Abstract
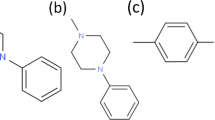
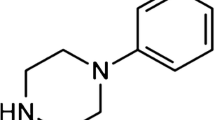
Purpose. To elucidate the efflux transporter(s) responsible for restricting the permeation of an acyloxyalkoxy-based cyclic prodrug of the opioid peptide DADLE (AD) through Caco-2 cell monolayers.
Methods. The cellular permeation characteristics of AD were investigated using Caco-2 cells, Madin-Darby canine kidney wild-type II cells (MDCK-WT), MDCK cells transfected with the human MDR1 gene (MDCK-MDR1), and MDCK cells transfected with the human MRP2 gene (MDCK-MRP2). These cells were grown as monolayers onto microporous membranes. The disappearance of AD from the donor side and its appearance on the receiver side were monitored by high-performance liquid chromatography. The substrate activity of AD for P-glycoprotein (P-gp) was determined using GF120918, a known P-gp specific inhibitor. The substrate activity of AD for MRP2 was determined by using cyclosporin A, a known MRP2 and P-gp inhibitor.
Results. In Caco-2 cells, the ratio of the apparent permeability coefficients (Papp) of AD flux measured in the basolateral (BL) to apical (AP) direction vs. the flux in the AP-to-BL direction (Papp BL-to-AP/
Papp AP-to-BL) was 99. In the presence of 2 μM GF120918 or 25 μM cyclosporin A, the Papp BL-to-AP/Papp AP-to-BL ratio was decreased to 11. In MDCK-WT, MDCK-MDR1, and MDCK-MRP2 cells, the Papp BL-to-AP/Papp AP-to-BL ratios of AD were 4.7, 10, and 5.8, respectively. A mixture of GF120918 (2 μM) and cyclosporin A (25 μM) decreased the Papp BL-to-AP/Papp AP-to-BL ratios of AD in MDCK-WT, MDCK-MDR1, and MDCK-MRP2 cells to 1.2, 1.8, and 2.3, respectively.
Conclusions. These data suggest that AD is a much better substrate for P-gp than MRP2 and that the restricted permeation of this cyclic prodrug in Caco-2 cells and in the intestinal mucosa probably is due primarily to its substrate activity for P-gp.
Similar content being viewed by others
REFERENCES
U. Bickel, T. Yoshikawa, and W. M. Pardridge. Delivery of peptides and proteins through the blood-brain barrier. Adv. Drug Deliv. Rev. 46:247–279 (2001).
C. L. Neilan, T. M. Nguyen, P. W. Schiller, and G. W. Pasternak. Pharmacological characterization of the dermorphin analog. Eur. J. Pharmacol. 419:15–23 (2001).
U. B. Kompella and V. H. Lee. Delivery systems for penetration enhancement of peptide and protein drugs: design considerations. Adv. Drug Deliv. Rev. 46:211–245 (2001).
T. K. Sawyer. (1995) Peptidomimetic Design and Chemistry Approaches to Peptide Metabolism, American Chemical Society, Washington, DC.
R. T. Borchardt, J. Aube, T. J. Siahaan, S. Gangwar, and G. M. Pauletti. Improvement of oral peptide bioavailability: Peptidomimetics and prodrug strategies. Adv. Drug Deliv. Rev. 27:235–256 (1997).
L. Prokai. Peptide drug delivery into the central nervous system. Prog. Drug Res. 51:95–131 (1998).
V. J. Wacher, J. A. Silverman, Y. Zhang, and L. Z. Benet. Role of P-glycoprotein and cytochrome P450 3A in limiting oral absorption of peptides and peptidomimetics. J. Pharm. Sci. 87:1322–1330 (1998).
J. W. Polli, J. L. Jarrett, S. D. Studenberg, J. E. Humphreys, S. W. Dennis, K. R. Brouwer, and J. L. Woolley. Role of P-glycoprotein on the CNS disposition of amprenavir (141W94), an HIV protease inhibitor. Pharm. Res. 16:1206–1212 (1999).
