Abstract
Objectives
Experimental studies indicate a role for galectin-1 and galectin-3 in metabolic disease, but clinical evidence from larger populations is limited.
Methods
We measured circulating levels of galectin-1 and galectin-3 in the Prospective investigation of Obesity, Energy and Metabolism (POEM) study, participants (n = 502, all aged 50 years) and characterized the individual association profiles with metabolic markers, including clinical measures, metabolomics, adipose tissue distribution (Imiomics) and proteomics.
Results
Galectin-1 and galectin-3 were associated with fatty acids, lipoproteins and triglycerides including lipid measurements in the metabolomics analysis adjusted for body mass index (BMI). Galectin-1 was associated with several measurements of adiposity, insulin secretion and insulin sensitivity, while galectin-3 was associated with triglyceride-glucose index (TyG) and fasting insulin levels. Both galectins were associated with inflammatory pathways and fatty acid binding protein (FABP)4 and -5-regulated triglyceride metabolic pathways. Galectin-1 was also associated with several proteins related to adipose tissue differentiation.
Conclusions
The association profiles for galectin-1 and galectin-3 indicate overlapping metabolic effects in humans, while the distinctly different associations seen with fat mass, fat distribution, and adipose tissue differentiation markers may suggest a functional role of galectin-1 in obesity.
Similar content being viewed by others
Introduction
There is increasing interest in the role of galectins in human health [1,2,3]. Highly conserved between species, galectins mediate a range of physiological effects, including inflammation, tissue remodeling, and metabolism [4]. Galectins miss the classical signal peptide for secretion, are found in high intracellular concentrations, but are readily measurable in human blood [5]. Furthermore, galectins are known to bind to numerous glycoproteins and glycolipids on the cell surface, but the definitive cellular origin, and physiological role of circulating galectins has not yet been demonstrated [5].
Meta-analyses have reported elevated levels of circulating galectin-3 in individuals with obstructive sleep apnea [6], diabetic nephropathy [7] and high plasma levels are associated with increased risk of cardiovascular mortality [8]. Plasma galectin-3 is also higher during early pregnancy in women with gestational diabetes, suggesting a role in metabolic disease [9]. Galectin-3 is involved in the development of insulin resistance through direct interactions with the insulin receptor, with altered insulin-regulated glucose metabolism in adipocytes, myocytes and hepatocytes [10]. Galectin-3 has also been related to lipid content in the liver through interactions with the lipid uptake marker CD36 and PPAR-γ, and ablation of galectin-3 in mice provided a protective effect on non-alcoholic steatohepatitis by reducing liver steatosis [11, 12].
Emerging evidence suggests that another lectin, galectin-1, could have an equal or even more significant role in obesity and metabolic disease [13,14,15,16]. An unbiased proteomic analysis of adipose tissue interstitial fluid in patients with type 2 diabetes (T2D) and healthy controls reported elevated galectin-1 levels in T2D [14]. A cross-sectional community-based study of 989 individuals, found that serum galectin-1 was independently associated with high BMI and serum insulin levels [13]. Increased serum galectin-1 levels were also associated with a higher incidence of T2D in a longitudinal study of 4022 individuals [15]. Furthermore, it has been shown that Lgals1−/− mice on high-fat diet gain less weight than wild-type mice and that galectin-1 interacts with PPAR-γ signaling [16]. Mechanistic studies also suggest a direct role for galectin-1 on lipid metabolism in cultured adipocytes [17]. Taken together, it is likely that the metabolic effects of galectin-1 found in animal models, explain the associations between galectin-1 and T2D in humans.
With the growing number of reports on metabolic effects of different galectins, and the discovery of feasible galectin-1 and galectin-3 inhibitors for human treatment, larger studies on human metabolism are needed [1, 3]. There is also a need for context and overview as to which effects are specific for each galectin, and which effects are general for many galectins [18]. Here, we seek to assess the association profiles of galectin-1 and galectin-3 to glucose homeostasis and different obesity-related variables in the cross-sectional, population-based Prospective investigation of Obesity, Energy and Metabolism (POEM) cohort study from Sweden.
Subjects and methods
Design
This study adopts a cross-sectional, population-based association study design in a cohort (n = 502) of mainly white participants from urban Uppsala, Sweden (Supplementary Fig.).
POEM study participants
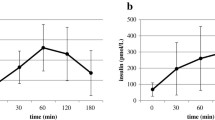
Clinical characteristics and other details of the POEM cohort have been published previously [19,20,21] but is also shown in a Supplementary Table. In brief, 502 participants were invited to participate 1 month after their 50th birthday. Weight, height, waist, and hip measurements were recorded, and total body fat was assessed through bio-impedance (Tanita BC-418, Tokyo, Japan). Participants performed an oral glucose tolerance test (OGTT), with ingestion of 75 g of glucose and continuous measurements of glucose and insulin every 30 min for 2 h. The homeostatic model assessment (HOMA), and the Matsuda index were calculated as previously defined [22, 23]. Further, we calculated TyG index [24] known to be associated with insulin resistance and increased risk to develop cardiometabolic disease [24,25,26].
