Abstract
Attention-deficit/hyperactivity disorder (ADHD) is a prevalent, chronic, and impairing mental health disorder of childhood. Decades of empirical research has established a strong evidence-based intervention armamentarium for ADHD; however, limitations exist in regards to efficacy and effectiveness of these interventions. We provide an overview of select evidence-based interventions for children and adolescents, highlighting potential approaches to further improving the efficacy and effectiveness of these interventions. We conclude with broader recommendations for interventions, including considerations to moderators and under-explored intervention target areas as well as avenues to improve access and availability of evidence-based interventions through leveraging underutilized workforces and leveraging technology.
Similar content being viewed by others
Evidence-based treatments for ADHD - an Overview
Multiple groups, committees, and professional organizations have provided the field with recommendations for evidence-based treatment approaches for ADHD. There is clear consensus across these recommendations that pharmacological treatments, notably stimulant medication, psychosocial treatments, and a combination of these two approaches have the strongest evidence base. Table 1 provides a brief overview of the major conclusions of each guideline for the treatment of ADHD in children. It is clearly recommended that families should receive psychoeducation regarding ADHD, and that the evidence-based psychosocial treatments are behavioral parent training (BPT), behavioral interventions in classroom and peer settings, and organizational skills training [1,2,3,4,5].
There are inconsistencies among the guidelines that make broad statements of consensus difficult. For instance, there are differences in precision in recommendations for psychosocial treatments, with some very broad in scope [6] compared to others with more precise recommendations regarding particular treatment types (e.g., BPT [2]) and particular populations (e.g., children under six; [5]). Broad suggestions of seeking “psychological” or “educational” treatment is unhelpful in some guidelines and practice parameters, as there are many approaches that fall under this category and some are clearly efficacious whereas other approaches commonly deployed do not have evidence of efficacy for ADHD [1,2,3,4]. There are also differences in the strength of recommendations, with more contemporary guidelines emphasizing multimodal treatments more so than older guidelines. However, perhaps most notably, there is not clear consensus among the recommendations on the best sequence or combination of treatments for ADHD, even though this is a key question for most families pursuing treatment for ADHD. It is also important to note that most guidelines focus on proximal ADHD treatment – as ADHD is now conceptualized as a life-course persistent disorder [7], treatment efforts will need to be protracted across time and appropriate for evolving developmental levels.
Efforts at improving efficacy and effectiveness of psychosocial intervention for ADHD: what do we know and where do we go?
Given the prominent role of psychosocial, primarily behavioral interventions, for ADHD, we highlight the evidence for several of these key interventions, integrating the literature on improving efficacy and effectiveness of these interventions. We also discuss digital therapeutics given the explosion in its availability and purported efficacy for children with ADHD. Following this, we close with potential broad future directions for psychosocial treatments for children with ADHD.
Behavioral parent training
Behavioral parent training (BPT) is likely the most well-studied psychosocial intervention for children’s mental health disorders, including for ADHD [8]. It serves as the first line intervention approach for younger children with ADHD and is an integral part of comprehensive intervention approaches for school-age children with ADHD. Importantly, BPT is less studied in adolescents with ADHD. Although parenting is not etiological to ADHD, there are clear reasons to focus on parenting when supporting a child with ADHD. Of primary importance is that raising a child with ADHD is stressful, and not surprisingly, elicits ineffectual parenting practices (e.g., inconsistent, harsh, lax, overreactive, less responsive). As a result, parents often have lower parenting efficacy/competence, higher levels of coercive management practices, utilize maladaptive coping strategies (e.g., increased use of alcohol), and have more negative attributions/perceptions of their child [8]. These parent-level challenges can be addressed, in part, by supporting parents to utilize more proactive and effective parenting practices which can help improve functioning for themselves and ultimately their children. Importantly, the most common comorbidities with ADHD, Oppositional Defiant Disorder [ODD] and Conduct Disorder (CD) are best treated with BPT—making BPT an essential treatment for the most common disruptive behavior disorders in childhood [8].
BPT is based on operant-conditioning and social learning theories, with techniques that focus on antecedents (e.g., effective instructions, rules) and consequences (e.g., active ignoring, time-out from positive reinforcement) of behaviors. This core content is delivered in a flexible manner with varying formats (e.g., group, individual) durations (brief vs longer), with or without child involvement, delivery (e.g., with or without video-based learning). Moreover, over the past two decades, there have been efforts at tailoring BPT to meet the needs of specific populations (e.g., single mothers, fathers; Latine; [9,10,11,12]). These BPT programs, often referred to as “homegrown” BPT as compared to commercialized BPT programs (those that have been more extensively developed, manualized and are commercially available; e.g., Defiant Children [13]) retain the core content of traditional BPT but have modifications to format or additional content that are based on the needs of the targeted populations. Overall, commercialized BPT and homegrown BPT have been found to be effective in improving the functioning of children with ADHD and their parents [14,15,16]. A recent meta-analysis also suggests sustained benefits of BPT over the course of a year on child ADHD symptoms, parenting behavior, parenting sense of competence and parental mental health [17]. The significance of BPT should be, however, put into a broader context to appreciate the clinical benefits of this intervention. While multiple randomized controlled trials have established the statistical significance of BPT for ADHD, the effect size for BPT ranges from small to medium effects, depending upon the outcome [18]. This means that for many outcomes, the effect sizes would be “visible to the naked eye of a careful observer” [19]. While there is limited data, only a significant minority of children are “normalized” following BPT [15]. Collectively, a more nuanced perspective on BPT for ADHD suggests that it is an evidence-based intervention that can result in visible improvements on key outcomes. There is room, however, to improve the potency of BPT. The implications of the findings reported above suggest several broad areas for further investigation. First is to increase access to BPT given the benefits of the intervention. Wolraich et al. [20] note that there is a lack of an adequate pool of behavioral and mental health specialists who are available to provide evidence-based psychosocial treatments for ADHD, including BPT. National data suggest that the majority of youth with ADHD are receiving no treatment, even when identified, and the lack of BPT treatment is most pronounced in young children with ADHD [21]. Efforts at utilizing technology to increase the workforce offers novel and promising approaches to address this issue [22].
A second area is to increase the potency of BPT. We believe there are multiple ways to achieve this goal, with the most apparent being improving the extent to which parents fully engage in BPT, given the relation between increased engagement and improved potency of outcomes [23]. It is common for families of children with ADHD, even those who have enrolled in BPT, to not initiate treatment or drop out of BPT prior to completion [9, 23]. Given this, there have been notable efforts at improving engagement to BPT through addressing perceptual (e.g., expectations about BPT), practical (e.g., transportation) and cultural barriers to treatment prior to BPT [10, 24] as well as during BPT [25]. Given that engagement challenges often involve practical barriers (e.g., transportation, child care, fixed appointment times), there has been efforts at increasing access through reducing these barriers such as providing BPT through mobile applications [26], web-based platforms [27] and telehealth delivery [28, 29]. These efforts have led to improved engagement and associated outcomes for families, beyond traditional BPT [30]. Engagement with BPT remains an important area of research, particularly the extent to which these enhancements to BPT can be readily applied in routine settings [25, 31, 32], an understudied empirical question.
