Abstract
Introduction
In 2019 the World Health Organisation published a report which concluded microplastics in drinking water did not present a threat to human health. Since this time a plethora of research has emerged demonstrating the presence of plastic in various organ systems and their deleterious pathophysiological effects.
Methods
A scoping review was undertaken in line with recommendations from the Johanna Briggs Institute. Five databases (PubMed, SCOPUS, CINAHL, Web of Science and EMBASE) were systematically searched in addition to a further grey literature search.
Results
Eighteen articles were identified, six of which investigated and characterised the presence of microplastics and nanoplastics (MNPs) in the human urinary tract. Microplastics were found to be present in kidney, urine and bladder cancer samples. Twelve articles investigated the effect of MNPs on human cell lines associated with the human urinary tract. These articles suggest MNPs have a cytotoxic effect, increase inflammation, decrease cell viability and alter mitogen-activated protein kinases (MAPK) signalling pathways.
Conclusion
Given the reported presence MNPs in human tissues and organs, these plastics may have potential health implications in bladder disease and dysfunction. As a result, institutions such as the World Health Organisation need to urgently re-evaluate their position on the threat of microplastics to public health.
Impact statement
This scoping review highlights the rapidly emerging threat of microplastic contamination within the human urinary tract, challenging the World Health Organisation’s assertion that microplastics pose no risk to public health. The documented cytotoxic effects of microplastics, alongside their ability to induce inflammation, reduce cell viability and disrupt signalling pathways, raise significant public health concerns relating to bladder cancer, chronic kidney disease, chronic urinary tract infections and incontinence. As a result, this study emphasises the pressing need for further research and policy development to address the challenges surrounding microplastic contamination.

Similar content being viewed by others
Introduction
Since their widespread adoption in the mid-20th century, plastics have transformed from a novel substance into a versatile range of materials that pervade all aspects of society. The extensive integration of plastics into all industries and facets of society led to the production of 368 million tonnes of plastic in 2019, a figure expected to double by 2039 [1, 2]. The production and degradation of plastic, a process involving a combination of physical, chemical and biological processes, has resulted in the accumulation of miniscule fragments termed microplastics (MPs) or nanoplastics (NPs) [3], residing within all aspects of our environment including flora [4] and fauna [5,6,7], streams and oceans [8], air [9], and soil [10]. Beyond the well-documented environmental impacts of MPs and NPs, evidence for their presence within human organ systems and their role in driving various pathophysiological processes and diseases is rapidly emerging [11,12,13,14,15]. Of notable concern is their presence within the urinary tract and consequent impact on renal and bladder disease and dysfunction, as seen in animal studies [16, 17].
As the impact of plastic pollution becomes increasingly evident, so too does the need for internationally standardised definitions of MPs and NPs. Government publications reveal notable discrepancies in the definition of such fragmented plastics between organisations. For example, MPs are described by the European Union as “…small pieces of plastics, usually smaller than 5 millimetre (mm)”, and there is no formal definition provided for NPs [18]. The National Science Foundation describes MPs and NPs as fragments less than 5 mm and less than 100 nanometre (nm), respectively [19]. In contrast, the International Organisation for Standardisation (ISO) offers a more detailed classification, defining MPs as solid plastic particles insoluble in water, ranging from 1 micrometre (µm) to 1000 µm (1 mm), and NPs as particles smaller than 1 µm [20]. This variation and lack of consensus across different regulatory bodies exemplifies the challenges associated with mitigating the environmental and health-related impacts of microplastics and nanoplastics (MNPs).
Following their intrusion into the human body, whether through inhalation, ingestion, or through the skin (wound, hair follicle, sweat gland) [21,22,23], MNPs have been observed to cross biological barriers, leading to systemic exposure, and resulting in their detection in multiple critical organ systems [24]. To date, the presence of MNPs has been demonstrated to have deleterious pathophysiological implications resulting in inflammation, alterations in cellular metabolism, mechanically induced cellular damage and decreased cell viability [25,26,27].
Pathologies of the urinary tract, partially resulting from issues surrounding increasing antimicrobial resistance, rates of cancer and ageing populations, result in significant health-related economic expenditure, morbidity and mortality. Globally, an estimated 404.61 million urinary tract infections (UTIs) occurred in 2019 alone, resulting in over 236 000 deaths and 520 000 disability adjusted life years (DALYs) [28]. The cost of renal replacement, while only utilised by 0.15% of the population, represents 2–4% of total healthcare expenditure in some countries [29]. As a result, the detection of MNPs in the human urinary tract, in conjunction with a lack of understanding regarding their effects, currently provides reason for concern within the healthcare community. These concerns are potentially augmented by foreseeable difficulties in the removal of plastics from organs and the treatment of plastic-associated diseases.
Therefore, this scoping review aims to systematically explore and summarise the literature regarding the presence of MNPs in the human urinary tract and their pathological consequences, and explore the methodologies used in their detection and analysis, guided by the following research questions:
RQ1: What are the characteristics of plastics which have been found in the human urinary tract?
RQ2: How are MPs and NPs currently defined within the literature?
RQ3: What methodologies are currently utilised to explore the presence of MNPs and their effects?
RQ4: What are the pathophysiological consequences of the presence of MNPs in the human urinary tract?
For the purpose of this review, a broad definition of the term ‘urinary tract’ will be employed, inclusive of the kidneys, bladder, ureter, urethra, and urine. This will ensure that a broad scope of the literature is undertaken which may assist in elucidating the complex interactions between plastic in urine and adjacent structures. By focusing on the urinary tract, this review attempts to solidify the field’s understanding of MNPs, raise awareness of this important emerging issue, and lay the foundation for further research which may assist in the development of public health policies and clinical practice guidelines.
Methods
Protocol and registration
An a priori protocol (https://osf.io/wjk9u) was developed in line with the recommendation of the Joanna Briggs Institute (JBI) and the PRISMA extension for scoping reviews reporting guidelines (PRISMA-ScR). This protocol was published on the Open Science Framework on the 20/02/2024.