Blood analysis
Blood was collected after overnight fasting. Analyses were conducted using standard laboratory procedures. Plasma C-peptide levels were measured by enzyme-linked immunosorbent assay (ELISA, Mercodia, Uppsala, Sweden, within assay variation CV < 5%). Plasma galectin-1 levels were determined using ELISA (intra- and inter-assay coefficients of variation were 7.1% and 9.5%, respectively, R&D systems, USA), while plasma galectin-3 was measured with the proximity extension assay technology (Olink, Sweden) [27]. Galectin measurements were performed on all volunteers but one, due to a missing sample.
Imaging and imiomics analyses
A dual-energy X-ray absorptiometry scanner (DXA; Lunar Prodigy, GE Healthcare, USA) determined the participants’ regional (trunk, leg, arm) and total body fat and lean mass. The precision error was 1.5% and 1.0% for total fat and lean mass, respectively. The validity of fat mass derived by Lunar Prodigy has been evaluated against the 4-compartment model, the tool that is currently considered the gold-standard method of body composition appraisal, resulting in 1.7–2.0% higher fat mass estimates with this narrow fan-beam DXA equipment [28].
Whole-body magnetic resonance imaging (MRI) was conducted using a 1.5 T clinical MR system (Philips Achieva, Philips Healthcare, Best, Netherlands). The Imiomics technique utilized in POEM has been described in detail previously [29]. In the Imiomics-analysis, the participants’ voxel-based MRI imaging data are deformed to fit a reference image. The resulting deformation data allow for voxel-wise whole-body statistical analysis of tissue volumes and fat content from the imaging results in relation to non-imaging variables [29, 30]. Quantifying the visceral adipose tissue (VAT) and subcutaneous adipose tissue (SAT) depots was performed by deforming manually defined depots to all subjects. The quantification of liver fat and pancreas fat was performed using dedicated imaging and analysis protocols [30, 31].
Nightingale metabolomics analysis
Targeted metabolomics measurements were performed on stored fasting plasma samples using the Nightingale proton nuclear magnetic resonance (NMR) metabolomics platform (Nightingale Health Ltd., Helsinki, Finland). The method has previously been described in detail, and utilized in several large epidemiological studies [32,33,34]. In brief, a total of 224 metabolites are measured through this technique from the NMR-spectral analysis of two molecular windows, covering various aspects of an individual’s metabolic profile; 171 lipoprotein-related variables and 53 variables related to other metabolic classes are included in the full analysis (https://research.nightingalehealth.com/, last accessed on 2022-05-18).
In this project, we focused on estimates from the main metabolic pathways, including total VLDL (very low-density lipoprotein), LDL (low-density lipoprotein), and HDL (high-density lipoprotein) levels of cholesterol and triglycerides, and total fatty acid levels as well as levels separated by saturation status, amino acids, and other non-lipid metabolites. Stratified data on different lipoprotein particle sizes and markers not directly related to nutrient metabolism, including creatinine and albumin, were excluded in this analysis to simplify the presentation of results.
Metabolon metabolomics analysis
Non-targeted metabolomics measurements were performed on stored fasting plasma samples as previously detailed (Metabolon Inc., USA) [21]. In brief, metabolomics analyses include combining measurements from four different analyses on each sample: two reverse phases (RP)/UPLC-MS/MS (ultra-performance liquid chromatography-mass spectroscopy/MS) methods with positive ion mode electrospray ionization (ESI), one RP/UPLC-MS/MS method with negative ion mode ESI, and one hydrophilic interaction liquid chromatography (HILIC)/UPLC-MS/MS method with negative ion mode ESI. Only annotated, non-xenobiotic metabolites with a call rate >75% were used in the analyses, and values were normalized and given in arbitrary units. Linear regression models assessed the association between each metabolite and galectin-1 or -3 levels, adjusted for sex, education, smoking, exercise habits, and BMI. All Human Metabolome Database IDs of metabolites with a statistically significant association for each galectin, after Bonferroni adjustment for the total number of analyzed metabolites, were uploaded to the MetaboAnalyst 5.0 website in order to perform a targeted metabolic pathway analysis (https://www.metaboanalyst.ca/, accessed on 2023-02-23).
Proteomic analysis
Utilizing proximity extension assay technology coupled with next-generation sequencing (NGS) (Olink Proteomics, Uppsala, Sweden), 1320 proteins from the human proteome were measured in fasting plasma samples [35]. In brief, two oligonucleotide-coupled antibodies are used for each protein. The oligonucleotides hybridize to form a DNA template for NGS, when the antibodies bind close enough on the target. This allows for precise quantification of the proteins. Linear regression models determined the association between each protein and galectin-1 or -3, adjusted for sex, education, smoking, exercise habits, and BMI. All proteins with a statistically significant association for each galectin, after Bonferroni adjustment for the total number of analyzed proteins, were uploaded to the Reactome pathway analysis tool (https://reactome.org/, accessed on 2023-01-27) to explore possible signaling pathways associated with each galectin [36].
Statistics
Continuous variables were z-transformed to allow for effect size comparisons between galectin-1 and galectin-3, with the average set to 0 and the standard deviation to 1. Skewed variables were log-transformed with the natural logarithm for a near normal distribution as indicated in tables. Data were analyzed using linear models, adjusted for sex, education, smoking, and exercise habits unless otherwise specified. The confounders were chosen as plausible factors to influence metabolic outcomes. Due to the previously reported association between galectin-1 and BMI, additional models also adjusting for BMI are presented. A p value below 0.05 was considered statistically significant. Only proteins and metabolites statistically associated with the galectins after Bonferroni adjustment for multiple comparisons were included in the subsequent exploratory pathway analysis.
