Abstract
This chapter discusses cardiogenic shock, a common condition encountered in the ICU. Cardiogenic shock results from decreased cardiac output and manifests as end-organ ischemia. The key diagnostic criteria for cardiogenic shock are identified, and the different clinical presentations of left and right heart failure are described. Fluid management in patients with an impaired cardiac function is complex, and clinicians traditionally titrate fluid therapy based on central venous pressure and clinical examination. However, there may be an overemphasis on fluid restriction in patients with heart failure, and physicians need to identify the subgroup of patients with cardiogenic shock who might actually benefit from fluid replacement. Fluid boluses need to be titrated to specific end points of end-organ perfusion guided by dynamic measures of fluid responsiveness and repeated echocardiographic assessments. While the pulmonary artery (PA) catheter continues to be the gold standard in assessing hemodynamics and fluid requirements in these patients, less invasive or noninvasive modes have shown potential in providing equivalent information without the risks associated with the PA catheter. Understanding the etiology and type of heart failure is crucial in providing additional information and the likelihood of a favorable response to fluid resuscitation. Take-home messages include the importance of identifying different subtypes of cardiogenic shock and etiology, the definitive role of ultrasound and other invasive or noninvasive hemodynamic monitors to guide fluid management, and the need for carefully titrated fluid boluses to specific end points in patients with impaired cardiac function.
You have full access to this open access chapter, Download chapter PDF
Similar content being viewed by others
Keywords
- Cardiogenic shock
- Fluid management
- VExUS
- Heart failure, left sided
- Heart failure, right sided
- Congestive heart failure
Cardiogenic shock is a life-threatening medical condition where the heart fails to pump enough blood to meet the metabolic demands of tissues. Managing fluids in patients with cardiogenic shock can be challenging, as even small volumes of intravenous fluids can lead to worsening symptoms. Classification of subtypes of cardiogenic shock can aid in determining the underlying pathophysiology and initial management approach. There is a critical need for research on appropriate fluid management strategies in patients with cardiogenic shock. While pulmonary artery catheterization remains the gold-standard monitoring tool, noninvasive or minimally invasive hemodynamic tools such as focused echocardiography, PICCO, or other continuous cardiac output monitors can guide fluid management in patients with left-ventricular failure. For patients with right-ventricular failure, optimizing preload is essential to maintain forward flow, and fluid administration can be guided by echocardiography, dynamic changes in central venous pressure (CVP), passive leg raising, or a pulmonary artery catheter. Fluid administration should be guided by hemodynamic monitoring and targeted to end points of improvement in tissue oxygen delivery.
FormalPara Learning Objectives-
1.
To introduce cardiogenic shock and subtypes.
-
2.
To overview and understand the spectrum of clinical presentation.
-
3.
To learn about assessment of fluid responsiveness and fluid management in left- and right-ventricular failures.
Mr. H, aged 72, is brought to the emergency room with sudden-onset chest pain, excessive sweating, nausea, and dyspnea. He has a history of type II diabetes mellitus on diet control, has arterial hypertension on medications which he takes irregularly, and is a chronic smoker (20 pack-years). He is agitated upon arrival and unable to give any history. Vital signs upon arrival are as follows: heart rate (HR) 145/min, blood pressure (BP) 80/50 mmHg, respiratory rate (RR) 35–40/min, SpO2 62% on room air. He has cold clammy skin and cyanosed extremities. Bilateral diffuse crackles and gallop rhythm are present on auscultation,
Questions
-
Q1. How do you resuscitate this patient?
-
Q2. Is there a role for fluid boluses during the resuscitation process?
Introduction
Cardiogenic shock is frequently encountered by physicians in the intensive care unit (ICU). It manifests as a state of end-organ ischemia secondary to a decreased cardiac output. The established criteria for the diagnosis of cardiogenic shock are as follows [1]:
-
Sustained hypotension: systolic blood pressure < 90 mmHg for 30 min or requirement of vasopressors to achieve a blood pressure ≥ 90 mmHg.
-
Reduced cardiac index (<2.2 L/min/m2).
