to protein intake that were not included in our study.
Conclusion
Our study suggests that a diet high in animal but low in plant protein intake may contribute to higher BP, while a plant rich diet may contribute to lower BP. Our findings support the notion that the differential relationships of protein type with BP is likely due to the unique protein characteristics (non-protein components and AA composition). Higher animal protein intake may be related to increased BMI and saturated fat intake, which are significant determinants of SBP. Furthermore, we demonstrated that adults with a plant protein rich diet had higher levels of urinary AAs together with lower free and short chain acylcarnitines compared to those with an animal protein rich diet. In the adults with a plant protein rich diet, AAs that were higher, inversely associated with SBP, suggesting a protective role of increased plant protein intake against higher BP.
References
Jeemon P, Séverin T, Amodeo C, Balabanova D, Campbell NRC, Gaita D, et al. World heart federation roadmap for hypertension–A 2021 update. Glob Heart. 2021;16:63 https://doi.org/10.5334/gh.1066.
NCD Risk Factor Collaboration. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021;398:957–80.
Food Agriculture Organization of the United Nations, World Health Organization. Sustainable healthy diets: guiding principles. Rome: FAO; WHO; 2019.
Herforth A, Arimond M, Álvarez-Sánchez C, Coates J, Christianson K, Muehlhoff E. A global review of food-based dietary guidelines. Adv Nutr. 2019;10:590–605.
de Roos B. Diet, blood pressure, and heart disease—precision nutrition approaches to understand response to diet and predict disease risk. Am J Clin Nutr. 2021;114:1581–2.
Brennan L, de Roos B. Nutrigenomics: lessons learned and future perspectives. Am J Clin Nutr. 2021;113:503–16.
Dong C, Bu X, Liu J, Wei L, Ma A, Wang T. Cardiovascular disease burden attributable to dietary risk factors from 1990 to 2019: a systematic analysis of the Global Burden of Disease study. Nutr Metab Cardiovasc Dis. 2022;32:897–907.
American Heart Association. Plant-Based Sources of Protein Infographic. 2020. https://www.heart.org/en/healthy-living/healthy-eating/eat-smart/nutrition-basics/plant-based-protein-infographic.
Gibbs J, Gaskin E, Ji C, Miller MA, Cappuccio FP. The effect of plant-based dietary patterns on blood pressure: a systematic review and meta-analysis of controlled intervention trials. J Hypertens. 2021;39:23–27.
Huang J, Liao LM, Weinstein SJ, Sinha R, Graubard BI, Albanes D. Association between plant and animal protein intake and overall and cause-specific mortality. JAMA Intern Med. 2020;180:1173–84.
Budhathoki S, Sawada N, Iwasaki M, Yamaji T, Goto A, Kotemori A, et al. Association of animal and plant protein intake with all-cause and cause-specific mortality in a Japanese cohort. JAMA Intern Med. 2019;179:1509–18.
Borgi L, Curhan GC, Willett WC, Hu FB, Satija A, Forman JP. Long-term intake of animal flesh and risk of developing hypertension in three prospective cohort studies. J Hypertens. 2015;33:2231–8.
Song M, Fung TT, Hu FB, Willett WC, Longo VD, Chan AT, et al. Association of animal and plant protein intake with all-cause and cause-specific mortality. JAMA Intern Med. 2016;176:1453–63.
Lépine G, Fouillet H, Rémond D, Huneau JF, Mariotti F, Polakof S. A scoping review: metabolomics signatures associated with animal and plant protein intake and their potential relation with cardiometabolic risk. Adv Nutr. 2021;12:2112–31.
Richter CK, Skulas-Ray AC, Champagne CM, Kris-Etherton PM. Plant protein and animal proteins: do they differentially affect cardiovascular disease risk? Adv Nutr. 2015;6:712–28.
Haytowitz DB, Ahuja JK, Wu X, Khan M, Somanchi M, Nickle MS, et al. USDA National Nutrient Database for Standard Reference, Legacy Release. Nutrient Data Laboratory, Beltsville Human Nutrition Research Center, ARS, USDA; 2019. https://doi.org/10.15482/USDA.ADC/1529216.