Results
The association profile for galectin-1 and galectin-3 with adipose tissue variables
Galectin-1 levels were associated with all measures of adiposity in the analysis. The highest β-coefficients were seen with BMI, VAT, and SAT (Table 1). Associations were also significant for fat deposition in sub-compartments from the liver and pancreas, and to total fat-free mass. After additional adjustment for BMI, the galectin-1 associations with fat mass, VAT and SAT were still significant. Plasma galectin-3 levels did not present statistically significant linear associations with any body composition variable.
The association profile for galectin-1 and galectin-3 on metabolic variables
Galectin-1 levels were negatively associated with glucose and positively associated with C-peptide levels, fasting insulin, and insulin resistance measured as HOMA and the Matsuda index (Table 1). Additional adjustment for BMI mitigated most associations. While associations between C-peptide levels, TyG-index and the Matsuda index remained statistically significant, levels of fasting insulin and HOMA results did not. The inverse association with fasting glucose increased both in effect size and degree of significance (lower p value). Galectin-3 levels were also negatively associated with glucose levels and positively associated with fasting insulin levels and TyG-index. However, galectin-3 was not associated with levels of C-peptide or insulin resistance as measured by HOMA and the Matsuda index. Adjustments for BMI drastically weakened the association with fasting insulin, while increasing the inverse association with fasting glucose levels, as observed for galectin-1.
Imiomics associations for galectin-1 and galectin-3
Galectin-1 levels were related to SAT volume in both the upper and lower parts of the body. These associations were generally more pronounced in men than women (Fig. 1A). Galectin-1 was furthermore related to the size of the liver and VAT, and to skeletal muscle volume in the legs. Again, these relationships were more pronounced in men. Levels of galectin-1 were also related to heart size and inversely related to the size of the lungs in both sexes. The fat fraction of SAT and in the liver was related to galectin-1 levels, especially in men. Galectin-1 levels were furthermore related to the intramuscular fat fraction in leg skeletal muscle, as well as to pericardial fat fraction in both sexes. Galectin-3 levels were weakly related to the SAT volume in the hip region in women only (Fig. 1B).
Imiomics associations with galectin-1 (A) and galectin-3 (B) in one representative male (left) and female (right) participant. Associations are presented for tissue volume (left) and fat content (right). Significant (p < 0.05) voxel wise non-parametric Spearman rank coefficient correlation values (r-maps) are shown in the color scale. Positive associations are shown in warm colors (yellow—red) and negative associations are shown in cool colors (green—blue), see the color bars. Pixels with non-significant correlations show the underlying water signal values (gray scale).
Nightingale metabolomics associations for galectin-1 and galectin-3
The BMI-adjusted associations for galectin-1 and galectin-3 with lipoprotein metabolic markers are presented in Fig. 2A. The two galectins had almost identical association patterns with all markers of lipoprotein metabolism. Both galectins were associated with higher levels of total, remnant, LDL, and VLDL cholesterol, as well as serum triglycerides and triglycerides in most lipoproteins. Although similar effect sizes, only galectin-3 and not galectin-1 levels were statistically significantly associated with free cholesterol and HDL triglyceride levels. Conversely, there was a statistically significant inverse association between galectin-1 and HDL and HDL2 cholesterol levels, which was not found with galectin-3. Examining the associations with free fatty acid levels and with other metabolites in glucose and fatty acid metabolism (Fig. 2B), the overall similarities between the two proteins were evident. Both galectins were associated with total-, saturated- and unsaturated fatty acid levels. Inverse associations with glucose, and positive associations with citrate, were also seen for both galectin-1 and -3. There was a statistical difference for docosahexaenoic acid which was only significantly associated with galectin-3 levels, and an association with acetate only significant for galectin-1. However, the directions of effect were similar for these markers. Similarities were also present in the association profile with amino acids (Fig. 2C). Galectin-1 was associated with isoleucine, alanine, and phenylalanine levels, while galectin-3 was associated with leucine and isoleucine and presented an inverse association with tyrosine.
Body mass index-adjusted linear associations for the two markers with markers of lipoprotein metabolism (A), fatty-acid and glucose metabolism (B), and amino acids (C). HDL high-density lipoprotein, IDL intermediate-density lipoprotein, LDL low-density lipoprotein, VLDL very low-density lipoprotein.
Metabolon metabolomics and MetaboAnalyst results for galectin-1 and galectin-3
Galectin-1 presented a larger number of statistically significant associations with other metabolites than galectin-3 after adjustment for multiple comparisons (81 versus 19 associated metabolites). Galectin-1-associated metabolites were overrepresented in histidine metabolism, pentose, and glucuronate interconversions, ascorbate and aldarate metabolism, cysteine and methionine metabolism, as well as in the citrate cycle (TCA cycle) (Table 2). Galectin-3 associated metabolites were overrepresented in sphingolipid metabolism and glycosylphosphatidylinositol (GPI)-anchor biosynthesis (Table 2).
