Abstract
As a crucial arm of innate immunity, the complement cascade (ComC) is involved both in mobilization of normal hematopoietic stem/progenitor cells (HSPCs) from bone marrow (BM) into peripheral blood and in their homing to BM. Despite the fact that ComC cleavage fragments alone do not chemoattract normal HSPCs, we found that leukemia cell lines as well as clonogenic blasts from chronic myeloid leukemia and acute myeloid leukemia patients respond robustly to C3 and C5 cleavage fragments by chemotaxis and increased adhesion. This finding was supported by the detection of C3a and C5a receptors in cells from human malignant hematopoietic cell lines and patient blasts at the mRNA (reverse transcriptase-polymerase chain reaction) and protein level (fluorescence-activated cell sorting), and by the demonstration that these receptors respond to stimulation by C3a and C5a by phosphorylation of p42/44 and p38 mitogen-activated protein kinases (MAPK), and protein kinase B (PKB/AKT). We also found that inducible heme oxygenase 1 (HO-1) is a negative regulator of ComC-mediated trafficking of leukemic cells, and that stimulation of leukemic cells by C3 or C5 cleavage fragments activates p38 MAPK, which downregulates HO-1 expression, rendering cells more mobile. We conclude that activation of the ComC in leukemia/lymphoma patients (for example, as a result of accompanying infections) enhances the motility of malignant cells and contributes to their spread in a p38 MAPK–HO-1-dependent manner. Therefore, inhibition of p38 MAPK or upregulation of HO-1 by small-molecule modulators would have a beneficial effect on ameliorating cell migration-mediated expansion of leukemia/lymphoma cells when the ComC becomes activated.
Similar content being viewed by others
Introduction
The complement cascade (ComC) is a crucial element of innate immunity and is involved in several processes related to fighting infection.1 This developmentally ancient system of zymogens, activated in a hierarchical proteolytic cascade, shows multiple effects.2, 3 For instance, ComC cleavage fragments, in addition to their immunological functions, have been reported to modulate stem cell migration during organogenesis.1, 4, 5 On the other hand, evidence has accumulated that the C3 and C5 cleavage fragments (C3a and C5a, respectively) orchestrate the egress of hematopoietic stem progenitor cells (HSPCs) from bone marrow (BM) into peripheral blood (PB) and their homing after transplantation.6, 7, 8 This function is also retained by the derivatives of C3a and C5a, desArgC3a and desArgC5a, respectively, which are the products of caboxypeptidase B.1 However, these pro-mobilization and pro-homing effects are not related directly to the chemoattraction of HSPCs,6, 7, 8, 9 but rather indirectly due to the induction of a proteolytic10, 11, 12, 13, 14, 15, 16 and lipolytic17 microenvironment in BM; the chemoattraction of granulocytes and monocytes that pave the way for HSPCs to cross the BM–sinusoid endothelium barrier;9 and by increasing the level of chemotactic factors in blood plasma. Thus, despite the fact that normal human HSPCs express C5a receptor (C5aR; CD88) and respond to stimulation by C3a, surprisingly, they do not show spontaneous chemotaxis in response to complement cleavage fragments.6, 7, 8, 9, 10, 11
Evidence has accumulated that the ComC has a role in the pathogenesis of several solid tumors by modifying their growth, affecting their metastatic potential and response to therapeutics.17, 18, 19 For example, the C1q receptor has been reported to be a key regulator for lamellipodia formation during cancer cell migration and metastasis.20 On the other hand, overexpression of the membrane complement regulatory protein CD59 is a prognostic biomarker for poor outcomes in breast cancer patients.21 Moreover, enhanced expression of C5aR correlates with enhanced metastatic potential and poor survival in non-small cell lung cancer,22 nasopharyngeal carcinoma,23 renal carcinoma24 and ovarian cancer.25 These latter effects are related to the C5a interaction with the C5aR expressed on tumor cells, which is involved in tumor growth and metastasis.26, 27, 28
In contrast to solid tumors, there is relatively little evidence concerning ComC involvement in leukemia. Although the expression of functional C3aR and C5aR receptors has been reported in U937 and HL-60 cells,29, 30, 31, 32, 33, 34 more extensive data on leukemic cell lines and primary patient samples are lacking.
To fill in this knowledge gap, we asked whether human leukemia cell lines and primary patient leukemic blasts express functional C3 and C5 cleavage-fragment receptors (C3aR and C5aR, respectively) and whether activation of the ComC and release of C3a and C5a anaphylatoxins affects the biology of leukemic cells. To address these questions, we employed several established human myeloid and lymphoma cell lines and purified CD33+ blasts from leukemia patients. We evaluated the effect of C3a and C5a on proliferation, survival, migration and adhesion. As the activation of the ComC is negatively regulated by heme oxygenase 1 (HO-1),35 and the ComC may downregulate HO-1,36, 37 we tested the involvement of the C3a/C5a–p38 mitogen-activated protein kinases (MAPK)–HO-1 signaling axis in these phenomena.
We concluded that activation of the ComC in leukemia/lymphoma patients (for example, as the result of accompanying infections) and release of C3 and C5 cleavage fragments enhances the motility of malignant cells in a p38 MAPK–HO-1-dependent manner and may contribute to their spread. Therefore, inhibition of p38 MAPK or upregulation of HO-1 could have a beneficial effect on decreasing the risk of expansion of leukemia/lymphoma cells when the ComC becomes activated, as seen, for example, during infections or after chemotherapy.
Materials and methods
Human leukemia cell lines and patient samples
We used twelve human malignant hematopoietic cell lines of various lineages (ATCC), including seven myeloid (HEL, K-562, THP-1, U937, KG-1a, HL-60, DAMI) and five lymphoid (DAUDI, RAJI, NALM-6, JURKAT, MOLT4) cell lines. All cell lines were cultured in Roswell Park Memorial Institute (RPMI) 1640 maedium containing l-glutamine (GE Healthcare, South Logan, UT, USA), 10% heat-inactivated fetal bovine serum (FBS; Seradigm, Radnor, PA, USA), 100 units/ml penicillin and 10 μg/ml streptomycin (Corning Costar, Corning, NY, USA), and cultured in a humidified atmosphere of 5% CO2 at 37 °C, with an exchange of medium every 48 h.
Ten patients with recently diagnosed acute myeloid leukemia (AML) (n=6) and chronic myeloid leukemia (CML) (n=4) were obtained for this study according to Institutional IRB guidelines. Ethylenediaminetetraacetic acid-anticoagulated whole blood was obtained from these patients, and peripheral blood mononuclear cells (PB-MNCs) were immediately separated by density-gradient centrifugation using Histopaque 1077 medium (Sigma-Aldrich, St Louis, MO, USA).
Reverse transcriptase-polymerase chain reaction (RT-PCR)
Total RNA was extracted and purified from cells using the RNeasy Mini kit (Qiagen Inc., Valencia, CA, USA) after treatment with DNase I (Qiagen Inc.) and reverse-transcribed into cDNA as previously described.36 The sequence-specific primers employed for amplification were as follows: human complement component 3a receptor 1 (hC3aR1; sense, 5′-agaaagacagccaccaccacg-3′; antisense, 5′-gccgcctggagaaatgaatgatagg-3′); human complement component 5a receptor 1 (hC5AR1; sense, 5′-accttcgatcctcggggagc-3′; antisense, 5′-gcgtacatgttgagcaggat-3′); human C5a receptor-like 2 (hC5L2; sense, 5′-ggattacagcgacctctcgg-3′; antisense, 5′-gcagagacaaacagcacagc-3′). Samples without template controls and reverse transcriptase were used in each run. All primers were designed using the NCBI/Primer-Blast program, and at least one primer in each pair included an exon–intron boundary. Afterwards, all PCR products were analyzed by 2% agarose gel electrophoresis.