Flores-Guerrero JL, Groothof D, Connelly MA, Otvos JD, Bakker SJL, Dullaart RPF. Concentration of branched-chain amino acids is a strong risk marker for incident hypertension. Hypertension. 2019;74:1428–35.
Lin C, Sun Z, Mei Z, Zeng H, Zhao M, Hu J, et al. The causal associations of circulating amino acids with blood pressure: a Mendelian randomization study. BMC Med. 2022;20:414.
Strauss-Kruger M, Kruger R, Jansen Van Vuren E, Jacobs A, Louw R, Mels C. Identifying a metabolomics profile associated with masked hypertension in two independent cohorts: data from the African-PREDICT and SABPA studies. Hypertens Res. 2022;45:1781–93.
Louca P, Nogal A, Moskal A, Goulding NJ, Shipley MJ, Alkis T, et al. Cross-sectional blood metabolite markers of hypertension: a multicohort analysis of 44,306 individuals from the COnsortium of METabolomics Studies. Metabolites. 2022;12:601.
Mels CM, Delles C, Louw R, Schutte AE. Central systolic pressure and a nonessential amino acid metabolomics profile: the African prospective study on the early detection and identification of cardiovascular disease and hypertension. J Hypertens. 2019;37:1157–66.
Stamler J, Brown IJ, Daviglus ML, Chan Q, Kesteloot H, Ueshima H, et al. Glutamic acid, the main dietary amino acid, and blood pressure: the INTERMAP Study (International Collaborative Study of Macronutrients, Micronutrients and Blood Pressure). Circulation. 2009;120:221–8.
Schutte AE, Gona PN, Delles C, Uys AS, Burger A, Mels CM, et al. The African prospective study on the early detection and identification of cardiovascular disease and hypertension (African-PREDICT): design, recruitment and initial examination. Eur J Prev Cardiol. 2019;26:458–70.
Yang WY, Thijs L, Zhang ZY, Asayama K, Boggia J, Hansen TW, et al. Evidence-based proposal for the number of ambulatory readings required for assessing blood pressure level in research settings: an analysis of the IDACO database. Blood Press. 2018;27:341–50.
WHO/PAHO Regional Expert Group for Cardiovascular Disease Prevention through Population-wide Dietary Salt Reduction Sub-group for Research and Surveillance. Protocol for population level sodium determination in 24-hour urine samples. Switzerland: World Health Organization Geneva; 2010.
Ba DM, Gao X, Chinchilli VM, Liao D, Richie JP, Al-Shaar L. Red and processed meat consumption and food insecurity are associated with hypertension; analysis of the national health and nutrition examination survey data, 2003–2016. J Hypertens. 2022;40:553–60.
Masala G, Bendinelli B, Versari D, Saieva C, Ceroti M, Santagiuliana F, et al. Anthropometric and dietary determinants of blood pressure in over 7000 Mediterranean women: the European prospective investigation into cancer and nutrition-florence cohort. J Hypertens. 2008;26:2112–20.
Griep LMO, Seferidi P, Stamler J, Linda VAN, Queenie C, Tzoulaki I, et al. Relation of unprocessed, processed red meat and poultry consumption to blood pressure in East Asian and Western adults. J hypertens. 2016;34:1721.
Allen TS, Bhatia HS, Wood AC, Momin SR, Allison MA. State-of-the-art review: evidence on red meat consumption and hypertension outcomes. Am J Hypertens. 2022;35:679–87.
Zhang Y, Zhang D-Z. Red meat, poultry, and egg consumption with the risk of hypertension: a meta-analysis of prospective cohort studies. J Hum Hypertens. 2018;32:507–17.
Briggs MA, Petersen KS, Kris-Etherton PM. Saturated fatty acids and cardiovascular disease: replacements for saturated fat to reduce cardiovascular risk. Healthcare. 2017;5:29.