A second and meaningful line of research to improve the potency of BPT has been focused on improving specificity of BPT content by translating contemporary theories of ADHD into refinements to BPT. Van der Oord and Tripp [33]), utilizing contemporary motivational reinforcement-based theories of ADHD, suggest that given altered reinforcement sensitivity in ADHD, rewards and punishment should be judiciously provided. As an example, they note evidence that while mild negative punishment (e.g., response-cost, time-out from positive reinforcement) improves on-task behavior in children with ADHD, mild punishment can also lead to more errors on tasks, increased emotionality in children with ADHD, missed learning opportunities, and lack of task persistence [34, 35]. These authors note caution in the use of punishment, especially positive punishment (e.g., verbal reprimands), with children with ADHD. Rather, there should be a focus on rewarding alternative adaptive behaviors to reduce the need to use punishment. These theory-driven considerations to adapting BPT are important, yet empirically understudied. As such, the extent to which these ADHD-theory-adapted BPT results in improved outcomes relative to standard BPT is not known. Importantly, however, some efforts in this area have resulted in little difference for ADHD-adapted BPT relative to standard BPT. As an example, in an RCT, the New Forest Parenting Program (NFPP), which was developed to address underlying mechanisms of ADHD (self-regulatory and cognitive problems [36] was found to be no better than a standard BPT program and in some areas less effective (e.g., parental stress, parenting behavior, parent reports of ADHD symptoms at follow-up) for preschool children with ADHD [37]. These data suggest the importance of rigorously evaluating novel approaches that are considered improvements to BPT to well-established traditional BPT for ADHD.
Overall, the efficacy of BPT suggests that this should be first-line intervention approach for children with ADHD, with significant and noticeable effects of BPT on both parent- and child-level outcomes with maintenance of gains over the course of a year. This statement comes with the caveat that there is room for improvement in the potency of BPT. As we will discuss in the future directions section below, greater attention must be given to dissemination of BPT (and all psychosocial interventions for ADHD) within routine systems of care and evaluation of the effectiveness of these interventions alone and in combination when delivered within these systems.
Behavioral classroom management
ADHD is largely defined by challenges in settings such as schools where behavioral expectations are often demanding of attention capacity and self-control, and so it is not surprising that many of the efficacious treatments for ADHD have focused on improving academic functioning and classroom behaviors. Children with ADHD are effectively treated with classroom contingency management strategies [38]. Systematic reviews [1, 2, 4, 5, 39] as well as meta-analyses [40,41,42] clearly illustrate that behavioral classroom management is an efficacious treatment for ADHD.
As noted above, behavioral classroom management is an efficacious treatment for ADHD. Before discussing evidence for efficacy and effectiveness of behavior classroom management, it is worth noting approaches that do not strongly support positive outcomes. In the United States, children with ADHD are eligible for behavioral classroom management support through Section 504 Accommodation plans administered through the Americans with Disabilities Act or through an Individualized Education Program if the committee on special education determines it is needed. These policies have provided school-based behavioral supports for students with ADHD for over 30 years. However, given that follow-up studies indicate that the long-term educational outcomes for students with ADHD are modest, at best [43,44,45,46], it is important to emphasize that these accommodation plans or individualized education programs are only useful if they include effective interventions and supports for the child or adolescent with ADHD.
Practically speaking, behavioral classroom management approaches that are effective will include setting clear goals and rules, ensure that the child receives clear feedback on progress toward meeting goals, and that consequences, typically rewards and privileges contingent on meeting behavioral goals and following rules, are provided liberally. It is important to note that positive behavior support strategies are interwoven into the fabric of elementary school classrooms - teachers provide rules and structure for activities, there is praise issued for appropriate behavior, and schools have standard discipline procedures including office referrals or detentions for rule violations. Feedback is provided on a regular, if infrequent basis (i.e., on quarterly report cards). For most children with ADHD this provides a reasonable baseline of behavioral classroom management, but additional strategies and supports are typically needed to make the overall approach to supporting a child with ADHD more efficacious.
Children with ADHD typically need much more frequent behavioral feedback and positive consequences for appropriate behavior in schools. For that reason, a daily report card is among the most efficacious positive behavior supports within a classroom [47, 48]. The daily report card has long been used effectively to treat ADHD, monitor outcomes, and open a daily line of communication between teachers and the child’s parent [49,50,51,52,53,54,55,56,57], and it is a procedure aligned with a long tradition of using contingency management with children with disruptive behavior in general educational settings [58] and in special education settings [57, 59, 60]. In addition to being among the most efficacious classroom interventions, it is also one of the most cost effective [61].
Recent changes in the ways schools address social, emotional, and behavioral challenges may promote greater effectiveness of the implementation of classroom behavior management strategies. Multi-tiered systems of support (MTSS [62] in schools conceptualize the behavior of children as being within a continuum, and through regular screening and progress monitoring, provide more intensive intervention, when indicated and for as long as is needed. Currently MTSS efforts in schools are focused on academic achievement targets, and there is less emphasis on MTSS for behavior [63]. However, the MTSS model of screening and intervention is similar to the single case design approach to intervention that has been long-used within the ADHD treatment literature [4, 5, 47]. In this approach, following the collection of baseline data, behavior classroom management interventions are systematically introduced to evaluate their effectiveness. Educators also benefit from ongoing coaching, support, and monitoring of progress to promote consistent and protracted use of these behavioral interventions [64].
Supporting this approach to school-based intervention is a recent study that evaluated the effectiveness of different sequences of ADHD treatment [65]. In this study, using a sequential, multiple assignment randomized trial (SMART [66]), children were randomly assigned to begin the school year with one of the two evidence-based treatments for ADHD - a low dose of stimulant medication or an initial course of behavior therapy (eight parent training sessions and a daily report card intervention at school). Teachers provided feedback on how the child was functioning in the classroom, and if there was evidence of impaired functioning, the child was then randomly assigned to more treatment – either a greater dose of the treatment at the start of the school year, or a other modality. Thus, children could have a treatment sequence of: (1) medication followed by an increased dose of medication; (2) medication with behavior therapy added; (3) behavior therapy followed by an increased dose of behavior therapy; or (4) behavior therapy followed by medication. Results were interesting as they illustrated the best sequence of treatment for reducing discipline referrals and disruptive behaviors observed in the classroom were those that started with behavior therapy first. Further, the behavior therapy first approaches also cost less to implement across the school year than the treatment sequences that included medication [61]. Importantly, this study of the effectiveness of treatment sequencing spanned an entire school year, improving upon the research base of efficacy treatments where many studies focused on shorter time periods. While the Pelham study provides a foundation for considering combined and sequenced approaches, far less has been done on the effectiveness of behavioral classroom approaches when conducted within and supported entirely by school-staff over the course of multiple school years.
Overall, there is strong support for behavioral classroom interventions, including the Daily Report Card [48, 50, 67], and it is strongly recommended that this intervention be initiated for children with ADHD experiencing classroom-based impairment. For older children (e.g., middle school, high school), a behavioral contract may be used to initiated contingency management across the multiple classrooms characteristic of this grade level. Educators and parents should ensure that school-based interventions are implemented consistency and continuously, as school-based behavioral challenges are likely to extend across school years and grade levels.
Organization skills training
Related to their difficulties staying on task and following the rules in the classroom setting, children with ADHD have impaired organization, time management, and planning skills that undermine their academic abilities and potential. Homework management and organizational skills have been shown to predict concurrent GPA and later academic outcomes [68, 69]. Organizational skills training (OST) interventions utilize behavioral methods to teach skills directly to students with ADHD. The training programs often include behavioral management procedures administered by a counselor, parent, or teacher to reinforce skill use and progress in treatment. Organizational interventions have largely targeted middle school to early high school students with ADHD (ages 10–14 [70]), with sessions focusing on materials organization, understanding time and time management, and planning larger assignments. Session frequency and length vary widely from about 10, 60-minute family sessions in a clinic [71] to 40, 2.5-hour student sessions in an after-school setting [72]. Multicomponent OST packages lead to improvements in organizational skills, planner use, and adolescent impairment [73].