-
Pulmonary congestion or elevated left-ventricular filling pressures with a pulmonary capillary wedge pressure (PCWP) or pulmonary artery occlusion pressure (PAOP) >15 mmHg or right-ventricular end-diastolic pressure (RVEDP) >10 mmHg.
-
Signs of impaired organ perfusion manifesting as.
-
altered mental status, cold, clammy skin, and prolonged capillary refill time (>2 s),
-
oliguria (<0.5 mL/kg/h),
-
increased serum lactate (or decreased mixed venous or central venous oxygen saturation).
-
These signs of impaired perfusion are present despite adequate intravascular volume and persist even after attempting to correct hypovolemia, arrhythmia, hypoxia, and acidosis.
Cardiogenic shock is a life-threatening clinical entity that occurs as a progression of dysfunction in the right or left side of the heart. Right- and left-sided heart failure are distinct clinical entities though there may be considerable overlap in signs and symptoms with disease progression.
-
Left-ventricular (LV) failure is more likely to present with symptoms of pulmonary congestion in the form of hypoxemia, orthopnea, paroxysmal nocturnal dyspnea, pink frothy sputum production, cough, and wheezing.
-
Right-ventricular (RV) failure on the other hand presents with symptoms of systemic venous congestion, an elevated jugular venous pulse, congestive hepatomegaly, extremity edema, and anasarca.
Since both chambers (right and left) share a common interventricular septum (interventricular independence) and are in series, both forms of heart failure will ultimately manifest in the form of decreased end-organ perfusion resulting in oliguria, hypotension, exercise intolerance, fatigue, and cold clammy extremities leading to life-threatening cardiogenic shock. This chapter will focus on adult patients, and more information on fluid therapy in children can be found in Chap. 20. Some other chapters will discuss fluids in specific populations: sepsis (Chap. 14), trauma (Chap. 16), neurocritical care (Chap. 17), perioperative setting (Chap. 18), burns (Chap. 19), liver failure (Chap. 21), abdominal hypertension (Chap. 22), and COVID-19 (Chap. 26).
Fluid Management of Left-Ventricular Failure
Cardiogenic shock may arise de novo, manifesting as acute heart failure, or it may arise on a background of chronic heart failure. Conventionally, most patients with chronic heart failure are believed to be fluid overloaded with little scope for further fluid resuscitation. They belong to Forrester subgroup IV (Fig. 15.1), have a low cardiac index, high systemic vascular resistance and would benefit from vasopressor and inotropic support. Some of these patients, especially those presenting with acute-on-chronic cardiac failure, may be volume overloaded and conversely may be better treated with diuresis. This situation is common in the ICU.
Spectrum of hemodynamic presentation in cardiogenic shock according to Forrester (adapted from Forrester JS, Diamond G, Chatterjee K, Swan HJ. Medical therapy of acute myocardial infarction by application of hemodynamic subsets. N Engl J Med. 1976;295(24):1356–1362). C(A)RS cardio (abdominal) renal syndrome, CI cardiac index, JVP jugular vein pressure, PAOP pulmonary artery occlusion pressure, US ultrasound
The achievement of an adequate circulating volume is a vital part of the management for most patients with chronic heart failure (Fig. 15.1). Many of these patients will be volume deficient and will therefore respond to a fluid challenge.
It is a common misconception that the pulmonary edema in all acute de novo heart failure is the result of excessive blood volume. This is not generally the case; in fact, many such patients respond favorably to fluid challenge [2]. The elevation of venous pressure observed in these patients is the result of reduced forward flow, causing an increased “back pressure” and congestion in the venous circulation. The role of loop diuretics in the management of acute heart failure seems to contradict this. In fact, the beneficial effect of furosemide is often the result of its vasodilator effect rather than diuresis. It is not uncommon to see large doses of diuretics given to patients with acute pulmonary edema irrespective of their volume status; this can lead to hypovolemia and subsequent hypotension and deterioration of kidney function.
How Should Fluid Responsiveness Be Assessed and Fluid Therapy Titrated in these Patients?