Quantitative real-time PCR (RT-qPCR)
Cells were stimulated in vitro with C3a, C5a or SDF-1 after pretreatment with or without SB203580, a p38 MAPK inhibitor (20 μmol/l; Selleckchem, Houston, TX, USA). The purified RNA was reverse-transcribed with MultiScribe Reverse Transcriptase, oligo(dT), and a random hexamer primer mix (all from Applied Biosystems Life Technologies, CA, USA). Quantitative evaluation of the target gene was then performed by using an ABI Prism 7500 sequence detection system (Applied Biosystems Life Technologies) with Power SYBR Green PCR Master Mix reagent and specific primers (hHO-1; sense, 5′-gggtgatagaagaggccaagact-3′; antisense, 5′-agctcctgcaactcctcaaga-3′). The PCR cycling conditions were 95 °C (15 s), 40 cycles at 95 °C (15 s) and 60 °C (1 min). According to melting point analysis, only one PCR product was amplified under these conditions. The relative quantity of a target gene, normalized to the β2-microglobulin gene as the endogenous control and relative to a calibrator, was expressed as 2–ΔΔCt (fold difference).
Flow cytometry analysis
The expression of C3aR1 and C5aR1 receptors on the surface of malignant hematopoietic cells was analyzed by fluorescence-activated cell sorting (FACS). Cells (5 × 105 cells per test) were washed first and then stained with allophycocyanin-labeled anti-human C3AR1 (clone no. hC3aRZ8) and phycoerythrin-labeled anti-human CD88 (also known as C5aR1, clone no. S5/1) monoclonal antibodies (mAbs) for 30 min in phosphate-buffered saline (PBS; Ca and Mg free), supplemented with 2% FBS at 4 °C. All antibodies were purchased from Biolegend (San Diego, CA, USA). In all experiments, an isotype-matched immunoglobulin was used as a control for each mAb. Cells were washed, and the staining analysis was immediately performed on an LSR II flow cytometer using BD FACSDiva version 6.1.1 software (BD Bioscience, San Jose, CA, USA) as described in the past.36
Transwell migration assay
Quiescent cells were seeded (1 × 104 cells per well) onto the upper chambers of 24-well Transwell inserts with polycarbonate membranes (Corning Costar). The lower Boyden chambers received different concentrations of recombinant human complement proteins (C3a, C5a and desArgC5) in RPMI medium with 0.5% BSA (650 μl). All were purchased from Millipore (Billerica, MA, USA). In some experiments, stromal-derived factor 1 (SDF-1, 10 ng/ml; PeproTech, Rocky Hill, NJ, USA) plus C3a was added to the lower chamber to monitor their priming effect on the migration of malignant hematopoietic cells, and the migrated cells were collected and scored using the FACS analysis. The results are presented as a chemotactic ratio (the number of cells that migrated toward the medium containing C3a and/or SDF-1, C5a or desArgC5 divided by the number of cells that migrated toward the medium alone × 100). In other experiments, quiescent U937 and KG-1a hematopoietic cells were first incubated with SB203580 (20 μmol/l) for 6 h in serum-free medium. The cells were then washed and seeded onto the upper inserts, and their Transwell migration toward C3a, C5a or SDF-1 was evaluated after 3 h incubation. To analyze whether the increase in motility of malignant hematopoietic cell lines stimulated with C3a and C5a was the result of a directional (chemotactic) and/or a random (chemokinetic) response, we performed a checkerboard assay in which C3a (1 μg/ml), and C5a (140 ng/ml) proteins were added at the same time into the upper and the lower Transwell chambers.
Adhesion of malignant hematopoietic cells to fibronectin
Cells were made quiescent for 5 h in RPMI 1640 medium with 0.5% BSA in a humidified atmosphere of 5% CO2 at 37 °C. Next, the leukemia cells were cultured in RPMI 1640 medium with 0.5% BSA alone, or with C3a and/or SDF-1, C5a or desArgC5 proteins at low and high concentrations. Cells (3 × 103 cells per well) were then added directly and allowed to adhere to the fibronectin-coated wells in 96-well plates at 37 °C as we previously outlined.36
Signal transduction studies
To analyze the functionality of these complement receptors (C3aR, C5aR), quiescent cells were stimulated with RPMI 1640 medium with 0.5% BSA alone, C3a (1 μg/ml), C5a (140 ng/ml), desArgC5a (140 ng/ml), C3a plus SDF-1 (10 ng/ml) or SDF-1 alone (300 ng/ml) for 5 min at 37 °C. Cells were also pretreated with SB203580 for 6 h in serum-free RPMI medium at 37 °C and afterwards exposed to C3a, C5a or SDF-1 at the indicated concentrations for 5 min at 37 °C. The protein lysates were extracted and measured as described before,36 the adjusted extracted proteins (20 μg per each sample) were then separated on a 4–12% SDS–PAGE gel, and the fractionated proteins were transferred to a PVDF membrane (Bio-Rad). All membranes were blocked with 2.5% BSA. Phosphorylation of the intracellular kinase p44/42 mitogen-activated protein kinase (p42/44 MAPK), p38 MAPK and protein kinase B (PKB/AKT) was detected by incubating the membranes overnight at 4 °C with phosphospecific anti-p-p42/44 MAPK (clone no. 9101, diluted 1:1000), anti-p-AKT (Ser473; clone no. 9271, diluted 1:1000) rabbit polyclonal antibodies and anti-p-p38 MAPK (Thr180/Thr182; clone no. 9216, diluted 1:2000) mouse monoclonal antibodies (Cell Signaling, Danvers, MA, USA). Next, the membranes were incubated with horseradish peroxidase (HRP)-conjugated goat anti-rabbit or anti-mouse IgG secondary antibodies (Santa Cruz Biotech, Santa Cruz, CA, USA, 1:5000). To confirm equal protein loading in all lanes, the blots were stripped using stripping buffer (Thermo Scientific) and then reprobed with appropriate anti-rabbit p42/44 MAPK (clone no. 9102), anti-rabbit p38 MAPK (clone no. 9212) and anti-rabbit PKB/AKT (clone no. 9272) antibodies (all from Cell Signaling). Enhanced chemiluminescence reagent (Amersham Life Sciences, Amersham, UK) and film (Hyperfilm, Amersham Life Sciences) were used for band visualization using an automatic film processor with fresh warm developer and fixer solutions.
Detection of HO-1 by western blotting
Cells were cultured with C3a (1 μg/ml), C5a (140 ng/ml) or SDF-1 (300 ng/ml) in serum-free RPMI 1640 medium for 6 h at 37 °C. U937 and KG-1a hematopoietic cells were pretreated first with SB203580 for 6 h in serum-free medium, and after washing and replacement of the medium, the cells were then exposed to C3a, C5a or SDF-1 for a further 6 h at the indicated concentrations. The detection of HO-1 protein by western blotting has been performed as described by us by employing rabbit anti-HO-1 polyclonal antibody (Enzo Life Sciences, Farmingdale, NY, USA; diluted 1:1000).43
HO-1 overexpression and short hairpin RNA-mediated knockdown
HO-1-upregulated and HO-1-knockdown hematopoietic cell lines were created as described in our recently published paper.43 In brief, the cells were electroporated, either with a human HO-1 expression vector under the control of a CMV promoter (pCMV6-HO-1, vector SC320297; Origene, Rockville, MD, USA) or with an empty control vector containing CMV-driven eGFP (pEGFP-C2; Clontech Laboratories, Mountain View, CA, USA). After electroporation, both pCMV-hHO-1- and pEGFP-nucleofected cells were subjected to an antibiotic-mediated selection using G418 (800–2000 μg/ml, Life Technologies). In shRNA-mediated HO-1 knockdown experiments, cells were electroporated with either 15 μg of a Mission shRNA construct targeting human HO-1 (TRCN0000290436; Sigma-Aldrich) or a non-targeted shRNA control (SHC016; Sigma-Aldrich). After RNA interference, the cells underwent antibiotic-mediated selection using puromycin (2–5 μg/ml) 48 h after electroporation.