Embedding OST in schools is key to enhancing the reach of these interventions. Though availability of school personnel to implement OST varies across districts, current work aims to train school counselors to implement OST with students with ADHD [74]. Langberg and colleagues [74] found that OST delivered by school staff led to improvements in organization, time management, and planning skills as performance and behavior during homework based on parent-report. Importantly, these results were found despite the school counselors receiving only 2 h of training in the intervention with no ongoing supervision. Purposefully limiting training and post-training investment allows for the examination of treatment effects in the context in which they would likely be provided—i.e., in schools, by school mental health providers with little funding for training and ongoing supervision. Toward the same goal of increasing the sustainability of OST within schools, investigators are developing online tools to assist school staff with OST implementation at low to no cost [75].
Psychosocial treatments for children with ADHD have primarily been researched in elementary-age youth, and early work in developing organizational skills interventions addressed this gap by upwardly extending treatments to middle school age youth. As the evidence accumulated that such interventions were efficacious among children with ADHD in middle school [1, 2], further developmental extension was clearly justified [76]. adapted their OST program developed for middle schoolers to pilot with high school students with ADHD. Pilot data demonstrated feasibility and indicated that high schoolers may need about 50 sessions to benefit from the OST program. In the full-scale randomized clinical trial [77], high schoolers attended an average of 40 brief OST sessions while their caregivers attended an average of 4 behavioral parent training sessions. Compared to the control group, beneficial effects of treatment were found on parent-reported academic functioning and organizational skills, and no significant effects on grades, teacher-reported, or self-reported outcomes were found. Results are promising, and much more work is needed to support the academic functioning of older adolescents with ADHD.
Digital therapeutics
Of all the available non-medication treatments, this category is the only one that features protocols patented by the US Patent and Trademark Office (USPTO) and cleared by the U.S. Food and Drug Administration (FDA) for the treatment of ADHD. It is also the most controversial, with competing consensus statements concluding that these types of interventions have proven effective vs. proven ineffective [78], millions of dollars in fines for false advertising [78], and a perceived disconnect between benchmarks for effectiveness between the FDA and professional organizations that evaluate psychosocial treatments for children [79]. Overall, there appears to be evidence for small benefits of cognitive training on reducing inattentive symptoms, and potentially overall ADHD symptoms [80]. However, we contend that omnibus meta-analytic effect sizes are fundamentally uninterpretable in the context of cognitive training/digital therapeutics because the treatments that fall under this general umbrella feature wide variations in neurocognitive/neurological training targets, conceptual models of neurocognition that define these intended training targets, success/failure to meaningfully engage and improve the intended training target(s), and technologies employed to ‘hit’ the intended target(s). Therefore, what these treatments share are more peripheral features, rather than core mechanistic features necessary to meet meta-analytic assumptions. Even interventions given the same, more specific label (e.g., “working memory training”) vary widely in their approach, conceptual basis, and success/failure at engaging their mechanistic target as shown previously [81]. It will be important for the field to evaluate each intervention on its own merits because these protocols generally share very little with each other except for the use of a serious games approach [82] to engaging children in treatment.
Several neurocognitive training protocols have been developed and tested for children with ADHD; we briefly review three of the most prominent: EndeavorRX, CogMed, and Central Executive Training (Cenextra; an intervention developed by one of the co-authors). All three of these approaches are computerized digital therapeutics that include gaming elements and adaptive changes in difficulty. EndeavorRX trains cognitive attention abilities [83], Cenextra trains the ‘working’ components of working memory [84] and CogMed is intended to improve attention and working memory abilities [85], though clinical trial and meta-analytic evidence indicates that CogMed successfully engages short-term memory but not working memory abilities [81, 86, 87].
In terms of efficacy, EndeavorRX showed early promise in pilot/uncontrolled studies given generally favorable feasibility, acceptability, and engagement data [83]. In addition, EndeavorRX showed potential for reductions in parent-reported ADHD symptoms in proof-of-concept and open-label trials with children with ADHD [88, 89]. However, the only controlled trial to date [83] demonstrated that these potential reductions were likely attributable to placebo effects – that is, Endeavor RX failed to show superior improvements in ADHD behavioral symptoms relative to a control condition (a spelling game). Evans et al. [79] concluded that “there is no evidence that using this game will result in any benefit in terms of their functioning and presenting problems.” (p. 125).
Cenextra also showed early promise in a head-to-head comparison with behavioral parent training (BPT) indicating favorable feasibility, acceptability, and engagement data. Cenextra was superior to BPT for improving working memory (d = 1.06) and reducing objectively-assessed hyperactivity (d = 0.74), and equivalent to BPT for reducing parent-reported ADHD symptoms at post-treatment [90]. These benefits were largely confirmed in an RCT comparing Cenextra with an active, credible digital therapeutic control called Inhibitory Control Training (ICT; [84]). Evidence suggesting improved functional outcomes is also emerging, and includes superior improvements relative to both BPT and ICT on masked teacher perceptions of organizational skills, academic success, impulse control, and academic productivity 1–2 months after treatment ended [91, 92].
Similar to EndeavorRX and Cenextra, Cogmed showed considerable promise in early trials, and is arguably the most extensively studied neurocognitive training program. Results from meta-analytic reviews and RCTs, however, suggest that CogMed does not improve working memory, but rather improves select components of short-term memory (meta-analytic d = 0.63; [81, 86, 93, 94]. This is an important limitation for at least two reasons: First, most children with ADHD do not have deficits in short term memory (20–38% impairment rates) despite the majority having impairments in working memory (75–81%; [95,96,97]). Second, short-term memory abilities are not significantly associated with ADHD symptoms in most studies [81, 95], which suggests limited potential for downstream improvements in ADHD behavioral symptoms. Indeed, conclusions from multiple meta-analytic reviews suggest that benefits on ADHD behavioral symptoms from CogMed are generally limited to unblinded parent ratings [81, 93]. Notably, however, a more recent meta-analysis published by the developer of CogMed suggests significant, small benefits for reducing inattention (d = 0.37; [98]), though the extent to which this was driven by unblinded parent ratings was unclear.
A key benefit of digital therapeutics – and ‘software as medicine’ in general – is that they have the potential to continually adapt and improve based on real-time patient data. Thus, it is possible that interventions that are not showing the behavioral/functional benefits we had hoped for now could begin to do so in the future. Thus, we highlight some key areas for improvement based on conceptual models and the limited available literature on moderators of cognitive training efficacy for children with ADHD. First, there is a need to maximize dosage. In the context of digital therapeutics, ‘dosage’ refers to the quantity and quality of time spent actively engaging with the training exercises. Most existing protocols have been studied over a relatively limited time frame of 4–10 weeks of training, with a total training time of about 10–12 h across intervention protocols [83, 84, 99]. It is possible that this level of training is insufficient for producing large enough neurocognitive improvements to translate into meaningful – and statistically detectable – gains in downstream behavioral/functional outcomes, suggesting the need for more intensive/longer duration training.
An option closely related to maximizing dosage is increasing the specificity of the neurocognitive training target(s). Although training a variety of neurocognitive functions is appealing at face value, meta-analytic evidence indicates that such protocols produce smaller near-transfer effects than protocols that focus on a single neurocognitive training target [81]. It is presumed that the reason for this finding is that the more different cognitive ‘muscles’ that we are trying to train, the less time we can spend on any one of those ‘muscles’. Thus, it appears likely that maximizing efficacy will require separate protocols for each neurocognitive function that is impaired in ADHD, combined with a ‘personalized medicine’ approach in which each child’s neurocognitive profile is estimated at pre-treatment, and then a treatment plan is developed to target each of their identified weaknesses. We must leverage basic science to link training targets with behavioral/functional outcomes. Related to dosage and specificity issues is the idea of matching neurocognitive training targets with the specific outcome(s) of interest. Stated bluntly, neurocognitive training is not likely to be helpful if we are training neurocognitive abilities that are not robustly linked with the reason(s) a child presents for treatment. On the other hand, neurocognitive training protocols have great potential if they are able to produce robust improvements in their training target, and if that training target is robustly associated with the observable behaviors/functional outcomes we are trying to improve. A final area that shows promise for improving the efficacy of digital therapeutic interventions is augmentation: Combining them with existing treatments to (potentially) produce synergistic and/or augmentative benefits. This area of inquiry is in its infancy, and currently shows more conceptual promise than actual benefits [100].