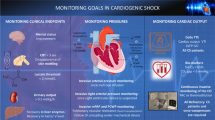
Literature on fluid management of patients with cardiogenic shock is scarce. The pulmonary artery catheter remains the gold standard in providing reliable continuous and reproducible measures of filling pressures of both the right and left heart and monitoring the response of cardiac output to volume therapy. Traditional markers such as central venous or pulmonary artery wedge pressure continues to be used widely but are relatively poor markers of predicting fluid responsiveness [3]. Empiric fluid boluses of 250 mL (4 mL/kg) over 10–15 min of isotonic saline have been advocated previously as long as there is no evidence of pulmonary congestion on physical examination, chest X-ray, or lung ultrasound (B-lines). However, such indiscriminate fluid challenges in patients with impaired ventricular function carry the risk of precipitating pulmonary edema. Use of fluid challenges in left-ventricular failure has to be titrated carefully perhaps guided by dynamic markers of fluid responsiveness. Continuous monitoring of cardiac output is strongly advocated in these patients using transpulmonary thermodilution in combination with pulse wave contour analysis along with measurement of central venous or mixed venous oxygen saturation [4].
In a retrospective study by Adler and colleagues, in patients with cardiogenic shock following cardiac arrest, the PICCO (Pulsion Medical Systems, Munich, Germany) was used as a modality of monitoring fluid therapy guided by additional functional hemodynamic variables (Fig. 15.2) such as PPV (pulse pressure variation), SVV (stroke volume variation), and volumetric indices such as EVLW (extravascular lung water) and GEDV (global end-diastolic volume). The targets for SVV/PPV were set at <10% and a GEDV of 700–800 mL/m−2, while the risk of pulmonary edema was minimized by keeping EVLW <10 mL/kg. This led to a greater use of fluids (5449 ± 449 mL vs. 4375 ± 1285 mL, p = 0.007) in the first 24 h following arrest and a lower incidence of AKI compared to conventional treatment (4.3% vs. 28.6%, p = 0.03) suggesting the potential role of more liberal fluid administration guided by advanced hemodynamic variables in patients post cardiac arrest with compromised cardiac function [5].
Example of fluid unresponsiveness. Increased pulse (PPV) and systolic pressure variations (SPV) in a patient with IAP of 16 mmHg and cardiorenal syndrome. The PPV can be calculated as [(PPmax – PPmin)/PPmean] × 100 (%). After an apnea test it becomes clear that the increased SPV and PPV seen on the monitor is mainly related to a Δup phenomenon as only a smaller portion is caused by Δdown. This means that the increased PPV and SPV are not necessarily correlated to fluid responsiveness and higher thresholds are probably needed.
Passive leg raising (PLR) is a reversible fluid challenge that predicts whether cardiac output will increase with volume expansion. By transferring a volume of around 300 mL of venous blood from the lower body toward the right heart, PLR mimics an endogenous fluid challenge (Fig. 15.3). However, no fluids are actually infused, and the hemodynamic effects are rapidly reversible. The ability of PLR to correctly predict fluid responsiveness in patients with compromised cardiac function was explored in study by Xiang and colleagues [6]. The authors found that the ability of PLR to correctly predict fluid responsiveness was dependent on the systolic function of the heart with sensitivity, specificity, and AUC all higher in the near-normal systolic function group than in the group with impaired systolic function.
The passive leg raising (PLR) test. (a). Starting position with HOB at 45. (b). Passive leg raising via Trendelenburg position with HOB at 45°. In order to perform a correct PLR test, one should not touch the patient in order to avoid sympathetic activation. The PLR is performed by turning the bed from the starting position with head of bed elevation at 30–45° (Panel A) to the Trendelenburg position (Panel B). The PLR test results in an autotransfusion effect via the increased venous return from the legs and the splanchnic mesenteric pool. Monitoring of cardiac output volume is required as a positive PLR test is defined by an increase in SV of at least 10% (adapted with permission from [8])
With the widespread use of bedside echocardiography, cardiac function can be reliably assessed at the bedside and repeated echocardiographic assessment is probably the way forward in titrating fluid therapy in these group of patients. The FALLS protocol (fluid administration limited by lung sonography) emphasizes the use of lung sonography as a valuable adjunct to limit the use of fluids once B-lines are visualized (Fig. 15.4) [7].