V. J. Wacher, L. Salphati, and L. Z. Benet. Active secretion and enterocytic drug metabolism barriers to drug absorption. Adv. Drug Deliv. Rev. 46:89–102 (2001).
G. M. Pauletti, S. Gangwar, B. Wang, and R. T. Borchardt. Esterase-sensitive cyclic prodrugs of peptides: evaluation of a phenylpropionic acid promoiety in a model hexapeptide. Pharm. Res. 14:11–17 (1997).
G. M. Pauletti, S. Gangwar, F. W. Okumu, T. J. Siahaan, V. J. Stella, and R. T. Borchardt. Esterase-sensitive cyclic prodrugs of peptides: evaluation of an acyloxyalkoxy promoiety in a model hexapeptide. Pharm. Res. 13:1615–1623 (1996).
O. S. Gudmundsson, G. M. Pauletti, W. Wang, D. Shan, H. Zhang, B. Wang, and R. T. Borchardt. Coumarinic acid-based cyclic prodrugs of opioid peptides that exhibit metabolic stability to peptidases and excellent cellular permeability. Pharm. Res. 16:7–15 (1999).
S. Gangwar, S. D. Jois, T. J. Siahaan, D. G. Vander Velde, V. J. Stella, and R. T. Borchardt. The effect of conformation on membrane permeability of an acyloxyalkoxy-linked cyclic prodrug of a model hexapeptide. Pharm Res. 13:1657–1662 (1996).
A. Bak, T. J. Siahaan, O. S. Gudmundsson, S. Gangwar, G. J. Friis, and R. T. Borchardt. Synthesis and evaluation of the physicochemical properties of esterase-sensitive cyclic prodrugs of opioid peptides using an (acyloxy)alkoxy linker. J. Pept. Res. 53:393–402 (1999).
A. Bak, O. S. Gudmundsson, G. J. Friis, T. J. Siahaan, and R. T. Borchardt. Acyloxyalkoxy-based cyclic prodrugs of opioid peptides: evaluation of the chemical and enzymatic stability as well as their transport properties across Caco-2 cell monolayers. Pharm. Res. 16:24–29 (1999).
P. Artursson, K. Palm, and K. Luthman. Caco-2 monolayers in experimental and theoretical predictions of drug transport. Adv. Drug Deliv. Rev. 46:27–43 (2001).
R. T. Borchardt. The application of cell culture systems in drug discovery and development. J. Drug Target. 3:179–182 (1995).
C. Bailey, P. Bryla, and A. Malick. The use of the intestinal epithelial cell culture model, Caco-2, in pharmaceutical development. Adv. Drug Deliv. Rev. 22:85–103 (1996).
A. H. Schinkel, J. J. Smit, O. van Tellingen, J. H. Beijnen, E. Wagenaar, L. van Deemter, C. A. Mol, M. A. van der Valk, E. C. Robanus-Maandag, H. P. te Riele, A. J. M. Berns, and P. Borst. Disruption of the mouse mdr1a P-glycoprotein gene leads to a deficiency in the blood-brain barrier and to increased sensitivity to drugs. Cell 77:491–502 (1994).
J. Hunter, M. A. Jepson, T. Tsuruo, N. L. Simmons, and B. H. Hirst. Functional expression of P-glycoprotein in apical membranes of human intestinal Caco-2 cells. Kinetics of vinblastine Efflux Transporter Restricting Intestine Permeation of DADLE-Prodrug 785 secretion and interaction with modulators. J. Biol. Chem. 268: 14991–14997 (1993).
P. Borst, R. Evers, M. Kool, and J. Wijnholds. The multidrug resistance protein family. Biochim. Biophys. Acta. 1461:347–357 (1999).
J. Gao, E. D. Hugger, M. S. Beck-Westermeyer, and R. T. Borchardt. In H. Doyle, J. B. Griffiths, and D. J. Newell (eds.), Current Protocols in Pharmacology, Vol. 7.2, John Wiley & Sons, Inc., New York, 2000 pp. 1–23.
F. Tang, H. Kazutoshi, and R. T. Borchardt. Are MDCK cells transfected with the human MDR1 gene a good model of the human intestinal mucosa? Pharm. Res. 19:765–772 (2002).