Future directions in improving efficacy and effectiveness
This brief review of psychosocial treatments for ADHD illustrates the robust evidence in support of these interventions. Importantly, there is no panacea or magic bullet for ADHD; the interventions reviewed herein have notable limitations and response to interventions vary. As such, there continues to be efforts at refining existing approaches and developing novel approaches to treating the complex presentation of ADHD. We highlight here what we believe are key future directions, broadly speaking, in improving the effectiveness and efficacy of treatment for ADHD. These fall under two broad areas: future directions in treatments and future directions in service delivery of these treatments.
Future directions in treatment for ADHD
Moderators of treatment effects
Much of the intervention literature has focused on static factors or social addresses (terms that describe rather than explain; e.g., marital status, child age;) as factors, largely because these are measures of convenience. Efforts toward using dynamic factors have shed light on what works for whom and can further refine an intervention to increase potency. As an example, in BPT, parent-level variables (e.g., parenting stress [101]) have been shown to moderate BPT engagement and outcomes, suggesting that future refinements to BPT that more directly address parental stress may increase the potency of BPT. Such efforts should be employed across all psychosocial interventions for ADHD. Importantly, as we have discussed elsewhere [8, 102], efforts should go beyond variable-centered approaches (e.g., child age, parent stress) toward holistic, person- and/or family-centered approaches (the clustering of variables that more fully represent a child/parent/family). As an example, Dale et al. [103] employed a person-centered approach to create subgroups of families based on the intersection of multiple parent, child, and family factors to understand response to BPT for families of preschool children with ADHD. Three distinct family profiles emerged, with data suggesting differential response for families with high stress, elevated parental anxiety, and elevated parental depression. These typological approaches better reflect reality- people are more accurately reflected as a complex intersection of variables rather than just any one variable- and taking this approach may better result in a nuanced understanding of response to treatment and further inform treatment for types of people and families.
ADHD is complex and presentations vary. It is not uncommon for children and adolescents with ADHD to also have significant difficulties outside of core symptoms of ADHD (e.g., emotion dysregulation, sleep disturbances) that may moderate treatment response. As an example, ADHD is frequently associated with emotional regulation challenges, with studies suggesting that the vast majority of children with ADHD (i.e., 75%) have some symptoms of emotion dysregulation, with 25% having severe emotion dysregulation [104]. In fact, children with ADHD and severe emotion dysregulation are more likely to have complex presentations, cross-situational impairments and severe psychopathology [105]. Interestingly, there are few rigorous randomized controlled trials evaluating the effects of psychosocial interventions for emotion dysregulation in children with ADHD [106]. These and other moderators may best be evaluated through novel approaches such as individual participant data meta-analysis [107]. Addressing the needs of youth with ADHD and their families will require going beyond addressing core symptoms of ADHD. In fact, we have long argued that these types of functional impairments (e.g., academic, social functioning) should be the targets for ADHD treatment rather than ADHD symptoms [8].
Novel intervention targets
The presentation of ADHD at key developmental periods/tasks may pose significant challenges for affected youth and their families- necessitating novel targets of intervention. An example of this is the transition to learning to drive. Adolescents are the riskiest drivers on the roadway, overall; if an adolescent has ADHD they are significantly more at risk for negative driving outcomes including accidents, accidents that cause injury, and fatalities [108, 109]. The period of time when individuals with ADHD are learning to drive may therefore be a critical, and also opportune time to initiate intervention. A recent RCT with adolescents with ADHD [110], evaluated a specially designed computerized simulated-driving program with feedback and found reduced problematic driving as compared with a control program. During real-world driving in the year after training, the rate of collisions and near-collisions was lower in the intervention group. These efforts highlight the potential of psychosocial interventions for addressing impairments inherent with developmental transitions for youth with ADHD. Related work suggests that intervening with adolescents at the transition to middle school and high school with intensive summer “bridge” programs may be a useful approach with high levels of engagement [111]. Future work should focus on embedding treatment efforts into other developmental tasks/transitions/tasks (e.g., start of preschool or initiation of employment).
Future directions in service delivery
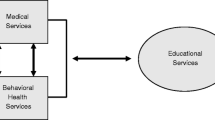
ADHD is now very clearly understood to persist throughout development and into adulthood and there has rightfully been a shift toward a chronic care model [7]. Given this, attention must be given to developing integrated, consistently available and longitudinal approaches embedded in routine service systems such that children, adolescents (and even adults) with ADHD and their families can receive appropriate care. Unfortunately, availability and access to evidence-based interventions are limited. Recent studies suggest that only 31% of families of children with ADHD receive BPT [21] and just 32% receive behavioral classroom management [112]. Given this, we highlight herein issues related to increasing availability and access to evidence-based psychosocial treatment for ADHD- important goals to help close the science-to-service-gap in ADHD. More specifically, we briefly highlight efforts on (1) leveraging the existing workforce, and (2) using technology to deliver evidence-based psychosocial treatments.
Leveraging existing workforces
In light of mental health workforce shortages (https://data.hrsa.gov/topics/health-workforce/workforce-projections) new models of care will need to utilize and expand existing, but underdeveloped, non-professional and paraprofessional workforces [31, 32]. One example of a sustainable, scalable model of care is the Family Peer Advocate (FPA) ADHD Model [25]. FPAs are part of a national family support model of current and former parent/caregivers of children with identified mental health needs who provide a range of services, including parenting skills training, emotional support, education about mental health services, and direct advocacy [30]. FPA-services are flexibly delivered in a variety of parent-identified settings (e.g., parent’s homes, community settings) and often connect and engage parents with key service settings/providers (e.g., schools, primary care, mental health clinics), reducing the systemic barriers associated with traditional service delivery models. Moreover, FPAs have many shared experiences with the families they serve including personal experience with providing care and navigating the service system for children with mental health challenges, often within the same community as those they serve. As a result, FPA care is associated with high acceptability ratings and increased engagement [113]. This FPA Model appears to be especially effective in reaching ethnically diverse families from socioeconomically disadvantaged backgrounds [30, 113]. Emerging data suggest that FPAs can reliably and effectively deliver BPT for youth with ADHD [25], suggesting that this and other workforce (e.g., ADHD Coaches) should be leveraged in order to increase availability and access to evidence-based psychosocial interventions for ADHD.
The idea of leveraging the existing workforce also applies to school settings. The MTSS intervention framework, which embeds intervention in schools into universal, targeted, and indicated approaches is an example of a potential means of re-allocating professional time and expertise. Rather than waiting for school psychologists and special educators to get involved only when the child is considered for special education, a MTSS approach might utilize the expertise of these professionals to consult with the general education teacher on how to implement positive behavior supports for a child with ADHD. In this way, intervention is implemented quicker, in the setting where the initial impairment is identified, by existing school professionals [56, 114].