Gorissen SHM, Crombag JJR, Senden JMG, Waterval WAH, Bierau J, Verdijk LB, et al. Protein content and amino acid composition of commercially available plant-based protein isolates. Amino Acids. 2018;50:1685–95.
Chaturvedi P, Kamat PK, Kalani A, Familtseva A, Tyagi SC. High methionine diet poses cardiac threat: a molecular insight. J Cell Physiol. 2016;231:1554–61.
Meléndez-Hevia E, de Paz-Lugo P, Cornish-Bowden A, Cárdenas ML. A weak link in metabolism: the metabolic capacity for glycine biosynthesis does not satisfy the need for collagen synthesis. J Biosci. 2009;34:853–72.
Aguayo-Cerón KA, Sánchez-Muñoz F, Gutierrez-Rojas RA, Acevedo-Villavicencio LN, Flores-Zarate AV, Huang F, et al. Glycine: the smallest anti-inflammatory micronutrient. Intern J Mol Sci. 2023;24:11236.
Gómez-Zamudio JH, García-Macedo R, Lázaro-Suárez M, Ibarra-Barajas M, Kumate J, Cruz M. Vascular endothelial function is improved by oral glycine treatment in aged rats. Can J Physiol Pharm. 2015;93:465–73.
Craig A, Kruger R, Gafane-Matemane LF, Louw R, Mels CMC. Early vascular ageing phenotypes and urinary targeted metabolomics in children and young adults: the ExAMIN Youth SA and African-PREDICT studies. Amino Acids. 2023;55:1049–62.
Wittemans LBL, Lotta LA, Oliver-Williams C, Stewart ID, Surendran P, Karthikeyan S, et al. Assessing the causal association of glycine with risk of cardio-metabolic diseases. Nat Commun. 2019;10:1060.
Díaz-Flores M, Cruz M, Duran-Reyes G, Munguia-Miranda C, Loza-Rodríguez H, Pulido-Casas E, et al. Oral supplementation with glycine reduces oxidative stress in patients with metabolic syndrome, improving their systolic blood pressure. Can J Physiol Pharmacol 2013;91:855–60.
Arjmand B, Dehghanbanadaki H, Yoosefi M, Rezaei N, Mohammadi Fateh S, Ghodssi-Ghassemabadi R, et al. Association of plasma acylcarnitines and amino acids with hypertension: a nationwide metabolomics study. PloS one. 2023;18:e0279835.
Handzlik MK, Metallo CM. Sources and sinks of serine in nutrition, health, and disease. Annu Rev Nutr. 2023;43:123–51.
Teymoori F, Asghari G, Farhadnejad H, Nazarzadeh M, Atifeh M, Mirmiran P, et al. Various proline food sources and blood pressure: substitution analysis. Intern J Food Sci Nutr. 2020;71:332–40.
Trexler ET, Smith-Ryan AE, Stout JR, Hoffman JR, Wilborn CD, Sale C, et al. International society of sports nutrition position stand: Beta-Alanine. J Intern Soc Sports Nutr. 2015;12:30.
Feehan J, Hariharan R, Buckenham T, Handley C, Bhatnagar A, Baba SP, et al. Carnosine as a potential therapeutic for the management of peripheral vascular disease. Nutr Metab Cardiovasc Dis. 2022;32:2289–96.
Botha D, Breet Y, Schutte AE. Comparing the associations of clinic vs. ambulatory blood pressure with subclinical organ damage in young healthy adults: the African-PREDICT study. Hypertens Res. 2021;44:840–9.
Erasmus D, Mels Carina MC, Louw R, Lindeque JZ, Kruger R. Urinary metabolites and their link with premature arterial stiffness in Black boys: the ASOS Study. Pulse. 2018;6:144–53.
Pencheva D, Teneva D, Denev P. Validation of HPLC method for analysis of gamma-aminobutyric and glutamic acids in plant foods and medicinal plants. Molecules. 2022;28:84.
Ramos-Ruiz R, Poirot E, Flores-Mosquera M. GABA, a non-protein amino acid ubiquitous in food matrices. Cogent Food Agriculture. 2018;4:1534323.
