Abstract
Aim In clinically challenging scenarios with limited bone height and anatomical restrictions, the use of short implants have been proposed as a potential treatment strategy. The purpose of this retrospective study was to evaluate the clinical outcomes of short implants supporting prostheses in the posterior premolar region of the maxilla and mandible.
Materials and methods A total of 30 patients requiring short 6 mm length implant placement in the posterior premolar region were included. Following a period of osseointegration, the implants were restored with either single crowns, fixed bridges or implant-supported removable overdentures. Implant and prosthetic survival with technical complications were recorded.
Results In total, 45 implants were placed, with four failures reported before loading in two patients, resulting in a patient implant survival rate of 93.3% over the two-year follow-up. There was no statistically significant difference found between implant failure and arch placement. Prosthetic survival was 100% and minor technical complications recorded were low.
Conclusion This study showed that short 6 mm implants could provide a viable treatment option, with high survival rates comparable with alternative bone augmentation procedures. Further research with longer observation periods would be required to validate these current findings.
Key points
-
Analysis of survival rates with the use of short implants.
-
Comparison with alternate invasive bone augmentation procedures.
-
Evaluating implant placement in areas of anatomical restrictions.
Similar content being viewed by others
Introduction
The use of dental implants has been widely advocated for predictable success in oral rehabilitation. However, limited bone volume and anatomical constraints, such as those presented by the maxillary sinus and inferior alveolar nerve, can pose significant challenges, particularly in the posterior regions of the maxilla and mandible.1 Moreover, sinus pneumatisation and resorption of the alveolar ridge following exodontia can result in inadequate availability of vertical bone height. In such clinical scenarios, clinicians may consider additional surgical procedures to augment bone, such as guided bone regeneration, block grafting, sinus elevation, inferior alveolar nerve transposition and distraction osteogenesis.2,3,4 Although these procedures have demonstrated success, they are more invasive and entail more morbidity, increased treatment time and higher costs, which may act as deterrents for patients seeking implant treatment.
An alternative to conventional implants and complex surgical procedures to simplify treatment is the use of short implants. Previous systematic reviews and meta-analyses have demonstrated that short implants exhibit comparable survival rates to standard-sized implants.5,6,7 Advances in technology, such as surface modifications and improved macrodesign features, have further enhanced their performance.8 Previous recommendations have supported the rigid splinting of short implants, particularly in the posterior regions, to increase functional surface area and improve occlusal force distribution.9,10 Despite this, most studies have focused on single-crown restorations or combined splinted crowns, with limited analysis on the comparison with varying restoration designs, including their use with removable prostheses.
Traditionally, dental implant failures have been classified as either biological or technical in nature.11 Although biological failures have been extensively studied with measures of marginal bone loss, the same criteria applied for success may prove more detrimental in cases with a pre-existing shorter implant length. Mechanical failures, although less commonly reported, include implant and abutment fractures, screw loosening and ceramic chipping as the most frequently encountered. Additionally, factors related to the crown, such as the occlusal area and higher crown-to-implant ratio with short implants, may alter the biomechanical behaviour of the implant and surrounding tissues, potentially leading to complications and failures.12
The aim of this retrospective study was to evaluate clinical outcomes, including implant and prosthetic survival with technical complications, associated with the use of short 6 mm implants supporting prostheses in the posterior premolar region of the maxilla and mandible over a two-year period. While it is recognised that this study has a shorter-term follow-up, the results should therefore be interpreted with a degree of caution.
Materials and methods
Study design
This retrospective study was performed in a single-centre university dental hospital. All study participants recruited signed an informed written consent before undertaking any treatment. The study design was reviewed by the local ethics committee within the institution. The study was deemed to adhere to the guidelines for reporting observational studies and ethical approval was not required.13
The hospital implant database was used to obtain the sample of patients, which was done by reviewing the implants ordered and subsequently filtering those to include 6 mm length implants only. Data collection was completed retrospectively by assessing digital records at two years following treatment and data were recorded for the following domains: sex, smoking status, periodontal history, ASA (American Society of Anaesthesiologists) status, indication for treatment and survival rates.