F. Tang, H. Kazutoshi, and R. T. Borchardt. Are MDCK cells transfected with the human MRP2 gene a good model of the human intestinal mucosa? Pharm. Res. 19:773–779 (2002).
S. P. Letrent, G. M. Pollack, K. R. Brouwer, and K. L. Brouwer. Effects of a potent and specific P-glycoprotein inhibitor on the blood-brain barrier distribution and antinociceptive effect of morphine in the rat. Drug Metab Dispos. 27:827–834 (1999).
A. J. Smith, U. Mayer, A. H. Schinkel, and P. Borst. Availability of PSC833, a substrate and inhibitor of P-glycoproteins, in various concentrations of serum. J. Natl. Cancer Inst. 90:1161–1166 (1998).
A. T. Nies, T. Cantz, M. Brom, I. Leier, and D. Keppler. Expression of the apical conjugate export pump, Mrp2, in the polarized hepatoma cell line, WIF-B. Hepatology 28:1332–1340 (1998).
R. L. Juliano and V. Ling. A surface glycoprotein modulating drug permeability in Chinese hamster ovary cell mutants. Biochim. Biophys. Acta. 455:152–162 (1976).
A. H. Schinkel, C. A. Mol, E. Wagenaar, L. van Deemter, J. J. Smit, and P. Borst. Multidrug resistance and the role of P-glycoprotein knockout mice. Eur. J. Cancer 31A:1295–1298 (1995).
J. Konig, A. T. Nies, Y. Cui, I. Leier, and D. Keppler. Conjugate export pumps of the multidrug resistance protein (MRP) family: localization, substrate specificity, and MRP2-mediated drug resistance. Biochim. Biophys Acta. 1461:377–394 (1999).
P. L. Jansen, W. H. Peters, and W. H. Lamers. Hereditary chronic conjugated hyperbilirubinemia in mutant rats caused by defective hepatic anion transport. Hepatology 5:573–579 (1985).
R. Evers, M. Kool, L. van Deemter, H. Janssen, J. Calafat, L. C. Oomen, C. C. Paulusma, R. P. Oude Elferink, F. Baas, A. H. Schinkel, and P. Borst. Drug export activity of the human canalicular multispecific organic anion transporter in polarized kidney MDCK cells expressing cMOAT (MRP2) cDNA. J. Clin. Invest. 101:1310–1319 (1998).
F. Hyafil, C. Vergely, P. Du Vignaud, and T. Grand-Perret. In vitro and in vivo reversal of multidrug resistance by GF120918, an acridonecarboxamide derivative. Cancer Res. 53:4595–4602 (1993).
M. de Bruin, K. Miyake, T. Litman, R. Robey, and S. E. Bates. Reversal of resistance by GF120918 in cell lines expressing the ABC half-transporter, MXR. Cancer Lett. 146:117–126 (1999).
M. J. Cho, D. P. Thompson, C. T. Cramer, T. J. Vidmar, and J. F. Scieszka. The Madin Darby canine kidney (MDCK) epithelial cell monolayer as a model cellular transport barrier. Pharm. Res. 6:71–77 (1989).
J. D. Irvine, L. Takahashi, K. Lockhart, J. Cheong, J. W. Tolan, H. E. Selick, and J. R. Grove. MDCK (Madin-Darby canine kidney) cells: A tool for membrane permeability screening. J. Pharm. Sci. 88:28–33 (1999).
R. Evers, N. H. Cnubben, J. Wijnholds, L. van Deemter, P. J. van Bladeren, and P. Borst. Transport of glutathione prostaglandin A conjugates by the multidrug resistance protein 1. FEBS Lett. 419:112–116 (1997).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tang, F., Borchardt, R.T. Characterization of the Efflux Transporter(s) Responsible for Restricting Intestinal Mucosa Permeation of an Acyloxyalkoxy-Based Cyclic Prodrug of the Opioid Peptide DADLE. Pharm Res 19, 780–786 (2002). https://doi.org/10.1023/A:1016144530146
Issue Date:
DOI: https://doi.org/10.1023/A:1016144530146