Eligibility criteria
A pre-determined eligibility criteria was developed, informed by the population (human), concept (microplastics or nanoplastics and their effects) and context (urinary tract). Pre-determined definitions were developed and outlined within the a priori protocol after careful evaluation of the existing literature. For clarity, plastics were defined as a synthetic or semi-synthetic material comprising organic polymers from plant extracts or fossil fuels. The term ‘urinary tract’ was defined, in line with the National Institute of Diabetes and Digestive and Kidney Diseases, as a system of organs, including the kidneys, ureter, bladder, and urethra, responsible for the production, storage and excretion of urine [30]. To ensure a broad and thorough scope of the literature was undertaken, all research methodologies and abstracts were included with the exception of narrative reviews. Pre-print articles were included following a critical review of the article’s methodology by authors experienced in laboratory methodologies.
Search strategy
A search strategy was developed utilising a three-step methodological approach originally proposed by Arksey and O’Malley [31] and further outlined by the JBI [32]. Firstly, a pilot search of PubMed and Google Scholar was undertaken on the 19/01/2024. Secondly, results were reviewed to identify additional search terms, with the final search strategy being translated for additional search engines with the assistance of a validated search engine translation software (Systematic Review Accelerator [SRA] Polyglot [33]) (Appendix 1). An additional search for grey literature was undertaken utilising Research Rabbit [34], TERA Farmer [35] and Perplexity [36].
Information sources
Five databases (PubMed, EMBASE, CINAHL, SCOPUS and Web of Science) were searched on the 15/02/2024. Results from database searches were exported in EndNote X9 [37].
Selection of sources of evidence
Duplicate results were removed utilising automation software (SRA Deduplicator) [38]. Articles were screened by two authors (AG and LO) by title and abstract within SRA Screenatron [38]. Full text screening was undertaken within Covidence [39] by two authors (AG and LO). Due to a lack of disagreement, a third author was not required to resolve disputes.
Data charting of data items
A draft extraction table was developed within Microsoft Excel to align with the aims of the scoping review, which was piloted and refined prior to two authors (AG and LO) undertaking full data extraction. Where information was not relevant or not reported, this was recorded for clarity.
Synthesis of results
Data pertaining to definitions was extracted, and where possible, synthesised to assist in analysis. Data pertaining to the countries and years of publication was tabulated and visually represented. To assist in evaluation, studies identifying the presence of plastic in human specimens, and studies evaluating the effects of plastic on cellular viability, uptake, and function have been tabulated separately.
Results
Selection of sources of evidence
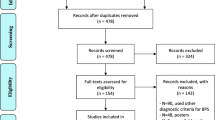
Database searching led to the retrieval of 2534 articles, of which 1536 articles were removed via automation. Title and abstract screening of the remaining 998 articles led to the exclusion of a further 977 articles. The full text of the remaining 21 articles was successfully retrieved and screened with substantial agreement between authors (Cohen’s Kappa = 0.765), leading to the exclusion of a further five articles [40]. A final grey literature search revealed two additional articles, one of which was a pre-print (Fig. 1).
Synthesis of results
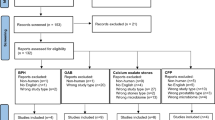
Of the 18 identified articles, the authorship groups represent seven countries: Pakistan (n = 1), Netherlands (n = 1), the United States of America (n = 1), Taiwan (n = 1), Germany (n = 3), China (n = 5), and Italy (n = 6). Only one identified article was published prior to 2022 (Fig. 2). Six articles (Fig. 3) identified and characterised the presence of MNPs in human urine (n = 5), human kidney samples (n = 2), and bladder cancer (n = 1). In addition, 12 articles investigated the effect of MNPs on human renal tubular epithelial cells (HK-2) (n = 5), human embryonic kidney cells (HEK 293) (n = 4), human embryonic kidney SV40 large T antigen cells (293T) (n = 3) and human podocytes (n = 1).
Definitions of microplastics and nanoplastics
Only 12 out of the 18 articles provided a description of MPs or NPs (Table 1). The size of MPs varied between 0.1 μm and 5 mm. In addition, six out of the 12 articles differentiated between MPs and NPs. Descriptions of NPs varied between 1 μm and <0.1 μm.
Identification techniques and characteristics of microplastics and nanoplastics
The most commonly utilised method for detecting and characterising MNPs in human samples was Raman spectroscopy (5/6; 83%) (Fig. 4). Alternatively, Song et al. [41] utilised pyrolysis-gas chromatography mass spectroscopy combined with laser direct infrared spectroscopy. Four articles described the number of samples in which MNPs were identified (Table 2). MNPs were identified in 15/28 (54%) of the human urine samples, 13/19 (68%) of the human bladder cancer samples and 7/10 (70%) of the human kidney samples. Both MNP fibres and particles were identified within specimens with large variations in size, from 0.1 nm to 871 μm (Fig. 5). Thirteen types of polymers were identified within the samples. Polystyrene was the only polymer which was identified across urine, kidney and bladder cancer samples (Table 2).
In vitro exposure of MNPs in renal cells
A significant proportion of studies (9/12 or 75%) used fluorescence labelling to track the internalisation of MNPs in renal cells, suggesting that fluorescence-based techniques are commonly employed for the visualisation and quantification of MNP uptake (Table 3). The primary techniques across studies varied, but included cell viability assays, microscopy, and flow cytometry. Interestingly, almost all studies (8/12 or 67%) used polystyrene as the model for MNPs, with size ranging from 20 nm to 3.39 μm. Additionally, 3/12 of the studies (27%) utilised polyethylene, and one study used a combination of polyvinyl chloride (PVC), polypropylene (PP), polyamide (PA), and tyre wear particles. Moreover, 8/12 of the studies (67%) described the shape of the MNPs used as spherical. Most studies used human renal tubular epithelial cells (HK-2) (5/12 or 42%) and human embryonic kidney cells (HEK 293 and HEK 293T) (6/12 or 50%), with one study using human podocyte cells. Common endpoints included cell viability, inflammatory response, oxidative stress, apoptosis, and changes in MAPK and PI3K-AKT signalling pathways. The exposure of MNPs to renal cells resulted in decreased cell viability [42,43,44,45], increased inflammation and activation of potentially cancer-inducing pathways [43, 46]. One study demonstrated that MNPs facilitated the infection of HEK 293T cells with SARS-CoV-2 [47].