Patient selection
To be recruited for the study, the patients had to meet the following inclusion criteria: at least 18 years of age; systematically healthy; edentulism in the posterior premolar region of the maxilla or mandible; and available bone volume for the placement of short 6 mm implants. The following exclusion criteria were applied: previous bone grafting at the planned implant site; active caries or periodontal disease; head and neck radiation >60 gy; and intravenous bisphosphonates. The presence of periodontal disease was identified by the patient's BPE (Basic Periodontal Examination) score, and those having a score of three or higher were excluded. None of the exclusion criteria applied to patients in the dataset of this study.
Baseline examination
All patients included in the study were examined for caries and periodontal status where applicable at the initial consultation stage. If periodontal therapy was required, patients were subsequently referred to have this completed before implant placement in accordance with the current periodontology management guidelines.14 Impressions were taken to create a wax-up of the planned prosthetic component, together with a surgical stent if required to aid surgical planning.
Surgical procedure
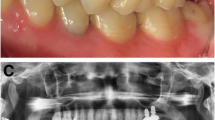
The implant surgery was performed according to the protocol of the manufacturer, with cases being performed under local anaesthesia or with intravenous sedation. Radiographic investigations, including plain imaging or cone beam computed tomography scans, were obtained to determine bone availability and proximity to anatomical structures, such as the maxillary sinus and mandibular canal (Fig. 1). Implant placements were carried out by multiple operators across different specialties and surgical notes were reviewed during data collection to evaluate the treatment protocol followed. All patients selected required either single or multiple short 6 mm implants in the posterior premolar region (Fig. 2). Antibiotics were given pre-operatively as a stat dose of 3 g amoxicillin, or 600 mg clindamycin if allergic to penicillin. Following mid-crestal incisions or raising of full-thickness mucoperiosteal flaps as necessary, a surgical stent was used if constructed overlying the occlusal plane to determine the position of the osteotomy preparation (Fig. 3). The osteotomy site was prepared using the sequence of burs recommended by the manufacturer from the initial twist drill to the step drills up to the diameter required for the implant.
All implants placed were 6 mm in length, Astra Tech EV (Dentsply Sirona, North Carolina, USA), and were 3.6, 4.2 or 4.8 mm in diameter. Implant sites were prepared with a safety margin of at least 2 mm relative to the maxillary sinus floor or mandibular canal before placement (Fig. 4). No additional bone augmentation was undertaken at the implant site. In accordance with the two-stage surgical protocol, cover screws were tightened onto the implants and the flaps were repositioned and sutured to allow submerged healing for 12 weeks. Surgical complications such as pain, infection or other adverse events were recorded if noted. Provisional prosthetic restorations could be worn during the healing phase but adjustments may have been required to avoid excessive loading.
Prosthetic procedure
Following a 12-week healing period, the cover screws were uncovered and replaced with a healing abutment to allow for transmucosal healing and to manually assess implant stability at this stage. Impressions were then taken and provisional restorations fabricated together with the completion of any additional restorative requirements (Fig. 5). Definitive prostheses in the form of single-crown restorations, fixed bridges, or removable implant-supported overdentures were subsequently fitted within one month of the second-stage surgery (Fig. 6). Clinical follow-ups were performed after six months and yearly up to the two-year observation period covered in this study. Patients also continued regular follow-ups with their general dental practitioner. At each visit, implant and prosthetic survival was evaluated together with any complications and clinical parameters were recorded.
Outcome measures
Implant survival was defined as implants that were in situ and functioning at the time of follow-up. Implant success was based on the absence of clinical signs of pain, infection and mobility, with no radiographic features of failed osseointegration.15 Owing to the retrospective design of the study, not all parameters for these criteria were available. Consequently, the decision was made to assess implant survival. With regards to implant failure, this was classified as either early with the need for implant removal due to the absence of osseointegration before loading, or late due to excess bone loss after loading.
