Abstract
Liver-enhancing modalities, such as portal vein embolization, are increasingly employed prior to major liver resection to prevent postoperative liver dysfunction. Selection criteria for such techniques are not well described. This study uses CT-based volumetric analysis as a tool to identify patients at highest risk for postoperative hepatic dysfunction. Between July 1999 and December 2000, a total of 126 consecutive patients who were undergoing liver resection for colorectal metastasis and had CT scans at our institution were included in the analysis. Volume of resection was determined by semiautomated contouring of the liver on preoperative volumetrically (helical) acquired CT scans. Hepatic dysfunction was defined as prothrombin time greater than 18 seconds or serum bilirubin level greater than 3 mg/dl. Marginal regression was used to compare the predictive ability of volumetric analysis and the extent of resection. The percentage of liver remaining was closely correlated with increasing prothrombin time and bilirubin level (P < 0.001). After trisegmentectomy, 90% of patients with ≤s25% of liver remaining developed hepatic dysfunction, compared with none of the patients with more than 25% of liver remaining after trisegmentectomy (P < 0.0001). The percentage of liver remaining was more specific in predicting hepatic dysfunction than was the anatomic extent of resection (P = 0.003). Male sex nearly doubled the risk of hepatic dysfunction (odds ratio = 1.89, P = 0.027), and having ≤25% of liver remaining more than tripled the risk (odds ratio = 3.09, P < 0.0001). Hepatic dysfunction and ≤25% of liver remaining were associated with increased complications and length of hospital stay (P < 0.0001 and P = 0.0003, respectively). Preoperative assessment of future liver volume remaining distinguishes which patients undergoing liver resection will most likely benefit from preoperative liver enhancement techniques such as portal vein embolization.
Similar content being viewed by others
References
Fong Y, Fortner J, Sun RL, Brennan MF, Blumgart LH. Clinical score for predicting recurrence after hepatic resection for metastatic colorectal cancer. Analysis of 1001 consecutive cases. Ann Surg 1999;230:309–318.
Scheele J, Stang R, Altendorf-Hofmann A, Paul M. Resection of colorectal liver metastases. World J Surg 1995;19:59–71.
Rosen CB, Nagorney DM, Taswell HF, Helgeson SL, Ilstrup DM, van Heerden JA, Adson MA. Perioperative blood transfusion and determinants of survival after liver resection for metastatic colorectal carcinoma. Ann Surg 1992;216:492–505.
Jaeck D, Bachellier P, Guiguet M, Boudjema K, Vaillant JC, Balladur P, Nordlinger B. Long-term survival following resection of colorectal hepatic metastases. Br J Surg 1997; 84:977–980.
deBaer T, Roche A, Elias D, Lasser P, Lagrange C, Bousson V. Preoperative portal vein embolization for extension of hepatectomy indications. Hepatology 1996;24:1386–1391.
Wajabayashi H, Ishimura K, Okano K, Izuishi K, Karasawa Y, Goda F, Maeba T, Maeta H. Is preoperative portal vein embolization effective in improving prognosis after major hepatic resection in patients with advanced-stage hepatocellular carcinoma? Cancer 2001;92:2384–2390.
Elias D, deBaere T, Roche A, Bonvallot S, Lasser P. Preoperative selective portal vein embolizations are an effective means of extending the indications of major hepatectomy in the normal and injured liver. Hepatogastroenterology 1998;45:170–177.
Makuuchi M, Thai BL, Takayasu K, Takayama T, Kosuge T, Gunven P, Yamazaki S, Hasegawa H, Ozaki H. Preoperative portal embolization to increase safety of major hepatectomy for hilar bile duct carcinoma: A preliminary report. Surgery 1990;107:521–527.
Abdalla EK, Hicks ME, Vauthey JN. Portal vein embolization: Rationale, technique and future prospects. Br J Surg 2001;88:165–175.
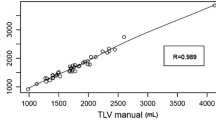
Vauthey JN, Chaoui A, Do KA, Bilimoria MM, Fenstermacher MJ, Charnsangavej C, Hicks M, Alsfasser G, Lauwers G, Hawkins IE, Caridi J. Standardized measurement of the future liver remnant prior to extended liver resection: Methodology and clinical associations. Surgery 2000;127:512–519.
Leisenring W, Alonzo T, Pepe M. Comparisons of predictive values of binary medical diagnostic tests for paired designs. Bioemtrics 2001;56:345–351.
Casella G. Refining binomial confidence intervals. Can J Stat 1987;14:113–129.
Shirabe K, Shimada M, Gion T, Hasegawa H, Takenaka K, Utsunomiya T, Sugimachi K. Postoperative liver failure after major hepatic resection for hepatocellular carcinoma in the modern era with special reference to remnant liver volume. J Am Coll Surg 1999;188:304–307.
Jarnagin WR, Gonen M, Fong Y, DeMatteo RP, Ben-Porat L, Little S, Corvera C, Weber S, Blumgart LH. Improvement in perioperative outcome after hepatic resection: Analysis of 1803 consecutive cases over the past decade. Ann Surg 2002;236:397–406.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shoup, M., Gonen, M., D’Angelica, M. et al. Volumetric analysis predicts hepatic dysfunction in patients undergoing major liver resection. J Gastrointest Surg 7, 325–330 (2003). https://doi.org/10.1016/S1091-255X(02)00370-0
Issue Date:
DOI: https://doi.org/10.1016/S1091-255X(02)00370-0