Discussion
To the best of our knowledge, this scoping review provides the first effort to collate and synthesise research investigating the presence and effect of MNPs on the human urinary tract. Considering the World Health Organisation’s (WHO) 2019 statement entitled ‘Microplastics in drinking water’, which downplays the significance of MPs in drinking water, the findings of articles included within this scoping review challenge this position [2]. The WHO’s assertion, made in a 124-page report, that “there is no evidence to indicate a human health concern” is increasingly contradicted by emerging research [2]. Since this report, and a call for further research to be conducted by the WHO, there has been a 15-fold increase in the number of publications made investigating the harmful impacts of MNPs [48] with numerous publications demonstrating harmful effects [43, 45, 49, 50]. The articles identified in this scoping review reported MNPs led to increased inflammation [43, 45, 49, 50], cellular toxicity [42,43,44,45, 49, 51], and disruption to normal physiological processes [43, 46, 52]. While not the focus of this scoping review, an even greater number of animal studies report similar findings highlighting MNP exposure as a threat to One Health [53]. This challenges the WHO’s initial assessment and highlights the urgent need for revaluation of MNPs impact on human health.
Defining micro-nano-plastics
Significant inconsistencies exist between definitions of MPs and NPs within academic literature, in addition to those proposed by industrial bodies and government authorities. The majority of articles [41, 42, 44, 45, 50, 52, 54, 55] adopt a size-related definition of MPs as plastic particles less than 5 mm, in line with the position of the European Union. However, a number of these articles specify a lower limit for the size of MPs, choosing to also define NPs. For instance, Li et al. [45] and Song et al. [41] define NPs as particles smaller than 1 μm, while Zhu et al. [43] set the limit at 0.1 μm. The size of the MNPs significantly impacts the manner and rate of uptake by cells with smaller particles having been observed to be internalised at a greater rate through endocytic or passive uptake processes, whereas larger particles are more dependent on phagocytosis mechanisms [56, 57]. Similarly, the pathophysiological effects of MNPs have been observed to be size-dependent, potentially due to a higher surface area to volume ratio [58]. Polystyrene nanoparticles (20–50 nm), for example, induce apoptosis and inflammation in HK-2 cells [43]. Additionally, HEK 293 cells exposed to polystyrene NPs (20, 60, 100, 500, 1000 nm) showed size- and concentration-dependent toxicity, with smaller particles causing more significant viability reduction and oxidative damage [45]. Moreover, a study on mice demonstrated that microplastics (5 μm and 20 μm) accumulated in the kidney, liver and gut, with smaller particles showing higher tissue accumulation and associated toxic effects, including oxidative stress and inflammation [59]. This size-dependent toxicity highlights the need for standardised definitions to ensure consistent communication of research findings. In addition, further categorisation may be required to take into account other variables such as morphology (e.g. shape, surface characteristics and polymer matrix), additives including pigments, and particle charge. As research continues to be undertaken, it is essential for clear universal definitions surrounding MNPs to ensure they are useful for academic and clinical science while facilitating accuracy through consistency within this rapidly evolving field.
Cytotoxicity of MNPs
The cytotoxic effect of MNPs, and the various mechanisms by which MNPs induce cellular damage, has received increasing attention within research in recent years amongst a variety of organ systems, such as the gastrointestinal tract and cell lines, including peripheral blood lymphocytes [60,61,62,63,64]. To date, a limited number of polymer types and shapes have been utilised within cells lines relating to the urinary tract to investigate their potential deleterious effects. Currently, pristine polystyrene spheres are the most commonly utilised MNP model. Previously, rat models have demonstrated the nephrotoxicity of polystyrene NPs, highlighting their potential ability to induce oxidative damage and endoplasmic reticulum stress [17, 65]. The study by Li et al. [45] highlights the significant cytotoxicity of polystyrene NPs on HEK 293T cells, which found a 74.8% and 53.0% reduction in cell viability after 12 h when exposed to 60 nm and 20 nm particles, respectively. Importantly, these results may significantly underestimate the true toxic effect of MNPs. Dailianis et al. demonstrated that polystyrene NPs following degradation via ultraviolet radiation exposure, a more realistic simulation of human environmental exposure, had a significant increase in cytotoxicity [66]. Regardless, these findings are particularly concerning when compared to the cytotoxic effects of the chemotherapy drug cisplatin, commonly used to treat bladder [67], testicular [68], lung [69], ovarian [70], head and neck [71], and cervical cancer [67]. On the same HEK 293T cell line, cisplatin reduced cell viability by ~80% over 24 h [72]. The comparison underscores the potent cytotoxicity of NPs, which rivals that of pharmaceutical agents specifically designed to kill cancer cells. Increased nephrotoxicity, associated with lifelong accumulation of MNPs, has potential aetiological implications for chronic kidney disease. Of particular concern are patients who progress to requiring dialysis, which may inadvertently introduce massive quantities of MNPs directly into the bloodstream (Fig. 6) [73].
MNP associated renal disease
Recent animal studies have elucidated multiple pathways through which these plastic particles can induce renal injury. Renal damage from disruption of the gut-kidney axis may occur as a result of increased intestinal inflammation-associated permeability following MNP ingestion. This could have the flow-on effect of leading to the translocation of lipopolysaccharides into the bloodstream and activation of the C5a/C5aR pathway [74].