Xenotransplantation in immunodeficient mice
The care and use of mice in the present study was carried out in accordance with the guidelines provided by the Institutional Animal Care and Use Committee of the University of Louisville, which conform to the Guide for Care and Use of Laboratory Animals (Department of Health and Human Services, NIH publication no. 86-23). Human HO-1-overexpressing (RAJI-pCMV6-hHO-1) and knockdown (RAJI-shHO-1) hematopoietic cell lines and their respective control counterparts, RAJI-pEGFP-control and RAJI-shRNA cells, were prepared for in vivo transplantation (10 × 105 per mouse). On the other hand, before in vivo transplantation, non-transfected U937 cells (10 × 105 per mouse) were treated ex vivo for 6 h with C3a (1 μg/ml), C5a (140 ng/ml) or vehicle only as a control. In parallel, some cells were also exposed to a small-molecule HO-1 inhibitor (tin protoporphryin IX dichloride [SnPP], TOCRIS Bioscience, 50 μmol/l), HO-1 activator (cobalt protoporphryin IX chloride [CoPP], TOCRIS Bioscience, 50 μmol/l) or vehicle alone for 2 h. All treated cells were then washed and transplanted into severe combined immunodeficient (SCID)-beige inbred mice (n=3 per group), which were initially irradiated with 350 cGy at 24 h before transplantation. At 24 h post transplantation, BMs, livers and lungs were collected, and the presence of metastasized cancer cells (that is, murine–human chimeras) was evaluated as previously described.36
Sorting of CD33+ blasts and RT-PCR
CD33+ blast isolation was performed from both AML and CML PB-MNC patient samples using magnetic cell sorting (MACS, Miltenyi Biotec), according to the manufacturer’s instructions as described by us in the past36 and mRNAs were purified from CD33+ cells enriched in AML and CML blast patient primary cells using the RNeasy Micro kit (Qiagen). For cDNA synthesis, 10 μg of mRNA from each sample was reverse-transcribed using a high-capacity cDNA reverse transcription kit (Life Technologies). To evaluate the expression of C3a and C5a receptors, the amplification of synthesized cDNA fragments was performed using Amplitaq Gold polymerase (Applied Biosystem, Foster City, CA, USA) as described above. In parallel, the expression of these receptors was also assessed at the protein level for CD33+ blasts purified from AML and CML PB-MNC samples by FACS separation, as described above.
Chemotaxis and clonogenic assays
CD33+ blasts purified from primary human AML and CML patients were also subjected to transmigration assays in response to C3a, C5a and desArgC5a proteins in serum-free medium at the described concentrations and methods. At the same time, cell migration was also evaluated in response to an SDF-1 gradient or medium without stimulants. After a 3-h stimulation, the migrated cells were collected and plated with methylcellulose base medium and growth factors (GM-CSF (25 ng/ml) and IL-3 (10 ng/ml)). After 14 days of culture at 37 °C and 5% CO2 atmosphere, the numbers of granulocyte/macrophage colony-forming units were scored using an inverted microscope (Olympus, Center Valley, PA, USA).
Data analysis
Statistical analysis was carried out using GraphPad Prism 6 (GraphPad Software Inc., La Jolla, CA, USA) and Sigma software (Sigma Software Inc., San Jose, CA, USA). All data are presented as the mean±s.d. Statistical analysis of the data was done using one-way ANOVA and Tukey’s test for post hoc pairwise multiple comparison. In all analyses, P<0.05, P<0.01 and P<0.001 were considered significant.
Results
Functional C3a and C5a receptors are expressed on human leukemic cells
First, to address the role of the ComC in leukemia we evaluated expression of the C3a and C5a receptors (C3aR and C5aR, respectively) on established human myeloid and lymphoid cell lines by employing RT-PCR (Figure 1a) and FACS (Figure 1b). We found that all cell lines evaluated in our studies express mRNA for both receptors, except for K-562, which does not express C3aR, and DAMI and Jurkat cells, which do not express C5aR. At the same time, all cell lines employed in our experiments expressed a second non-signaling receptor, C5a-like receptor 2 (C5L2, Figure 1a). Moreover, the pattern of mRNA expression corresponded with the FACS results (Figure 1b).
Human malignant hematopoietic cell lines express functional complement anaphylatoxin receptors (C3aR, C5aR) and C5a receptor-like 2 (C5L2). (a) Expression of C3aR1, C5aR1 (also known as CD88) and C5L2 was detected in purified mRNA samples from various myeloid and lymphoid leukemia cell lines by RT-PCR. Samples containing only water instead of cDNA and samples without reverse transcriptase were used in each run as negative controls. Representative agarose gels of the RT-PCR amplicons are shown. (b) Flow cytometric analyses of C3aR1 and C5aR1 expression in the leukemia cell lines, and the representative histograms of C3aR1 and C5aR1 expression are shown. As shown here, the data obtained by FACS is consistent with the RT-PCR results. (c) The effect of recombinant human complement C3a, C5a and C5adesArg proteins on the phosphorylation of p42/44 MAPK and AKTser473 intracellular pathway proteins in both myeloid and lymphoid leukemia cell lines was analyzed by western blotting. These cells (2 × 106 cells per ml) were rendered quiescent for 5 h in RPMI medium containing 0.5% BSA at 37 °C, and afterwards the protein lysates were collected after 5 min of stimulation with C3a (1 μg/ml), C5a (140 ng/ml) or C5adesArg (140 ng/ml) proteins. The cells were also treated with C3a plus a low dose of SDF-1 (10 ng/ml), SDF-1 alone or only serum-free medium. The experiment was carried out twice with similar results, and representative blots are shown.
In the next step, we evaluated the functionality of C3aR and C5aR by studying the phosphorylation of p42/44 MAPK and PKB/AKT after stimulation with C3a and C5a (Figure 1c), and found that these receptors are functional. However, as expected based on the RT-PCR and FACS expression results, K-562 cells did not respond to C3a stimulation, and DAMI and Jurkat cells did not respond to stimulation by C5a and desArgC5a. We also observed, somewhat to our surprise, that Jurkat cells, which highly express C3aR, did not respond to stimulation by C3a. At the same time, in control studies, all of these CXCR4+ leukemia cell lines responded to SDF-1 stimulation.
Effect of C3 and C5 cleavage fragments on migration and adhesion of human leukemia cells
The biological responses of leukemia cell lines to C3 and C5 cleavage fragments were subsequently studied in a Transwell migration assay as well as in an assay for cell adhesion to fibronectin-coated plates (Figure 2). In our control experiments, SDF-1 at a high concentration (300 ng/ml) was employed as a positive control. Moreover, based on our previous finding that C3a may enhance the responsiveness of cells to a shallow SDF-1 gradient,6, 7, 8, 36 we also combined C3a with a low dose of SDF-1 (10 ng/ml) in some of our experiments.