The FALLS protocol. A decision tree facilitating the understanding of the FALLS protocol. According to the Weil classification, cardiac and lung ultrasound sequentially rule out obstructive, cardiogenic (from left heart), hypovolemic, and finally distributive shock, i.e., septic shock in current practice. Adapted from (33). FALL protocol, fluid administration limited by lung sonography; BLUE protocol, bedside lung ultrasound in emergency; RV right ventricle, PneumoTx pneumothorax. Adapted with permission from [9]
Fluid Management in Right-Ventricular Failure
Failure of the right heart is characterized by inadequate right-ventricular forward flow eventually leading to a decreased left-ventricular preload. The failing right ventricle generates back-pressure changes manifested by systemic venous congestion, pulsatile liver, and lower extremity edema. The goals of therapy in RV failure encompasses the basic principles of maintaining an optimal RV preload, decreasing RV afterload, and augmenting RV contractility through the use of inotropes and mechanical circulatory support as indicated.
The use of fluids in RV failure to augment RV stroke volume requires an in-depth understanding of RV physiology. The RV pumps its blood against a low-pressure pulmonary circuit in contrast to the LV which pumps blood against a high-pressure systemic circulation. The arterioles act as the resistance vessels in the systemic circulation leading to a large pressure drop across the arterial to venous side of the circulation. The pressure difference while moving from the arterial to the venous side in the pulmonary circulation is markedly less and rarely exceeds 10 mmHg [10].
The RV is a thin-walled chamber that seems to wrap around the more muscular left ventricle. The thickness of the RV wall is only about one-third that of the left ventricle [11]. Therefore, the contractile force of the RV is much less compared to the LV. The RV compensates for this by achieving a much larger end-diastolic volume and surface area per unit volume of blood. The right ventricle musculature is arranged in a superficial transverse layer and a longitudinal muscle layer that extends from apex to base. Sequential contraction of the longitudinal muscle layer from the apex to base dilates the outflow region of the RV and the proximal pulmonary artery to accommodate the RV stroke volume. The RV forward flow is further aided by the low pressure in the pulmonary circulation.
The thin-walled RV chamber is thus much more sensitive to acute changes in afterload, while the thick-walled LV tolerates an increase in afterload better than the RV. The LV is much more sensitive to an acute increase in preload because of its thick muscular walls. In contrast, the RV seems to tolerate an increase in preload much better than the LV. The important anatomical and physiological differences in between the left and right ventricles are summarized in Table 15.1.
The concept of volume replacement to treat RV failure is therefore based on the inherent differences in structure and function of the right ventricle compared to the left ventricle. Volume replacement has been used historically to treat RV failure caused by RV infarction. A plethora of studies had validated the usefulness of volume loading to augment RV stroke volume in cases of RV infarction [12,13,14]. Traditional approaches to the treatment of RV failure have advocated use of fluid boluses in targeting a higher right atrial pressure in patients without concomitant pulmonary congestion [15]. However, subsequent clinical studies failed to replicate the beneficial effect of liberal volume loading in patients with RV infarction and demonstrated that in some instances it might be harmful leading to increased right atrial pressures without an increase in RV stroke volume [16].
In a study of patients with echocardiography-proven RV infarction, the beneficial effect of fluid loading on RV stroke work index was found at a right atrial pressure of 10–14 mmHg. However, volume replacement with right atrial pressure more than 14 mmHg was accompanied by a reduction in the RV stroke index [17]. The harmful effect of overaggressive fluid loading in patients with RV infarction is explained by the interventricular interdependence. The RV and the LV are enclosed by the pericardium and share a common interventricular septum. Overaggressive volume loading of the RV will lead to an increase in RV end-diastolic pressure and shifting of the interventricular septum toward the side of LV, compromising LV filling and resultant cardiac output. This is classically seen in echocardiography in parasternal short axis view as a D-shaped LV with the septum encroaching on the LV cavity (Fig. 15.5).
