Abstract
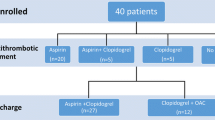
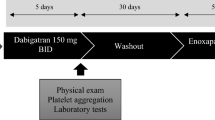
Thromboembolic complications are reported to occur in up to 0.5–2% of left cardiac catheterizations and angiographies. Activation of the hemostatic system may contribute to their onset. To prevent platelet and thrombin activity during catheterization, aspirin or systemic heparin are often used in addition to heparinized flush solutions. We investigated whether aspirin alone can prevent platelet and thrombin activity induced by catheterization in ten consecutive patients (nine males, mean 50 ± 8 years) undergoing elective left cardiac catheterization after at least 5 days of oral aspirin (75–300 mg/d). Anticoagulant drugs were not given. Peripheral venous samples were drawn before, immediately after (time 0), and at 15, 60, and 180 minutes after the procedure for measurement of thrombin–antithrombin (TAT), prothrombin fragment 1.2 (F 1.2), fibrinopeptide A (FPA), and β-thromboglobulin (β-TG). TAT, F1.2, and FPA increased significantly at time 0 compared with both before and 180 minutes after the procedure (P < 0.04); β-TG values were higher at time 0 compared with 180 minutes later (P = 0.01). TAT levels were related to those of FPA (r = 0.66; P = 0.0003), F1.2 (r = 0.35; P = 0.01), and β-TG (r = 0.37; p = 0.04). Thus, routine left cardiac catheterization is associated with transient, systematically detectable, activation of coagulation and platelets, despite aspirin therapy. Newer antiplatelet agents may be more effective in preventing hemostatic activation induced by catheterization.
Similar content being viewed by others
References
Davis K, Kennedy JW, Kemp HG, et al. Complications of coronary arteriography from the collaborative study of coronary artery surgery (CASS). Circulation 1979;59: 1105–1111.
Cheng TO. Fatal thromboembolism following selective coronary arteriography. Chest 1972;62:1–2.
Johnson LW, Lozner EC, Johnson S, et al. Coronary arteriography 1984–1987: A report of the Registry of the Society for Cardiac Angiography and Interventions. Results and complications. Cathet Cardiovasc Diag 1989;17:5–10.
Jackson DMA, Dawson P. Current usage of contrast agents, anticoagulant and antiplatelet drugs in angiography and angioplasty in the UK. Clin Radiol 1995;50:699–704.
Hill JA, Grabowski EF. Relationship of anticoagulation and radiographic contrast agents to thrombosis during coronary angiography and angioplasty. Cathet Cardiovasc Diagn 1992;25:200–208.
Adams DF, Fraser DB, Abrams HL. The complications of coronary arteriography. Circulation 1973;48:609–618.
Wyman RM, Safian RD, Portway U, et al. Current complications of diagnostic and therapeutic cardiac catheterization. J Am Coll Cardiol 1988;12:1400–1406.
Ciabattoni G, Ujang S, Sritara P, et al. Aspirin, but not heparin, suppresses the transient increase in thromboxane biosynthesis associated with cardiac catheterization or coronary angioplasty. J Am Coll Cardiol 1993;21:1377–1381.
Rosenberg RD, Rosenberg JS. Natural anticoagulant mechanisms. J Clin Invest 1984;74:1–9.
Stein B, Fuster V, Israel DH, et al. Platelet inhibitor agents in cardiovascular disease. An update. J Am Coll Cardiol 1986;14:813–824.
Brown BG, Zhao XQ, Bordsley J, Albers JJ. Secondary prevention of heart disease amongst patients with lipid abnormalities: Practice and trends in the United States. J Intern Med 1997;241:283–294.
Ludlam CA, Cash JD. Studies on the liberation of b-thromboglobulin from human platelets in vitro. Br Haematol 1976;33:239–247.
Verstraete M, Vermylen J. Coagulation tests as possible indicators of established thrombosis. In: Thrombosis. Oxford: Pergamon Press, 1984:64.
Schafer Al. Antiplatelet therapy. Am J Med 1996;101: 199–209.
Biasucci L, Liuzzo G, Caligiuri G, et al. Temporal relation between ischemic episodes and activation of the coagulation system in unstable angina. Circulation 1996;93:2121–2127.
Andreotti F, Pasceri V, Hackett DR, Davies GJ, Haider AW, Maseri A. Preinfarction angina as a predictor of more rapid coronary thrombolysis in patients with acute myocardial infartion. N Engl J Med 1996;334:7–12.
Katayama H, Yamaguchi K, Kozuka T, et al. Adverse reactions to ionic and non-ionic contrast media. Radiology 1990;175:621–628.
Chronos NAF, Goodall AH, Wilson DJ, Sigwart U, Buller NP. Profound platelet degranulation is an important side effect of some types of contrast media used in interventional cardiology. Circulation 1993;88:2035–2044.
Fareed J, Walenga JM, Saravia GE, Moncada RM. Thrombogenic potential of non ionic contrast media? Radiology 1990;174:321–325.
Wallace S, Medellin H, De Jongh D, et al. Systemic heparinization for angiography. Am J Radiol 1972;116:204–206.
Antonic R, Rosch J, Dotter CT. The value of systemic arterial heparinization in transfemoral angiography; a prospective study. Am J Radiol 1976;126:223–225.
Glickstein MF, McLean GK, Sussman SK. Optimizing heparin utilization in angiographic flush solution. Angiology 1990;41:825–828.
The EPIC Investigators. Use of a monoclonal antibody directed against the platelet glycoprotein IIb/IIIa receptor in high-risk coronary angioplasty. N Engl J Med 1994;330: 956–961.
Balsano F, Rizzon P, Violi, et al. and the STA I Group. Antiplatelet treatment with Ticlopidine in unstable angina: A controlled multicenter trial. Circulation 1990;82:17–24.
Maresta A, Balducelli M, Contini L, et al. Trapidil (triazolopyridine), a platelet-derived growth factor antagonist, reduces restenosis after percutaneous transluminal coronary angioplasty. Results of the randomized, double blind STARC study. Studio Trapidil versus aspirina nella restenosi coronarica. Circulation 1994;90:2710–2715.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Andreotti, F., Lefroy, D.C., Sciahbasi, A. et al. Platelet and Thrombin Activity Following Cardiac Catheterization Despite Treatment with Aspirin. J Thromb Thrombolysis 6, 141–145 (1998). https://doi.org/10.1023/A:1008805823198
Issue Date:
DOI: https://doi.org/10.1023/A:1008805823198