Prosthetic evaluation was recorded from initial placement to the end of the two-year observational period. Survival was defined as the prosthesis still being in function despite the need for any smaller renewals and replacement not being required due to extensive fracture or inferior aesthetics.15
Any adverse technical complications that occurred during the follow-up period were recorded, including screw loosening or fractures, ceramic fractures and fracture of the implant or prosthetic abutment. Prostheses with minor chipping, occlusal roughness and minimal contour deficiencies that did not require replacement were regarded as successful.
Statistical analysis
Statistical analysis was performed using SPSS (IBM Corporation, New York, USA). The results of the clinical parameters and quantitative data are presented using descriptive methods including the mean, standard deviation, and range for the outcome variables. Tables of implant and prosthetic success rates have been presented and the level of significance for comparisons was set at 0.05.
Results
Demographic data
A total of 30 patients (12 men and 18 women; mean age = 46 years; range = 29-80 years) that fitted the inclusion criteria were included in the study. From analysis of the patient characteristics included, the majority were non-smokers without a history of periodontal disease that required a maintenance programme prior (Table 1).
A total of 45 Astra Tech EV 6 mm implants were placed, with 33 in the maxilla and 12 in the mandible. From the implants placed, 31 (68.9%), were 3.6 mm in diameter, 12 (26.7%) were 4.2 mm in diameter, and the remaining two (4.4%) were 4.8 mm in diameter. All implants selected were placed in the posterior premolar sites (Table 2). The cases enrolled fitted the established priority groups for patients eligible to receive NHS-funded dental implants as per the Royal College of Surgeons (RCS) guidelines.16 The majority of these cases selected were for patients with hypodontia or dental trauma, respectively (Table 3). Following a delayed loading approach, the implants were restored with either single crowns, fixed bridges or implant-supported removable overdentures.
Implant survival
Four implants in two patients failed, resulting in an implant survival rate of 91.1% at the implant level and 93.3% at the patient level. All four implants lost were early within the first three months before loading, with two implants in one patient from the maxilla, and two implants in another patient from the mandible. The implants were removed due to clinical signs of mobility and loss of osseointegration with no objective signs of infection observed (Table 4). No further implants were lost after loading during the two-year follow-up period and there was no statistically significant different between failure and loading arch.
Prosthetic survival
Prosthetic failures were assessed15 and there were no adverse prosthetic events that occurred during the evaluation period with survival recorded as 100%. The two implants that failed in the mandible were planned to have single implant-retained crowns but were lost before loading. The two failures in the maxilla were the distally positioned implants supporting an implant-retained overdenture. Despite their loss, the prosthesis was still fabricated and in function at the end of the follow-up period (Table 5).
Technical complications
In total, only three implants exhibited technical complications, which included screw loosening and minor ceramic fractures (Table 6). None of these required prosthesis replacement, with the overall complication rate at the two-year follow-up being 6.6%.
Discussion
The current study demonstrated that the use of 6 mm implants is a viable option for supporting prostheses in the posterior premolar region of both the maxilla and mandible, in the context of the two-year follow-up period assessed in this study. The short implants were successfully loaded after a delayed approach and exhibited a high survival rate of 93.3%, which is consistent with previous systematic reviews and meta-analyses.17,18 Notably, all implant failures were early in nature and no implants were lost after loading, with only minor technical complications encountered during the two-year follow-up period.
Several factors that may influence the success of short implants have been examined. Studies have found that smokers and those with poorer bone quality can experience lower survival rates.19,20,21 In this study, an equal number of implant losses were observed in both the maxilla and mandible, and no significant difference was detected between the two arches in terms of implant failure. Two of the implant failures in the mandible occurred in a patient who was a smoker with an additional confounding risk factor. Meanwhile, the two implants that failed in the maxilla were supporting an implant-retained overdenture. Therefore, it is possible that the increased load of the overlying prosthesis may have contributed to the implant failures. Overall, these findings suggest that patient-related factors, such as smoking status and bone quality, as well as prosthesis-related factors, such as implant load, should be carefully considered when using short implants.