The degree of septal shift is dependent on the extent in the rise of RV end-diastolic pressure in comparison to the LV end-diastolic pressure. Under normal conditions, an increase in RV end-diastolic pressure due to volume loading leads to an increase in RV stroke volume and subsequent increase in LV end-diastolic pressure so that the relative differences between LV and RV end-diastolic pressures are maintained. However, in conditions associated with an increase in pulmonary vascular resistance or an increase in RV afterload (e.g., pulmonary embolism), the RV fails to increase its forward flow to fluid replacement, leading to an impaired LV filling and harmful effects of fluid resuscitation. In such cases, the therapy should be focused on relieving the cause of increased RV afterload rather than fluid loading to augment preload.
Another harmful effect of excessive fluid loading with compromised RV function is excessive RV wall tension leading to a decreased coronary perfusion of the right ventricle with resultant RV ischemia.
The importance of venous congestion in the development of worsening renal function in advanced decompensated heart failure can possibly explain the greatest improvement of the renal function after medical treatment in patients characterized by echocardiographic signs of the impact of right-ventricular dysfunction on inferior vena cava, portal, hepatic, and renal veins. Recently, a novel grading system was proposed for venous congestion, the Venous Excess Ultrasound (VExUS) grading system based on the combination of multiple ultrasound findings (Table 15.2).
How to Assess Fluid Responsiveness and Titrate Fluids in RV Failure?
Identification of RV failure has classically relied on the well-described clinical signs of an elevated jugular venous pulsation, splitting of the second heart sound, and a prominent tricuspid regurgitation murmur.
Critically ill patients with RV failure need adequate RV preload to maintain optimal RV forward flow. They might often be volume depleted secondary to bleeding, increased vascular permeability, or insensible losses. Positive-pressure ventilation impedes venous return. Sedatives and analgesics can blunt the sympathetic response and venous tone further aggravating the problem. Therefore, careful volume titration is necessary in such patients. The right atrial pressure targets guided by central venous pressure (CVP) should be kept in the high normal range of 8–12 mmHg and titrated further on the basis of hemodynamics and cardiac output (e.g., with the two-to-five rule, Table 15.3) [18].
Monitoring of pulse pressure variation (PPV) with an arterial catheter in situ has been used as a predictor of fluid responsiveness [20]. The PPV is less reliable in the setting of acute respiratory distress syndrome (ARDS) given poor lung compliance, low tidal volumes, and also when the patient is breathing spontaneously.
However, one must exercise a note of caution when using PPV to predict RV fluid responsiveness. RV is exquisitely sensitive to increase in afterload. Therefore, an increase in PPV above conventionally described thresholds of 12–13% in the setting of RV failure maybe an indicator of RV afterload responsiveness and potential volume overloaded state. Such a patient may potentially decompensate from overzealous fluid administration. Therefore, one should not use PPV in isolation in deciding to fluid challenge a patient with RV failure but look for other signs of potential RV overload (e.g., dilated RV in echocardiography, elevated CVP, distended inferior vena cava). One may also use a PLR maneuver to look for change in PPV in such cases. No change or worsening of PPV post PLR could indicate RV afterload dependence, while decrease in PPV following PLR could indicate fluid responsiveness [21].
Echocardiography can be used to assess RV function more objectively by measurement of tricuspid annular plane systolic excursion in a four-chambered view using tissue Doppler over the tricuspid annulus. Assessment of RV chamber size can also be used to detect RV dilatation. The ratio of RV to LV end-diastolic area between 0.6 and 1 indicates RV dilatation, while a ratio greater than 1 indicates severe RV dilatation. Acute cor pulmonale in echocardiography is indicated by RV–LV size greater than 0.6 in combination with paradoxical septal motion [22]. Along with an assessment of RV function, echocardiography and other modalities should be used to look for the precipitating cause of RV failure (e.g., infarction, embolism, valve disease). This is necessitated by the understanding that RV failure caused by conditions of increased afterload is less likely to respond to fluid resuscitation. Echocardiography is a useful tool to detect features of RV overload such as septal shift toward the LV and thereby guide decisions regarding further fluid therapy. Serial hemodynamic assessment guided by echocardiography is an absolute necessity in titrating fluids in this group of patients. In cases where the RV preload is too high, diuretics and renal replacement therapy to remove excess fluid can be associated with an improvement in cardiac output. The Frank–Starling curve of the RV is flatter and wider than the LV. Hence, a significant amount of fluid needs to be removed before an appreciable increase in cardiac output is achieved in a volume overloaded RV.