Martins-Pinge MC, Mueller PJ, Foley CM, Heesch CM, Hasser EM. Regulation of arterial pressure by the paraventricular nucleus in conscious rats: interactions among glutamate, GABA, and nitric oxide. Front Physiol. 2013;3:490.
Rebouche CJ. Carnitine. In: Ross AC, Caballero B, Cousins RJ, Tucker KL, Ziegler RT, editors. Modern Nutrition in Health and Disease 11th Ed. Burlington: MA: Jones & Bartlett Learning; 2014.
Brunt VE, Casso AG, Gioscia-Ryan RA, Sapinsley ZJ, Ziemba BP, Clayton ZS, et al. Gut microbiome-derived metabolite trimethylamine n-oxide induces aortic stiffening and increases systolic blood pressure with aging in mice and humans. Hypertension. 2021;78:499–511.
Mels C, Schutte A, Erasmus E, Huisman H, Schutte R, Fourie C, et al. L-Carnitine and long-chain acylcarnitines are positively correlated with ambulatory blood pressure in humans: the SABPA Study. Lipids. 2013;48:63–73.
Trefely S, Lovell CD, Snyder NW, Wellen KE. Compartmentalised acyl-CoA metabolism and roles in chromatin regulation. Mol Metab. 2020;38:100941.
Lopaschuk GD, Ussher JR, Folmes CDL, Jaswal JS, Stanley WC. Myocardial fatty acid metabolism in health and disease. Physiol Rev. 2010;90:207–58.
Wilson C, Lee MD, Buckley C, Zhang X, McCarron JG. Mitochondrial ATP production is required for endothelial cell control of vascular tone. Function. 2023;4:zqac063.
du Toit WL, Kruger R, Gafane-Matemane LF, Schutte AE, Louw R, Mels CMC. Using urinary metabolomics to identify metabolic pathways linked to cardiac structural alterations in young adults: the African-PREDICT study. Nutr Metab Cardiovasc Dis. 2023;33:1574–82.
Acknowledgements
The authors are grateful to all individuals who voluntarily participated in the African-PREDICT study. The dedication of the support and research staff as well as students at the Hypertension Research and Training Clinic at the North-West University are also duly acknowledged.
Funding
The research funded in this manuscript is part of an ongoing larger research project financially supported by the South African Medical Research Council (SAMRC) with funds from National Treasury under its Economic Competitiveness and Support Package; the South African Research Chairs Initiative (SARChI) of the Department of Science and Technology and National Research Foundation (NRF) of South Africa (GUN 86895); SAMRC with funds received from the South African National Department of Health, GlaxoSmithKline R&D (Africa Non-Communicable Disease Open Lab grant), the UK Medical Research Council and with funds from the UK Government’s Newton Fund; and corporate social investment grants from Pfizer (South Africa), Boehringer-Ingelheim (South Africa), Novartis (South Africa), the Medi Clinic Hospital Group (South Africa) and in-kind contributions of Roche Diagnostics (South Africa). This work is based on the research supported in part by the NRF of South Africa (Grant Number: UID: 138499). Any opinion, findings, and conclusions or recommendations expressed in this material are those of the authors, and therefore, the NRF does not accept any liability in this regard. Open access funding provided by North-West University.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
MP, TvZ, RK, EJvV, AJ, RL, and CM reported no COI. Scholarship or donation: MSK (Postdoctoral grant from the National Research Foundation, South Africa).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Strauss-Kruger, M., Pieters, M., van Zyl, T. et al. Urinary metabolomics signature of animal and plant protein intake and its association with 24-h blood pressure: the African-PREDICT study. Hypertens Res 47, 2456–2470 (2024). https://doi.org/10.1038/s41440-024-01767-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-024-01767-8
- Springer Nature Singapore Pte Ltd.
Key words
This article is cited by
-
Amino acid profiles associated with plant-rich protein diets may contribute to lower blood pressure
Hypertension Research (2024)