Recent findings from Xu et al. further elucidate the impact of polystyrene MPs, particularly when combined with a high-fat diet, using mouse models [75]. Utilising single-cell RNA sequencing, they revealed that polystyrene MPs alongside a high-fat diet exacerbate kidney injury in mice, inducing a profibrotic microenvironment and reshaping kidney cellular components [75]. This treatment inhibited renal development and induced ROS-driven carcinogenesis, through the activation of cancer-related signalling pathways like PI3K-AKT, MAPK and IL-17 in endothelial cells [75]. These findings are similar to those of Shu et al. and Xiao et al. who reported the activation of P13K-AKT and MAPK within human HK-2 cell lines [43, 46]. Additionally, PF4+ macrophages were identified as key players in promoting renal fibrosis and a pro-tumorigenic microenvironment [75]. While MNPs have not been observed within human kidney tumours to date, their presence in 13 out of 19 bladder cancers and presence within other tumours at rates higher than adjacent healthy tissue warrants further investigation.
Adding to this, Wang et al. investigated the nephrotoxicity of polystyrene MPs in juvenile rats [17]. Their study demonstrated that oral exposure (1000 nm, 2.0 mg/kg/d for 28 days) significantly reduced growth rates and organ indices, and induced oxidative stress, inflammation and endoplasmic reticulum stress in kidneys. Histological analysis showed kidney lesions, disrupted serum biomarkers (blood urea nitrogen and creatinine) related to acute kidney injury [76], and elevated pro-inflammatory mediators (IL-1β, IL-6, TNF-α) [17]. Furthermore, they found that polystyrene MP exposure led to renal cell apoptosis and endoplasmic reticulum stress, confirmed by increased expression of apoptosis-related genes [17]. Treatments with N-acetyl-cysteine and Salubrinal somewhat alleviated these effects, highlighting oxidative stress and ER stress as central mechanisms in polystyrene MP-induced nephrotoxicity [17], while also demonstrating the potential for pharmacological treatments in future to combat the potential harmful effects of MNP exposure. The widespread physiological mechanisms through which MNPs have the potential to alter renal physiology, in combination with their demonstrated involvement in the aetiology of atherosclerosis, [77,78,79,80] also suggests MNPs may play a role in the aetiology of renal vascular diseases (such as renal artery stenosis and renovascular hypertension), as well as lower urinary tract symptoms relating to storage and voiding [81].
MNP associated bladder disease and dysfunction
The urothelium lining of the bladder, originally viewed as a passive barrier, is now recognised as a primary transducer of specialised sensory properties, containing adrenergic, muscarinic, and purinergic receptors, and facilitating secretion of mediators including acetylcholine (ACh), nitric oxide (NO), adenosine triphosphate (ATP) and prostaglandins [82]. These mediators are vital for the urothelium’s role in modulating detrusor muscle contractions and sensing bladder fullness. The confirmed uptake of MNPs by cells, as evidenced by multiple studies [44,45,46, 51, 83, 84], demonstrates mechanisms by which MNPs could interfere with these critical functions.
For example, both animal and human cell line studies indicate that polystyrene MNPs cause significant mitochondrial damage, as evidenced by significantly decreased ATP production and increased oxidative stress in human umbilical vein endothelial cells (up to 82% decrease) [85], embryonic kidney (293T) and liver (LO2) cells [45]. This disruption in ATP production has implications for bladder physiology with clinical relevance for patients with urinary incontinence, due to ATPs requirement in activating purinergic receptors, such as P2X1, P2Y12, and A2b, involved in controlling the contractility and relaxation of bladder smooth muscle cells [81]. Additionally, Wang et al. [86] investigated the neurotoxic effects of polystyrene MPs on brain tissue in mice, finding that exposure to these plastics resulted in decreased levels of ACh. ACh has an important role in normal bladder function as the main stimulus for contraction of the urinary bladder smooth muscle [87]. Despite having not been investigated to date, the distension of the bladder endothelium during filling is likely to increase the permeability and, consequently, uptake of MNPs in a similar manner to pulmonary cells, potentially assisting in the exacerbation of some of these effects [88]. Regardless, the MNPs could have profound effects on urinary bladder health and incontinence, underscoring the pressing need for targeted research to understand the impact of MNPs on the urinary system.
Implications for infections affecting the urinary tract
The presence of MNPs in the urinary tract could increase the risk of UTIs including cystitis, urethritis, and pyelonephritis, by facilitating the intracellular transport of pathogenic microbes by trojan horse mechanisms, such as the formation of a protein corona, and reducing the efficacy of the innate immune system [4789,90,91]. Zhang et al. [47] demonstrated the potential for MNPs to facilitate the infection of HEK293T cells by shuttling the virus into the endo-lysosomal compartment. The ability for MNPs to facilitate infection has also been demonstrated with influenza-A within A549 cell lines [91]. The rough surfaces of MNPs provide an ideal environment for bacterial adhesion and biofilm formation, potentially leading to more persistent and recurrent UTIs [92, 93]. The widespread presence of MNPs within human testicles and semen [94, 95] also highlights the potential increased transmission risk and difficulties in the treatment of sexually transmitted infections facilitated by immune suppression and trojan horse transmission [96]. As a result, MNP-associated infections impacting the urinary tract may have significant implications for worldwide antimicrobial resistance [97].
Limitations of the papers included in this review
This scoping review highlights a lack of research into the effects of various surface characteristics and particle charges, factors which have been shown to dramatically increase the toxicity of MNPs within other organ systems. A methodological focus on the use of Raman spectroscopy to analyse the presence of microplastics in human tissue prevents an accurate understanding of the degree of MNP contamination in humans considering smaller particles are more readily endocytosed. As a result, the dosage of MNPs within cell line studies is arguably speculative to date and may significantly depend on populations and demographics. Moving forward, the use of a multistage analysis process which aims to elucidate the physical characterisation of particles followed by chemical characterisation (e.g. scanning electron microscopy coupled with Raman spectroscopy) may assist in overcoming this limitation [98]. Additionally, the use of atomic force microscopy, although cost prohibitive, may assist in determining surface charges which have been shown to affect the cytotoxicity of NPs and the degree to which they disrupt cellular metabolism [98].