Proteomic associations for galectin-1 and galectin-3
Galectin-1 presented a larger number of statistically significant associations with other proteins than galectin-3 after Bonferroni-adjustment for multiple comparisons (354 versus 57 associated proteins). Associated proteins were used to examine associated pathways using the Reactome pathway analysis tool, with several similarities between galectin-1 and galectin-3 regarding the most highly associated pathways (Table 3). Both galectin-1 and galectin-3 were associated with proteins in interleukin and tumor necrosis factor-signaling. Galectin-1 was also associated with the more general pathway of the immune system, as well as neutrophil degranulation. In contrast, galectin-3 was associated with TP53-regulated cell death. Neither galectin presented significant associations with the general pathways of carbohydrate, lipid, or amino acid metabolism. However, both galectin-1 and galectin-3 were significantly associated with proteins in the triglyceride metabolism pathway (p = 0.015 and p = 0.005, respectively). While plasma galectin-1 and plasma galectin-3 levels were both associated with the proteins fatty acid binding protein (FABP) 4 and -5 in this pathway, only galectin-1 was also associated with FABP1, perilipin-1, and perilipin-3 (Table 4). Plasma levels of both galectins were also associated with the LDL-receptor (p < 0.001 for both). Furthermore, plasma galectin-1 but not plasma galectin-3 associated with proteins in the transcriptional regulation of the white adipocyte differentiation pathway (p = 0.006 and p = 0.100, respectively). Proteins from this pathway associated with galectin-1 were angiopoietin-like 4, perilipin-1, FABP4, leptin, and transforming growth factor (TGF)-β1. Plasma galectin-1 and plasma galectin-3 also presented significant association with each other, and with other galectins (galectin-1 with galectin-7 and -9, and galectin-3 with galectin-4 and -9) (data not shown).
Discussion
We thoroughly characterized the association patterns of galectin-1 and galectin-3 to established and exploratory markers of metabolic disease in a community-based cohort. This allowed us to identify clear distinctions and striking similarities between the two blood-based biomarkers in different aspects of metabolism. While plasma galectin-1 was associated with adipose tissue markers on both an anatomic and proteomic level, galectin-3 showed no such tendency. Conversely, the two galectins were sometimes associated with different insulin sensitivity markers. Galectin-1 was associated with C-peptide, TyG-index and the Matsuda index, while galectin-3 was associated with fasting insulin and TyG-index in the fully adjusted models. Both presented negative associations with fasting glucose, and positive associations with cholesterol, fatty acid, and triglyceride metabolism. Similar associations on the protein level reflected this, with associated proteins including FABP4 and -5, as well as the LDL-receptor. A potential metabolic role of these galectins is interesting, as galectin inhibitors are studied in clinical trials [1].
There was a clear distinction between the two galectins when comparing the association profiles and the Imiomics analysis for galectin-1 and galectin-3 on measures of obesity and adipose tissue distribution. Plasma levels of galectin-1 were closely associated with all adiposity variables, both in the subcutis and viscera. Ectopic fat deposition in the liver and pancreas were no longer significant after BMI adjustment, suggesting indirect associations secondary to BMI. Several studies have reported close associations between galectin-1 and adipose tissue measures [13, 14, 37], and studies in animal models suggest a role for galectin-1 in adipocyte handling of lipids [16, 17]. Several previously proposed mechanisms fit with the observations we find in the proteomic analysis, suggesting that galectin-1 may play a role in adipose tissue organization also in humans [17, 38]. It could be speculated that galectin-1 interacts with leptin, FABP1, -4 and -5, TGF-β1, and perilipin-1 and -3 to modulate whole body lipid storage as indicated by our measurements on BMI, body fat, and Imiomics. The absence of associations between circulating galectin-3 levels and adipose tissue deposition was unexpected, given that both galectins were associated with plasma levels of LDL-cholesterol, triglycerides and fatty acids as well as protein markers of lipid metabolism including the LDL-receptor, FABP4 and -5. However, the observational design does not allow for any conclusion regarding function of the galectins, and it is possible that these associations are mediated by unknown factors. It could also be that galectin-3 has a more prominent role in other metabolically active organs than the adipose tissue, such as the liver. This idea is currently explored as pharmacological galectin-3 inhibitors are under evaluation in clinical trials for the treatment of non-alcoholic steatohepatitis [39].
Several reports have previously indicated associations for galectin-1 with glucose and insulin, and a functional role is suggested in animal models [13, 14, 17]. Here, galectin-1 was associated with all glucose homeostasis variables except for end-OGTT glucose value before BMI adjustment. The closest associations were seen for C-peptide and the insulin resistance measures, HOMA, TyG-index and the Matsuda index, suggesting a role involving insulin resistance rather than glucose or insulin itself. As these associations were mitigated or lost after adjustments for BMI, the functional role of galectin-1 may lie in adipose tissue metabolism as suggested previously [16, 17]. The association with C-peptide aligns with a proposed role of galectin-1 on insulin release in the pancreas of mice [40]. On the contrary, plasma galectin-3 was not associated with C-peptide and pancreas function. However, in similarity with galectin-1, it was associated with TyG index, a marker of insulin resistance that is superior to HOMA-index in Nonalcoholic Fatty Liver Disease (NAFLD) [41]. Galectin-1 has previously been associated with an improved glucose uptake, independent of insulin secretion, which may explain the inverse association observed for both galectins with fasting glucose [42, 43]. This could also explain the lack of association with the 2-h glucose measurement. Fasting glucose levels are closely dependent on hepatic glucose production, regulated by the fasting insulin levels. Thus, a direct effect of the galectins on the hepatocyte is another possibility for the inverse association. Plasma galectin-3 was associated with TyG-index, but not with any other marker of insulin resistance. Several studies have previously found associations between galectin-3 and insulin resistance markers in experimental studies in animal models [10, 44]. The different associations for plasma galectin-1 and -3 with the various markers of insulin resistance may reflect involvement in different metabolic contexts, which should be validated in mechanistic studies [45].
