Abstract
Purpose. Pregabalin is being evaluated for the treatment of neuropathic pain. Two phase 2 studies were simulated to determine how precisely the dose that caused a one-point reduction in the pain score could be estimated. The likelihood of demonstrating at least a one-point change for each available dose strength was also calculated.
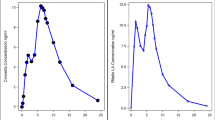
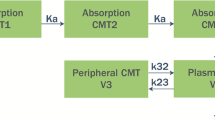
Methods. A pharmacokinetic-pharmacodynamic (PK/PD) model relating pain relief to gabapentin plasma concentrations was derived from a phase 3 study. The PK component of the model was modified to reflect pregabalin PK. The PD component was modified by scaling the gabapentin concentration-effect relationship to reflect pregabalin potency, which was based on preclincal data. Uncertainty about the potency difference and the steepness of the concentration-response slope necessitated simulating a distribution of outcomes for a series of PK/PD models.
Results. Analysis of the simulated data suggested that after accounting for the uncertainty, there was an 80% chance that the dose defining the clinical feature was within 45% of the true value. The likelihood of estimating a dose that was within an acceptable predefined precision range relative to a known value approximated 60%. The minimum dose that should be studied to have a reasonable chance of estimating the dose that caused a one-point change was 300 mg.
Conclusions. Doses that identify predefined response may be imprecisely estimated, suggesting that replication of a similar outcome may be elusive in a confirmatory study. Quantification of this precision provides a rationale for phase 2 trial design and dose selection for confirmatory studies.
Similar content being viewed by others
References
Tufts Center for the Study of Drug Development. Tufts CSSD new drug development cost study. www.tufts.edu/med/cssd/Nov30CostStudy/PressRelease.html (2001).
J. Cross, H. Lee, A. Westelinck, J. Nelson, C. Grudzinskas, and C. Peck. Postmarketing drug dosage changes of 499 FDA-approved new molecular entities. Pharmacoepidemiol. Drug Safety 11:439-446 (2002).
E. R. Heerdink, J. Urquhart, and H. G. Leufkens. Changes in prescribed drug doses after market introduction. Pharmacoepidemiol. Drug Safety 11:447-453 (2002).
N. H. G. Holford, H. C. Kimko, J. P. R. Monteleone, and C. C. Peck. Simulation of clinical trials. Annu. Rev. Pharmacol. Toxicol. 40:209-234 (2000).
P. L Bonate. Clinical trial simulation in drug development. Pharm. Res. 17:3252-3256 (2000).
J. T. Farrar, J. P. Young, Jr., L. LaMoreaux, J. L. Werth, and R. M. Poole. Clinical importance of changes in chronic pain intensity measured on an 11-point numerical pain rating scale. Pain 94:149-158 (2001).
M. Backonja, A. Beydoun, K. R. Edwards, S. L. Schwartz, V. Fonseca, M. Hes, L. LaMoreaux, and E. Garofalo. Gabapentin for the symptomatic treatment of painful neuropathy in patients with diabetes mellitus: a randomized controlled trial. JAMA 280:1831-1836 (1998).
B. Schmidt. Potential antiepileptic drugs; gabapentin. In: R. Levy, R. Mattson, B. Meldrum, J. K. Penry, and F. E. Dreifuss (eds). Antiepileptic Drugs, 3rd ed. Raven Press, New York, 1989, pp. 925-935.
H. N. Bockbrader. Clinical pharmacokinetics of gabapentin. Drugs Today 31:613-619 (1995).
R. A. Blum, J. Comstock, D. A. Sica, R. W. Schultz, E. Keller, P. Reetze, H. Bockbrader, D. Tuerck, J. Busch, P. A. Reece, and A. J. Sedman. Pharmacokinetics of gabapentin in subjects with varying degrees of renal function. Clin. Pharmacol. Ther. 56:154-159 (1994).
D. R. Luke, C. E. Halstenson, J. A. Opsahl, and G. R. Matzke. Validity of creatinine clearance estimates in the assessment of renal function. Clin. Pharmacol. Ther. 48:503-508 (1990).
B. H. Stewart, A. R. Kugler, P. R. Thompson, and H. N. Bockbrader. A saturable transport mechanism in the intestinal absorption of gabapentin is the underlying cause of the lack of proportionality between increasing dose and drug levels in plasma. Pharm. Res. 10:276-281 (1993).
N. H. G. Holford and L. B. Sheiner. Understanding the dose–effect relationship: clinical application of pharmacokinetic and pharmacodynamic models. Clin. Pharmacokinet. 6:429-453 (1981).
S. L. Beal and L. B. Sheiner. NONMEM users guides, part I–VIII. University of California, San Francisco, 1996.
J. A. Busch, J. A. Strand, E. L. Posvar, H. N. Bockbrader, and L. L. Radulovic. Pregabalin (CI-1008) single-dose pharmacokinetics and safety/tolerance in healthy subjects after oral administration of pregabalin solution or capsule doses. Epilepsia 39(Suppl 6):58(1998).
D. Dubuisson and S. G. Dennis. The formalin test:A quantitative study of the analgesic effects of morphine, meperidine, and brain stem stimulation in rats and cats. Pain 4:161-174 (1977).
H. Wheeler-Aceto and A. Cowan. Standardization of the rat paw formalin test for the evaluation of analgesics. Psychpharmacol. 104:35-44 (1991).
K. Hargreaves, R. Dubner, F. Brown, C. Flores, and J. Joris. A new and sensitive method for measuring thermal nociception in cutaneous hyperalgesia. Pain 32:77-88 (1988).
L. O. Randall and J. J. Selitto. A method for measurement of analgesic activity on inflamed tissue. Arch. Int. Pharmacodyn. 111:409-419 (1957).
T. J. Brennan, E. P. Vandermeulen, and G. F. Gebhart. Characterization of a rat model of incisional pain. Pain 64:493-501 (1996).
M. J. Field, S. McCleary, J. Hughes, and L. Singh. Gabapentin and pregabalin, but not morphine and amitriptyline, block both static and dynamic components of mechanical allodynia induced by streptozocin in the rat. Pain 80:391-398 (1999).
Pharsight Trial Simulator Version 1. Pharsight Corporation, Mountain View, California, 1998.
S-Plus 4 for Windows. Insightful Corporation, Seattle, Washington, 1998.
R. Gomeni, C. Falcoz, C. D'Angeli, and A. Bye. In-silico prediction of drug properties in man using preclinical data and computer assisted drug development. Drug Inf. J. 35:1047-1063 (2001).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lockwood, P.A., Cook, J.A., Ewy, W.E. et al. The Use of Clinical Trial Simulation to Support Dose Selection: Application to Development of a New Treatment for Chronic Neuropathic Pain. Pharm Res 20, 1752–1759 (2003). https://doi.org/10.1023/B:PHAM.0000003371.32474.ee
Issue Date:
DOI: https://doi.org/10.1023/B:PHAM.0000003371.32474.ee