Abstract
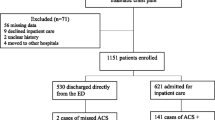
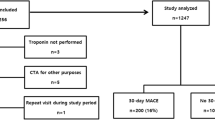
Identification of patients with acute cardiac ischemia (ACI) remains challenging. The object of this study was to examine the role of clinical findings in the diagnosis/triage of emergency department (ED) patients with symptoms suggestive of ACI. The study was designed as a secondary data analysis of a multicenter prospective controlled clinical trial. It was set in 10 midwest, southeast, and northeast U.S. hospitals, and 10,689 patients with chest pain or other symptoms suggesting ACI presenting from May 1993 to December 1993, participated. The results indicated that ACI patients were more likely to have chest pain as a chief complaint or presenting symptom (P = 0.001). The presenting symptom of nausea was more commonly associated with a final diagnosis of ACI (P = 0.003). Shortness of breath as the chief complaint and presenting symptoms of abdominal pain, nausea, dizziness, and fainting were less frequent among patients with a final diagnosis of ACI (P = 0.001). A past history of diabetes mellitus, myocardial infarction, or angina pectoris was more frequently associated with a final diagnosis of ACI (P = 0.001). A lower pulse rate in patients with a final diagnosis of ACI (P = 0.001) was not considered clinically significant. Median first and highest systolic blood pressures (SBPs) were higher, median lowest SBPs were lower, median diastolic blood pressure of the lowest SBPs were lower, and initial and highest pulse pressures were wider in patients with a final diagnosis of ACl (P = 0.001). On arrival, these blood pressure variables in AMI patients, subsequently classified as Killip class 4, were above the threshold for this classification. Rales were more commonly present in patients with a final diagnosis of ACI (P= 0.001). All primary ST-segment abnormalities, Q waves, and T-wave abnormalities, except T-wave flattening, were seen more frequently in patients with a final diagnosis ACI (P= 0.001). Normal ECGs were more frequently associated with a non-ACI final diagnosis, yet 20% of AMI patients and 37% of Unstable Angina Pectoris (UAP) patients had normal ECGs. It can be concluded that certain clinical features can help to identify ED patients with ACI. Initially normal ECGs can be seen in 20% of patients with AMI and 37% of patients with UAP. Patients with ACI can present with “normal” blood pressures and develop cardiogenic shock. Clinical outcome data for ACI patients are presented.
Similar content being viewed by others
References
Heberden W. Some account of a disorder of the breast. Med Trans R Coll Phys Lond, 1772.
Herrick JB. Clinical features of sudden obstruction of the coronary arteries. JAMA 1912;59:2015-2020.
Vander Does E, Lubsen J, Poul J, et al: Acute coronary events in a general practice: objectives and design of the Imminent Myocardial Infarction. Rotterdam Study Heart Ball 7:91-98, 1976.
McCaig L. National Hospital Ambulatory Care Survey: 1992 Emergency Department Summary. Advanced Data, 1994;245:1-12.
Pozen MW, D'Agostino RB, Selker HP, Sytkowski PA, Hood WB Jr. A predictive instrument to improve coronary care unit admission practices in acute ischemic heart disease: A prospective multicenter clinical trial. N Engl J Med 1984; 310:1273-1278.
Goldman L, Weinberg M, et al. A computer-derived protocol to aid in the diagnosis of emergency room patients with acute chest pain. N Engl J Med 1982;307:588-596.
Schor S, Behar S, Modan B, Drory J, Kariv I. Disposition of presumed coronary patients from an emergency room: A follow-up study. JAMA 1976;236:941-943.
Lee TH, Rouan GW, Weisberg MC, et al. Clinical characteristics and natural history of patients with acute myocardial infarction sent home from the emergency room. Am J Cardiol 1987;60:219-224.
Pozen MW, D'Agostino RB, Mitchell JB, et al. The usefulness of a predictive instrument to reduce inappropriate admissions to the coronary care unit. Ann Intern Med 1980;92:238-242.
Selker Hp, Pozen MW, D'Agostino RB. Optimal identification of the patient with acute myocardial ischemia in the emergency room. In Calif RM, Wagner GS, eds. Acute Coronary Care: Principles and Practice. Boston: Martinus Nijhoff, 1985:289-298.