Limitations of this review
The rapid emergence of literature in this field will necessitate a re-evaluation of this review in the near future. In addition, this review is limited by the nature of articles which were included. Specifically, while the abstracts allowed for relevant data to be extracted, they provided a limited discussion of the implications of the research and the future directions, which would assist in informing and organising further research in this field.
Future directions and authors’ recommendations
While a limited number of human tissue samples to date have been analysed, the high rates of MP contamination warrants significant concern. To fully understand the potential implications of MNPs on the urinary tract, further research is required to detect and characterise MNPs in kidney, bladder, ureter and urethral samples. In addition, complementary research methodologies such as surveys should be employed to assist in elucidating how variables such as environments (e.g. city or rural) and lifestyle factors (e.g. food or cosmetic use) affect the level of MNP contamination. The current brevity of research in combination with the high heterogeneity of MNPs suggests that further research is required to fully characterise these exogenous particles (Table 4). This lack of basic understanding of the contamination rate of organs within the human urinary tract currently hinders researchers from undertaking research on cell lines with plastic models (e.g. polymer types, shapes, additives, etc.), similar to those found within human samples. In addition, IC50 values for MNPs within cell dose-response studies would assist in developing our understanding of the toxicity of various polymer types and morphologies while allowing for a comparison between other cytotoxic compounds.
Conclusion
MNPs are increasingly being detected within human organs systems including the human urinary tract. While a limited amount of research has been conducted to date to characterise the types of plastic and their effects on the human urinary tract, growing evidence for the deleterious effects of MNPs on inflammation, cell viability, metabolism and cancer-related pathways warrants significant concern. The WHO, as well as other national and international health authorities, are urged to review current recommendations that human consumption of MPs present no threat to the health and wellbeing of the public. Moving forward, urgent research is required to (a) investigate and characterise MNP contamination, (b) understand the effects of MNPs and their impact on global burden of diseases, (c) develop solutions to prevent and treat MNP contamination within the human urinary tract, and (d) develop a standardised definition of MPs and NPs to be adopted globally, to facilitate research and assist with its translation into policy and healthcare.
Data availability
Data is available upon reasonable request to the corresponding author.
References
Walker TR, Fequet L. Current trends of unsustainable plastic production and micro(nano)plastic pollution. TrAC Trends Anal Chem. 2023;160:116984.
Microplastics in drinking water World Health Organization World Health Organization 2019 28/08/2019. Report No.: 978-92-4-151619-8.
Cai Z, Li M, Zhu Z, Wang X, Huang Y, Li T, et al. Biological degradation of plastics and microplastics: a recent perspective on associated mechanisms and influencing factors. Microorganisms. 2023;11:1661.
Aydın RB, Yozukmaz A, Şener İ, Temiz F, Giannetto D. Occurrence of microplastics in most consumed fruits and vegetables from Turkey and public risk assessment for consumers. Life. 2023;13:1686.
Lim X. Microplastics are everywhere—but are they harmful. Nature. 2021;593:22–5.
Susanti N, Mardiastuti A, Wardiatno Y. Microplastics and the impact of plastic on wildlife: a literature review. IOP Conf. Ser Earth Environ Sci. 2020;528:012013.
Wootton N, Ferreira M, Reis-Santos P, Gillanders BM. A comparison of microplastic in fish from Australia and Fiji. Front Mar Sci. 2021;8:690991.
Hale RC, Seeley ME, La Guardia MJ, Mai L, Zeng EY. A global perspective on microplastics. J Geophys Res Oceans. 2020;125:e2018JC014719.
Gasperi J, Wright SL, Dris R, Collard F, Mandin C, Guerrouache M, et al. Microplastics in air: are we breathing it in? Curr Opin Environ Sci Health. 2018;1:1–5.
Yang L, Zhang Y, Kang S, Wang Z, Wu C. Microplastics in soil: a review on methods, occurrence, sources, and potential risk. Sci Total Environ. 2021;780:146546.
Zhang D, Wu C, Liu Y, Li W, Li S, Peng L, et al. Microplastics are detected in human gallstones and have the ability to form large cholesterol-microplastic heteroaggregates. J Hazard Mater. 2024;467:133631.
Horvatits T, Tamminga M, Liu B, Sebode M, Carambia A, Fischer L, et al. Microplastics detected in cirrhotic liver tissue. EBioMedicine. 2022;82:104147.
Yang Y, Xie E, Du Z, Peng Z, Han Z, Li L, et al. Detection of various microplastics in patients undergoing cardiac surgery. Environ Sci Technol. 2023;57:10911–8.
Braun T, Ehrlich L, Henrich W, Koeppel S, Lomako I, Schwabl P, et al. Detection of microplastic in human placenta and meconium in a clinical setting. Pharmaceutics. 2021;13:921.
Huang S, Huang X, Bi R, Guo Q, Yu X, Zeng Q, et al. Detection and analysis of microplastics in human sputum. Environ Sci Technol. 2022;56:2476–86.
Wang Y-L, Lee Y-H, Hsu Y-H, Chiu I-J, Huang CC-Y, Huang C-C, et al. The kidney-related effects of polystyrene microplastics on human kidney proximal tubular epithelial cells HK-2 and male C57BL/6 mice. Environ Health Perspect. 2021;129:057003.
Wang W, Guan J, Feng Y, Nie L, Xu Y, Xu H, et al. Polystyrene microplastics induced nephrotoxicity associated with oxidative stress, inflammation, and endoplasmic reticulum stress in juvenile rats. Front Nutr. 2023;9:1059660.