A Swan–Ganz pulmonary artery catheter can also be placed to derive reliable, continuous, and objective information about the RV function and response to fluid therapy. The PA catheter allows measurement of cardiac output and mixed venous oxygen saturation, in addition to other static measures such as pulmonary artery occlusion pressure and PA pressure. Measurement of cardiac output using cold saline through PA catheter may underestimate the actual cardiac output, if the patient has significant tricuspid regurgitation, while, the PA catheter continues to be the gold standard in the measurement of cardiac output and systemic and pulmonary vascular resistance. However, it is being used in limited centers worldwide, due to its invasiveness and limited evidence on outcome benefit in the management of cardiac failure. The advanced systems based on the principle of transpulmonary thermodilution have been used to calculate derived indices such as extravascular lung water (EVLW) and pulmonary vascular permeability index (PVPI) to detect pulmonary congestion early in the setting of compromised cardiac function.
Case Vignette
In the case vignette described in the beginning of this chapter, Mr. H appears to be in cardiogenic shock, belonging to wet and cold subtype of the Forrester classification. The patient presents with ischemic chest pain and has risk factors for acute coronary syndrome with past medical history of arterial hypertension, type 2 diabetes mellitus, and chronic smoking. Initial part of his management should focus on stabilizing his ABCs, with supplemental O2 (escalation to noninvasive ventilation, if required), and starting norepinephrine to support his MAP to ensure adequacy of organ perfusion. Along with blood investigations, an immediate 12-lead electrocardiogram and troponin levels should be performed to rule out a possible ischemic event and manage accordingly. In addition, it would be prudent to look for other precipitating causes. Aggressive fluid resuscitation should be withheld at his stage given his clinical features of volume overload (crackles, gallop rhythm), and any fluid replacement should be guided by a bedside echocardiography and hemodynamic monitoring.
Conclusion
To summarize, fluid management in patients with impaired cardiac function is complex. In the absence of widespread literature, clinicians continue to titrate the fluid therapy based on traditional measures of central venous pressure and clinical examination. There is an overemphasis on restricting fluids in patients with heart failure, but the physician needs to identify the subgroup of patients with cardiogenic shock who might actually benefit from fluid replacement. The fluid boluses need to be titrated to specific end points of end-organ perfusion guided by dynamic measures of fluid responsiveness and frequent echocardiographic assessments. While the PA catheter continues to be the gold standard in assessment of hemodynamics and fluid/vasopressor requirements in these patients, minimally invasive or noninvasive modes have shown potential in providing equivalent information without the attendant risks associated with the placement and maintenance of a PA catheter. One needs to understand the etiology and the type of heart failure that might provide additional information and likelihood of a favorable response to fluid resuscitation.
Take Home Messages
-
It is important to identify different subtypes of cardiogenic shock and etiology.
-
Not all patients with cardiogenic shock are fluid depleted.
-
There is a definitive role of ultrasound and other invasive or noninvasive hemodynamic monitors to guide fluid management.
-
Carefully titrated fluid boluses to specific end points are the key in patients with impaired cardiac function.
References
Thiele H, Ohman EM, Desch S, Eitel I, De WS. Clinical update management of cardiogenic shock. Eur Heart J. 2015;36:1223–30.
Mebazaa A, Gheorghiade M, Piña IL, et al. Practical recommendations for prehospital and early in-hospital management of patients presenting with acute heart failure syndromes. Crit Care Med. 2008;36(1 Suppl):S129–39.
Marik PE, Baram M, Vahid B. Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares. Chest. 2008;134:172–8.
Levy B, Bastien O, Bendjelid K, Cariou A, Chouihed T, Combes A, et al. Experts’ recommendations for the management of adult patients with cardiogenic shock. Ann Intensive Care. 2015;5:1–10. https://doi.org/10.1186/s13613-015-0052-1.