Complement C3 and C5 cleavage fragments accelerate migration and adhesiveness of human leukemia cells to fibronectin. (a, c). Chemotaxis of malignant myeloid and lymphoid cells toward different concentrations of C3a (0.5–1 μg/ml), C5a (70–140 ng/ml) and C5adesArg (70–140 ng/ml) through Transwell membranes (8-μm pore size) was assessed. The priming effect of C3a on chemotaxis toward a low dose of SDF-1 was also tested by exposing the cells to C3a (500 ng/ml) plus SDF-1 (10 ng/ml) or C3a (1 μg/ml) plus SDF-1 (10 ng/ml). Before stimulation, cells were rendered quiescent in serum-free medium for 5 h at 37 °C. All leukemia cell lines employed (105 cells per 100 μl per insert) were also evaluated for migration in response to a high dose of SDF-1 (300 ng/ml) or toward RPMI medium containing 0.5% BSA as a positive or negative control, respectively. Three hours post stimulation, loaded inserts were carefully removed, and the migrated cells were afterwards collected and counted by the FACS analysis. Data are extracted from at least triplicate samples in three independent experiments. (b, d) Adhesion of myeloid and lymphoid leukemia cell lines to fibronectin-coated surfaces in response to C3a (0.5–1 μg/ml), C5a (70–140 ng/ml), C5adesArg (70–140 ng/ml), C3a (500 ng/ml) plus a low dose of SDF-1 (10 ng/ml) or C3a (1 μg/ml) plus a low dose of SDF-1 (10 ng/ml). Quiescent cells (3000 cells per 100 μl) were stimulated in medium with 0.5% BSA for 5 min at 37 °C. After the non-adherent cells were removed via three consecutive washes with PBS, the number of adherent cells was directly scored by the microscopic analysis. Cells were also evaluated for adhesion in response to a high dose of SDF-1 (300 ng/ml) or to RPMI medium containing 0.5% BSA as a positive or negative control, respectively. Data were extracted from at least triplicate samples in three independent experiments. In all experiments, the negative control values are normalized to 100%. Data are displayed as means±s.d., with a statistical significance *P<0.05 and **P<0.01 in both migration and adhesion assays between cells exposed to anaphylatoxins and control (unstimulated) cells. (e) The increase in motility of malignant hematopoietic cell lines toward C3a and C5a cleavage fragments is the result of a random chemokinetic response. A checkerboard assay was performed in which C3a (1 μg/ml) and C5a (140 ng/ml) proteins were added at the same time into the upper and the lower Transwell chambers. Data are displayed as means±s.d., with a statistical significance *P<0.05 versus control (unstimulated) cells.
As shown in Figures 2a and b, the response of leukemic cell lines in both chemotaxis and adhesion assays corresponded with receptor expression (Figures 1a and b) and activation of intracellular signaling pathways after stimulation by C3a or C5a (Figure 1c). The exception was the K-562 cell line, which does not express C3aR but responded by enhanced migration and adhesion to stimulation by C3a plus SDF-1. To explain this observation, the ‘priming effect’ of C3a on the responsiveness of cells to an SDF-1 gradient is not C3aR driven38 but depends on C3a-mediated promotion of membrane lipid raft formation.39 In this case, when incorporated into membrane lipid rafts, CXCR4 responds more robustly to an SDF-1 gradient.38, 39 Similarly as for C3a stimulation, we found that all cell lines that express C5aR responded to stimulation by C5a and desArgC5a (Figures 2c and d). Moreover, the effect of C3a and C5a cleavage on adhesion of the leukemic cells tested in our work to fibronectin-coated plates followed the pattern of C3a and C5a receptor expression (data not shown).
The motility of cells in response to a gradient of migration stimulatory factors may be the result of gradient-orchestrated unidirectional cell movement (chemotaxis) or random migration (chemokinesis).40 Therefore, we decided to test whether the effect of C3 and C5 cleavage fragments on the migration of human leukemic cell lines in a Transwell assay depends on directional cell chemotaxis or random chemokinetic motility. We found that chemokinesis is responsible for the enhanced migration of leukemic cells (Figure 2e).
Although C3 and C5 cleavage fragments were reported to stimulate proliferation of some solid cancer cell lines,20, 21, 22, 23, 41, 42 we did not observe any effect of C3a and C5a on proliferation of the human leukemic cell lines employed in our study (data not shown).
C3 and C5 cleavage fragments increase the migration of leukemic cells by downregulating the expression of heme oxygenase 1 (HO-1)
HO-1 is a negative regulator of ComC activation.35, 36, 37 Specifically, we recently reported that upregulation of HO-1 in human leukemic cell lines negatively regulates their migration, whereas downregulation of HO-1 has the opposite effect.43 To better understand this phenomenon, we stimulated U937 and KG-1a cells with C3a, C5a and SDF-1, and found that all of these pro-migratory factors downregulated the expression of HO-1 at the mRNA and protein level in leukemic cells (Figures 3a and b). At the same time, as expected, in U937 and KG-1a cells, C3a, C5a and SDF-1 upregulated the expression of p38 MAPK (Figure 3c), which negatively regulates HO-1 expression in these cells.44
Complement C3 and C5 cleavage fragments enhance migration of leukemic cells through phosphorylation of p38 MAPK-dependent downregulation of heme oxygenase 1 (HO-1). (a) RT-qPCR analysis of human HO-1 transcripts in mRNA samples purified from U937 (left) and KG-1a (right) cell lines cultured with C3a (1 μg/ml), C5a (140 ng/ml) or SDF-1 (300 ng/ml) in serum-free medium for 6 h at 37 °C. β2-microglobulin was used as an endogenous control. Samples containing only water instead of cDNA were used in each run as a negative control. Cells without any stimulation served as a control. *P<0.05 is considered statistically significant between cells exposed to anaphylatoxins or SDF-1 and unstimulated cells. (b) Western blot for human HO-1 in protein lysates collected from U937 (left) and KG-1a (right) cell lines (20 μg per sample). After incubation of cells with C3a, C5a or SDF-1 at the doses indicated above, protein was immediately extracted and later quantified using the Pierce BCA Protein Assay Kit (Thermo Scientific, Rockford, IL, USA) and Multimode Analysis Software (Beckman Coulter Inc, Fullerton CA, USA). In parallel, β-actin was also analyzed to ensure the equivalence of loading. Proteins extracted from cells cultured in only assay medium served as a control. (c) Western blot analysis for phospho-p38 MAPK in protein lysates collected from quiescent U937 (left) and KG-1a (right) cell lines. Cells were stimulated with 0.5% BSA in RPMI 1640 medium, C3a (1 μg/ml), C5a (140 ng/ml) or SDF-1 (300 ng/ml) for 5 min at 37 °C. Total p38 MAPK was also analyzed to ensure equal protein loading in each lane.
This result suggests that C3 and C5 cleavage fragments and SDF-1 enhance cell migration of leukemic cells in a p38 MAPK–HO-1-dependent manner.
Inhibition of p38 MAPK or upregulation of HO-1 inhibits migration of leukemic cells
As activation of the ComC and release of C3 and C5 cleavage fragments leads to downregulation of HO-1 in a p38 MAPK-dependent manner (Figure 3), strategies to consider for inhibiting the migration and spread of leukemic cells include (i) intracellular inhibiton of p38 MAPK and (ii) upregulation of HO-1 expression.
To address this issue, we first downregulated p38 MAPK in U937 and KG-1a cells by employing the specific small-molecule inhibitor SB203580, and in its presence, neither cell line responded with p38 MAPK activation after stimulation with C3a, C5a and SDF-1 (Figure 4a). As expected, downregulation of p38 MAPK resulted in upregulation of HO-1 in these cells (Figure 4b). Also as expected, SB203580 was a potent inhibitor of leukemic cell migration in response to C3a, C5a or SDF-1 gradients in Transwell chemotactic assays (Figure 4c).