Several proposed ligands are shared between galectin-1 and galectin-3, independently identified in separate studies [46, 47]. It has been argued that these interactions mediate cellular responses, although this remains to be definitively shown [5]. Our study measuring both galectins in the same cohort found similar association patterns between them and several lipid metabolites, as well as markers of lipid metabolism and inflammation, suggestively indicating an overlapping role for the two galectins in these processes. The similar associations with proteins in triglyceride metabolism and the LDL-receptor further support this. In spite of overlapping interaction profiles in vivo and in vitro [48], the global expression is somewhat different. Galectin-1 protein expression is highest in adipose tissue, muscle, and tissues present in females, while galectin-3 expression is highest in the gastrointestinal tract, lungs, skin, kidneys, and bone marrow (https://www.proteinatlas.org/, last accessed on 2022-02-15).
In the targeted metabolomics analysis, associations with cholesterol, fatty acid, and triglyceride markers were almost identical, with few exceptions including free-cholesterol and HDL-metabolites, where statistical significance was not matching. This lends further support for the possibility of overlapping functionalities between the two galectins. It was interesting to find similar associations with both LDL cholesterol and triglycerides for the galectins, as BMI is normally more closely associated with TG than with LDL. Nonetheless, both LDL and triglycerides are known to associate with abdominal fat deposition and a positive energy balance [49, 50]. This aligns with previous studies in galectin-1 deficient mice, and experiments using a galectin-3 specific inhibitor, which have reported that galectin-1 and galectin-3 may interact with the PPAR-γ pathway although in different tissues [11, 16]. Additionally, both galectin-1 and galectin-3 were associated with IL-10 and TNF signaling, pathways previously related to galectins [51,52,53,54] and with a role in obesity-related inflammation and lipid metabolism [55, 56].
In our non-targeted metabolomics analysis, the two galectins presented associations with metabolites in distinctly different pathways. Galectin-1-associated metabolites were related to histidine and cysteine metabolism, which both have a known role in galectin-1 function [57, 58]. Pentose and glucuronate interconversion and the TCA cycle pathways are related to carbohydrate metabolism, which may tie together with our observed associations with clinical variables. Pentose and glucuronate interconversions, histidine metabolism, and ascorbate and aldarate metabolism have previously been reported to be altered together in other inflammatory contexts [59, 60]. If galectin-1 and inflammation is linked through these metabolic pathways remains to be determined in future studies. Galectin-3 was related to sphingolipid metabolism, which may be explained by the reported capacity for galectin-3 to interact with glycosphingolipids, e.g., during endocytosis [61]. Sphingolipid metabolism and GPI-anchor biosynthesis pathways have previously been reported to be altered together in a study of a lipid-lowering drug on high-fat-fed mice [62]. These metabolic pathways may be related to our other observed associations between galectin-3 and lipid metabolism, including fatty acids, cholesterols, and FABP4 and -5.
Strengths and limitations
This study provides new data on how plasma galectin-1 and galectin-3 associate with variables from a comprehensive metabolic characterization in a population-based study. The combination of several different “omic” techniques, with measurements of both galectin-1 and galectin-3 within the same study, allows for a better understanding of similarities and differences between the two lectins on a whole-body level. There are also some limitations to consider in this study. The POEM cohort consists almost exclusively of white participants, and may not be generalizable to other ethnicities. The cross-sectional design does not allow for any conclusions on the direct contribution of galectin-1 and -3 to the studied profiles. We only stratified the Imiomics by sex, because of the sample size. However, the stratified analysis did not indicate any major difference between males and females, and all analyses were adjusted for sex to limit potential bias. The association between galectin-1 and adiposity also complicates the analysis of other variables related to obesity, as there is a risk in over-adjusting the linear models. As galectin-1 can be an agent in obesity released from the adipocytes to regulate metabolic actions, adjusting for BMI might introduce bias to the analysis. Therefore, we present associations with clinical variables before and after adjustment for BMI.
Conclusion
Taken together, we show that while galectin-1 and galectin-3 in plasma reveal distinctly different associations with obesity and adipose tissue distribution, they also present very similar associations with markers of glucose and lipid metabolism, including cholesterol, fatty acids, and triglycerides. Thus, we find that plasma galectin-1 and galectin-3 have overlapping metabolic associations but profiled toward different tissues. Functional studies are warranted to investigate the metabolic role of galectin-1 and galectin-3 in vitro and in vivo for validation of these results. This information may reveal if galectins hold future potential for treatment of metabolic diseases.
Data availability
The datasets analyzed during the current study are not publicly available due to restrictions in the ethical permission, but the data can be accessed through the corresponding author upon reasonable request and with permission of the POEM study steering committee.
References
Sethi A, Sanam S, Alvala R, Alvala M. An updated patent review of galectin-1 and galectin-3 inhibitors and their potential therapeutic applications (2016-present). Expert Opin Ther Pat. 2021;31:709–21.
Fryk E, Silva VRR, Jansson PA. Galectin-1 in obesity and type 2 diabetes. Metabolites. 2022;12:1–21.