Microplastics European Commission [cited 2024 Feb 28]. Available from: https://environment.ec.europa.eu/topics/plastics/microplastics_en#:~:text=Related%20links-,Overview,hard%20to%20remove%20from%20nature
Critical Aspects of Sustainability (CAS): MIcro- and Nanoplastics (MNP) U.S. National Science Foundation U.S. National Science Foundation [cited 2024 Feb 28]. Available from: https://www.nsf.gov/pubs/2020/nsf20050/nsf20050.jsp#1
Plastics—Environmental Aspects—State of knowledge and methodologies. International Standards Organisation International Standards Organisation 2024 [cited 2024 Feb 28]. Available from: https://www.iso.org/obp/ui/#iso:std:iso:tr:21960:ed-1:v1:en:en%20
Schneider M, Stracke F, Hansen S, Schaefer UF. Nanoparticles and their interactions with the dermal barrier. Derm-Endocrinol. 2009;1:197–206.
Yee MS-L, Hii L-W, Looi CK, Lim W-M, Wong S-F, Kok Y-Y, et al. Impact of microplastics and nanoplastics on human health. Nanomaterials. 2021;11:496.
Wu P, Lin S, Cao G, Wu J, Jin H, Wang C, et al. Absorption, distribution, metabolism, excretion and toxicity of microplastics in the human body and health implications. J Hazard Mater. 2022;437:129361.
Zhu L, Xie C, Chen L, Dai X, Zhou Y, Pan H, et al. Transport of microplastics in the body and interaction with biological barriers, and controlling of microplastics pollution. Ecotoxicol Environ Saf. 2023;255:114818.
Prata JC, da Costa JP, Lopes I, Duarte AC, Rocha-Santos T. Environmental exposure to microplastics: an overview on possible human health effects. Sci Total Environ. 2020;702:134455.
Gautam R, Jo J, Acharya M, Maharjan A, Lee D, Kc PB, et al. Evaluation of potential toxicity of polyethylene microplastics on human derived cell lines. Sci Total Environ. 2022;838:156089.
Fleury J-B, Baulin VA. Microplastics destabilize lipid membranes by mechanical stretching. Proc Natl Acad Sci USA. 2021;118:e2104610118.
Yang X, Chen H, Zheng Y, Qu S, Wang H, Yi F. Disease burden and long-term trends of urinary tract infections: a worldwide report. Front Public Health. 2022;10:888205.
Vanholder R, Annemans L, Brown E, Gansevoort R, Gout-Zwart JJ, Lameire N, et al. Reducing the costs of chronic kidney disease while delivering quality health care: a call to action. Nat Rev Nephrol. 2017;13:393–409.
The urinary tract and how it works National Institute of Diabetes and Digestive and Kidney Diseases [cited 2024]. Available from: https://www.niddk.nih.gov/health-information/urologic-diseases/urinary-tract-how-it-works#:~:text=The%20urinary%20tract%20is%20the,Kidneys
Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8:19–32.
JBI Mevidence Synthesis 2024 Edition JBI; [cited 2024]. Available from: https://jbi-global-wiki.refined.site/space/MANUAL
Kung JY. Polyglot search translator. J Can Health Libraries Assoc. 2022;43:35.
Research Rabbit [05/03/2024]. Available from: https://www.researchrabbit.ai/
TERA Farmer [05/03/2023]. Available from:https://terafarmer.tera-tools.com/
Perplexity.ai. Available from: https://www.perplexity.ai/
EndNote X9 [05/03/2024]. Available from: https://endnote.com/
Systematic Review Accelerator. Available from: https://sr-accelerator.com/#/
Covidence [05/03/2024]. Available from: https://Covidence.org
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Song X, Chen T, Chen Z, Du L, Qiu X, Zhang Y, et al. Micro(nano)plastics in human urine: a surprising contrast between Chongqing’s urban and rural regions. Sci Total Environ. 2024;917:170455.
La Porta E WCN23-0982 The burden of plastic in human health: presence of microplastics in kidney and their prospective nephrotoxicity. Kidney Int Rep. 2023;8:S254.
Zhu Z, Liao R, Shi Y, Li J, Cao J, Liao B, et al. Polystyrene nanoplastics induce apoptosis of human kidney proximal tubular epithelial cells via oxidative stress and MAPK signaling pathways. Environ Sci Pollut Res Int. 2023;30:110579–89.
Chen YC, Chen KF, Lin KA, Chen JK, Jiang XY, Lin CH The nephrotoxic potential of polystyrene microplastics at realistic environmental concentrations. J Hazard Mater. 2022;427:127871.
Li Y, Li Y, Li J, Song Z, Zhang C, Guan B. Toxicity of polystyrene nanoplastics to human embryonic kidney cells and human normal liver cells: Effect of particle size and Pb(2+) enrichment. Chemosphere. 2023;328:138545.
Xiao M, Li X, Zhang X, Duan X, Lin H, Liu S, et al. Assessment of cancer-related signaling pathways in responses to polystyrene nanoplastics via a kidney-testis microfluidic platform (KTP). Sci Total Environ. 2023;857:159306.
Zhang G, Cao G, Luo R-H, Song Q, Zeng Y, Liu K, et al. Microplastics interact with SARS-CoV-2 and facilitate host cell infection. Environ Sci Nano. 2022;9:2653–64.
WHO calls for more research into microplastics and a crackdown on plastic pollution: World Health Organisation [cited 2024 Mar 18]. Available from: https://www.who.int/news/item/22-08-2019-who-calls-for-more-research-into-microplastics-and-a-crackdown-on-plastic-pollution
Beltrame A, Rumeo N, La Porta E, Verzola D, Angeletti A, Lugani F, et al. PRO-inflammatory effects of bisphenol A and polyethylene microplastics on human renal tubular cells. Nephrol Dial Transplant. 2023;38:gfad063c_5502.
Cervello C, Bruschi M, Candiano G, Kajana X, Garbarino A, Rumeo N, et al. Microplastics: first extended proteomic analysis on kidney tubular cells. Nephrol Dial Transplant. 2023;38:gfad063a_6225.
Yarbakht M, Sarau G, Kling L, Müller-Deile J, Kotb A, Christiansen S, et al. Analyzing the effect of microplastic particles on human podocytes. Nephrology Dialysis Transplantation. 2021;36:gfab079.0011.