Antagonism of p38 MAPK inhibits migration of leukemic cells by downregulation of HO-1. (a) Western blot analysis of phospho-p38 MAPK in protein lysates collected from quiescent U937 (top, left) and KG-1a (top, right) cell lines. Cells were pretreated with SB203580 (20 μmol/l) for 6 h at 37 °C in serum-free medium. Cells were afterwards washed with PBS and stimulated with 0.5% BSA in RPMI 1640 medium, C3a, C5a or SDF-1 for 5 min at 37 °C. Total p38 MAPK was also analyzed to confirm equal loading of protein in each lane. (b) In parallel, HO-1 expression was evaluated at both the mRNA (RT-qPCR) and protein (western blotting) levels in U937 (bottom, left) and KG-1a (bottom, right) cell lines. The mRNA samples and protein lysates were obtained after pretreatment first with SB203580 for 6 h and followed by washing with PBS and a further 6-h exposure in serum-free medium at 37 °C to C3a, C5a or SDF-1 gradients. In the two latter experiments, β2-microglobulin and β-actin were employed as endogenous controls, respectively. For RT-qPCR, samples containing only water instead of cDNA were used in each run as a negative control. Cells kept unstimulated (that is, in only serum-free medium) served as a negative control. *P<0.05 is considered significant versus the unstimulated (control) cells. (c) Chemotaxis of U937 (left) and KG-1a (right) cells was also assayed after inhibition of p38 MAPK by incubation of cells with SB203580 in RPMI 1640 medium with 0.5% BSA. Six hours later, the cells were then washed with PBS and evaluated for migration (105 cells per 100 μl per insert) toward medium alone, C3a (1 μg/ml), C5a (140 ng/ml) or SDF-1 (300 ng/ml). The loaded inserts were afterwards carefully removed, and the migrated cells were collected and counted by the FACS analysis 3 h after loading into the inserts. Data are extracted from at least triplicate samples in three independent experiments. Significance is indicated at *P<0.05, where P represents a statistical difference in migration between treated cells compared with untreated cells.
To better address the role of C3 and C5 cleavage fragments and HO-1 in the potential spread of leukemic cells, we performed complementary in vivo studies. In these experiments, U937 cells were exposed for 2 h to C3a, C5a, the HO-1 inhibitor SnPP and the HO-1 activator CoPP and injected intravenously 24 h after irradiation with 350 cGy into immunodeficient SCID mice. The mice were subsequently sacrificed 24 h after intravenous injection of leukemic cells, and the seeding of human malignant cells to BM, lung and liver was evaluated by real-time quantitative polymerase chain reaction (RQ-PCR) detection of human satellite DNA sequences, as described by us.36
As demonstrated in Figure 5a, exposure to C3a and C5a as well as the HO-1 inhibitor SnPP enhanced the spread of leukemic cells to murine organs, although having the opposite effect on HO-1 activation as CoPP. Similar effects of HO-1 upregulation or downregulation on the spread of leukemic cells in an in vivo immunodeficient SCID mouse model were confirmed in Raji cells in which HO-1 expression was stably up- or downregulated (Figure 5b).
Complement C3 and C5 cleavage fragments and downregulation or inhibition of HO-1 enhance metastasis, whereas upregulation or activation of HO-1 inhibits the metastasis of leukemic cells in vivo. (a) Detection of transplanted human U937 cells (10 × 105 per mouse) in the organs of irradiated (SCID)-beige inbred mice after in vivo transplantation. Pre-implantation, the cells were incubated ex vivo with vehicle only, C3a (1 μg/ml), or C5a (140 ng/ml) for 6 h and HO-1 activator (CoPP, 50 μmol/l) or HO-1 inhibitor (SnPP, 50 μmol/l) for 2 h. Under all conditions, serum-free medium was used. Human cells were detected in BM (top row), lung (middle row) and liver (bottom row) by the presence of human Alu sequences in purified genomic DNA samples according to RT-qPCR. (b) Evaluation of the spread of transplanted leukemic cells in vivo after up- and downregulation of HO-1. Human HO-1-overexpressing (RAJI-pCMV6-hHO-1) and knockdown (RAJI-shHO-1) hematopoietic cell lines and RAJI-pEGFP and RAJI-shRNA cells as control counterparts, respectively, were prepared for in vivo transplantation (10 × 105 per mouse). Twenty-four hours after cell transplantation into irradiated SCID mice the organs were collected, and detection and quantification of the human cells was then analyzed by RT-qPCR. For statistical comparisons, a one-way analysis of variance and a Tukey’s test for post hoc analysis were carried out, and means±s.d. are shown. Significance levels are indicated at P<0.05, P<0.01 and P<0.001 for comparison with untreated or control-transfected cells.
Human CML- and AML-derived CD33+ blasts express C5R and C3R and respond by chemotaxis and adhesion to stimulation by C3 and C5 cleavage fragments
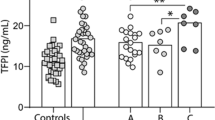
Finally, we evaluated the expression of C3aR and C5aR receptors on patient CD33+ blasts purified from CML and AML patients. Both receptors were expressed both at the mRNA (not shown) and protein levels (Figure 6a). Overall, according to the FACS analysis, C5aR and C3aR expression by human CD33+ CML blasts was 41±21 and 40±17%, respectively, and by human AML blasts was 56±15 and 28±17%, respectively.
Primary human leukemia CD33+ blasts express functional complement cascade (CC) receptors. Expression of C3a and C5a receptors was evaluated in purified PB CD33+ blast samples from chronic myeloid leukemia (CML, n=4) (a, top) cells and acute myeloid leukemia cells (AML, n=6) (a, bottom) cells by flow cytometry. Representative plots of sorted CD33+ CML and AML cells are shown. The components of the CC (C5a, C3a and desArgC5a) are chemoattractants for CFU-GM leukemia progenitors. Human CD33+ leukemia blasts purified from CML (n=4) (b, left) and AML (n=6) (b, right) patients. Transmigration of these primary CD33+ CML and AML blasts through Transwell membranes in response to C5a, C3a and desArgC5a at the indicated concentrations was analyzed. After magnetic separation, the CD33+ cells were resuspended in 0.5% BSA in RPMI 1640 medium. The effects of the CC components on migration of CD33+ leukemia cells were evaluated in RPMI medium containing 0.5% BSA. As a positive control, SDF-1 was used, whereas serum-free medium was used as a negative control. Next, the migrated cells were harvested and counted by the FACS analysis, and a clonogenic assay for CFU-GM was immediately performed on only migrated cells. Data are displayed as means±s.d., with a statistical significance compared with the control, *P<0.05 and **P<0.01.
More importantly, these receptors were functional, as CML and AML clonogenic progenitors responded similarly as cells from established leukemic cell lines by chemokinesis to C3a, C5a and desArgC5a gradients (Figure 6b). Interestingly, this responsiveness to C3 and C5 cleavage fragments was quite robust and comparable to high doses of SDF-1. In control experiments, normal BM- or PB-derived clonogenic progenitors as already reported by us in the past6, 8 did not respond by enhanced migration after exposure to C3a or C5a (data not shown).
Discussion
The most important finding of this study is that the cleavage fragments (C3a and C5a) of the activated ComC products C3 and C5, respectively, are potent chemokinetic factors for several human leukemic cell lines. This effect, in contrast to normal clonogenic HSPCs, was also observed for human clonogenic AML and CML blasts. This finding indicates that the responsiveness of clonogenic leukemic HSPCs to C3a and C5a is the result of their malignant transformation.