Marino KV, Cagnoni AJ, Croci DO, Rabinovich GA. Targeting galectin-driven regulatory circuits in cancer and fibrosis. Nat Rev Drug Discov. 2023;22:295–316.
Brinchmann MF, Patel DM, Iversen MH. The role of galectins as modulators of metabolism and inflammation. Mediators Inflamm. 2018;2018:9186940.
Liu FT. Regulatory roles of galectins in the immune response. Int Arch Allergy Immunol. 2005;136:385–400.
Khalaji A, Amirkhani N, Sharifkashani S, Behnoush AH. Role of galectin-3 as a biomarker in obstructive sleep apnea: a systematic review and meta-analysis. Sleep Breath. 2023;27:2273–82.
Guo Y, Li L, Hu S. Circulating galectin-3 levels and diabetic nephropathy: a systematic review and meta-analysis. BMC Nephrol. 2023;24:163.
Imran TF, Shin HJ, Mathenge N, Wang F, Kim B, Joseph J, et al. Meta-analysis of the usefulness of plasma galectin-3 to predict the risk of mortality in patients with heart failure and in the general population. Am J Cardiol. 2017;119:57–64.
Deng Y, Jin H, Ning J, Cui D, Zhang M, Yang H. Elevated galectin-3 levels detected in women with hyperglycemia during early and mid-pregnancy antagonizes high glucose-induced trophoblast cells apoptosis via galectin-3/foxc1 pathway. Mol Med. 2023;29:115.
Li P, Liu S, Lu M, Bandyopadhyay G, Oh D, Imamura T, et al. Hematopoietic-derived galectin-3 causes cellular and systemic insulin resistance. Cell. 2016;167:973–84.e12.
Yu H, Yang F, Zhong W, Jiang X, Zhang F, Ji X, et al. Secretory galectin-3 promotes hepatic steatosis via regulation of the PPARgamma/CD36 signaling pathway. Cell Signal. 2021;84:110043.
Iacobini C, Menini S, Ricci C, Blasetti Fantauzzi C, Scipioni A, Salvi L, et al. Galectin-3 ablation protects mice from diet-induced NASH: a major scavenging role for galectin-3 in liver. J Hepatol. 2011;54:975–83.
Fryk E, Strindberg L, Lundqvist A, Sandstedt M, Bergfeldt L, Mattsson Hulten L, et al. Galectin-1 is inversely associated with type 2 diabetes independently of obesity—a SCAPIS pilot study. Metab Open. 2019;4:100017.
Fryk E, Sundelin JP, Strindberg L, Pereira MJ, Federici M, Marx N, et al. Microdialysis and proteomics of subcutaneous interstitial fluid reveals increased galectin-1 in type 2 diabetes patients. Metab Clin Exp. 2016;65:998–1006.
Drake I, Fryk E, Strindberg L, Lundqvist A, Rosengren AH, Groop L, et al. The role of circulating galectin-1 in type 2 diabetes and chronic kidney disease: evidence from cross-sectional, longitudinal and Mendelian randomisation analyses. Diabetologia. 2022;65:128–39.
Baek JH, Kim DH, Lee J, Kim SJ, Chun KH. Galectin-1 accelerates high-fat diet-induced obesity by activation of peroxisome proliferator-activated receptor gamma (PPARgamma) in mice. Cell Death Dis. 2021;12:66.
Mukherjee R, Kim SW, Park T, Choi MS, Yun JW. Targeted inhibition of galectin 1 by thiodigalactoside dramatically reduces body weight gain in diet-induced obese rats. Int J Obes. 2015;39:1349–58.
Mansour AA, Krautter F, Zhi Z, Iqbal AJ, Recio C. The interplay of galectins-1, -3, and -9 in the immune-inflammatory response underlying cardiovascular and metabolic disease. Cardiovasc Diabetol. 2022;21:253.
Lind L. Relationships between three different tests to evaluate endothelium-dependent vasodilation and cardiovascular risk in a middle-aged sample. J Hypertens. 2013;31:1570–4.
Lind L, Salihovic S, Sundstrom J, Elmstahl S, Hammar U, Dekkers K, et al. Metabolic profiling of obesity with and without the metabolic syndrome: a multisample evaluation. J Clin Endocrinol Metab. 2022;107:1337–45.
Lind L, Sundstrom J, Elmstahl S, Dekkers KF, Smith JG, Engstrom G, et al. The metabolomic profile associated with clustering of cardiovascular risk factors—a multi-sample evaluation. PLoS ONE. 2022;17:e0274701.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care. 1999;22:1462–70.
da Silva A, Caldas APS, Rocha D, Bressan J. Triglyceride-glucose index predicts independently type 2 diabetes mellitus risk: a systematic review and meta-analysis of cohort studies. Prim Care Diabetes. 2020;14:584–93.
Khalaji A, Behnoush AH, Khanmohammadi S, Ghanbari Mardasi K, Sharifkashani S, Sahebkar A, et al. Triglyceride-glucose index and heart failure: a systematic review and meta-analysis. Cardiovasc Diabetol. 2023;22:244.
Tahapary DL, Pratisthita LB, Fitri NA, Marcella C, Wafa S, Kurniawan F, et al. Challenges in the diagnosis of insulin resistance: focusing on the role of HOMA-IR and tryglyceride/glucose index. Diabetes Metab Syndr. 2022;16:102581.