Goodman KE, Hua T, Sang QA. Effects of polystyrene microplastics on human kidney and liver cell morphology, cellular proliferation, and metabolism. ACS Omega. 2022;7:34136–53.
Morrison M, Trevisan R, Ranasinghe P, Merrill GB, Santos J, Hong A, et al. A growing crisis for One Health: impacts of plastic pollution across layers of biological function. Front Mar Sci. 2022;9:980705.
Exacoustos O, Artini C, Massardo S, Caboni C, Pastorino A, Chiarenza S, et al. First identification and characterization of microplastics in human kidney and urine. Nephrol Dial Transplant. 2023;38:gfad063a_6111.
Massardo S, Verzola D, Alberti S, Caboni C, Santostefano M, Eugenio Verrina E, et al. MicroRaman spectroscopy detects the presence of microplastics in human urine and kidney tissue. Environ Int. 2024;184:108444.
Florence AT, Hillery AM, Hussain N, Jani PU. Factors affecting the oral uptake and translocation of polystyrene nanoparticles: histological and analytical evidence. J Drug Target. 1995;3:65–70.
Liu L, Xu K, Zhang B, Ye Y, Zhang Q, Jiang W. Cellular internalization and release of polystyrene microplastics and nanoplastics. Sci Total Environ. 2021;779:146523.
Banerjee A, Shelver WL. Micro- and nanoplastic induced cellular toxicity in mammals: a review. Sci Total Environ. 2021;755:142518.
Deng Y, Zhang Y, Lemos B, Ren H. Tissue accumulation of microplastics in mice and biomarker responses suggest widespread health risks of exposure. Sci Rep. 2017;7:46687.
Çobanoğlu H, Belivermiş M, Sıkdokur E, Kılıç Ö, Çayır A. Genotoxic and cytotoxic effects of polyethylene microplastics on human peripheral blood lymphocytes. Chemosphere. 2021;272:129805.
Zhang Y, Wang S, Olga V, Xue Y, Lv S, Diao X, et al. The potential effects of microplastic pollution on human digestive tract cells. Chemosphere. 2022;291:132714.
Goodman KE, Hare JT, Khamis ZI, Hua T, Sang Q-XA. Exposure of human lung cells to polystyrene microplastics significantly retards cell proliferation and triggers morphological changes. Chem Res Toxicol. 2021;34:1069–81.
Barceló D, Picó Y, Alfarhan AH. Microplastics: detection in human samples, cell line studies, and health impacts. Environ Toxicol Pharmacol. 2023;101:104204.
Schirinzi GF, Pérez-Pomeda I, Sanchís J, Rossini C, Farré M, Barceló D. Cytotoxic effects of commonly used nanomaterials and microplastics on cerebral and epithelial human cells. Environ Res. 2017;159:579–87.
Choi YJ, Park JW, Lim Y, Seo S, Hwang DY. In vivo impact assessment of orally administered polystyrene nanoplastics: biodistribution, toxicity, and inflammatory response in mice. Nanotoxicology. 2021;15:1180–98.
Dailianis S, Rouni M, Ainali NM, Vlastos D, Kyzas GZ, Lambropoulou DA, et al. New insights into the size-independent bioactive potential of pristine and UV-B aged polyethylene microplastics. Sci Total Environ. 2024;918:170616.
Brown A, Kumar S, Tchounwou PB. Cisplatin-based chemotherapy of human cancers. J Cancer Sci Ther. 2019;11:97.
Hu Z, Yu J, Gui G, Chen Y, Huang R, Jiang L, et al. Cisplatin for testicular germ cell tumors: a rapid review. J Evid Based Med. 2016;9:144–51.
Fennell D, Summers Y, Cadranel J, Benepal T, Christoph D, Lal R, et al. Cisplatin in the modern era: the backbone of first-line chemotherapy for non-small cell lung cancer. Cancer Treat Rev. 2016;44:42–50.
Song M, Cui M, Liu K. Therapeutic strategies to overcome cisplatin resistance in ovarian cancer. Eur J Med Chem. 2022;232:114205.
Schaeffers AW, Devriese LA, van Gils CH, Dankbaar JW, Voortman J, de Boer JP, et al. Low dose cisplatin weekly versus high dose cisplatin every three weeks in primary chemoradiotherapy in head and neck cancer patients with low skeletal muscle mass: the CISLOW-study protocol. Plos one. 2023;18:e0294147.
Zhou Y-D, Hou J-G, Yang G, Jiang S, Chen C, Wang Z, et al. Icariin ameliorates cisplatin-induced cytotoxicity in human embryonic kidney 293 cells by suppressing ROS-mediated PI3K/Akt pathway. Biomed Pharmacother 2019;109:2309–17.
Passos RS, Davenport A, Busquets R, Selden C, Silva LB, Baptista JS, et al. Microplastics and nanoplastics in haemodialysis waters: Emerging threats to be in our radar. Environ Toxicol Pharmacol. 2023;102:104253.
Liang Y, Liu D, Zhan J, Liu X, Li P, Ma X, et al. Polystyrene microplastics induce kidney injury via gut barrier dysfunction and C5a/C5aR pathway activation. Environ Pollut. 2024;342:122909.
Xu W, Ye S, Liu W, Guo H, Zhang L, Wei S, et al. Single-cell RNA-seq analysis decodes the kidney microenvironment induced by polystyrene microplastics in mice receiving a high-fat diet. J Nanobiotechnol. 2024;22:13.
Uchino S, Bellomo R, Goldsmith D. The meaning of the blood urea nitrogen/creatinine ratio in acute kidney injury. Clin Kidney J. 2012;5:187–91.
Marfella R, Prattichizzo F, Sardu C, Fulgenzi G, Graciotti L, Spadoni T, et al. Microplastics and nanoplastics in atheromas and cardiovascular events. N. Engl J Med. 2024;390:900–10.