Previous research has suggested that short implants can achieve clinical outcomes comparable to longer implants placed in augmented bone.22,23,24 However, wider implant bodies have often been used to compensate for the lack of implant height. Functional load on narrow implants is distributed over a smaller surface area, resulting in higher loads that can lead to accelerated bone remodelling and loss. Despite this, the findings of this study show no significant association between implant diameter and implant failure, as two implants failed in the narrow diameter (3.6 mm) group and two in the regular diameter (4.2 mm) group. There were no implants that failed in the wide diameter (4.8 mm) group, although this group had the smallest sample size. These findings suggest that while wider implant bodies may be used to offset the effects of shorter implant heights, implant diameter does not appear to have a significant impact on survival.
In this study, the analysis conducted included several covariates and found no increase in the risk of prosthetic failure associated with any of the potential risk factors assessed. Additionally, no prosthetic failures were reported during the evaluation period. The only complications observed during the follow-up period were screw loosening and minimal ceramic chipping, which occurred in 6.6% of cases. While this was slightly higher than previous reports, it should be noted that prosthetic complications are often under-reported in the literature.25 From a clinical standpoint, while these complications are typically considered technical failures, they were easily repaired and none of them resulted in the need for prosthesis replacement.
It has been hypothesised in the literature that patients with periodontitis may experience a greater number of biological complications, although implant survival rates do not seem to differ from those of healthy patients.26,27,28 The findings of the present study are consistent with this. This study included patients with a history of periodontitis but excluded those with active periodontal disease and there was no statistically significant difference in implant survival observed between healthy patients and those with a history of periodontitis. However, as there are only a limited number of studies available on the impact of periodontal disease on short implant survival, it can be challenging to draw definitive conclusions. Further research is therefore necessary to analyse the influence of periodontitis on the long-term success rate of short implants.
The present study provides a valuable insight into the use of short implants in supporting prostheses with a delayed loading approach in the posterior premolar region of the maxilla and mandible. However, it should be noted that the follow-up period may not provide a sufficient length of time to evaluate the long-term impact on survival as a high loading force on a short implant with limited contact with bone could exert its influence over time. While the current results are encouraging, the authors acknowledge that more research on longer-term survival is required to endorse these findings. If the efficacy of short implants is validated, they may become the preferred treatment modality due to their simplicity and cost-effectiveness, as well as the potential to avoid complications associated with augmentation procedures.29,30
A further limitation of the current study is that it was not designed as a randomised clinical trial with an augmentation procedure and placement of longer implants as a control group. Given that the study involved implant treatment performed by multiple operators, prior calibration was not achievable due to constraints of the setting in a teaching institution. Despite this, the short-term results suggest the use of 6 mm implants were beneficial as they offered favourable results and a safe treatment protocol with minimal complications. Further studies are warranted to expand the patient population beyond a single-centre university setting and to increase the sample size. Additionally, analysis of marginal bone loss over the study period would augment the value of these findings.
Conclusion
Within the limitations of this study, it can be concluded that the use of short 6 mm implants in the posterior maxilla and mandible region can serve as a viable treatment option, as they have demonstrated high survival rates throughout the two-year follow-up period. The study failed to identify any direct correlation between implant failure and arch placement. Further research, including a longer follow-up period with study designs that entail comparisons between augmentation procedures, would contribute to the existing body of evidence available and to support these conclusions.
Data availability
Not applicable.
References
Bell R B, Blakey G H, White R P, Hillebrand D G, Molina A. Staged reconstruction of the severely atrophic mandible with autogenous bone graft and endosteal implants. J Oral Maxillofac Surg 2002; 60: 1135-1141.