Adler C, Reuter H, Seck C, Hellmich M, Zobel C. Fluid therapy and acute kidney injury in cardiogenic shock after cardiac arrest. Resuscitation. 2013;84(2):194–9.
Si X, Cao DY, Chen J, Wu JF, Liu ZM, Xu HL, et al. Effect of systolic cardiac function on passive leg raising for predicting fluid responsiveness: a prospective observational study. Chin Med J. 2018;131(3):253–62.
Lichtenstein D. FALLS-protocol: lung ultrasound in hemodynamic assessment of shock. Heart Lung Vessel. 2013;5(3):142–7.
Hofer C, Cannesson M. Monitoring fluid responsiveness. Acta Anaesthesiol Taiwan. 2011;49(2):59–65.
Lichtenstein D, van Hooland S, Elbers P, Malbrain ML. Ten good reasons to practice ultrasound in critical care. Anaesthesiol Intensive Ther. 2014;46(5):323–335.
Bhattacharya J, Staub NC. Direct measurement of microvascular pressures in the isolated perfused dog lung. Science. 1980;210:327–8.
Greyson CR. Pathophysiology of right ventricular failure. Crit Care Med. 2008;36(1, Suppl):S57–65.
Lopez-Sendon J, Coma-Canella I, Vinuelas AJ. Volume loading in patients with ischemic right ventricular dysfunction. Eur Heart J. 1981;2:329–38.
Baigrie RS, Haq A, Morgan CD, et al. The spectrum of right ventricular involvement in inferior wall myocardial infarction: a clinical, hemodynamic and noninvasive study. J Am Coll Cardiol. 1983;1:1396–404.
Goldstein JA, Vlahakes GJ, Verrier ED, et al. Volume loading improves low cardiac output in experimental right ventricular infarction. J Am Coll Cardiol. 1983;2:270–8.
Siniorakis EE, Nikolaou NI, Sarantopoulos CD, et al. Volume loading in predominant right ventricular infarction: bedside hemodynamics using rapid response thermistors. Eur Heart J. 1994;15:1340–7.
Ferrario M, Poli A, Previtali M, et al. Hemodynamics of volume loading compared with dobutamine in severe right ventricular infarction. Am J Cardiol. 1994;74:329–33.
Berisha S, Kastrati A, Goda A, et al. Optimal value of filling pressure in the right side of the heart in acute right ventricular infarction. BMJ. 1990;63:98–102.
Ventetuolo CE, Klinger JR. Management of acute right ventricular failure in the intensive care unit. Ann Am Thorac Soc. 2014;11(5):811–22.
Malbrain ML, Marik PE, Witters I, et al. Fluid overload, de-resuscitation, and outcomes in critically ill or injured patients: a systematic review with suggestions for clinical practice. Anaesthesiol Intensive Ther. 2014;46(5):361–80.
Yang X, Du B. Does pulse pressure variation predict fluid responsiveness in critically ill patients? A systematic review and meta-analysis. Crit Care. 2014;18:650.
Vieillard-Baron A, Matthay M, Teboul JL, et al. Experts' opinion on management of hemodynamics in ARDS patients: focus on the effects of mechanical ventilation. Intensive Care Med. 2016;42(5):739–49.
Vieillard-Baron A, Prin S, Chergui K, Dubourg O, Jardin F. Echo-Doppler demonstration of acute cor pulmonale at the bedside in the medical intensive care unit. Am J Respir Crit Care Med. 2002;166:1310–9.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Open Access This chapter is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made.
The images or other third party material in this chapter are included in the chapter's Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the chapter's Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder.
Copyright information
© 2024 The Author(s)
About this chapter
Cite this chapter
Srinivasan, S., Kundu, R. (2024). Fluid Management in Cardiogenic Shock. In: Malbrain, M.L., Wong, A., Nasa, P., Ghosh, S. (eds) Rational Use of Intravenous Fluids in Critically Ill Patients. Springer, Cham. https://doi.org/10.1007/978-3-031-42205-8_15
Download citation
DOI: https://doi.org/10.1007/978-3-031-42205-8_15
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-031-42204-1
Online ISBN: 978-3-031-42205-8
eBook Packages: MedicineMedicine (R0)