Use of technology
Technology-based approaches to delivering evidence-based interventions have the potential to revolutionize mental health service access and delivery across multiple mental health disorders [115]. Online self-directed BPT approaches are potentially more feasible, affordable, and acceptable, can have significant reach to include traditionally underserved populations, and are readily scalable and sustainable [116, 117]. Over 13 studies have recently been conducted demonstrating that online BPT can improve child behavioral outcomes. Importantly, a recently published trial compared Triple P Online (TPO; an evidence-based, commercially available, self-directed online BPT) to a face-to-face (F2F) therapist-delivered Triple P for preschool children with disruptive behavior problems [118]. This large randomized controlled trial found that TPO was non-inferior to F2F Triple P on observed and parent-reported child behavior, with clinically meaningful effect sizes. This study, combined with several other studies [27, 119, 120] demonstrate the effectiveness of online BPT in general and specifically for ADHD. Technology is increasingly being utilized in practice settings (e.g., ADHD Care Assistant in primary care [121]; Online Daily Report Card in schools [122]) to increase access to evidence-based psychosocial interventions. Concerted efforts and rigorous empirical investigation will be necessary to further determine the effectiveness of these approaches. Importantly, while there is high potential for such technology-delivered approaches, engagement to these formats will remain important to address [123].
Conclusions
ADHD is a prevalent, pervasive, chronic and impairing disorder that necessitates early, integrated, continuous interventions over a child’s development. Fortunately, several psychosocial interventions are available that address key functional impairments in children and adolescents with ADHD. Given the complex presentation of ADHD, novel approaches to address both underlying pathophysiological mechanisms associated with ADHD (e.g., working memory) as well as domains closely impacted in those with ADHD (e.g., emotion regulation) and key developmental tasks (e.g., driving) are emerging areas in ADHD intervention science. Efforts to improve the efficacy of psychosocial interventions remain important as the acute benefits of these interventions do not result in normalized functioning for many youth and there remains an under-appreciation for whom these interventions are most impactful. Likely most pressing is the translation of the intervention science to improve outcomes for the millions of youth affected by ADHD, the science-to-service gap is prominent; many children who can benefit from evidence-based psychosocial interventions do not receive them. Improving access and availability of evidence-based psychosocial interventions remains critical to ensure that the significant efforts made over decades in developing and evaluating interventions for ADHD result in population-level benefits for youth with ADHD.
References
Evans SW, Owens JS, Bunford N. Evidence-based psychosocial treatments for children and adolescents with attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2014;43:527–51.
Evans SW, Owens JS, Wymbs BT, Ray AR. Evidence-based psychosocial treatments for children and adolescents with attention deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2018;47:157–98.
Pelham WE Jr, Fabiano GA. Evidence-based psychosocial treatments for attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2008;37:184–214.
Pelham WE Jr, Wheeler T, Chronis A. Empirically supported psychosocial treatments for attention deficit hyperactivity disorder. J Clin Child Adolesc Psychol. 1998;27:190–205.
Barbaresi WJ, Campbell L, Diekroger EA, Froehlich TE, Liu YH, O’Malley, et al. Society for Developmental and Behavioral Pediatrics clinical practice guideline for the assessment and treatment of children and adolescents with complex attention-deficit/hyperactivity disorder. J Dev Behav Pediatr. 2020;41:S35–S57.
American Academy of Child and Adolescent Psychiatry. Practice parameters for assessment and treatment of children and adolescents with Attention-Deficit/Hyperactivity Disorder. J Am Acad Child Adolesc Psychiatry. 2007;46:894–921.
DuPaul GJ, Evans SW, Mautone JA, Owens JS, Power TJ. Future directions for psychosocial interventions for children and adolescents with ADHD. J Clin Child Adolesc Psychol. 2020;49:134–45.
Chacko A, Alan C, Uderman J, Cornwell M, Anderson L, Chimiklis A. Ch 10. In: Barkley R, editor. Attention deficit hyperactivity disorder: a handbook for diagnosis and treatment, 4th edn. New York: Guilford Press; 2015.
Chacko A, Wymbs BT, Arnold FW, Pelham WE, Swanger-Gagne M, Girio EL, et al. Enhancing traditional behavioral parent training for single-mothers of children with ADHD. J Clin Child Adolesc Psychol. 2009;38:206–18.
Chacko A, Wymbs BT, Chimiklis A, Wymbs FA, Pelham WE. Evaluating a comprehensive strategy to improve engagement to group-based behavioral parent training for high-risk families of children with ADHD. J Abnorm Child Psychol. 2012;40:1351–62.
Gerdes AC, Kapke TL, Grace M, Castro A. Feasibility, acceptability, and preliminary outcomes of a culturally-adapted evidence-based treatment for Latino youth with ADHD. J Atten Disord. 2021;25:432–47.
Fabiano GA, Pelham WE, Cunningham CE, Yu J, Gangloff B, Buck M, et al. A waitlist-controlled trial of behavioral parent training for fathers of children with ADHD. J Clin Child Adolesc Psychol. 2012;41:337–45.
Barkley RA, Benton CM. Your defiant child: eight steps to better behavior. Chicago: Guilford Press; 2013.
Leijten P, Melendez-Torres GJ, Knerr W, Gardner F. Transported versus homegrown parenting interventions for reducing disruptive child behavior: a multilevel meta-regression study. J Am Acad Child Adolesc Psychiatry. 2016;55:610–7.
Rajwan E, Chacko A, Wymbs BT, Wymbs FA. Evaluating clinically significant change in parent and child functioning: Comparison of traditional and enhanced behavioral parent training. J Abnor Chil Psychol. 2014;42:1407–12.
Marquet-Doléac J, Biotteau M, Chaix Y. Behavioral parent training for school-aged children with ADHD: a systematic review of randomized control trials. J Atten Disord. 2023;28:377–93.
Doffer DPA, Dekkers T, Hornstra R, van der Oord S, Luman M, Leijten P, et al. Sustained improvements by behavioural parent training for children with attention-deficit/hyperactivity disorder: a meta-analysis into longer-term child and parental outcomes. JCCP Adv. 2023;3:e12196.
Fabiano GA, Schatz NK, Aloe AM, Pelham WE Jr, Smyth AC, Zhao X, et al. Comprehensive meta-analysis of attention-deficit/hyperactivity disorder psychosocial treatments investigated within between group studies. Rev Educ Res. 2021;91:718–60.
Cohen J. Things I have learned (so far). In: Annual Convention of the American Psychological Association, 98th, 1990, Boston, MA, USA; Presented at the aforementioned conference. American Psychological Association; 1992.
Wolraich ML, Hagan JF, Allan C, Chan E, Davison D, Earls M, et al. Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. Pediatrics. 2019;144:e20192528.
Danielson ML, Visser SN, Chronis-Tuscano A, DuPaul GJ. A national description of treatment among U.S. children and adolescents with ADHD. J Pediatr. 2018;192:240–6.
Ortiz C, Vidair HB, Acri M, Chacko A, Kobak K. Pilot study of an online parent-training course for disruptive behavior with live remote coaching for practitioners. Prof Psychol Res Pract. 2020;51:125–33.
Chacko A, Jensen S, Lowry LS, Cornwell M, Chimiklis A, Chan E, et al. Engagement in behavioral parent training: review of the literature and implications for practice. Clin Child Fam Psychol Rev. 2016;19:204–15.
Sanchez AL, Jent J, Aggarwal NK, Chavira D, Coxe S, Garcia D, et al. Person-centered cultural assessment can improve child mental health service engagement and outcomes. J Clin Child Adolesc Psychol. 2022;51:1–22.
Chacko A, Hopkins K, Acri M, Mendelsohn A, Dreyer B. Expanding ADHD service provision in urban socioeconomically disadvantaged communities: a pilot study. Clin Pract Pediatr Psychol. 2020;8:189–94.
Chacko A, Isham A, Cleek A, Mckay M. Using mobile health technology to improve homework implementation in evidence-based parenting intervention for disruptive behavior disorders in youth. Pilot Feasibility Stud. 2016;2:1–11.