Morand M, Irinakis T. The challenge of implant therapy in the posterior maxilla: providing a rationale for the use of short implants. J Oral Implantol 2007; 33: 257-266.
Felice P, Cannizzaro G, Barausse C, Pistilli R, Esposito M. Short implants versus longer implants in vertically augmented posterior mandibles: a randomised controlled trial with 5-year after loading follow-up. Eur J Oral Implantol 2014; 7: 359-369.
Renouard F, Nisand D. Impact of implant length and diameter on survival rates. Clin Oral Implants Res 2006; 17: 35-51.
Pommer B, Frantal S, Willer J, Posch M, Watzek G, Tepper G. Impact of dental implant length on early failure rates: a meta-analysis of observational studies. J Clin Periodontol 2011; 38: 856-863.
Telleman G, Raghoebar G M, Vissink A, den Hartog L, Huddleston Slater J J, Meijer H J. A systematic review of the prognosis of short (<10 mm) dental implants placed in the partially edentulous patient. J Clin Periodontol 2011; 38: 667-676.
Mezzomo L A, Miller R, Triches D, Alonso F, Shinkai R S. Meta-analysis of single crowns supported by short (<10 mm) implants in the posterior region. J Clin Periodontol 2014; 41: 191-213.
Buser D, Janner S F, Wittneben J G, Bragger U, Ramseier C A, Salvi G E. 10-year survival and success rates of 511 titanium implants with a sandblasted and acid-etched surface: a retrospective study in 303 partially edentulous patients. Clin Implant Dent Relat Res 2012; 14: 839-851.
Misch C E, Steignga J, Barboza E, Misch-Dietsh F, Cianciola L J, Kazor C. Short dental implants in posterior partial edentulism: a multicenter retrospective 6-year case series study. J Periodontol 2006; 77: 1340-1347.
Rossi F, Lang N P, Ricci E, Ferraioli L, Marchetti C, Botticelli D. Early loading of 6-mm short implants with a moderately rough surface supporting single crowns - a prospective 5-year cohort study. Clin Oral Implants Res 2015; 26: 471-477.
Quaranta A, Piemontese M, Rappelli G, Sammartino G, Procaccini M. Technical and biological complications related to crown to implant ratio: a systematic review. Implant Dent 2014; 23: 180-187.
Blanes R J. To what extent does the crown-implant ratio affect the survival and complications of implant-supported reconstructions? A systematic review. Clin Oral Implants Res 2009; 20: 67-72.
Von Elm E, Altman D G, Egger M, Pocock S J, Gøtzsche P C, Vandenbroucke J P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 2014; 12: 1495-1499.
Sanz M, Herrera D, Kebschull M et al. Treatment of stage I-III periodontitis - The EFP S3 level clinical practice guideline. J Clin Periodontol 2020; 47: 4-60.
Papaspyridakos P, Chen C-J, Singh M, Weber H-P, Gallucci G O. Success criteria in implant dentistry: a systematic review. J Dent Res 2012; 91: 242-248.
Chin J S, Rees J, Addy L. The provision of dental implants: current practice among university and hospital specialists in restorative dentistry within the UK and Ireland. Br Dent J 2020; 1: 39-43.
Srinivasan M, Vazquez L, Rieder P, Moraguez O, Bernard J P, Belser U C. Survival rates of short (6 mm) micro-rough surface implants: a review of literature and meta-analysis. Clin Oral Implants Res 2014; 25: 539-545.
Annibali S, Cristalli M P, Dell'Aquila D, Bignozzi I, La Monaca G, Pilloni A. Short dental implants: a systematic review. J Dent Res 2012; 91: 25-32.
Sun H L, Huang C, Wu Y R, Shi B. Failure rates of short (≤ 10 mm) dental implants and factors influencing their failure: a systematic review. Int J Oral Maxillofac Implants 2011; 26: 816-825.
