Abstract
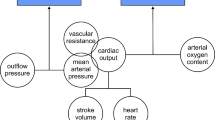
Objective. Critically ill patients frequently have indwelling arterial lines placed during their Intensive Care Unit stay. The lines are used to monitor blood pressure continuously, administer drugs and to draw blood for a variety of physiologic tests. Several blood-conserving arterial line systems have been developed to eliminate the need to discard blood in the process of obtaining undiluted and uncontaminated blood samples. The purpose of this study was to evaluate the dynamic performance of one such system – the Abbott Clinical Care System Safeset™ blood conserving arterial line system – in comparison to a conventional arterial line system. Methods. We studied ninety-nine patients who had indwelling arterial lines placed during surgery and who were admitted to our Surgical Intensive Care Unit (SICU). The patients were randomly placed into one of two groups. The control group received a conventional indwelling arterial line system; the experimental group received the Abbott Safeset™ system. We measured the damping coefficient and resonant frequency daily in order to evaluate and compare the dynamic performance of the two systems. We also measured discard volumes (in the control group) and blood sample sizes during the patients’ stays in the SICU. Results. The two patient groups were similar in regards to demographics and baseline clinical characteristics. A median 3 ml of blood per draw and 17.5 ml of blood per patient was discarded in purging the conventional arterial line system while, by design, no blood was discarded with the experimental system. There was no difference between the two groups with regard to damping coefficient. Both systems were underdamped. However, the conventional arterial line system had a significantly higher resonant frequency (16.7 Hz) compared to the Safeset™ system (12.5 Hz). Conclusions. Because the Abbott Safeset™ blood-conserving arterial line system is underdamped and has a lower resonant frequency compared to the traditional arterial system, it may overestimate systolic blood pressure, particularly in patients with high heart rates.
Similar content being viewed by others
REFERENCES
Lew JKL, Hutchison R, Lin ES. Intra-arterial blood sampling for clotting studies: Effects of heparin contam-ination. Anaesthesia 1991; 46: 719–721
Palermo LM, Andrews RW, Ellison N. Avoidance of heparin contamination in coagulation studies drawn from indwelling lines. Anesth Analg 1980; 59: 222–224
Patel H, Ryan SW, McLain B. Sources of error in neo-natal blood sampling. Archiv Dis Childhood 1988; 63: 752–753
Dennis RC, Ng R, Yeston NS, Statland B. Effect of ample dilutions on arterial blood gas determinations. Crit CareMed 1985; 13: 1067–1068
Soong WJ, Hwang B. Contamination errors when sam-pling blood from an arterial line. Clin Pediatr 1993; 32: 501–503
Reinhardt AC, Tonneson AS, Goodnough SK. Mini-mum discard volume from arterial catheters to obtain coagulation studies free of heparin effect. Heart Lung 1987; 16: 699–705
Gregersen RA, Underhill SL, Detter JC, Schmer G, Lax K. Accurate coagulation studies from heparinized radial artery catheters. Heart Lung 1987; 16: 686–692
Newton R, DeYoung JL, Levin HJ. Volumes of implant-able vascular access devices and heparin flush require-ments. J Natl IV TherAssoc 1985; 8: 137–140
Bourke D. Errors in intraoperative hematocrit determi-nation. Anesthesiology 1976; 45: 357
Lanuza DM, Jennrich JA. The amount of blood with-drawn for diagnostic tests in critically ill patients. Heart Lung 1976; 5: 933–938
Hashimoto F. Bleeding less for diagnostics. J Am Med Assoc 1982; 248: 171
Chernow B, Salem M, Stacey J. Blood conservation-A critical care imperative. Crit CareMed 1991; 19: 313–314
Ti¤n J, Jacobs M. The Dracula factor-red cell loss due to repeated blood sampling. South African Med J 1991; 79: 627–628
Smoller BR, Kruskall MS. Phlebotomy for diagnostic laboratory tests in adults: Pattern of use and effect on transfusion requirements. N Engl J Med 1986; 314: 1233–1235
Dech ZF. Blood conservation for the critically ill. Am Assoc Crit Care Nurses 1994; 5: 169–177
Cicala RS, Cannon K, Larson JS, Fabian TC. Evaluation of coagulation studies from heparinized arterial lines with use of Lab-Site high-pressure tubing. Heart Lung 1988; 17: 662–666
Silver MJ, Jubran H, Stein S, McSweeney T, Jubran F. Evaluation of a new blood-conserving arterial line sys-tem for patients in intensive care units. Crit Care Med 1993; 21: 507–511
Silver MJ, Li Y, Gragg LA, Jubran F, Stoller JK. Reduc-tion of blood loss from diagnostic sampling in critically ill patients using a blood-conserving arterial line system. Chest 1993; 104: 1711–1715
Weibley RE, Riggs CD. Evaluation of an improved sampling method for blood gas analysis from indwelling arterial catheters. Crit Care Med 1989; 17: 803–805
Peruzzi WT, Parker MA, Lichtenthal PR, Cochran-Zull C, Toth B, Blake M. A clinical evaluation of a blood conservation device in medical intensive care unit patients. Crit CareMed 1993; 21: 501–506
Gleason E, Grossman S, Campbell C. Minimizing diag-nostic blood loss in critically ill patients. Am J Crit Care 1992; 1: 85–90
Bedford RF. Invasive blood pressure monitoring. In: Blitt CD, eds. Monitoring in anesthesia and critical care medicine. New York: Churchill Livingstone 1990; 93–134
Gardner RM. Direct blood pressure measurement-Dynamic response requirements. Anesthesiology 1981; 54: 227–236
Yang SS, Bentivoglio LG, Maranhao V, Goldberg H. From cardiac catheterization data to hemodynamic pa-rameters. Philadelphia: FA Davis Company 1978; 3.
Gibbs NC, Gardner RM. Dynamics of invasive pressure monitoring systems: Clinical and laboratory evaluation. Heart Lung 1988; 17: 43–51
Shapiro BA, Mahutte CK, Cane RD et al. Clinical performance of a blood gas monitor: A prospective, multicenter trial. Crit CareMed 1993; 21: 487–494
Zimmerman JL, Dellinger RP. Initial evaluation of a new intra-arterial blood gas system in humans. Crit Care Med 1993; 21: 495–500
Barker SJ, Hyatt J. Continuous measurement of intra-arterial pHa, PaCO2 in the operating room. Anesth Analg 1991; 73: 43–48
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Woda, R.P., Dzwonczyk, R., Buyama, C. et al. On The Dynamic Performance Of The Abbott Safeset™ Blood-Conserving Arterial Line System. J Clin Monit Comput 15, 215–221 (1999). https://doi.org/10.1023/A:1009936917049
Issue Date:
DOI: https://doi.org/10.1023/A:1009936917049