DuPaul GJ, Kern L, Belk G, Custer B, Daffner M, Hatfield A, et al. Face-to-face versus online behavioral parent training for young children at risk for ADHD: treatment engagement and outcomes. J Clin Child Adolesc Psychol. 2018;47:S369–S383.
Myers K, Vander Stoep A, Zhou C, McCarty CA, Katon W. Effectiveness of a telehealth service delivery model for treating attention-deficit/hyperactivity disorder: a community-based randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2015;54:263–74.
Xie Y, Dixon JF, Yee OM, Zhang J, Chen YA, DeAngelo S, et al. A study on the effectiveness of videoconferencing on teaching parent training skills to parents of children with ADHD. Telemed J E Health. 2013;19:192–9.
Acri M, Hooley CD, Richardson N, Moaba LB. Peer models in mental health for caregivers and families. Community Ment Health J. 2017;53:241–9.
Chacko A, Scavenius C. Bending the curve: Community based behavioral parent training to address ADHD symptoms in the voluntary sector in Denmark. J Abnorm Child Psychol. 2018;46:505–17.
Chacko A, Gopalan G, Franco L, Dean-Assael K, Jackson J, Marcus S, et al. Multiple-Family Group service delivery model for the children with disruptive behavior disorders. J Emot Behav Disord. 2015;23:67–77.
Van der Oord S, Tripp G. How to improve behavioral parent and teacher training for children with ADHD: Integrating empirical research on learning and motivation into treatment. Clin Child Fam Psychol Rev. 2020;23:577–604.
Furukawa E, Alsop B, Sowerby P, Jensen S, Tripp G. Evidence for increased behavioral control by punishment in children with attention-deficit hyperactivity disorder. J Child Psychol Psychiatry. 2017;3:248–57.
Furukawa E, Alsop B, Shimabukuro S, Tripp G. Is increased sensitivity to punishment a common characteristic of attention deficit/hyperactivity disorder? An experimental study of response allocation in Japanese children. Atten Deficit Hyperact Disord. 2019;11:433–43.
Sonuga-Barke EJ, Thompson M, Abikoff H, Klein R, Brotman LM. Nonpharmacological interventions for preschoolers with ADHD: The case for specialized parent training. Infants Young Child. 2006;19:142–53.
Abikoff HB, Thompson M, Laver‐Bradbury C, Long N, Forehand RL, Miller Brotman L, et al. Parent training for preschool ADHD: a randomized controlled trial of specialized and generic programs. J Child Psychol Psychiatry. 2015;56:618–31.
DuPaul GJ. Attention deficit-hyperactivity disorder: classroom intervention strategies. Sch Psychol Int. 1991;12:85–94.
Harrison JR, Soares DA, Rudzinski S, Johnson R. Attention deficit hyperactivity disorders and classroom-based interventions: Evidence-based status, effectiveness, and moderators of effects in single-case design research. Rev Educ Res. 2019;89:569–611.
DuPaul GJ, Eckert TL. The effects of school-based interventions for attention deficit/hyperactivity disorder: a meta-analysis. Sch Psych Rev. 1997;26:5–27.
DuPaul GJ, Eckert TL, Vilardo B. The effects of school-based interventions for attention deficit hyperactivity disorder: A meta-analysis 1996–2010. Sch Psych Rev. 2012;41:387–412.
Fabiano GA, Pelham WE Jr, Coles EK, Gnagy EM, Chronis-Tuscano A, O’Connor BC. A meta-analysis of behavioral treatments for attention-deficit/hyperactivity disorder. Clin Psychol Rev. 2009;29:129–40.
Arnold LE, Hodgkins P, Kahle J, Madhoo M, Kewley G. Long-term outcomes of ADHD: academic achievement and performance. J Atten Disord. 2020;24:73–85.
Kent KM, Pelham WE, Molina BS, Sibley MH, Waschbusch DA, Yu J, et al. The academic experience of male high school students with ADHD. J Abnorm Child Psychol. 2011;39:451–62.
Kuriyan AB, Pelham WE, Molina BS, Waschbusch DA, Gnagy EM, Sibley MH, et al. Young adult educational and vocational outcomes of children diagnosed with ADHD. J Abnorm Child Psychol. 2013;41:27–41.
Molina BS, Hinshaw SP, Swanson JM, Arnold LE, Vitiello B, Jensen PS, et al. The MTA at 8 years: prospective follow-up of children treated for combined-type ADHD in a multisite study. J Am Acad Child Adolesc Psychiatry 2009. 2009;48:484–500.
Pyle K, Fabiano GA. A meta-analysis of single-subject design studies utilizing the daily report card intervention for students with ADHD. Excep Child. 2017;83:378–95.
Volpe R, Fabiano, GA. Daily behavior report cards: an evidence-based system of assessment and intervention. New York, NY: The Guilford Press; 2013.
Kelley ML. School-home notes: promoting children’s classroom success. New York: The Guilford Press; 1990.
O’Leary KD, Pelham WE, Rosenbaum A, Price GH. Behavioral treatment of hyperkinetic children: an experimental evaluation of its usefulness. Clin Pediatr. 1976;15:510–5.
Owens JS, Holdaway AS, Zoromski AK, Evans SW, Himawan LK, Girio-Herrera E, et al. Incremental benefits of a daily report card intervention over time for youth with disruptive behavior. Behav Ther. 2012;43:848–61.
Pelham WE, Fabiano GA, Massetti GM. Evidence-based assessment for attention-deficit/hyperactivity disorder in children and adolescents. J Clin Child Adolesc Psychol. 2005;34:449–76.
Pelham WE, Gnagy EM, Burrows-Maclean L, Williams A, Fabiano GA, Morrissey SM, et al. Once-a-day Concerta™ methylphenidate versus t.i.d. methylphenidate in laboratory and natural settings. Pediatrics. 2001;10:e105.
Pelham WE, Hoza B, Pillow DR, Gnagy EM, Kipp HL, Greiner AR, et al. Effects of methylphenidate and expectancy on children with ADHD: behavior, academic performance, and attributions in a summer treatment program and regular classrooms. J Consult Clin Psychol. 2002;70:320–35.
Pfiffner LJ, Mikami AY, Huang-Pollock C, Easterlin B, Zalecki C, McBurnett K. A randomized, controlled trial of integrated home-school treatment for ADHD, Primarily inattentive type. J Am Acad Child Adolesc Psychiatry. 2007;46:1040–51.
Pfiffner LJ, Villodas M, Kaiser N, Rooney M, McBurnett K. Educational outcomes of a collaborative school-home behavioral intervention for ADHD. Sch Psychol Q. 2013;28:25–36.
Vannest KJ, Davis JL, Davis CR, Mason BA, Burke MD. Effective intervention for behavior with a daily behavior report card: a meta-analysis. Sch Psych Rev. 2010;39:654–72.
Hops H, Walker HM. CLASS: contingencies for learning and academic and social skills. Seattle WA: Educational Achievement Systems; 1988.
Reid R, Maag JW, Vasa SF, Wright G. Who are the children with attention deficit-hyperactivity disorder? A school-based survey. J Spec Educ. 1994;28:117–37.
Schnoes C, Reid R, Wagner M, Marder C. ADHD among students receiving special education services: a national survey. Excep Child. 2006;72:483–96.
Page TF, Pelham WE III, Fabiano GA, Greiner AR, Gnagy EM, et al. Comparative cost analysis of sequential, adaptive, behavioral, pharmacological, and combined treatments for childhood ADHD. J Clin Child Adolesc Psychol. 2016;45:416–27.