It is well known that the C3a and C5a anaphylatoxins promote migration of differentiated hematopoietic cells, including granulocytes, monocytes, lymphocytes and NK cells.1, 45, 46, 47, 48, 49 Interestingly, despite the fact that normal CD34+ HSPCs express C5aR and some are also C3aR+, these cells do not show a migratory response to C3a, C5a or their carboxypeptidase-generated derivatives desArgC3a and desArgC5a.6, 7, 8, 9 However, activation of the ComC and generation of C3 and C5 cleavage fragments in the BM microenvironment is required to ensure proper egress of HSPCs from BM into PB9, 10, 11 and their homing to BM after transplantation.8, 50 Nevertheless, these effects are indirect and mediated by stimulation of granulocytes, monocytes, and in the endothelium of BM sinusoids, by C3a and/or C5a.9, 10, 11
As the ComC has an important role in the progression of several tumors,1, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28 we became interested in its role in malignant hematopoiesis. However, there are only a few reports in the literature on the signaling of ComC cleavage fragments and the expression of C3aR and C5aR in selected myeloid cell lines.29, 30, 31, 32, 33, 34 It has been demonstrated that the HL-60, THP-1 and U937 cell lines express these receptors29, 30, 31, 32, 33, 34 and that their expression may be regulated by interferon gamma (IFN-γ) and phorbol myristate acetate.30, 33 In contrast to normal hematopoiesis, data on the role of these receptors in regulating the biology of leukemic cells apparently do not exist.
In our current study, we demonstrate for the first time that leukemia cell lines, both myeloid and lymphoid, as well as clonogenic blasts from AML and CML patients express functional C3aR and C5aR receptors, and leukemic cells respond to stimulation by these anaphylatoxins by enhanced random migration known as chemokinesis.40 As the ComC may be activated in leukemic patients by coexisting infections or in response to chemotherapy,1, 51, 52 C3 and C5 cleavage fragments may facilitate the motility and spread of leukemic cells in the hematopoietic microenvironment as well as their egress from BM into PB. At the same time, in contrast to certain solid tumors,21, 22, 23, 41 we found that these potent anaphylatoxins do not affect the proliferation of leukemic cells. Thus, in our hands the ComC does not directly affect expansion of leukemic cells by enhancing their growth but it may enhance their spread by promoting their motility.
The migration of cells is a tightly regulated process, and in this study we demonstrated that HO-1 has an important role in inhibiting the migration of their malignant counterparts, as we previously demonstrated for normal hematopoietic cells.35, 43 In accord with this, HO-1 is an inducible enzyme that is upregulated in response to several oxidative stress stimuli,53 and the anti-inflammatory functions of HO-1 have been very well demonstrated in HO-1 KO mice35, 54 as well as in human HO-1 deficiency,55 in which HO-1 somehow balances the effects of ComC activation. One of the anti-inflammatory effects of HO-1 is inhibition of cell migration. We have recently demonstrated that upregulation of HO-1 in human leukemic cell lines decreases cell chemotaxis,43 whereas intracellular downregulation of HO-1 has the opposite effect.43 On the basis of this finding, we envisioned that upregulation of HO-1 in leukemic cells by the inducible HO-1 activator CoPP or overexpression of the HO-1 gene itself could decrease the chemokinetic spread of leukemic cells. Here, we showed that upregulation of HO-1 expression in human leukemia cells decreased their in vitro migration as well as their in vivo seeding to BM, liver and lungs after injection into an immunodeficient mouse xenotransplant model.
We also demonstrated that, as in vascular cells, HO-1 expression is negatively controlled by p38 MAPK.44, 56 As reported in this latter paper, downregulation of p38 MAPK by small-molecule inhibitors strongly enhanced hypoxia-induced expression of HO-1.44 In our current study, we confirmed that p38 MAPK is also a negative regulator of HO-1 in leukemic cells. Inhibition of p38 MAPK by SB203580 resulted in upregulation of HO-1. By contrast, stimulation of leukemic cells by C3a, C5a and SDF-1 led to upregulation of p38 MAPK, and as a result, to a decrease in expression of HO-1 and enhanced motility of leukemic cells. This effect was abolished in cells exposed to SB203580.
The inhibition of p38 MAPK could additionally result in several pleiotropic effects that could be beneficial in inhibition of myelodysplastic syndrome progression and improving hematopoiesis in these patients.57 However, how much of this latter effect depends on upregulation of HO-1 requires further study. Nevertheless, as reported here, inhibition of p38 MAPK, which leads to upregulation of HO-1, resulted in decreased migration of HSPCs in response to C3a, C5a and SDF-1 gradients. Thus, in addition to upregulation of HO-1 by the small-molecule stimulator CoPP, HO-1 upregulation due to blockade of p38 MAPK could potentially be employed as a strategy to ameliorate the motility and spread of leukemic blasts due to ComC activation. This mutual relationship between the ComC, p38 MAPK and HO-1 is summarized at Figure 7. In addition to the in vitro experiments performed in our study, we also confirmed these observations in vivo in an immunodeficient mouse model using human leukemia cells exposed before injection to a small-molecule p38 MAPK inhibitor.
The reciprocal communication between the ComC, p38 MAPK and HO-1. As illustrated, stimulation of C3 or C5 cleavage fragments by reason of infection leads to p38 MAPK-mediated HO-1 downregulation via their specific receptors in which the leukemia cells become easily mobilized, resulting in spread of the malignancy. On the basis of what we present here, the migratory response of leukemia cells could be constrained by either inhibition of p38 MAPK or upregulation of HO-1.
It is important to mention that the ComC also plays a pleotropic role in leukemia development as a link in the relationship between the tumor and the host immune system.1, 41, 42 Specifically, this relationship regulates tumor growth control in both positive and negative ways. On the one hand, activation of the ComC is an important element in antibody-dependent cellular toxicity, complement-dependent cytotoxicity and the clearance of apoptotic cells.1, 58 On the other hand, ComC activation may protect tumor cells from NK attack by membrane-bound and soluble regulators (for example, CD55, CD59 and factor H)59 and by suppression of anti-tumor T cell immunity.60 On the basis of these pleiotropic effects, the clinical application of general ComC inhibitors, such as eculizumab or compastatin,1 to inhibit the C3a- and C5a-mediated spread of leukemia cells would currently be problematic. By contrast, compounds that upregulate HO-1 and inhibit p38 MAPK could potentially find practical application, and our in vivo results lend support to this possibility.
In conclusion, our results indicate that activation of the ComC in leukemic patients may enhance the migratory potential of malignant blasts, and this enhanced motility may contribute to the systemic spread of leukemic cells. This possibility has to be considered in all clinical situations that lead to activation of the ComC, such as coexisting infections1, 51 or chemotherapy.1, 52 At the same time, more work is needed to fully understand the involvement of the ComC in anti-tumor immune surveillance of leukemia as well as in its contributory role in leukemogenesis. Our results demonstrating the presence of functional C3aR and C5aR on the surface of leukemic cells fully justify this approach.
References
Ricklin D, Hajishengallis G, Yang K, Lambris JD . Complement: a key system for immune surveillance and homeostasis. Nat Immunol 2010; 11: 785–797.
Amara U, Flierl MA, Rittirsch D, Klos A, Chen H, Acker B et al. Molecular intercommunication between the complement and coagulation systems. J Immunol 2010; 185: 5628–5636.
Kozarcanin H, Lood C, Munthe-Fog L, Sandholm K, Hamad OA, Bengtsson AA et al. The lectin complement pathway serine proteases (MASPs) represent a possible crossroad between the coagulation and complement systems in thromboinflammation. J Thromb Haemost 2016; 14: 531–545.