Lundberg M, Eriksson A, Tran B, Assarsson E, Fredriksson S. Homogeneous antibody-based proximity extension assays provide sensitive and specific detection of low-abundant proteins in human blood. Nucleic Acids Res. 2011;39:e102.
Toombs RJ, Ducher G, Shepherd JA, De Souza MJ. The impact of recent technological advances on the trueness and precision of DXA to assess body composition. Obesity. 2012;20:30–9.
Strand R, Kullberg J, Ahlstrom H, Lind L. Relationships between plasma levels and six proinflammatory interleukins and body composition using a new magnetic resonance imaging voxel-based technique. Cytokine X. 2021;3:100050.
Lind L, Strand R, Michaelsson K, Ahlstrom H, Kullberg J. Voxel-wise study of cohort associations in whole-body MRI: application in metabolic syndrome and its components. Radiology. 2020;294:559–67.
Langner T, Strand R, Ahlstrom H, Kullberg J. Large-scale biometry with interpretable neural network regression on UK Biobank body MRI. Sci Rep. 2020;10:17752.
Jelenkovic A, Bogl LH, Rose RJ, Kangas AJ, Soininen P, Ala-Korpela M, et al. Association between serum fatty acids and lipoprotein subclass profile in healthy young adults: exploring common genetic and environmental factors. Atherosclerosis. 2014;233:394–402.
Kettunen J, Tukiainen T, Sarin AP, Ortega-Alonso A, Tikkanen E, Lyytikainen LP, et al. Genome-wide association study identifies multiple loci influencing human serum metabolite levels. Nat Genet. 2012;44:269–76.
Soininen P, Kangas AJ, Wurtz P, Tukiainen T, Tynkkynen T, Laatikainen R, et al. High-throughput serum NMR metabonomics for cost-effective holistic studies on systemic metabolism. Analyst. 2009;134:1781–5.
Assarsson E, Lundberg M, Holmquist G, Bjorkesten J, Thorsen SB, Ekman D, et al. Homogenous 96-plex PEA immunoassay exhibiting high sensitivity, specificity, and excellent scalability. PLoS ONE. 2014;9:e95192.
Gillespie M, Jassal B, Stephan R, Milacic M, Rothfels K, Senff-Ribeiro A, et al. The reactome pathway knowledgebase 2022. Nucleic Acids Res. 2022;50:D687–92.
Roumans NJT, Vink RG, Bouwman FG, Fazelzadeh P, van Baak MA, Mariman ECM. Weight loss-induced cellular stress in subcutaneous adipose tissue and the risk for weight regain in overweight and obese adults. Int J Obes. 2017;41:894–901.
Rhodes DH, Pini M, Castellanos KJ, Montero-Melendez T, Cooper D, Perretti M, et al. Adipose tissue-specific modulation of galectin expression in lean and obese mice: evidence for regulatory function. Obesity. 2013;21:310–9.
Al Attar A, Antaramian A, Noureddin M. Review of galectin-3 inhibitors in the treatment of nonalcoholic steatohepatitis. Expert Rev Clin Pharm. 2021;14:457–64.
Sundblad V, Garcia-Tornadu IA, Ornstein AM, Martinez Allo VC, Lorenzo R, Gatto SG, et al. Galectin-1 impacts on glucose homeostasis by modulating pancreatic insulin release. Glycobiology. 2021;31:908–15.
Lee SB, Kim MK, Kang S, Park K, Kim JH, Baik SJ, et al. Triglyceride glucose index is superior to the homeostasis model assessment of insulin resistance for predicting nonalcoholic fatty liver disease in Korean adults. Endocrinol Metab. 2019;34:179–86.
Chen X, Yu C, Liu X, Liu B, Wu X, Wu J, et al. Intracellular galectin-3 is a lipopolysaccharide sensor that promotes glycolysis through mTORC1 activation. Nat Commun. 2022;13:7578.
Lee MY, Han HJ. Galectin-1 upregulates glucose transporter-1 expression level via protein kinase C, phosphoinositol-3 kinase, and mammalian target of rapamycin pathways in mouse embryonic stem cells. Int J Biochem Cell Biol. 2008;40:2421–30.
Menini S, Iacobini C, Blasetti Fantauzzi C, Pesce CM, Pugliese G. Role of galectin-3 in obesity and impaired glucose homeostasis. Oxid Med Cell Longev. 2016;2016:9618092.
van der Aa MP, Knibbe CA, Boer A, van der Vorst MM. Definition of insulin resistance affects prevalence rate in pediatric patients: a systematic review and call for consensus. J Pediatr Endocrinol Metab. 2017;30:123–31.
Jouve N, Despoix N, Espeli M, Gauthier L, Cypowyj S, Fallague K, et al. The involvement of CD146 and its novel ligand Galectin-1 in apoptotic regulation of endothelial cells. J Biol Chem. 2013;288:2571–9.
Zhang Z, Zheng Y, Wang H, Zhou Y, Tai G. CD146 interacts with galectin-3 to mediate endothelial cell migration. FEBS Lett. 2018;592:1817–28.
Blanchard H, Bum-Erdene K, Bohari MH, Yu X. Galectin-1 inhibitors and their potential therapeutic applications: a patent review. Expert Opin Ther Pat. 2016;26:537–54.