Burns MK, Jimerson SR, VanDerHeyden AM, Deno, SL. Toward a unified response-to-intervention model: Multi-tiered systems of support. In: Handbook of response to intervention: The science and practice of multi-tiered systems of support. Boston, MA: Springer US; 2015. p. 719–32.
Briesch AM, Chafouleas SM, Nissen K, Long S. A review of state-level procedural guidance for implementing multitiered systems of support for behavior (MTSS-B). J Posit Behav Inter. 2020;23:131–44.
Owens JS, McLennan JD, Hustus CL, Haines-Saah R, Mitchell S, Mixon CS, et al. Leveraging technology to facilitate teachers’ use of a targeted classroom intervention: Evaluation of the Daily Report Card. Online (DRC. O) System. Sch Ment Health. 2019;11:665–77.
Pelham WE, Fabiano GA, Waxmonsky JG, Greiner AR, Gnagy EM, Pelham WE III, et al. Treatment sequencing for childhood ADHD: A multiple-randomization study of adaptive medication and behavioral interventions. J Clin Child Adolesc Psychol. 2016;45:396–415.
Lei H, Nahum-Shani I, Lynch K, Oslin D, Murphy SA. A “SMART” design for building individualized treatment sequences. Annu Rev Clin Psychol. 2012;8:21–48.
Owens JS, Hustus CL, Evans SW. The daily report card intervention: Summary of the science and factors affecting implementation. In: Handbook of research on emotional and behavioral disorders. Routledge; 2020. p. 371–85.
Langberg JM, Epstein JN, Girio-Herrera E, Becker SP, Vaughn AJ, Altaye M. Materials organization, planning, and homework completion in middle-school students with ADHD: impact on academic performance. Sch Ment Health. 2011;3:93–101.
Langberg JM, Molina BSG, Arnold LE, Epstein JN, Altaye M, Hinshaw SP, et al. Patterns and predictors of adolescent academic achievement and performance in a sample of children with attention-deficit/hyperactivity disorder. J Clin Child Adolesc Psychol. 2011;40:519–31.
Bikic A, Reichow B, McCauley SA, Ibrahim K, Sukhodolsky DG. Meta-analysis of organizational skills interventions for children and adolescents with Attention-Deficit/Hyperactivity Disorder. Clin Psychol Rev. 2017;52:108–23.
Sibley MH, Graziano PA, Kuriyan AB, Coxe S, Pelham WE, Rodriguez L, et al. Parent–teen behavior therapy+ motivational interviewing for adolescents with ADHD. J Consult Clin Psychol. 2016;84:699.
Evans SW, Schultz BK, DeMars CE, Davis H. Effectiveness of the challenging horizons after-school program for young adolescents with ADHD. Behav Ther. 2011;42:462–74.
Chan E, Fogler JM, Hammerness P. Treatment of attention-deficit/hyperactivity disorder in adolescents: a systematic review. JAMA. 2016;315:1997–2008.
Langberg JM, Dvorsky MR, Molitor SJ, Bourchtein E, Eddy LD, Smith ZR, et al. Overcoming the research-to-practice gap: a randomized trial with two brief homework and organization interventions for students with ADHD as implemented by school mental health providers. J Consult Clin Psychol. 2018;86:39.
Pfiffner LJ, Dvorsky MR, Friedman LM, Haack LM, Chung S, Charalel JM, et al. Development of a web-based training platform for school clinicians in evidence-based practices for ADHD. Sch Ment Health. 2023;15:49–66.
Evans SW, Schultz BK, DeMars CE. High school–based treatment for adolescents with attention-deficit/hyperactivity disorder: results from a pilot study examining outcomes and dosage. Sch Psych Rev. 2104;43:185–202.
DuPaul GJ, Evans SW, Owens JS, Cleminshaw CL, Kipperman K, Fu Q, et al. School-based intervention for adolescents with attention-deficit/hyperactivity disorder: effects on academic functioning. J Sch Psychol. 2021;87:48–63.
Simons DJ, Boot WR, Charness N, Gathercole SE, Chabris CF, Hambrick DZ, et al. Do “brain-training” programs work? Psychol Sci. 2016;17:103–86.
Evans SW, Beauchaine TP, Chronis-Tuscano A, Becker SP, Chacko A, Gallagher R, et al. The efficacy of cognitive videogame training for ADHD and What FDA clearance means for clinicians. Evid Based Pract Child Adolesc Ment Health. 2021;6:116–30.
Westwood SJ, Parlatini V, Rubia K, Cortese S, Sonuga-Barke EJ. Computerized cognitive training in attention-deficit/hyperactivity disorder (ADHD): a meta-analysis of randomized controlled trials with blinded and objective outcomes. Mol Psychiatry. 2023;28:1402–14.
Rapport MD, Orban SA, Kofler MJ, Friedman LM. Do programs designed to train working memory, other executive functions, and attention benefit children with ADHD? A meta-analytic review of cognitive, academic, and behavioral outcomes. Clin Psychol Rev. 2013;33:1237–52.
Cannon-Bowers J, Bowers C, editors. Serious game design and development: technologies for training and learning. New York: IGI Global; 2010.
Kollins SH, DeLoss DJ, Cañadas E, Lutz J, Findling RL, Keefe RS, et al. A novel digital intervention for actively reducing severity of paediatric ADHD (STARS-ADHD): a randomised controlled trial. Lancet Digit Health. 2020;2:e168–e178.
Kofler MJ, Wells EL, Singh LJ, Soto EF, Irwin LN, Groves NB, et al. A randomized controlled trial of central executive training (CET) versus inhibitory control training (ICT) for ADHD. J Consult Clin Psychol. 2020;88:738–56.
Klingberg T, Fernell E, Olesen PJ, Johnson M, Gustafsson P, Dahlström K, et al. Computerized training of working memory in children with ADHD-a randomized, controlled trial. J Am Acad Child Adolesc Psychiatry. 2005;44:177–86.
Roberts G, Quach J, Spencer-Smith M, Anderson PJ, Gathercole S, Gold L, et al. Academic outcomes 2 years after working memory training for children with low working memory: a randomized clinical trial. JAMA Pediatr. 2016;170:e154568.
Chacko A, Bedard AC, Marks DJ, Feirsen N, Uderman JZ, Chimiklis A, et al. A randomized clinical trial of Cogmed working memory training in school‐age children with ADHD: A replication in a diverse sample using a control condition. J Child Psychol Psychiatry. 2014;55:247–55.
Davis NO, Bower J, Kollins SH. Proof-of-concept study of an at-home, engaging, digital intervention for pediatric ADHD. PLoS ONE. 2018;13:e0189749.
Kollins SH, Childress A, Heusser AC, Lutz J. Effectiveness of a digital therapeutic as adjunct to treatment with medication in pediatric ADHD. NPJ Digit Med. 2021;4:1–8.
Kofler MJ, Sarver DE, Austin KE, Schaefer HS, Holland E, Aduen PA, et al. Can working memory training work for ADHD? Development of central executive training and comparison with behavioral parent training. J Consult Clin Psychol. 2018;86:964.
Singh LJ, Gaye F, Cole AM, Chan ES, Kofler MJ. Central executive training for ADHD: effects on academic achievement, productivity, and success in the classroom. Neuropsychol. 2022;36:330–45.
Chan ESM, Gaye F, Cole AM, Singh LJ, Kofler MJ. Central executive training for ADHD: impact on organizational skills at home and school. A randomized controlled trial. Neuropsychol.
Chacko A, Feirsen N, Bedard AC, Marks D, Uderman JZ, Chimiklis A. Cogmed working memory training for youth with ADHD: a closer examination of efficacy utilizing evidence-based criteria. J Clin Child Adolesc Psychol. 2013;42:769–83.