Schraufstatter IU, Discipio RG, Zhao M, Khaldoyanidi SK . C3a and C5a are chemotactic factors for human mesenchymal stem cells, which cause prolonged ERK1/2 phosphorylation. J Immunol 2009; 182: 3827–3836.
Schraufstatter IU, Khaldoyanidi SK, DiScipio RG . Complement activation in the context of stem cells and tissue repair. World J Stem Cells 2015; 7: 1090–1108.
Reca R, Mastellos D, Majka M, Marquez L, Ratajczak J, Franchini S et al. Functional receptor for C3a anaphylatoxin is expressed by normal hematopoietic stem/progenitor cells, and C3a enhances their homing-related responses to SDF-1. Blood 2003; 101: 3784–3793.
Ratajczak J, Reca R, Kucia M, Majka M, Allendorf DJ, Baran JT et al. Mobilization studies in mice deficient in either C3 or C3a receptor (C3aR) reveal a novel role for complement in retention of hematopoietic stem/progenitor cells in bone marrow. Blood 2004; 103: 2071–2078.
Ratajczak MZ, Reca R, Wysoczynski M, Kucia M, Baran JT, Allendorf DJ et al. Transplantation studies in C3-deficient animals reveal a novel role of the third complement component (C3) in engraftment of bone marrow cells. Leukemia 2004; 18: 1482–1490.
Lee HM, Wu W, Wysoczynski M, Liu R, Zuba-Surma EK, Kucia M et al. Impaired mobilization of hematopoietic stem/progenitor cells in C5-deficient mice supports the pivotal involvement of innate immunity in this process and reveals novel promobilization effects of granulocytes. Leukemia 2009; 23: 2052–2062.
Ratajczak MZ . A novel view of the adult bone marrow stem cell hierarchy and stem cell trafficking. Leukemia 2015; 29: 776–782.
Ratajczak MZ, Kim CH, Wojakowski W, Janowska-Wieczorek A, Kucia M, Ratajczak J . Innate immunity as orchestrator of stem cell mobilization. Leukemia 2010; 24: 1667–1675.
Bonig H, Papayannopoulou T . Hematopoietic stem cell mobilization: updated conceptual renditions. Leukemia 2013; 27: 24–31.
Lapidot T, Kollet O . The brain-bone-blood triad: traffic lights for stem-cell homing and mobilization. Hematology Am Soc Hematol Educ Program 2010; 2010: 1–6.
Lévesque JP, Helwani FM, Winkler IG . The endosteal ‘osteoblastic’ niche and its role in hematopoietic stem cell homing and mobilization. Leukemia 2010; 24: 1979–1992.
Mantel CR, O'Leary HA, Chitteti BR, Huang X, Cooper S, Hangoc G et al. Enhancing hematopoietic stem cell transplantation efficacy by mitigating oxygen shock. Cell 2015; 161: 1553–1565.
Levesque JP, Liu F, Simmons PJ, Betsuyaku T, Senior RM, Pham C et al. Characterization of hematopoietic progenitor mobilization in protease-deficient mice. Blood 2004; 104: 65–72.
Adamiak M, Poniewierska-Baran A, Borkowska S, Schneider G, Abdelbaset-Ismail A, Suszynska M et al. Evidence that a lipolytic enzyme-hematopoietic-specific phospholipase C-beta2-promotes mobilization of hematopoietic stem cells by decreasing their lipid raft-mediated bone marrow retention and increasing the promobilizing effects of granulocytes. Leukemia 2016; 30: 919–928.
Imamura T, Yamamoto-Ibusuki M, Sueta A, Kubo T, Irie A, Kikuchi K et al. Influence of the C5a–C5a receptor system on breast cancer progression and patient prognosis. Breast Cancer 2015; e-pub ahead of print 22 October 2015.
Mikesch JH, Buerger H, Simon R, Brandt B . Decay-accelerating factor (CD55): a versatile acting molecule in human malignancies. Biochim Biophys Acta 2006; 1766: 42–52.
Kim KB, Yi JS, Nguyen N, Lee JH, Kwon YC, Ahn BY et al. Cell-surface receptor for complement component C1q (gC1qR) is a key regulator for lamellipodia formation and cancer metastasis. J Biol Chem 2011; 286: 23093–23101.
Ouyang Q, Zhang L, Jiang Y, Ni X, Chen S, Ye F et al. The membrane complement regulatory protein CD59 promotes tumor growth and predicts poor prognosis in breast cancer. Int J Oncol 2016; 48: 2015–2024.
Corrales L, Ajona D, Rafail S, Lasarte JJ, Riezu-Boj JI, Lambris JD et al. Anaphylatoxin C5a creates a favorable microenvironment for lung cancer progression. J Immunol 2012; 189: 4674–4683.
Cai K, Wan Y, Wang Z, Wang Y, Zhao X, Bao X . C5a promotes the proliferation of human nasopharyngeal carcinoma cells through PCAF-mediated STAT3 acetylation. Oncol Rep 2014; 32: 2260–2266.
Maeda Y, Kawano Y, Wada Y, Yatsuda J, Motoshima T, Murakami Y et al. C5aR is frequently expressed in metastatic renal cell carcinoma and plays a crucial role in cell invasion via the ERK and PI3 kinase pathways. Oncol Rep 2015; 33: 1844–1850.
Nunez-Cruz S, Gimotty PA, Guerra MW, Connolly DC, Wu YQ, DeAngelis RA et al. Genetic and pharmacologic inhibition of complement impairs endothelial cell function and ablates ovarian cancer neovascularization. Neoplasia 2012; 14: 994–1004.
Piao C, Cai L, Qiu S, Jia L, Song W, Du J . Complement 5a enhances hepatic metastases of colon cancer via monocyte chemoattractant protein-1-mediated inflammatory cell infiltration. J Biol Chem 2015; 290: 10667–10676.
Vadrevu SK, Chintala NK, Sharma SK, Sharma P, Cleveland C, Riediger L et al. Complement c5a receptor facilitates cancer metastasis by altering T-cell responses in the metastatic niche. Cancer Res 2014; 74: 3454–3465.
Nitta H, Wada Y, Kawano Y, Murakami Y, Irie A, Taniguchi K et al. Enhancement of human cancer cell motility and invasiveness by anaphylatoxin C5a via aberrantly expressed C5a receptor (CD88). Clin Cancer Res 2013; 19: 2004–2013.
Boulay F, Mery L, Tardif M, Brouchon L, Vignais P . Expression cloning of a receptor for C5a anaphylatoxin on differentiated HL-60 cells. Biochemistry 1991; 30: 2993–2999.
Burg M, Martin U, Bock D, Rheinheimer C, Kohl J, Bautsch W et al. Differential regulation of the C3a and C5a receptors (CD88) by IFN-gamma and PMA in U937 cells and related myeloblastic cell lines. J Immunol 1996; 157: 5574–5581.
Crass T, Raffetseder U, Martin U, Grove M, Klos A, Kohl J et al. Expression cloning of the human C3a anaphylatoxin receptor (C3aR) from differentiated U-937 cells. Eur J Immunol 1996; 26: 1944–1950.
Perianayagam MC, Madias NE, Pereira BJ, Jaber BL . CREB transcription factor modulates Bcl2 transcription in response to C5a in HL-60-derived neutrophils. Eur J Clin Invest 2006; 36: 353–361.
Rubin J, Titus L, Nanes MS . Regulation of complement 5a receptor expression in U937 cells by phorbol ester. J Leukoc Biol 1991; 50: 502–508.
Zahn S, Zwirner J, Spengler HP, Gotze O . Chemoattractant receptors for interleukin-8 and C5a: expression on peripheral blood leukocytes and differential regulation on HL-60 and AML-193 cells by vitamin D3 and all-trans retinoic acid. Eur J Immunol 1997; 27: 935–940.