Sato Y, Shindoi N, Hosokawa R, Tsuga K, Akagawa Y. A biomechanical effect of wide implant placement and offset placement of three implants in the posterior partially edentulous region. J Oral Rehabil 2000; 27: 15-21.
Romeo E, Ghisolfi M, Rozza R, Chiapasco M, Lops D. Short (8-mm) dental implants in the rehabilitation of partial and complete edentulism: a 3- to 14-year longitudinal study. Int J Prosthodont 2006; 19: 586-592.
Cannizzaro G, Felice P, Leone M, Viola P, Esposito M. Early loading of implants in the atrophic posterior maxilla: lateral sinus lift with autogenous bone and Bio-Oss versus crestal mini sinus lift and 8-mm hydroxyapatite-coated implants. A randomised controlled clinical trial. Eur J Oral Implantol 2009; 2: 25-38.
Felice P, Checchi V, Pistilli R, Scarano A, Pellegrino G, Esposito M. Bone augmentation versus 5-mm dental implants in posterior atrophic jaws. Four-month post-loading results from a randomised controlled clinical trial. Eur J Oral Implantol 2009; 2: 267-281.
Esposito M, Pellegrino G, Pistilli R, Felice P. Rehabilitation of postrior atrophic edentulous jaws: prostheses supported by 5 mm short implants or by longer implants in augmented bone? One-year results from a pilot randomised clinical trial. Eur J Oral Implantol 2011; 4: 21-30.
Rossi F, Botticelli D, Cesaretti G, De Santis E, Storelli S, Lang N P. Use of short implants (6 mm) in a single-tooth replacement: a 5-year follow-up prospective randomized controlled multicenter clinical study. Clin Oral Implants Res 2016; 27: 458-464.
Cecchinato D, Bengazi F, Blasi G, Botticelli D, Cardarelli I, Gualini F. Bone level alterations at implants placed in the posterior segments of the dentition: outcome of submerged/non-submerged healing. A 5-year multicenter, randomized, controlled clinical trial. Clin Oral Implants Res 2008; 19: 429-431.
Omran M T, Miley D D, McLeod D E, Garcia M N. Retrospective assessment of survival rate for short endosseous dental implants. Implant Dent 2015; 24: 185-191.
Correia F, Gouveia S, Felino A C, Costa A L, Almeida R F. Survival Rate of Dental Implants in Patients with History of Periodontal Disease: A Retrospective Cohort Study. Int J Oral Maxillofac Implants 2017; 32: 927-934.
Esposito M, Grusovin M G, Felice P, Karatzopoulos G, Worthington H V, Coulthard P. The efficacy of horizontal and vertical bone augmentation procedures for dental implants - a Cochrane systematic review. Eur J Oral Implantol 2009; 2: 167-184.
Lee H-W, Lin W-S, Morton D. A retrospective study of complications associated with 100 consecutive maxillary sinus augmentations via the lateral window approach. Int J Oral Maxillofac Implants 2013; 28: 860-868.
Acknowledgements
The authors would like to thank Dr Jared Smith for their independent review and approval of the statistical analysis.
Author information
Authors and Affiliations
Contributions
Murtaza Hirani led the data collection, analysis of results and manuscript writing. Hannah Arnantha collected the data and contributed to the manuscript writing. Azza Al-Mossallami contributed to the manuscript writing. George Paolinelis reviewed the final manuscript.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest.
The R&D Governance Facilitator at the NIHR GSTT/KCL Biomedical Research Centre confirmed that ethical approval was not required for this retrospective study. All study participants recruited signed an informed written consent before undertaking any treatment.
Rights and permissions
Open Access. This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0.© The Author(s) 2024.
About this article
Cite this article
Hirani, M., Arnantha, H., Al-Mossallami, A. et al. Clinical outcomes of short dental implants supporting prostheses in the posterior region. Br Dent J (2024). https://doi.org/10.1038/s41415-024-7610-6
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41415-024-7610-6
- Springer Nature Limited