Gimbrone MA Jr, García-Cardeña G. Endothelial cell dysfunction and the pathobiology of atherosclerosis. Circ Res. 2016;118:620–36.
Lee HS, Amarakoon D, Wei CI, Choi KY, Smolensky D, Lee SH. Adverse effect of polystyrene microplastics (PS-MPs) on tube formation and viability of human umbilical vein endothelial cells. Food Chem Toxicol. 2021;154:112356.
Lu YY, Li H, Ren H, Zhang X, Huang F, Zhang D, et al. Size-dependent effects of polystyrene nanoplastics on autophagy response in human umbilical vein endothelial cells. J Hazard Mater. 2022;421:126770.
Birder LA. Is there a role for oxidative stress and mitochondrial dysfunction in age-associated bladder disorders? Tzu Chi Med J. 2020;32:223–6.
Birder LA, de Groat WC. Mechanisms of disease: involvement of the urothelium in bladder dysfunction. Nat Clin Pr Urol. 2007;4:46–54.
Richards CJ, Burgers TCQ, Vlijm R, Roos WH, Åberg C. Rapid Internalization of Nanoparticles by Human Cells at the Single Particle Level. ACS Nano. 2023;17:16517–16529.
Firdessa R, Oelschlaeger TA, Moll H. Identification of multiple cellular uptake pathways of polystyrene nanoparticles and factors affecting the uptake: relevance for drug delivery systems. Eur J Cell Biol. 2014;93:323–37.
Fu Y, Fan M, Xu L, Wang H, Hu Q, Jin Y. Amino-functionalized polystyrene nano-plastics induce mitochondria damage in human umbilical vein endothelial cells. Toxics. 2022;10:215.
Wang S, Han Q, Wei Z, Wang Y, Xie J, Chen M. Polystyrene microplastics affect learning and memory in mice by inducing oxidative stress and decreasing the level of acetylcholine. Food Chem Toxicol. 2022;162:112904.
Nausch B, Heppner TJ, Nelson MT. Nerve-released acetylcholine contracts urinary bladder smooth muscle by inducing action potentials independently of IP3-mediated calcium release. Am J Physiol Regul Integr Comp Physiol. 2010;299:R878–88.
Cavanaugh KJ, Cohen TS, Margulies SS. Stretch increases alveolar epithelial permeability to uncharged micromolecules. Am J Physiol Cell Physiol. 2006;290:C1179–88.
Yang W, Jannatun N, Zeng Y, Liu T, Zhang G, Chen C, et al. Impacts of microplastics on immunity. Front Toxicol. 2022;4:956885.
Brouwer H, Porbahaie M, Boeren S, Busch M, Bouwmeester H. The in vitro gastrointestinal digestion-associated protein corona of polystyrene nano-and microplastics increases their uptake by human THP-1-derived macrophages. Part Fibre Toxicol. 2024;21:4.
Wang C, Wu W, Pang Z, Liu J, Qiu J, Luan T, et al. Polystyrene microplastics significantly facilitate influenza A virus infection of host cells. J Hazard Mater. 2023;446:130617.
Sooriyakumar P, Bolan N, Kumar M, Singh L, Yu Y, Li Y, et al. Biofilm formation and its implications on the properties and fate of microplastics in aquatic environments: a review. J Hazard Mater Adv. 2022;6:100077.
Hossain MR, Jiang M, Wei Q, Leff LG. Microplastic surface properties affect bacterial colonization in freshwater. J Basic Microbiol. 2019;59:54–61.
Zhao Q, Zhu L, Weng J, Jin Z, Cao Y, Jiang H, et al. Detection and characterization of microplastics in the human testis and semen. Sci Total Environ. 2023;877:162713.
Montano L, Giorgini E, Notarstefano V, Notari T, Ricciardi M, Piscopo M, et al. Raman Microspectroscopy evidence of microplastics in human semen. Sci Total Environ. 2023;901:165922.
Geng Y, Liu Z, Hu R, Huang Y, Li F, Ma W, et al. Toxicity of microplastics and nanoplastics: invisible killers of female fertility and offspring health. Front Physiol. 2023;14:1254886.
Zhang Y, Lu J, Wu J, Wang J, Luo Y. Potential risks of microplastics combined with superbugs: enrichment of antibiotic resistant bacteria on the surface of microplastics in mariculture system. Ecotoxicol Environ Saf. 2020;187:109852.
Mariano S, Tacconi S, Fidaleo M, Rossi M, Dini L. Micro and nanoplastics identification: classic methods and innovative detection techniques. Front Toxicol. 2021;3:636640.
Barnett AN, Arshad M, Nabi D. A snapshot into the invasion of plastics in human urine. chemRxiv:chemrxiv-2023-rp3vd [Preprint]. 2023 [cited 2023 Jul 25]: [29 p.]. Available from: https://doi.org/10.26434/chemrxiv-2023-rp3vd.
Pironti C, Notarstefano V, Ricciardi M, Motta O, Giorgini E, Montano L. First evidence of microplastics in human urine, a preliminary study of intake in the human body. Toxics. 2022;11:40.
Massardo S, La Porta E, Verrina EE, Lugani F, Alberti S, Caboni C, et al. First detection of microplastics fragments in human urine and kidney tissues: TH-PO1020. J Am Soc Nephrol. 2023;34:376–7.
Krafft C, Popp J, Bronsert P, Miernik A. Raman spectroscopic imaging of human bladder resectates towards intraoperative cancer assessment. Cancers. 2023;15:2162.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
The authors confirm that all listed authors meet the requirements for authorship.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This manuscript is a review article and does not involve a research protocol requiring the approval by the relevant institutional review board or ethics committee.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
O’Callaghan, L., Olsen, M., Tajouri, L. et al. Plastic induced urinary tract disease and dysfunction: a scoping review. J Expo Sci Environ Epidemiol (2024). https://doi.org/10.1038/s41370-024-00709-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41370-024-00709-3
- Springer Nature America, Inc.