Bloom B, Peterson O. End results, costs, and productivity of coronary care units. N Engl J Med 1973;288:72-78.
Eisenberg JM, Horowitz LN, Busch R, Arvan D, Rawnsley H. Diagnosis of acute myocardial infarction in the emergency room: A prospective assessment of clinical decision making and the usefulness of immediate cardiac enzyme determination. J Community Health 1979;4:190-198.
Fuchs R, Scheidt S. Improved criteria for admission to cardiac care units. JAMA 1981;246:2037-2041.
Tierney WM, Roth BJ, Psaty B, et al. Predictors of myocardial infarction in emergency room patients. Crit Care Med 1985;13:526-531.
Goldman L, Cook EF, Brand DA, et al. A computer protocol to predict myocardial infarction in emergency department patients with chest pain. N Engl J Med 1988;318:707-803.
McCarthy BD, Beshansky JR, D'Agostino RB, Selker HP. Missed diagnoses of acute myocardial infarction in the emer-Clinical Features of ED Patients with ACI 73 gency department: Results from a multicenter study. Ann Emerg Med 1993;22:579-582.
NIH National Heart Attack Alert Program Working Group on the Diagnosis of Acute Cardiac Ischemia Report. Ann Emerg Med 1997;29:1-87.
McCarthy BD, Wong JB, Selker HP. Detecting acute cardiac ischemia in the emergency department: A review of the literature. J Gen Intern Med 1990;5:365-373.
Gillum RF, Fortman SP, Prineas RF, et al: International diagnostic criteria for acute myocardial infarction and stroke. Am Heart J 1984;108:150-158.
Campeau L: Grading of angina pectoris. Circulation 1976; 54:522-523.
Selker HP, et al. The use of the ACI-TIPI to assist emergency department triage of patients with chest pain or other symptoms suggestive of acute cardiac ischemia: A multicenter controlled clinical trial. In press.
Jayes RL, et al, Do patient's coronary risk factor reports predict acute cardiac ischemia in the emergency department? A multicenter study. J Clin Epidemiol, 1992;45: 621-626.
Gordon T, Sorlie P, Kannel WB. Coronary heart disease, atherothrombotic brain infarction, intermittent claudication-a multivariate analysis of some factors related to their incidence: Framingham study, 16-year follow-up. In: Framingham Study, 16-year Follow-up. Sect 27. U.S. Government Printing Office, 1971.
Truett J, Cornfield J, Kannel W. A multivariate analysis of the risk of coronary heart disease in Framingham. J Chron Dis 1967;20:511-524.
Selker HP, Griffith JL, D'Agostino RB. A time-insensitive predictive instrument for acute myocardial infarction mortality: A multicenter study. Med Care 1991;29:1196-1211.
Rude RE, Poole WK, Muller JE, et al. Electrocardiographic and clinical criteria for recognition of acute myocardial infarction based on analysis of 3,697 patients. Am J Cardiol 1983;52:936-942
Selker HP, Beshansky JR, et al. Presenting pulse pressure predicts thrombolytic therapy-related intracranial hemorrhage. Circulation 1994;90:1657-1661.
Sawe U. Early diagnosis of acute myocardial infarction with special reference to the diagnosis of the intermediate coronary syndrome: A clinical study. Acta Med Scand 1972; 520(Suppl.):1-76.
Tierney WM, Roth BJ, Psaty B, et al. Predictors of myocardial infarction in emergency room patients. Crit Care Med 1985;13:526-31.
Killip T, Kimball JT. Treatment of myocardial infarction in a coronary care unit. A two year experience with 250 patients. Am J Cardiol 1967;20:457-64.
Lee TH, Cook F, Weisberg M, Sargent RK, Wilson C, Goldman L. Acute chest pain in the emergency room: Identification and examination of low-risk patients. Arch Intern Med 1985;145:65-69.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Pope, J.H., Ruthazer, R., Beshansky, J.R. et al. Clinical Features of Emergency Department Patients Presenting with Symptoms Suggestive of Acute Cardiac Ischemia: A Multicenter Study. J Thromb Thrombolysis 6, 63–74 (1998). https://doi.org/10.1023/A:1008876322599
Issue Date:
DOI: https://doi.org/10.1023/A:1008876322599