Ernersson A, Nystrom FH, Lindstrom T. Long-term increase of fat mass after a four week intervention with fast food based hyper-alimentation and limitation of physical activity. Nutr Metab. 2010;7:68.
Haarbo J, Hassager C, Riis BJ, Christiansen C. Relation of body fat distribution to serum lipids and lipoproteins in elderly women. Atherosclerosis. 1989;80:57–62.
van der Leij J, van den Berg A, Harms G, Eschbach H, Vos H, Zwiers P, et al. Strongly enhanced IL-10 production using stable galectin-1 homodimers. Mol Immunol. 2007;44:506–13.
Shirakawa K, Endo J, Kataoka M, Katsumata Y, Yoshida N, Yamamoto T, et al. IL (Interleukin)-10-STAT3-galectin-3 axis is essential for osteopontin-producing reparative macrophage polarization after myocardial infarction. Circulation. 2018;138:2021–35.
Udomsinprasert W, Ungsudechachai T, Wunthong S, Yuttanarad S, Jittikoon J, Honsawek S. Effect of galectin-3 on synovial inflammation in knee osteoarthritis via stimulating phosphatidylinositol-3-kinase/Akt pathway. Int Immunopharmacol. 2023;122:110673.
Fryk E, Wilsson A, Tompa A, Jansson PA, Faresjo M. Galectin-1 correlates with inflammatory markers and T regulatory cells in children with type 1 diabetes and/or celiac disease. Clin Exp Immunol. 2024;215:240–50.
Subramanian N, Tavira B, Hofwimmer K, Gutsmann B, Massier L, Abildgaard J, et al. Sex-specific regulation of IL-10 production in human adipose tissue in obesity. Front Endocrinol. 2022;13:996954.
Xu H, Hirosumi J, Uysal KT, Guler AD, Hotamisligil GS. Exclusive action of transmembrane TNF alpha in adipose tissue leads to reduced adipose mass and local but not systemic insulin resistance. Endocrinology. 2002;143:1502–11.
Hiramatsu H, Takeuchi K, Takeuchi H. Involvement of histidine residues in the pH-dependent beta-galactoside binding activity of human galectin-1. Biochemistry. 2013;52:2371–80.
Guardia CM, Caramelo JJ, Trujillo M, Mendez-Huergo SP, Radi R, Estrin DA, et al. Structural basis of redox-dependent modulation of galectin-1 dynamics and function. Glycobiology. 2014;24:428–41.
Chang H, Liu Q, Bai WF, Bai YC, Jia XY, Gao C, et al. Protective effects of Amygdalus mongolica on rats with renal fibrosis based on serum metabolomics. J Ethnopharmacol. 2020;257:112858.
Liu Y, Wang J, Guan X, Yu D, Huangfu M, Dou T, et al. Mogroside V reduce OVA-induced pulmonary inflammation based on lung and serum metabolomics. Phytomedicine. 2021;91:153682.
Lakshminarayan R, Wunder C, Becken U, Howes MT, Benzing C, Arumugam S, et al. Galectin-3 drives glycosphingolipid-dependent biogenesis of clathrin-independent carriers. Nat Cell Biol. 2014;16:595–606.
Ren J, Fang H, Yang L, Sun H, Song H, Yan G, et al. Fecal metabolomics analysis for deciphering the lipid-lowering effect of Qizhi capsule on high-fat feed induced hyperlipidemia. J Ethnopharmacol. 2023;308:116270.
Acknowledgements
We thank everyone in the POEM cohort for their contribution in this study.
Funding
Swedish Research Council [2022-01011, PAJ; 2016-01040, 2019-04756, JK], the Swedish Diabetes Foundation [DIA2021-631, PAJ], the state under the agreement between the Swedish government and the county councils, the ALF-agreement [2018-74560, PAJ; ALFGBG-935061, EF], the Novo Nordisk Foundation [NNF17OC0027458, PAJ], Sahlgrenska University Hospital funds [SU-971316, SU-984616, EF], Gothenburg Society of Medicine through Fred G and Emma E Kanolds stiftelse, John o Asta Falkmans fond, Therese Sandwalls fond & Vera och Hans Albrechtsons stiftelse [GLS-973024, GLS-985243, EF], R&D Centre Gothenburg and Södra Bohuslän (EF) and Swedish Heart-Lung Foundation [20220129, HA]. Open access funding provided by University of Gothenburg.
Author information
Authors and Affiliations
Contributions
EF, LL, and PAJ conceptualized and designed the study. VS and LS analyzed and interpreted the galectin-1 measurements. LL performed the statistical analysis. EF performed pathway analysis and formatted figures and tables and JK, HA and RS performed the imaging analysis. KM performed DXA-based body composition analysis. EF, JK, LL, and PAJ reviewed the data and wrote the first draft of the manuscript. All authors revised the manuscript critically for important intellectual content and gave final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Informed written consent was obtained from all participants before entering the POEM study and the Institutional Review Board in Uppsala, Sweden, approved the studies (Dnr 2009/057). All investigations were performed according to the Declaration of Helsinki.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fryk, E., Rodrigues Silva, V.R., Strindberg, L. et al. Metabolic profiling of galectin-1 and galectin-3: a cross-sectional, multi-omics, association study. Int J Obes (2024). https://doi.org/10.1038/s41366-024-01543-1
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41366-024-01543-1
- Springer Nature Limited