Wysoczynski M, Ratajczak J, Pedziwiatr D, Rokosh G, Bolli R, Ratajczak MZ . Identification of heme oxygenase 1 (HO-1) as a novel negative regulator of mobilization of hematopoietic stem/progenitor cells. Stem Cell Rev 2015; 11: 110–118.
Abdelbaset-Ismail A, Borkowska S, Janowska-Wieczorek A, Tonn T, Rodriguez C, Moniuszko M et al. Novel evidence that pituitary gonadotropins directly stimulate human leukemic cells-studies of myeloid cell lines and primary patient AML and CML cells. Oncotarget 2016; 7: 3033–3046.
Freitas A, Alves-Filho JC, Secco DD, Neto AF, Ferreira SH, Barja-Fidalgo C et al. Heme oxygenase/carbon monoxid–biliverdin pathway down regulates neutrophil rolling, adhesion and migration in acute inflammation. Br J Pharmacol 2006; 149: 345–354.
Wysoczynski M, Reca R, Lee H, Wu W, Ratajczak J, Ratajczak MZ . Defective engraftment of C3aR-/- hematopoietic stem progenitor cells shows a novel role of the C3a–C3aR axis in bone marrow homing. Leukemia 2009; 23: 1455–1461.
Ratajczak MZ, Adamiak M . Membrane lipid rafts, master regulators of hematopoietic stem cell retention in bone marrow and their trafficking. Leukemia 2015; 29: 1452–1457.
Petrie RJ, Doyle AD, Yamada KM . Random versus directionally persistent cell migration. Nat Rev Mol Cell Biol 2009; 10: 538–549.
Pio R, Ajona D, Lambris JD . Complement inhibition in cancer therapy. Semin Immunol 2013; 25: 54–64.
Markiewski MM, DeAngelis RA, Benencia F, Ricklin-Lichtsteiner SK, Koutoulaki A, Gerard C et al. Modulation of the antitumor immune response by complement. Nat Immunol 2008; 9: 1225–1235.
Adamiak M, Iv JB, Zhao J, Abdelbaset-Ismail A, Grubczak K, Borkowska S et al. Downregulation of heme oxygenase 1 (HO-1) activity in hematopoietic cells enhances their engraftment after transplantation. Cell Transplant 2016; 25: 1265–1276.
Naidu S, Vijayan V, Santoso S, Kietzmann T, Immenschuh S . Inhibition and genetic deficiency of p38 MAPK up-regulates heme oxygenase-1 gene expression via Nrf2. J Immunol 2009; 182: 7048–7057.
Honczarenko M, Ratajczak MZ, Nicholson-Weller A, Silberstein LE . Complement C3a enhances CXCL12 (SDF-1)-mediated chemotaxis of bone marrow hematopoietic cells independently of C3a receptor. J Immunol 2005; 175: 3698–3706.
Camous L, Roumenina L, Bigot S, Brachemi S, Fremeaux-Bacchi V, Lesavre P et al. Complement alternative pathway acts as a positive feedback amplification of neutrophil activation. Blood 2011; 117: 1340–1349.
Sadik CD, Kim ND, Luster AD . Neutrophils cascading their way to inflammation. Trends Immunol 2011; 32: 452–460.
Price PJ, Banki Z, Scheideler A, Stoiber H, Verschoor A, Sutter G et al. Complement component C5 recruits neutrophils in the absence of C3 during respiratory infection with modified vaccinia virus Ankara. J Immunol 2015; 194: 1164–1168.
Gutzmer R, Lisewski M, Zwirner J, Mommert S, Diesel C, Wittmann M et al. Human monocyte-derived dendritic cells are chemoattracted to C3a after up-regulation of the C3a receptor with interferons. Immunology 2004; 111: 435–443.
Kim CH, Wu W, Wysoczynski M, Abdel-Latif A, Sunkara M, Morris A et al. Conditioning for hematopoietic transplantation activates the complement cascade and induces a proteolytic environment in bone marrow: a novel role for bioactive lipids and soluble C5b-C9 as homing factors. Leukemia 2012; 26: 106–116.
Flierl MA, Rittirsch D, Nadeau BA, Day DE, Zetoune FS, Sarma JV et al. Functions of the complement components C3 and C5 during sepsis. FASEB J 2008; 22: 3483–3490.
Rutkowski MJ, Sughrue ME, Kane AJ, Mills SA, Parsa AT . Cancer and the complement cascade. Mol Cancer Res 2010; 8: 1453–1465.
Paine A, Eiz-Vesper B, Blasczyk R, Immenschuh S . Signaling to heme oxygenase-1 and its anti-inflammatory therapeutic potential. Biochem Pharmacol 2010; 80: 1895–1903.
Kapturczak MH, Wasserfall C, Brusko T, Campbell-Thompson M, Ellis TM, Atkinson MA et al. Heme oxygenase-1 modulates early inflammatory responses: evidence from the heme oxygenase-1-deficient mouse. Am J Pathol 2004; 165: 1045–1053.
Radhakrishnan N, Yadav SP, Sachdeva A, Pruthi PK, Sawhney S, Piplani T et al. Human heme oxygenase-1 deficiency presenting with hemolysis, nephritis, and asplenia. J Pediatr Hematol Oncol 2011; 33: 74–78.
Keum YS, Yu S, Chang PP, Yuan X, Kim JH, Xu C et al. Mechanism of action of sulforaphane: inhibition of p38 mitogen-activated protein kinase isoforms contributing to the induction of antioxidant response element-mediated heme oxygenase-1 in human hepatoma HepG2 cells. Cancer Res 2006; 66: 8804–8813.
Ganan-Gomez I, Bohannan ZS, Garcia-Manero G . p38 MAPK in MDS. Aging (Albany NY) 2015; 7: 346–347.
Sjoberg AP, Trouw LA, Blom AM . Complement activation and inhibition: a delicate balance. Trends Immunol 2009; 30: 83–90.
Morgan J, Spendlove I, Durrant LG . The role of CD55 in protecting the tumour environment from complement attack. Tissue Antigens 2002; 60: 213–223.
Liu J, Miwa T, Hilliard B, Chen Y, Lambris JD, Wells AD et al. The complement inhibitory protein DAF (CD55) suppresses T cell immunity in vivo. J Exp Med 2005; 201: 567–577.
Acknowledgements
This work was supported by NIH Grants 2R01 DK074720 and R01HL112788, the Stella and Henry Endowment and Harmonia NCN Grant: UMO-2014/14/M/NZ3/00475 to MZR. AAI was on leave of absence from Faculty of Vet. Med. Zagazig Univ., Egypt.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Abdelbaset-Ismail, A., Borkowska-Rzeszotek, S., Kubis, E. et al. Activation of the complement cascade enhances motility of leukemic cells by downregulating expression of HO-1. Leukemia 31, 446–458 (2017). https://doi.org/10.1038/leu.2016.198
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/leu.2016.198
- Springer Nature Limited
This article is cited by
-
Characterization of leukemia progression in the Cbfb-MYH11 knockin mice by single cell RNA sequencing
Leukemia (2023)
-
Intratumoral microbiota: roles in cancer initiation, development and therapeutic efficacy
Signal Transduction and Targeted Therapy (2023)
-
Cobalt protoporphyrin promotes human keratinocyte migration under hyperglycemic conditions
Molecular Medicine (2022)
-
C3a and C5a facilitates the metastasis of myeloma cells by activating Nrf2
Cancer Gene Therapy (2021)
-
C5aR1-positive neutrophils promote breast cancer glycolysis through WTAP-dependent m6A methylation of ENO1
Cell Death & Disease (2021)