Sala G, Gobet F. Working memory training in typically developing children: a meta-analysis of the available evidence. Dev Psychol. 2017;53:671–85.
Kofler MJ, Singh LJ, Soto EF, Chan ESM, Miller CE, Harmon SL, et al. Working memory and short-term memory deficits in ADHD: A bifactor modeling approach. Neuropsychol. 2020;34:686–98.
Fosco WD, Kofler MJ, Groves NB, Chan ESB, Raiker JS. Which ‘working’ components of working memory aren’t working in youth with ADHD? J Abnorm Child Psychol. 2020;48:647–60.
Karalunas S, Gustafsson H, Dieckmann N, Tipsord J, Mitchell SH, Nigg J. Heterogeneity in development of aspects of working memory predicts longitudinal attention deficit hyperactivity disorder symptom change. J Abnorm Child Psychol. 2017;126:774–92.
Spencer-Smith M, Klingberg T. Correction: benefits of a working memory training program for inattention in daily life: a systematic review and meta-analysis. PLoS ONE. 2016;11:e0167373.
Klingberg T, Forssberg H, Westerberg H. Training of working memory in children with ADHD. J Clin Exp Neuropsychol. 2002;24:781–91.
Chacko A, Bedard AC, Marks D, Gopalan G, Feirsen N, Uderman J, et al. Sequenced neurocognitive and behavioral parent training for the treatment of ADHD in school-age children. Child Neuro. 2018;24:427–50.
Chacko A, Feirsen N, Rajwan E, Wymbs BT, Wymbs FA. Distinguishing never-attenders, dropouts, and completers to behavioral parent training: The importance of parental cognitions. J Child Fam Stud. 2017;26:950–60.
Vardanian MM, Ramakrishnan A, Peralta S, Siddiqui Y, Shah S, Clark-Whitney E, et al. Clinically significant and reliable change: comparing an evidence-based intervention to usual care. J Child Fam Stud. 2020;29:921–33.
Dale C, Parent J, Forehand R, DiMarzio K, Sonuga-Barke E, Long N, et al. Behavioral parent training for preschool ADHD: family-centered profiles predict changes in parenting and child outcomes. J Clin Child Adolesc Psychol. 2021;51:726–39.
Sobanski E, Banaschewski T, Asherson P, Buitelaar J, Chen W, Franke B, et al. Emotional lability in children and adolescents with attention deficit/hyperactivity disorder (ADHD): clinical correlates and familial prevalence. J Child Psychol Psychiatry. 2010;51:915–23.
Qian Y, Chang W, He X, Yang L, Liu L, Ma Q, et al. Emotional dysregulation of ADHD in childhood predicts poor early-adulthood outcomes: a prospective follow up study. Res Dev Disabil. 2016;59:428–36.
Vacher C, Goujon A, Romo L, Purper-Ouakil D. Efficacy of psychosocial interventions for children with ADHD and emotion dysregulation: a systematic review. Psychiatry Res. 2020;291:113–51.
Groenman AP, Hornstra R, Hoekstra PJ, Steenhuis L, Aghebati A, Boyer BE, et al. An individual participant data meta-analysis: behavioral treatments for children and adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2022;61:144–58.
Aduen PA, Cox DJ, Fabiano GA, Garner AA, Kofler MJ. Expert recommendations for improving driving safety for teens and adult drivers with ADHD. ADHD Rep. 2019;27:8.
Aduen PA, Kofler MJ, Sarver DE, Wells EL, Soto EF, Cox DJ. ADHD, depression, and motor vehicle crashes: A prospective cohort study of continuously-monitored, real-world driving. J Psychiatr Res. 2018;101:42–49.
Epstein JN, Garner AA, Kiefer AW, Peugh J, Tamm L, MacPherson RP, et al. Trial of training to reduce driver inattention in teens with ADHD. N Engl J Med. 2022;387:2056–66.
Sibley MH, Coxe SJ, Campez M, Morley C, Olson S, Hidalgo-Gato N, et al. High versus low intensity summer treatment for ADHD delivered at secondary school transitions. J Clin Child Adolesc Psychol. 2018;47:248–65.
DuPaul GJ, Chronis-Tuscano A, Danielson ML, Visser SN. Predictors of receipt of school services in a national sample of youth with attention-deficit/hyperactivity disorder. J Atten Disord. 2019;23:1303–19.
Hoagwood KE, Cavaleri MA, Serene Olin S, Burns BJ, Slaton E, et al. Family support in children’s mental health: A review and synthesis. Clin Child Fam Psychol Rev. 2010;13:1–45.
Fabiano GA, Pyle K. Best practices in school mental health for attention-deficit/hyperactivity disorder: A framework for intervention. Sch Ment Health. 2019;11:72–91.
Nieuwboer CC, Fukkink RG, Hermanns JM. Online programs as tools to improve parenting: a meta-analytic review. Child Youth Ser Rev. 2013;35:1823–9.
Tan-MacNeill KM, Smith IM, Johnson SA, Chorney J, Corkum P. A systematic review of online parent-implemented interventions for children with neurodevelopmental disorders. Child Health Care. 2021;50:239–77.
Thongseiratch T, Leijten P, Melendez-Torres GJ. Online parent programs for children’s behavioral problems: a meta-analytic review. Eur Child Adolesc Psychiatry. 2020;29:1555–68.
Prinz RJ, Metzler CW, Sanders MR, Rusby JC, Cai C. Online‐delivered parenting intervention for young children with disruptive behavior problems: a noninferiority trial focused on child and parent outcomes. J Child Psychol Psychiatry. 2022;63:199–209.
Baker S, Sanders MR, Turner KM, Morawska A. A randomized controlled trial evaluating a low-intensity interactive online parenting intervention, Triple P Online Brief, with parents of children with early onset conduct problems. Behav Res Ther. 2017;91:78–90.
Franke N, Keown LJ, Sanders MR. An RCT of an online parenting program for parents of preschool-aged children with ADHD symptoms. J Atten Disord. 2020;24:1716–26.
Power TJ, Michel J, Mayne S, Miller J, Blum NJ, Grundmeier RW, et al. Coordinating systems of care using health information technology: development of the ADHD care assistant. Adv Sch Ment Health Promot. 2016;9:201–18.
Mixon CS, Owens JS, Hustus C, Serrano VJ, Holdaway AS. Evaluating the impact of online professional development on teachers’ use of a targeted behavioral classroom intervention. Sch Ment Health. 2019;11:115–28.
Breider S, de Bildt A, Nauta MH, Hoekstra PJ, van den Hoofdakker BJ. Self-directed or therapist-led parent training for children with attention deficit hyperactivity disorder? A randomized controlled non-inferiority pilot trial. Internet Interv. 2019;18:100262.
Coghill D, Banaschewski T, Cortese S, Asherson P, Brandeis D, Buitelaar J, et al. The management of ADHD in children and adolescents: bringing evidence to the clinic: perspective from the European ADHD Guidelines Group (EAGG). Eur Child Adolesc Psychiatry. 2021;32:1337–61.
Author information
Authors and Affiliations
Contributions
AC, BM, MJK and GAF were involved in the development, writing, review, revisions and final approval of the manuscript.
Corresponding author
Ethics declarations
Competing interests
MJK holds a patent for neurocognitive interventions that target central executive working memory and inhibitory control and that were recently licensed to Sky Therapeutics, a company for which MJK provides consulting and holds equity.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chacko, A., Merrill, B.M., Kofler, M.J. et al. Improving the efficacy and effectiveness of evidence-based psychosocial interventions for attention-deficit/hyperactivity disorder (ADHD) in children and adolescents. Transl Psychiatry 14, 244 (2024). https://doi.org/10.1038/s41398-024-02890-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-024-02890-3
- Springer Nature Limited